Daniella’s Stage 2 Primary Mediastinal B-Cell Lymphoma (PMBCL) Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

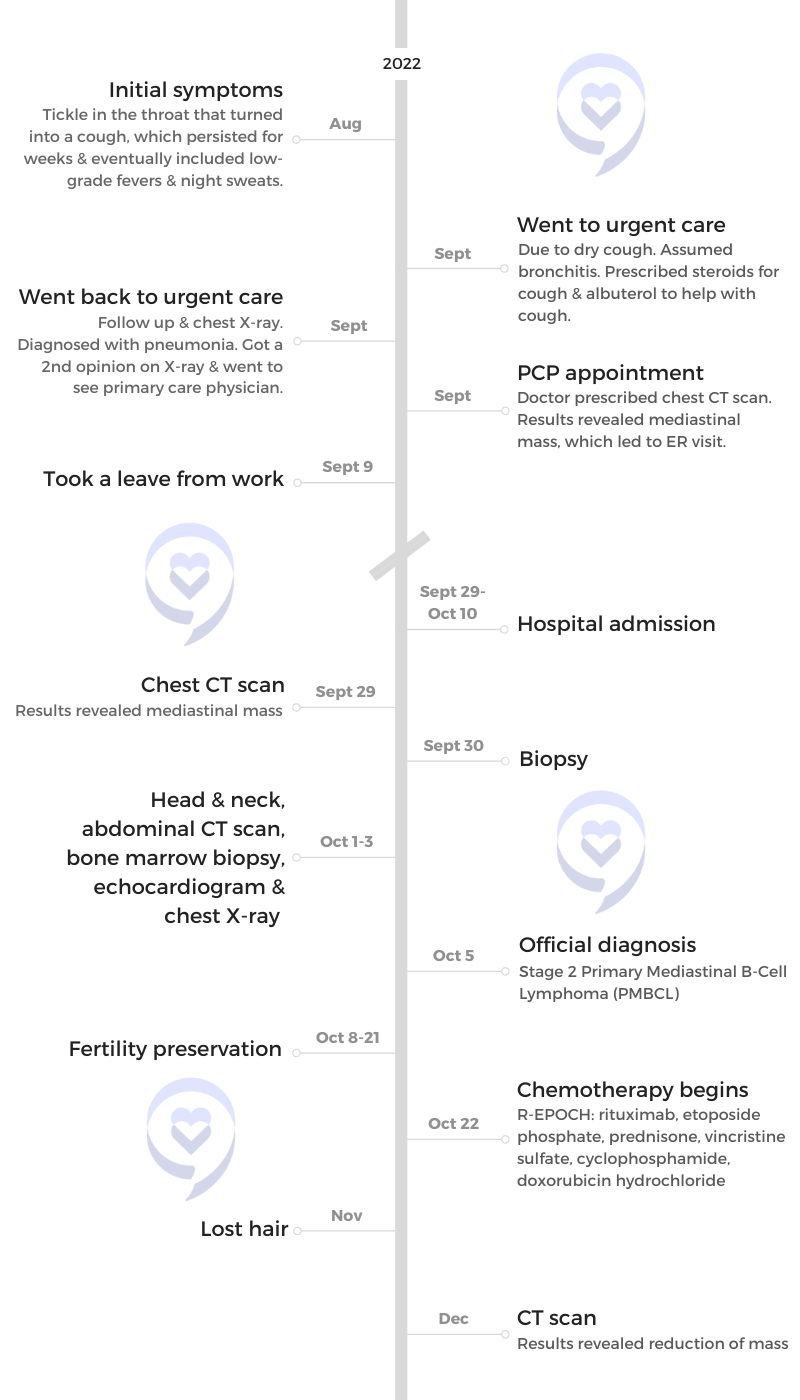
Daniella recounts her journey through a stage 2 PMBCL diagnosis. She underwent chemotherapy and CAR T-cell therapy, and ultimately achieved remission. Initially attributing her symptoms to allergies, she experienced a persistent cough that worsened over time, accompanied by night sweats and low-grade fevers. Concerned by her symptoms, she sought medical attention and underwent various tests, leading to a diagnosis of primary mediastinal B-cell lymphoma (PMBCL).
Facing the shock of her diagnosis as a 28-year-old with no prior health issues, Daniella embarked on a treatment journey that included chemotherapy, fertility preservation, CAR T-cell therapy, and radiation. Throughout her treatment, she experienced side effects such as hair loss, fatigue, nausea, and fever, but she found strength in focusing on the present moment and relying on her support system, including family, friends, and medical professionals.
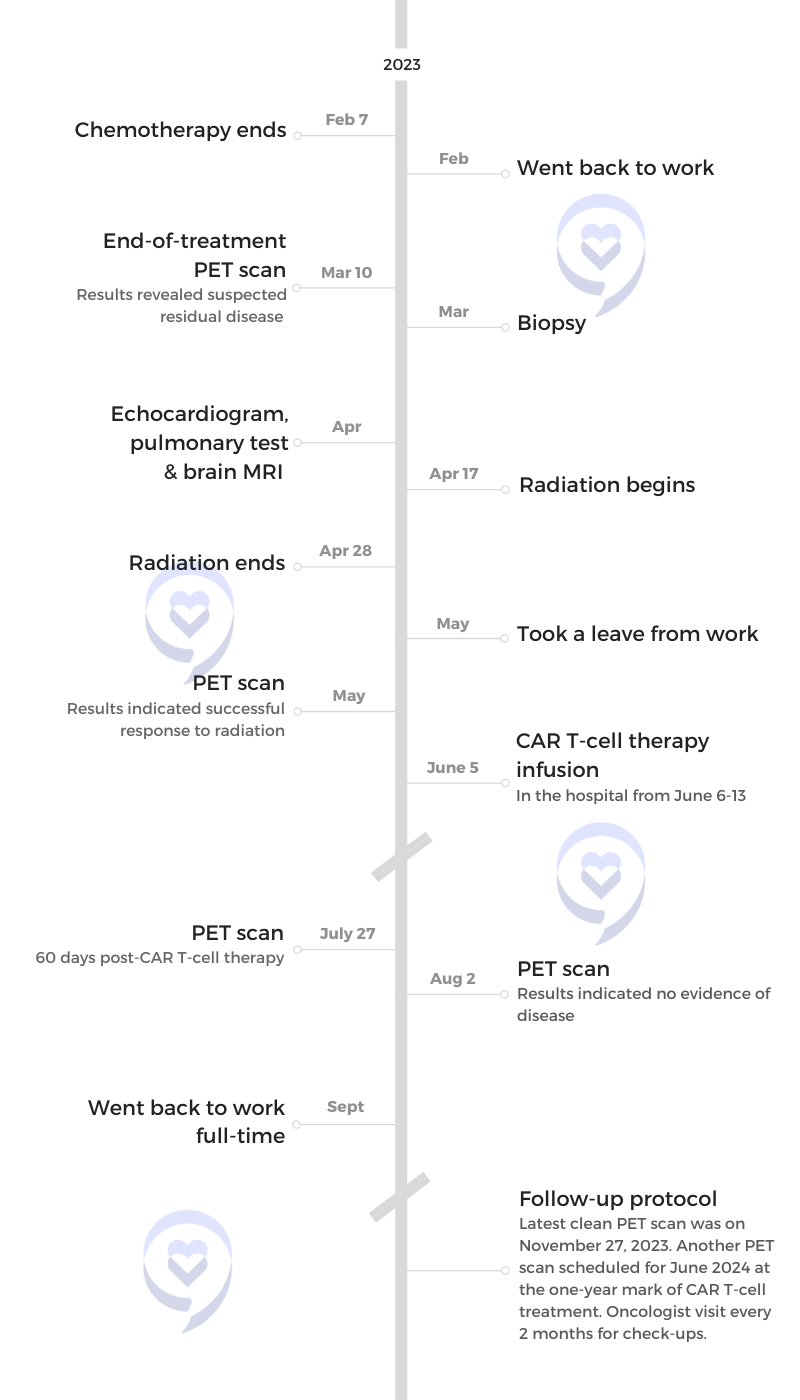
Despite setbacks and challenges, including a bout of COVID-19 and the discovery of residual disease after chemotherapy, Daniella remained resilient. She underwent CAR T-cell therapy, navigating delays and side effects, and ultimately achieved remission.
