Lauren’s Stage 1 CDH1+ Hereditary Diffuse Gastric Cancer Story
Lauren shares her stomach cancer story, one that began after testing positive for the CDH1 genetic mutation. She underscores going through a total gastrectomy, a surgical removal of her stomach, as well as recovery.
She also highlights how she navigated important quality of life issues, like the importance of patients advocating for themselves and finding support in a cancer community. Thanks for sharing your story, Lauren!
- Name: Lauren C.
- Diagnosis:
- Stomach cancer
- CDH1 Gene Mutation
- Staging: 1
- 1st Symptoms:
- Irregular bowel movement (stomach bile)
- Extreme pain eating certain foods or drinking alcohol
- Treatment: Total gastrectomy (surgical removal of entire stomach)
- CDH1 Genetic Mutation
- Screening for Stomach Cancer
- Treatment Decisions (Getting Stomach Surgery)
- Biggest risk: stomach cancer
- Physical signs something might be wrong
- Describe the physical pain (1 to 10)
- The moment you decided to pursue surgery
- Why did it take four years to schedule the surgery
- Finding the right surgeon (Be your own advocate)
- Dealing with unwanted opinions
- Emotionally preparing for major surgery
- What drove the fear?
- The Surgery (Gastrectomy)
- Surgery Recovery
- Dealing with News of Cancer
- How CDH1 Mutation Has Changed Your Life
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I’m surprised because beforehand, I wouldn’t even look at people who had it because I didn’t want that negativity in my life or at least I called it negativity.
But now, I’ve turned into that person that wants to share my story because I don’t want somebody to be as uninformed as I was.
Lauren C.
CDH1 Genetic Mutation
CDH1 genetic mutation
I have a genetic mutation called CDH1 and so I had a really high, over 80-percent chance compared to the normal person of having stomach cancer.
I have an over 60-percent chance of having breast cancer compared to the normal person. I have an increased risk of colon and ovarian cancer, as well.
I had biopsies done and they came back clear. I decided to get my stomach removed at a young age as a preventative surgery. I actually didn’t know I had cancer going into the surgery. I had a biopsy done three months before my procedure and it came back completely clear; no cancer was found.
It was only after I did the preventative surgery and they cut my stomach open completely, they found stage 1 cancer in three places. So I didn’t have any symptoms at all. I did this as a completely preventative action.
Luckily, I did.
How did you know you had the CDH1 mutation
My mom found out she had it. We had a genetic counselor reach out to us because cancer was really prevalent in our family. My grandma had breast cancer at 29 so that was a big red flag for them. They actually thought we had the BRCA gene which my mom tested negative for.
They went off on a whim and were like, ‘Hey we have this one test, it’s really, really rare and you probably don’t have it but we’re going to test you for it,’ because it was very new at the time.
I think we were the first people my genetic counselor had ever tested positive for. My mom tested positive. She was told each of her children had a 50-percent chance of having it.
I was already over 18 at the time. I went and got the test done. My brother tested negative. My sister and I tested positive.
Describe the genetic test
They call you into an office and you spit into a tube. That’s it. It took not long to get results. I was a little upset because I got the results over the phone from the counselor when she told me that they would call me in to tell me the results.
Since I tested positive, it was a very traumatic experience. It took about two weeks after getting the test done that I was told it was positive.

Getting the news over the phone
My mom had actually just had her stomach removed two weeks before I got the news. Once of her stitches had come undone and she had to go back to Johns Hopkins to get it fixed.
I was in my bedroom. I got the call and called her. I was screaming. I do take anxiety medication. It was very hard to take in. Thinking about that day is hard. It was bad.
Emotionally processing the news
My brother had just tested negative for it so I was very hopeful and positive in thinking there was no way I have it.
They kept emphasizing in the meetings with the genetic counselor how life-changing it would be if I had it. I had just watched my mom get her stomach removed and I knew I would have to do that, too. I was very traumatized after seeing my mom like that.
Once I got the news I’d have to go through that, too, it was almost too much for me to handle.
I almost thought about dropping out of college. I thought about a lot of really negative things. I went into a deep depression because I knew what the future held for me and I didn’t know if I could handle it.
I spoke with one of my professors in school whom I was close with. I didn’t see a therapist. I tried to on campus but they turned me away because they thought my story was too unique.
They were training therapists. So basically, the therapy program they had on campus they wouldn’t take me in because they felt my story was too complex and so that hurt to be turned away from therapy.
I just compartmentalized it. I didn’t think about it.
I worked really hard in school. Shockingly, I got a 3.8 gpa that following semester. I didn’t think about it, or tried not to. If I did, I would spiral so I just avoided the whole thought about it.
»MORE: Processing a cancer diagnosis
Guidance for others on how to move forward
Don’t turn to stuff that’s going to alter your mind, like pot, stuff like that. It’s not the solution. Anxiety medication is not the solution because you can get addicted to it.
I definitely recommend, even though it hurts, looking at the groups on Facebook and looking for people who have the mutation through Instagram, stuff like that.
I actually blogged after my surgery and so many people around my age have come to me thanking me for talking about it. If [only] I had just read the stories instead of seeing what my mom went through, because I based a lot of my fear on just her surgery.
I wish I could have gone back and talked to someone my age who had gone through it and had a much more positive experience, and realized you will be okay.
It will be okay. It’s not the end. It seems like it. It’s really hard for someone to tell you that’s going to get better.
I didn’t listen to anybody telling me it was going to get better. I didn’t listen to my mom. I didn’t listen to my boyfriend who’s now my husband. I didn’t listen to anybody.
I partied. I wish that I hadn’t really done it. I think I did put a lot of work into school which was a positive thing, but that’s the only positive thing I did afterwards. I regret a lot of that.
You have to make a decision. If you want to get the surgery done early, that’s great, but definitely use those resources online. Talk to people. Don’t hide away. Don’t ignore it because I did and it made the time when I went into the surgery so much worse.
»MORE: Read different experiences of a cancer diagnosis and treatment

Ongoing tests to monitor the CDH1 genetic mutation
I had to go in for a biopsy on my stomach once a year. I had three biopsies leading up to my stomach removal.
Every six months, I get testing on my breasts just because I have such a high chance of getting breast cancer. They switch it off every six months because it’s a lot of radiation or something involving the MRI machine isn’t good for you, if you’re so young.
So they do an MRI once a year and six months later if everything looks good, they’ll just do an ultrasound of the area. I’ve only had one breast biopsy done.
Screening for Stomach Cancer
Next steps after learning about CDH1 mutation
I met up with doctors at Johns Hopkins; that’s where my mom had her surgery. We decided those were the doctors we were going to go with. Also, we were going to go through a [genetic testing] company. They’re the ones who did my genetic testing.
I found an oncologist and a gastrointestinal doctor. I started getting the screening done pretty immediately. I had my first MRI within two months after I found out that I tested positive.
Describe the annual biopsies
You show up to the office, they take you back, they put an IV in you, you sign some papers saying you acknowledge what’s going on. Essentially, you get rolled away and put to sleep.
You wake up and then the doctor comes in, lets you know if he saw anything or if he saw anything weird. He takes a bunch of little samples, cuts little slits out of your stomach.
But the reason they didn’t catch mine is they can’t cut a whole chunk out of your stomach so it was just chunks of the inside, not the lining, not in between, which is where my cancer was.
When he was going in cutting out all those pieces, [it was] on the inside of my stomach, that’s why they couldn’t find it.

Are the biopsies painful
I will say that when you come out of the biopsy, it does hurt. They’re literally cutting little slits of your stomach out. It’s a little painful. It’s not terrible and it only lasts about two days of pain.
After my last biopsy, that’s when I started having the stomach bile happening very regularly. I don’t know if the biopsy triggered something in the stomach, my last one at least. I’m not sure.
On a scale of one to ten, if you’re just sitting there and not eating, because eating can disrupt it, it was a three. It’s not that bad. It’s just because they have to cut out little pieces, there is some pain associated with it.
Are there scars from biopsy surgery?
No, it heals itself because they’re so small. They’re just little slivers off the inside lining of your stomach that they take. They do it in different regions. They’ll explain it to you and show you the different regions they plan on taking. For me, they took from a bunch of different places because I have this gene.