She acknowledges the ongoing emotional and psychological impact of her cancer journey, emphasizing the importance of taking things day by day, seeking support, and connecting with others facing similar experiences. As she continues to navigate survivorship, she encourages others facing cancer to lean on their support networks, seek professional assistance when needed, and remain resilient in the face of adversity.
In addition to Daniella’s narrative, The Patient Story offers a diverse collection of primary mediastinal B-cell lymphoma (PMBCL) stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Daniella S.
- Diagnosis:
- Primary Mediastinal B-Cell Lymphoma (PMBCL)
- Staging:
- 2
- Initial Symptoms:
- Prolonged cough
- Low-grade fever
- Night sweats
- Treatment:
- Chemotherapy (R-EPOCH)
- Radiation
- CAR T-cell therapy
Introduction
I grew up in the Tri-State area. I work for a large communications firm in New York City and live in Jersey City with my fiancé and dog.
Pre-diagnosis
Initial Symptoms
The journey started in the summer of 2022. It began with a tickle in my throat, which was very vague, and I attributed it to either allergies or the dry air in my apartment.
After a while, that tickle turned into a cough, which didn’t go away. After a few weeks of having that cough, I decided to go to urgent care. They thought I had bronchitis, which I thought was likely. I figured whatever I had probably turned into bronchitis. I was working a very high-paced job, was very career-oriented, and dismissed a lot of my initial symptoms.

The doctor said it was the night sweats that concerned him the most. I don’t think that he thought of a potential cancer diagnosis because I was otherwise healthy.

Symptoms Worsening
My symptoms got worse. When I went to urgent care, I was diagnosed with bronchitis and they treated me with steroids. My cough improved, which was great, but when I went off the steroids, my cough came back immediately. I went back to urgent care and they thought I had pneumonia.
The cough lasted four weeks before I thought it seemed like a long time to be going through it. I also started to develop a low-grade fever in the evenings. Even further along, I started to have night sweats, which I later learned was one of the symptoms of lymphoma.
The night sweats became apparent to me because they came with low-grade fevers. That’s when I thought I needed to see a doctor urgently because I knew that I was sick.
The doctor said it was the night sweats that concerned him the most. I don’t think that he thought of a potential cancer diagnosis because I was otherwise healthy. He was ticking off other things that it could be, but he called out the night sweats as concerning.
The night sweats got progressively uncomfortable to the point where I was waking up in the middle of the night to change my clothes. But I attributed that to some infection that had gone on for too long and now becoming severe. I didn’t even consider cancer.
My mom pushed me to ask for a chest X-ray from the urgent care doctor. The radiologist thought it was pneumonia, but the doctor scared me when I was told that it could be tuberculosis. I decided to get a second opinion.
Getting a Second Opinion
I sent the X-ray to my cousin, who’s a radiologist. She said the X-ray would be a lot worse if I had pneumonia. She pushed me to get a CT scan. I went to my primary care doctor and got a CT scan, which immediately revealed a large mass in the center of my chest.

My cousin prepared us for the different possibilities, but it was still very much a shock.
Diagnosis
This was something that we were anticipating at this point. My cousin prepared us for the different possibilities, but it was still very much a shock. I was an otherwise healthy 28-year-old with no prior history of anything and no history of lymphoma.
My primary care doctor asked me, “Do you work around any chemicals?” I said, “Unless you’re talking about the chemicals from the New York City subway, I don’t. I work in an office. I work on the computer.”
It was a huge shock when I was initially diagnosed. Upon receiving the results of the CT, we immediately went to the ER. From there, the process started in terms of finalizing my diagnosis.
Reaction to the Diagnosis
It was a crazy out-of-body experience for me. I would say I was somewhat primed for it. I was with my fiancé at the time, but I don’t know how primed he was for it. I remember seeing his face and the color draining from it. I immediately had an out-of-body experience and emotionally shut down in a way.
I knew that I needed to go to the ER so I didn’t have time to process what it all meant. The moment I received the news, I was shaking.
From that point on until the day I heard I was in remission, every moment of my life was lived minute by minute. I remember thinking to myself, I’m going to the ER. I’m going to the front desk. I’m telling them what’s going on. I’m sitting in my chair, waiting. They’re going to take me back to the ER.
I was living moment to moment, doing my best to not anticipate what was next. My life went from everything being planned to getting through by the minute, by the hour, or by the day. It was a big mindset shift for me.
In the initial moments of my diagnosis, I distinctly remember thinking that this couldn’t be happening to me. This is too insane. I was supposed to get married in seven months.
I thought that I couldn’t do this. I have an extreme fear of needles. How am I going to make it through knowing that they’re going to need blood work? I actively avoided needles for a long time and any blood work that wasn’t necessary. That’s how bad my phobia was so that was one of the main things that I discussed with everybody because that was tough for me.

The interventional radiology team that did the biopsy was wonderful in keeping me calm throughout the process. They were so confident in what they were doing that it made me feel more relaxed and very well taken care of.