They said I had a higher chance of having it and because of that, he took from more places. My doctor was very aware of my situation and me having this mutation. I think he took from six places. I think they’d normally only do four. I know he took more from me. There’s no scarring.
How long does it take to get results from the biopsy
The doctor generally will give you the results for those in about two weeks. They can honestly say if they saw anything abnormal. If you have it and it’s bad enough, they’ll be able to see it when they go in for the biopsy.
At least that’s what they told me. I already had solid results but you will have some discomfort when you wake up from it. It just hurts a little.
Dealing with waiting for results
I’d gotten really good at compartmentalizing. Just remember it’s a biopsy and it doesn’t mean that you have it just because they do it. I hate to say it bluntly. If you have it, you’re going to find out you have it. It will change a lot. But there’s a chance you don’t have it.
The doctor I was working with said if it’s severe enough, they can tell when they go in there. He said he’d be able to notice something “off.” The doctor will come talk to you afterwards. If they say that it looked pretty clear, I wouldn’t completely disrupt your life over it.
I know that that’s hard to take into consideration because everybody reacts to stress differently. I just would say just stay as calm as you can.
Surround yourself with people who make you happy and do stuff that makes you happy. Don’t think about it until you are actually faced with the results.
Treatment Decisions (Getting Stomach Surgery)
Biggest risk: stomach cancer
They were more worried about my stomach than anything. The breast, they were like that can wait a little bit. We’re worried about getting your stomach out now. The meeting went like this:
I walked in, my sister and I were in there. I was still pretty young, around 23, almost 24. We walk into the hospital.
My sister had already found out she was positive. She was with me and my mom was there. They told us we’re worried about you getting your stomach out right now.
Your breast is a lot more easily detectable. Since this cancer grows in the lining of your stomach, a lot of times when they catch it, it’s too late. So in the meeting, I’m crying, obviously.
The doctor said, straight up, you’re gambling your life every year that goes by that you don’t get your stomach removed because it is that serious with this mutation.
They said they’d found cancer in patients as young as 16 years old who had this gene. Age doesn’t really matter is what they were saying. They were saying you could be whatever age, but they were very, very concerned and pushing very hard for me to get my stomach removed, even though it was something I wanted to do when I was 30.

Physical signs something might be wrong
There’d be stomach bile when I’d go to the bathroom instead of actual feces being solid, was something that would happen, which I thought was really weird.
It would happen randomly. I would get an abnormal amount of hemorrhoids from going to the bathroom too much. I would get really bad stomach pain when I drank. It happened mostly around alcohol, but it also would happen with certain foods.
I believed them when they said it was gastritis. It was odd that stomach bile was coming out of areas it shouldn’t be coming out. It was burning really bad when it came out, it was terrible. It would last for a whole week. I wouldn’t know what caused it.
One time I had an ale. It was my birthday weekend. I drank it and I could not do anything that whole weekend. I had to basically wear a diaper around because stomach acid was coming out of me.
It was stuff like that that I thought was so weird, I don’t know if it was the gastritis which is what they say it was, or if it was the cancer giving me signs, hey, I’m here.
Looking back, I don’t know. Maybe that was a sign or it was the cancer giving me signs, or it was the gastritis, I’m not really sure.
Describe the physical pain (1 to 10)
It was more involving my digestion, it wasn’t so much stomach pain. I did get abnormal stomach pains sometimes. It wasn’t terrible compared to menstrual cramping. I would blame it on that sometimes. I would put it at maybe a five. It really wasn’t that bad, not in the stomach.
The moment you decided to pursue surgery
I had decided in November 2018, that I was going to do it. I had graduated college. I wasn’t in a very serious career at the time. I was in real estate but I hated it so I was at a standstill in my life.
I thought that would be the best time to do it. I was also very fearful of getting cancer. It was starting to take over my life in a way to a point where I was so terrified, I decided to do it so I could get the fear out of me.
Why did it take four years to schedule the surgery
I was worried they were going to take it out and they wouldn’t have found cancer at all. Sounds kind of silly to say, but it’s true. I was really worried about that.
Obviously I didn’t want cancer but I didn’t want them to have taken it out for nothing so I was really concerned about the timing about the whole thing. I didn’t want to do it for nothing, essentially.
At first it was mainly because I was in school, still, and I really wanted to graduate college. That was the main leading factor for the first year. After that, it was fear. I was terrified of the surgery.
I also still believed I was too young. I still genuinely believed that. I thought I was way too young for this. I thought I could wait. Then it became more fear of actually having cancer. I don’t know how to explain it.
I was having some issues after my last biopsy. I was starting to have some issues with my stomach. They said it was gastritis, they didn’t say it was stomach cancer. I don’t know what it was, if it was either, but I was having some weird issues with my stomach.
I wasn’t able to drink properly for a young adult. I was having bowel issues. I hate to say it but I had a gut feeling around the time when I decided to do it. I just had a gut feeling that it was time.
I just decided I was going to get it done eventually, I might as well put the fear aside and just do it. It really was just a battle of do you want cancer or not?
They said I was going to get cancer in my stomach, they just didn’t know when, because I have this gene. So it was just a matter of when I wanted to do it or when to get cancer.
Finding the right surgeon (Be your own advocate)
I originally had planned to get the surgery done by one surgeon. I went and met with her, and my mom conference called in. This was in March when I went home to get some testing done before. I went to meet with my surgeon. I was supposed to get it done by one surgeon I will not name.
To be honest, she didn’t know what she was talking about.
She said a lot of stuff that didn’t make sense. She was saying I was too young. When you take your whole stomach out, they put a little pouch in to help keep food in. She was saying she wasn’t going to put the pouch in so my mom said no, you’re not getting it done by her.
I had a literal panic attack because that was my surgeon. I had my date scheduled already with her. So leaving her office I was already a mess because I knew I was about to get my stomach removed.
When I was home and met with the surgeon and it didn’t go well, my mom called Johns Hopkins and immediately they wanted to meet with me with their surgeon for this, their gastrointestinal surgeon. So while I was home, I met with him, too.
He was way more knowledgeable and we ended up picking him. They told me they would give me a call in a couple of weeks and they were going to schedule the surgery. I didn’t realize, ironically when they called me to schedule it, it was the same date that I had scheduled with the other surgeon.
I felt like it was fate. I was meant to get it done on that day because I didn’t even suggest that date to the other surgeon. They just called and said that date. It was really weird.
»MORE: How to be a self-advocate as a patient
Dealing with unwanted opinions
I had people doubting me. My husband doubted me. He was questioning why I was doing it so young. My father did not believe it at all. He pretty much didn’t believe the whole mutation was a thing and questioned me a lot, too. I had a lot of questioning from my family.
Not my mom, she was really the only one who didn’t question me because she had had it happen to her.
And she was in the doctor’s appointment when they told us we were ticking time bombs. That’s actually the exact words they used. Ticking time bombs. It was kind of scary. No one wants to hear that.
Emotionally preparing for major surgery
The day they officially scheduled with Johns Hopkins, I was terrified of getting it done. It was for sure going to happen. I remember getting really drunk. I could not deal with it.
I was actually in the car with one of my co-workers and I couldn’t even control myself. I couldn’t stop crying. I drove myself home. A lot of the time leading up to the surgery I just ate.
They said to put on a lot of weight because you lose so much weight when you don’t have a stomach. So I ate as much as I could. Honestly, I drank a lot of alcohol, I’m not going to lie about that.

What drove the fear?
I didn’t even know before that you could live without a stomach.
To say it out loud is one thing but when you’re actually on the schedule to get your stomach removed, that’s another thing. When it becomes a reality, it’s terrifying.
I had just turned 26, days before. I was about to get my stomach removed. I had seen my mom get sick almost every day for a whole year after her surgery. I didn’t want to get sick. I didn’t want to deal with that.
There’s this thing called “Dumping Syndrome” where you go to the bathroom uncontrollably because food moves through your intestines too quick. I didn’t want to deal with any of that.
I was terrified of the pain associated with the surgery. I was very, very scared it was going to hurt because I watched my mom go through it.
They did tell me I was going to have a nerve block but it was terrifying thinking about having something so major, something that you literally use every day, taken out of your body.