Doing the Biopsy
I was admitted upon going to the ER. They had my CT results. From there, there were various consultations with doctors and potential surgeons to understand what we should be doing about the mass, considering that it was pushing on my chest and my heart, causing me to cough and some fluid to build up in my lungs. There was a lot of discussion on what we should be doing at this point.
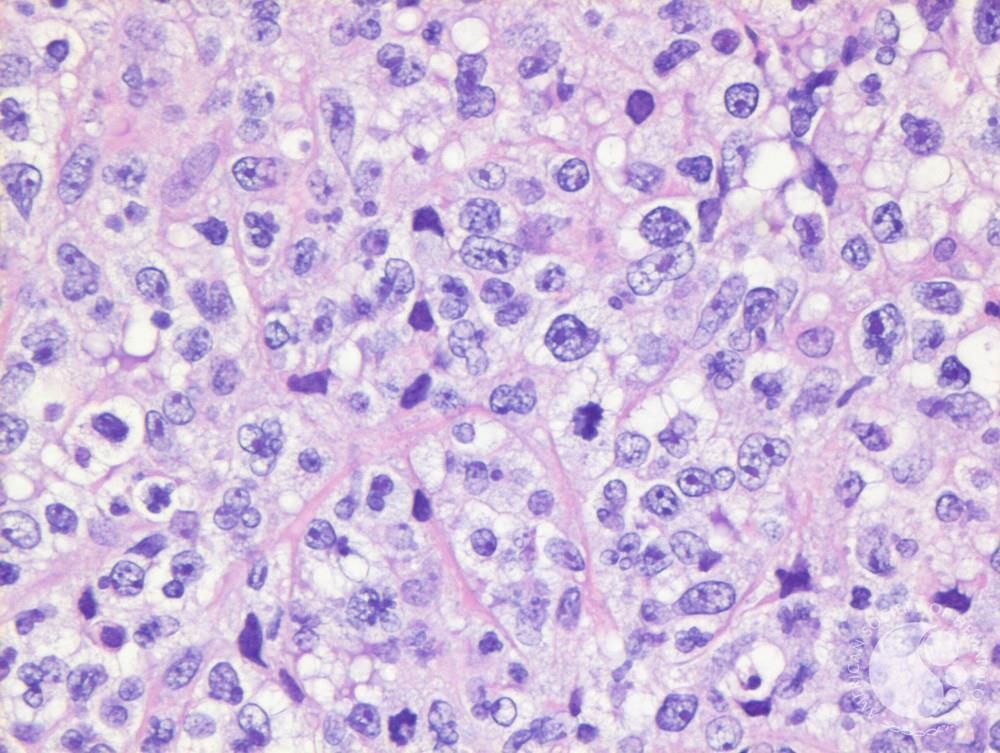
They ultimately decided that they didn’t need to do anything urgently, but they scheduled a biopsy for me. They went back and forth to decide what type of biopsy to do. Ultimately, they went with a needle biopsy to get pieces of the tumor in my chest to be able to do the diagnosis and staging.
They wanted to do the biopsy before the weekend. I wanted to be knocked out during the whole process, but unfortunately, I had breakfast that morning before I knew that they were going to do the biopsy. To do the biopsy under anesthesia, I wasn’t supposed to eat, so they had to do the biopsy while I was awake. Luckily, they gave me lorazepam (Ativan) via IV so I was able to calm down before the biopsy.
Honestly, that experience went well and opened my eyes to a lot in terms of how this medical process works. The interventional radiology team that did the biopsy was wonderful in keeping me calm throughout the process. They were so confident in what they were doing that it made me feel more relaxed and very well taken care of. It was the first procedure that happened to me in my journey that made me feel like I could do it. That was the first moment of encouragement for me, knowing I could get through this.
Additional Testing
Following the biopsy, I had to have additional CT scans of my head, neck, and stomach. I also had to have a bone marrow biopsy to confirm the staging to see if the lymphoma was anywhere else.
The bone marrow biopsy was done under anesthesia. I was a little sore afterward and a little nauseous from the anesthesia, but otherwise, it was fine.
Getting the Official Diagnosis
After all of that testing, I got my final diagnosis a few days later. It was confirmed that I had stage 2 PMBCL or primary mediastinal B-cell lymphoma.

I started the fertility preservation process while I was still in the hospital.