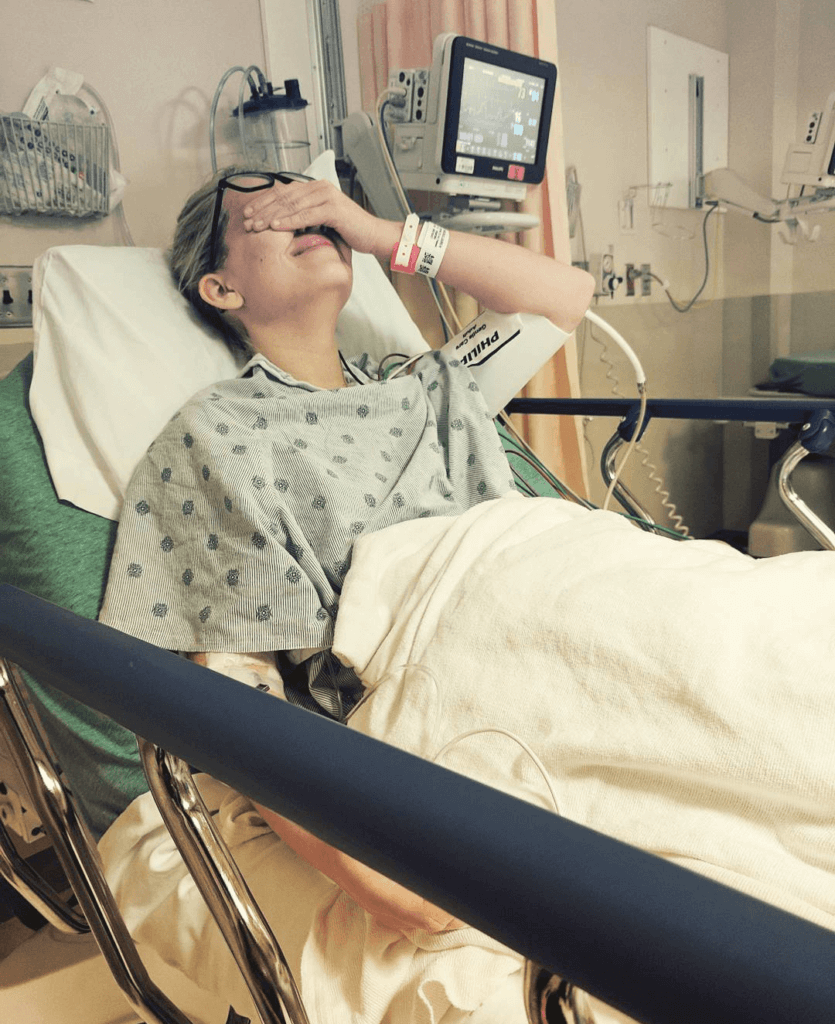
Even up until the morning of my surgery, I still couldn’t imagine living without a stomach until they were literally rolling me back. Then I was panicking. They gave me medication to help calm me down but I couldn’t fathom it until they were rolling me back.
The Surgery (Gastrectomy)
Preparing for the gastrectomy (stomach surgery)
I started putting on weight before scheduling the surgery, around November, because I got married December. My wedding dress couldn’t be altered so I was very small, petite the day of my wedding.
I only started putting on weight for less than six months and I put on over 30 pounds.I ate a lot of fast food. It was really bad for you but they told me to do it. They encouraged it actually.
Cleanse before surgery
I just had to take a laxative, Miralax, which takes a couple days to work sometimes. They didn’t tell me that. I wish I would’ve known. So no. It was a little weird. I was like what if there’s stuff in there?
I don’t know if that sounds silly, but someone else might be wondering it, too. Somehow they can take it out without you having to do a cleanse.
How long did the surgery take
It was longer than it should’ve been. He said it would only take six hours max. My surgeon actually got called into another surgery for an emergency. He had to leave my surgery at one point. I didn’t know obviously.
My family was like, what the hell, you just left. My dad apparently said to him, ‘So you left my daughter?’ My doctor said he had to. So I was in there an extra two hours, a total of seven hours.
»MORE: Read more patient experiences with surgery
Surgery Recovery
Waking up from surgery
Waking up, I remember my first moments of consciousness, which is weird when you’re under anesthesia, most people don’t. I woke up in the ICU and my family was surrounding my bed. I had a lot of family members there actually. I had a good amount.
My whole bed was surrounded by people. They were only allowed back there for a few minutes and then my husband was the only one allowed to stay.
Excuse my language, when I woke up, I said, ‘I did it, I fuckin’ did it’! I was awake. I was alive.
And there was pain but it was not unbearable. I could not believe that I had just gone through with it.

So I woke up in shock. The pain was bad but was it something that people can’t deal with? No. You’ll be fine. They give you medication to help you. The doctors want you to be as comfortable as possible.
When I was in the ICU the first night, I did fall asleep and my husband fell asleep, too, so I had nobody to press my medication button. You have a button that shoots Dilaudid or whatever into you and helps with your pain.
I fell asleep for about eight hours, woke up with excruciating pain, but once I called them in, the ICU people were rushing with medication and they helped me. I remember the first moments I walked.
They had me up and walking within 24 hours of being out of surgery.
I remember standing up for the first time and I could feel the emptiness and it was weird. It felt like everything was shifting into place because it was the first time gravity was taking effect.
It hurt. It definitely hurt to move. It was hard to move. I was walking so slowly. But the fact that I was up and moving within 24 hours was pretty amazing. They were very surprised.
My mom was not able to do that. That was the first day I was in the ICU and then I got my room. Then I was in the hospital for another six nights. I was there a total of seven nights.
Describe the weeklong hospital stay
Being in the hospital sucked, to be honest. I had to get Heparin shots, which is a blood thinner. Twice a day, every day. I was bruising so easily. I looked like a rag doll when I left. I had bruises all up my arms and my legs. I had just lost my stomach.
The first couple of days you aren’t allowed to eat or drink until they can make sure that the actual esophagus is fully combined with your intestine. To do that, they have to do an X-ray.
“Charcoal slushie” before X-ray
This is the worst part of it all, at least for me. When I went down to get the X-ray, they make you drink this charcoal drink so they can see what’s inside. I thought I was going to throw it up all over the techs. They kept messing up, too. I remember they had trainee people in there so I had to get up and down off that table four times.
I had just had my stomach removed. It was my third day out. I hadn’t drunk any water and here I am sucking down a charcoal slushie. The taste is indescribable and I will not sugarcoat that moment for anybody.
But the fact that I’m saying that is the worst moment for me in the hospital says a lot.
My surgeon did a really good job. It was laparoscopic so he didn’t cut me open, he did multiple incisions so the pain wasn’t as bad although my nurse had told me that laparoscopic you have a lot more gas in there because they had to pump you up with gas to see with the cameras. So I was bloated really badly.
Learning how to eat again
It wasn’t a fun experience at the hospital. I hated being there. By the time I left, I was able to eat soup and just liquids. Water, orange juice, apple juice for my blood sugar. I wasn’t hungry, anyway, so it didn’t bother me that I hadn’t eaten.
It was Day 5 when they were like okay, you can eat food. They tried to give me a shake. I almost threw it up. Ever since my surgery I’ve had an issue with lactose, milk even – I can’t drink milk. I found that out in the hospital really early on.
I’ve tested it since then and it’s terrible, so them giving it to me at that time was awful. I was able to eat a little bit of soup. I could eat sherbet. Little things of sherbet. I ate those easily. And sorbet.
Watching the bowel movements
I didn’t have a bowel movement in the hospital. They called me once a week for about three weeks after and the nurse who called would ask if I had a bowel movement.
I had at that point after leaving but when I was in the hospital I didn’t have a single one. Through the X-ray they could see that everything was intact and working properly. I just didn’t go to the bathroom.
What got you discharged from the hospital?
The doctors who were watching over me, my surgeon would only see me twice after the surgery because he wasn’t really in charge, they would come in and ask me:
What’s your pain level?
How are you doing?
Are you eating?
Are you able to eat?
Are you walking?
How much can you walk?
I was able to walk a lot. The hospital is in little quarters in a circle. The floor I was on, I could do eight laps if I really wanted to. I was walking a pretty good amount. They were very impressed at how quickly I was able to move. The fact that I was doing a lot of things on my own.
I could go to the bathroom on my own. I was doing pretty well. They were pretty surprised. I remember the sixth night I was there, the night before my last day, I was mad they were keeping me because they said they might have let me out on the sixth day but they didn’t. They kept me until the seventh.