Fertility Preservation
I was lucky to be able to do fertility preservation before starting chemotherapy, which I realized after my treatment was very rare. There were a lot of things that lined up that allowed me to do fertility preservation.
The fertility clinic is inside the hospital. When I was diagnosed, they kept me in the hospital for 10 days while they were doing all the procedures and monitoring. During that time, my doctor consulted with the fertility doctor at the clinic and she was able to come down to see me and talk to me about my options.
I started the fertility preservation process while I was still in the hospital. Had the clinic not been in the hospital building itself, they probably wouldn’t let me be discharged to undergo fertility preservation. When I decided to move forward, I was able to go to the clinic and do the tests that they needed. Otherwise, I don’t know if they would have let me so I was very fortunate in that sense.
Honestly, it took me a while to figure out that this was even going to be a part of the journey, but upon hearing what my options were, I was firm in my decision. That being said, I was also very scared because I knew it involved a lot more needles. Of course, that wasn’t fun, but I was no longer operating in what I wanted, but more so what I needed to do.
I went to the fertility clinic every day for blood work. They would monitor me and how my eggs were growing because they gave me hormones to stimulate my eggs so they could retrieve them.
I was doing hormone shots in the evening and going to the clinic so they could check on how my eggs were growing. After the clinic visit, I would go down to the cancer clinic where the doctor would check me. They were afraid that my cancer would grow since it’s a very aggressive lymphoma, that my symptoms would get bad again, and that I would need to start chemotherapy immediately.
I would go to the fertility clinic and then the cancer clinic every morning to see my doctor and get checked out. Then I would get myself an emotional support bagel and lay around all day and think about what was going on.
The fertility preservation process was not that bad. Besides some minor discomfort and minor bloating, it was very manageable.

They were able to retrieve seven eggs. My fiancé and I decided to fertilize all seven eggs in the hope of creating healthy embryos.

Egg Retrieval
Upon my egg retrieval, my doctor warned me that my body was fighting something so there was a chance that they might not be able to get any eggs. I went in understanding that it might not turn out how we wanted, but they were able to retrieve seven eggs. The procedure was done under anesthesia, which was something I was very familiar with at the time. The egg retrieval process itself was fine.
I had the egg retrieval done in the morning. I was out of there probably by noon or 1 o’clock. After they did the retrieval, they brought me to the recovery area. When I woke up from anesthesia, they wanted me to walk around a little bit before sending me home. That evening, I was admitted to the hospital for my first round of chemotherapy.
Embryo Freezing
They were able to retrieve seven eggs. My fiancé and I decided to fertilize all seven eggs in the hope of creating healthy embryos because that’s what my doctor recommended. If I were to freeze seven unfertilized eggs, they might not survive the thawing process. Embryos are a little more robust. They’re a little tougher so my doctor recommended trying to fertilize all seven eggs.
We had to wait a few days to find out how many of those eggs were fertilized and how many of those fertilized eggs turned into big enough embryos for us to freeze. We ended up being able to freeze five embryos, which is pretty good when you consider that we fertilized only seven eggs to get five good-quality embryos. That was a success.
Truthfully, I was so happy with how the experience went. Knowing that I had five embryos in storage was a big motivator for me and gave me a lot of hope that even beyond surviving cancer, I would still be able to have a family. I was thankful to be able to have that possibility.

If your fertility doctor can talk to your oncologist and make a plan, there can be workarounds that would allow you to do it.

Everybody’s scenario is different, but if it’s important to you, definitely explore every resource and avenue that you can to do it. It’s not easy, but it’s not too difficult if you want it and if it’s really important to you.
I’m a huge proponent of doing everything you can, advocating for yourself, and asking how you can get fertility preservation done. If your fertility doctor can talk to your oncologist and make a plan, there can be workarounds that would allow you to do it.
I had to be on blood thinners during the whole process. I gave myself blood thinner shots every morning while going through fertility preservation. My doctor was afraid that I would develop blood clots, especially considering the hormones. There were risks, but there are also ways to mitigate those risks and work around them. Advocate for fertility preservation, if it’s important to you.
Treatment
Discussing the Treatment Plan
Everything was moving pretty fast. I celebrated my birthday in the hospital. I was diagnosed on September 29th and turned 29 on October 1st, which was a very surreal experience to celebrate my birthday in the hospital during this time.
My doctor was very communicative about my treatment options, even though we were still confirming what type of lymphoma I had and what the staging was. He went through the options of either doing R-EPOCH chemotherapy or R-CHOP chemotherapy, both of which are similar to each other.
R-EPOCH is what he was leaning towards. He explained that R-EPOCH was going to be done inpatient at the hospital for five days. I would get chemo for five days, wait for three weeks, go back for the next round, and do that cycle for six rounds. R-CHOP would be outpatient.
After receiving my diagnosis, he said that I was going to do six rounds of R-EPOCH chemotherapy, which equated to about six months of treatment. I would be in the hospital receiving chemotherapy, come in to see him a few days later, and then two weeks after that, be back in the hospital for my next round of chemo.

The anticipation of side effects was worse than any side effects that I felt. I had a lot of anxiety about what I would feel and what I would be going through.

Side Effects of Chemotherapy
My oncologist explained what I could expect from the chemo, the first one being hair loss. He noted that I would be fatigued and that I could be nauseous. He was very good. He wrote down everything for me. He also drew pictures of where the lymphoma was. It was very helpful in those moments for him to write everything down for me.
He explained to me that I should expect to feel pretty crappy the week after chemotherapy and have a good week during that second-week break before I would be in for my next round.
The anticipation of side effects was worse than any side effects that I felt. I had a lot of anxiety about what I would feel and what I would be going through, but none of my worst nightmares came true except one.
The side effects were quite manageable. The hair loss was something I knew was a given upon diagnosis, so I tried my best to not focus on it. I didn’t want to give the thought of losing my hair power. What I was most concerned about was losing my eyebrows, which was tough.
After the first round of chemotherapy, I started to lose my hair, which was traumatic — I don’t think there’s any way that it can’t be. I cut my hair short before starting chemotherapy with the hope that it wouldn’t be as apparent when it did fall out, but it fell out in clumps in the shower. It was constant. I woke up with hair on my pillow. It was very hard to go through that process.
Once I was able to shave my head, it felt so much better because then I wasn’t constantly dealing with hair falling out in clumps. I bought a lot of head wraps and wore a lot of beanies. I was going through treatment during the winter time mainly, so I was able to do that. I tried to not give it so much power and kept telling myself that it would come back.

The side effects compounded as I got more and more chemo. As I went through the rounds, the side effects got a little tougher.

I struggled with fatigue and some nausea. The nausea wasn’t overwhelming and I was able to take ondansetron (Zofran) to handle it, but it was mainly overwhelming fatigue and an overall feeling of malaise. I would explain to my friends that it was like a bad hangover, a feeling of not having any energy and can’t get out of bed.
I stayed with my parents because they lived close to the hospital. There were days when I only stayed on one floor because I was afraid that if I went down the stairs, I wouldn’t have the strength to come back up or I would lose my balance.
There was always a general feeling of unwellness between cycles. My body would rebound in the last week and I would start to feel a little bit better and have a little bit more energy.
The side effects compounded as I got more and more chemo. As I went through the rounds, the side effects got a little tougher. Overall, I considered myself pretty lucky in the way that my body was able to handle all of the chemotherapy.
I had to deal with one bout of COVID during my second cycle of chemo, which was awful. My symptoms weren’t awful, but getting COVID set off a bunch of logistical headaches with my chemotherapy that were tough to deal with and manage. I had to advocate hard for myself. That was a tough roadblock, but we got through it.
Post-Treatment Scans
I finished treatment in February 2023. We were feeling very confident about how things were and how the treatment went. I had a good midway scan. They saw that the mass in my chest was shrinking a lot. Everything was moving back into place, as my doctor said. Things were clearing up so it was a good sign that the chemotherapy was working, which was great.
When I received the news that there was still residual disease, that was truly crushing not only for me but for my family and my fiancé who were on their own journeys considering my cancer diagnosis.
Residual Disease
I had to wait a month after I finished my last day of chemotherapy to have my last PET scan where two spots lit up. That was tough because we weren’t expecting it. There’s a 50% chance there could be inflammation and a 50% chance that it could be residual disease.
We had to do another biopsy, which was a little bit more invasive. They put me under for that one because they needed to get samples to see if it was residual disease, which it was.
Truthfully, those weeks were the toughest. After my diagnosis, I was able to tell myself that it was just six months of my life. I was going to be able to get through this and then everything’s going to go back to normal. I was going to get my life back. That’s what got me through the six rounds of intense chemotherapy, saying that it was only six months and that I could do this.
Since I had residual disease, I was going to be on this ride for a lot longer and I didn’t know what to expect. My doctors were very encouraging. Considering that I was so young, didn’t have a prior history, could handle the chemotherapy, and that it would probably work, I had a good chance of being cured.
We were holding on to that hope, but when I received the news that there was still residual disease, that was truly crushing not only for me but for my family and my fiancé who were on their own journeys considering my cancer diagnosis. It was heartbreaking news for all of us. There were definitely a lot of tears.
My team very quickly referred me to a larger cancer hospital and connected me with the CAR T team there. They had already gotten the ball rolling for me to do CAR T-cell therapy.