»MORE: Mental and emotional support when leaving the hospital
Tips on making hospital stay better
Sleep when you can, as much as you can, because there will be a tech in your room at midnight doing some vitals and it’s really annoying, changing your IVs. I think the worst thing about the hospital is just be ready for a lot of needles, as bad as that sounds.
I’ve never had a problem with them, I don’t love them, but I didn’t have an issue. I got a lot of shots. A lot of IV changes. Don’t expect the food to be good because it’s not. I can tell you that right now – the food sucks.
Not as painful as expected
I can say till I’m blue in the face, it’s not as painful as it was going to be. It really isn’t. I actually don’t feel like I have a super high tolerance for pain.
It wasn’t the pain I was expecting, at all. I was expecting much worse.
Dealing with News of Cancer
Results of cancer detection (appointment with surgeon)
It was originally supposed to be seven days after my surgery, but my surgeon was out of town, so it was about nine days after I had been discharged from the hospital, or about two weeks after the surgery in total. My husband was with me and I just had a gut feeling that I had cancer.
I’m kind of a pessimist to be honest so my husband’s like, “You don’t have cancer. They haven’t said anything, you’re fine.”
We’re sitting in the waiting room arguing about it right before I get called back. It was an emotional appointment.
They called me back and he’s like do you have any questions? I’m like obviously, did you find cancer in my stomach? He goes yeah we found cancer in three places. I just started sobbing. I knew it. I had a feeling in November the year before that I had it.

He was confused as to why I was crying and I was like, ‘Why are you confused? This is terrible! Do I have to get more testing done? Did it spread? Am I okay? Do I need chemo? Do I need radiation? Do I need help?’
He’s like, ‘No, the areas were so small, stage 1, they were all in the lining in your stomach, it did not spread.We caught it just in time.’
I said, ‘If I hadn’t come in and gotten it done when I did, how long would I have had?’ He said I would have at least known that I had it within a year.
It spreads super quickly. They kept saying this type of cancer spreads really fast and in the lining of your stomach, which is why it’s so dangerous.
He said I would have for sure known I had cancer within a year. I asked him would I have made it to 27? He said there’s no way to know exactly, but probably not.
How did you process the cancer diagnosis
I was upset. I was sad. I was really scared it spread and maybe he was wrong. Maybe he was wrong about that. Maybe it did spread. I called my mom. I was worried about my sister who’s younger than me and who has not had the procedure done.
I’m the youngest person in my family at this point in history to have had cancer. I was traumatized. I did not see any positive to it, at all. My husband did, he said, “They got it out in time! What’s wrong?” I’m like, “I had cancer! How does somebody just deal with that?”
»MORE: Processing a cancer diagnosis
Next steps
He was like we got it. He held my hand and said we did it just in time. He’s like you’re good. If you honestly want to get a follow-up appointment because you’re super paranoid, I understand, we can make that happen if you want to make sure it didn’t spread.
He’s like, I know it didn’t spread. We got it. I’m glad I did it when I did. That was a good decision.
Did you get a post-surgery scan?
I thought about it but no, I didn’t.
Finding your cancer community
I actually didn’t tell anybody. I told people closest to me, only one of my friends, that they had found cancer for about two months after the results. Then I finally made an Instagram about it. Then I actually started blogging about it, about my recovery.
And I’ve met so many people who have the same gene as me, just by doing that. I’m surprised because beforehand, I wouldn’t even look at people who had it because I didn’t want that negativity in my life, or at least I called it negativity.
But now, I’ve turned into that person that wants to share my story because I don’t want somebody to be as uninformed as I was.
»MORE: Join other patients and caregivers on The Patient Story social media community
How CDH1 Mutation Has Changed Your Life
Other cancer risks
I still worry about getting breast cancer. I have to get a double mastectomy as a preventative surgery, which I plan to do before I’m 30 because now I know cancer doesn’t discriminate against age.
I always knew that but I especially know it because it happened to me. So I don’t want to take a chance with my breasts. Since I’m going to get them done, I want to get it done before I’m 30.