There were a lot of questions about whether or not I needed CAR T-cell therapy or additional radiation to clear up the small spots that were left over. There was a lot of back and forth.
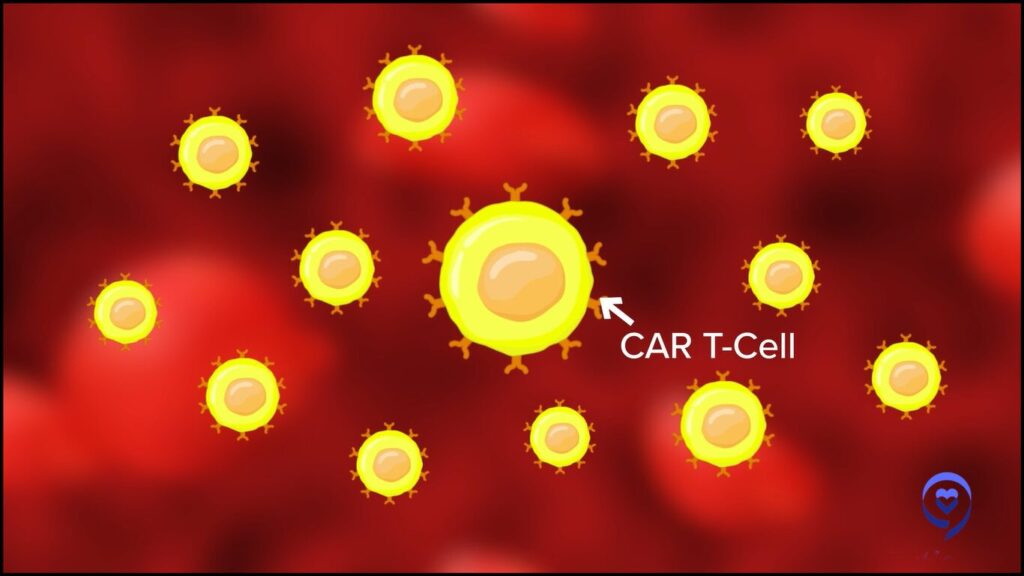
CAR T-cell Therapy
I knew about CAR T-cell therapy because I read stories on The Patient Story about other patients who had lymphoma and have gone through CAR T-cell therapy. I understood the basics and what patients can expect to go through. My family had a lot of learning to do. But again, I was still living moment to moment, day by day. What were the next steps? Who do I need to talk to about CAR T-cell therapy?
While I knew about it, it was still very scary to me. Mentally, I was at a point where I didn’t want more treatment, but, at the same time, I knew that I had to steel myself for additional treatment.
Once I met with my CAR T-cell therapy team, I felt like I was in very good hands. There were a lot of questions about whether or not I needed CAR T-cell therapy or additional radiation to clear up the small spots that were left over. There was a lot of back and forth.
My case was presented to a lymphoma tumor board where multiple doctors weighed in. I also got second and third opinions on CAR T-cell therapy from other oncologists. After speaking to the other doctors, I felt very confident in moving forward with CAR T-cell therapy because there was a consensus that it was the next step for me, with some radiation in between.