There is a part of me that is living in that moment, living in fear, still reminded that cancer could still very much happen to you, and that sucks. I really didn’t think that this would happen to me, but then again nobody ever thinks it would happen to them. I didn’t think I would have the gene in the beginning.
How has your lifestyle changed?
It’s changed. I cannot eat sweets. I get this thing called ‘Dumping Syndrome.’ It’s really awful which they’ll tell you if you have to get a total gastrectomy.
My diet is different. I eat smaller meals throughout the day rather than three meals. I eat six small meals a day. I have an issue with lactose, I can’t do anything with milk. I can do milk in moderation with cereal but sometimes it will make me super sick. I threw up last week or a couple days ago, so it does still happen.
It’s rare now but it was about three or four months I was throwing up almost everyday following the procedure. I couldn’t keep anything down. I would eat five dry cheerios and then I’d throw them right up.
It was a hard recovery, it’s worse than the procedure. Some people say you don’t get hungry because you don’t have a stomach but no, you’re still hungry. And you crave the foods that you ate before. You still want them.

Blogging
I wrote a whole blog article about it called “Trial and Error.” That’s what they tell you.
After the surgery, everything is trial and error. You’re going to eat some stuff that’s going to make you sick, but you’re going to have to eat it to know what you’re able to eat because everyone’s different.
I’ve come across people who can eat donuts and drink coffee. I can’t do that. I can’t eat donuts. I can’t do sweets at all. My mom can. Everyone is completely different with that. I am a lot better. I don’t get sick everyday.
There was a time for a while I was getting sick every single day. I was blogging about what I was going through and I did have some people who were reading it but as I got better, I stopped doing it.
B-12 shot (and tips)
I have to give myself a B-12 shot every month, which is weird, having to give yourself a shot. So there are small things like that you have to adjust to, that are hard. I do it in my leg.
It can be done anywhere because it’s intramuscular so you can do it anywhere, but I do it in my leg because I have the viewpoint on my leg and I can see what’s going on. I do it on my side of my leg, my outer thigh.
If you don’t like needles, just get your primary physician to do it. You can go in once a month and do it. I use a diabetic needle so it’s smaller. It’s really not bad.
I don’t think it’s bad, but I feel after you get your stomach taken out and having to go through all of the doctor’s appointments and the needles, the bloodwork, all that, I don’t know if you’ll be scared of needles after it. At least I’m not. It’s really not a big deal. I do it once a month.

Decision to get a double mastectomy
I don’t want to get cancer. My mom hasn’t even gotten her breasts done and she’s over 50. She says she doesn’t think she’s going to. But since I’ve already had cancer, I’m 25. The odds really don’t seem to be in my favor when it comes to my health, I don’t know why. I have switched to natural deodorant.
In the end, for me, when it comes down to it, I don’t want to suffer from cancer. I know breast cancer is more easily detectable, so if you’re willing to get the testing done and keep up with it, I think that’ great and I admire you. But I’d rather just get it done.
They give you implants. It’s basically just a boob job. For me, that’s just how I think of it and I would rather get it done and not have to worry about it. My anxiety is terrible revolving around it.
Message to other CDH1 mutation carriers
It’s honestly not that bad. It does suck and sometimes I still say, man, God, I wish I had a stomach so I could drink my Starbucks and not get sick. Or eat or drink this, and not get sick.
But one of my doctors, who I’m still pretty good friends with, I still call her, she’s the one who asked me to do this.
She told me to put my big girl pants on because a lot of people have it worse. And I’ll be okay.

Inspired by Lauren's story?
Share your story, too!
Stomach Cancer (Adenocarcinoma) Stories
Lauren C., Stomach Cancer Stage 1, CDH1 Mutation
Cancer details: CDH1 mutation led to “hereditary diffuse gastric cancer” (HDGC)
HDCG cancer risks: “Frequently, HDGC-related cancers develop in individuals before the age of 50” (NIH)
Treatments: Total gastrectomy (surgery to remove whole stomach)
...
Viola K., Stomach Cancer, Stage 4
Symptoms: Persistent fatigue, Weight loss, Occasional pain, Persistent weakness
Treatment: Chemotherapy (FLOT), HIPEC (Surgery + Hot Chemotherapy), 2nd intestinal surgery
...