Once I knew that CAR T-cell therapy was the best next step, I mentally was ready for it. You don’t have a choice, so you have to be ready. I felt very confident going into it.
All’s well that ends well. I was focused on the mission and the mission was to get my T cells and send them out.
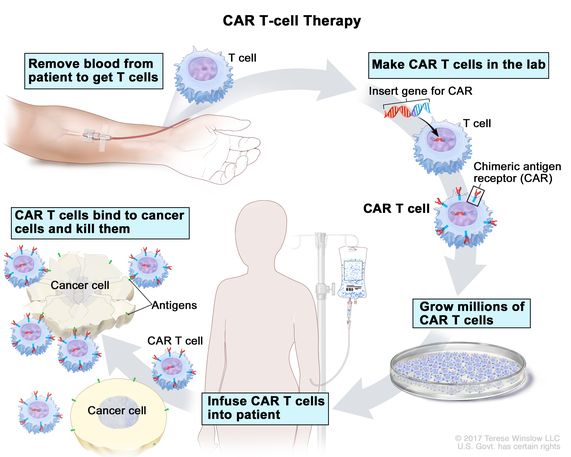
Process of CAR T-cell Therapy
My team went over in detail what the process entailed, so that made me feel a lot better because I was prepared for what to expect. They gave me resources and booklets. They connected me with a resource that will help sponsor hotel stays close to the hospital because you have to stay close to the hospital when you receive CAR T-cell therapy.
There was a little bit of a wait of a few weeks to a month between the first meeting with my team and cell collection day.
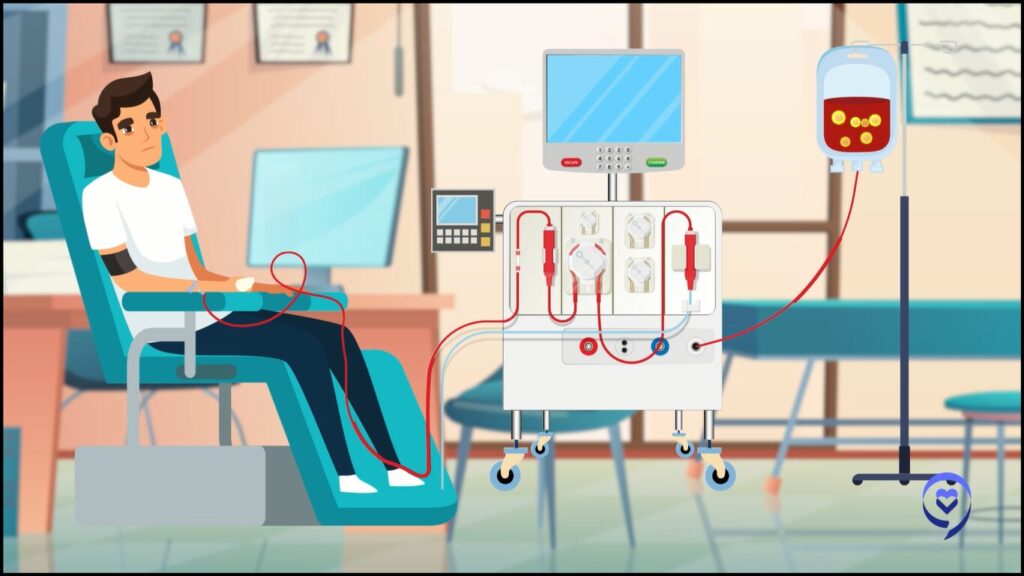
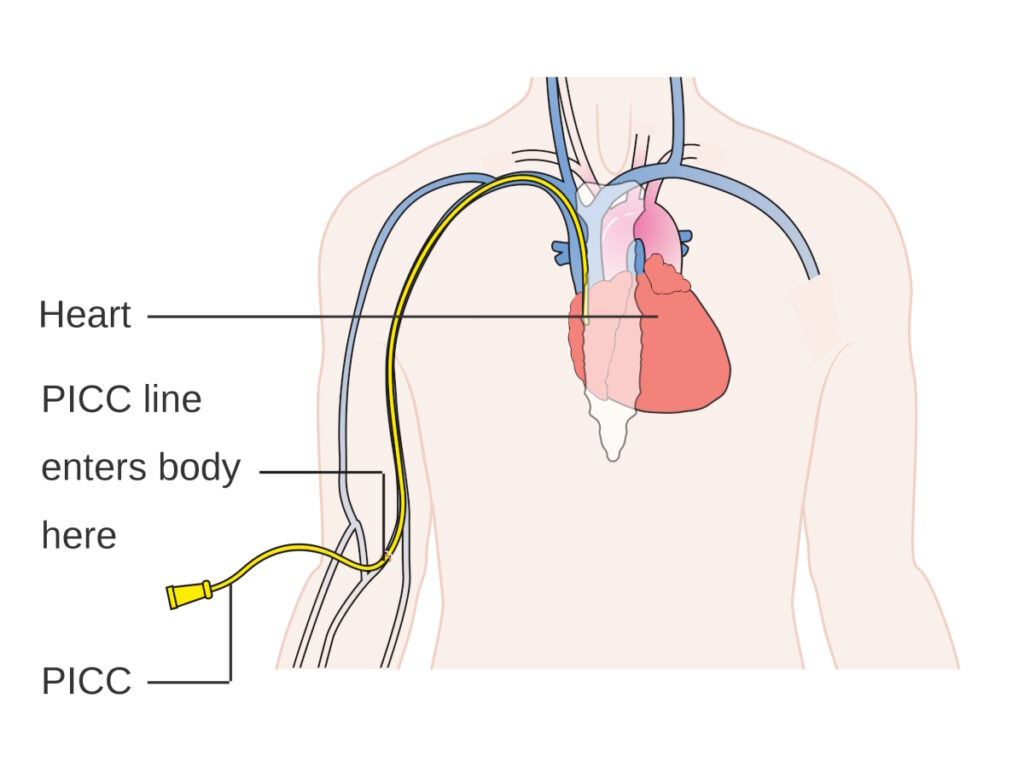
The first step is collecting the T cells. They do that by putting your blood through a machine that separates your T cells, which are then sent to the manufacturer of the CAR T that you’re going to be receiving. I received liso-cel (Breyanzi).
If you have good veins, they can do it through the peripheral veins in your arms. I have small veins that are very hard to access, which is why I have needle phobia. They had to put a catheter in my neck. It’s not comfortable. However, I was given lorazepam and I told myself that I could get through this. They put the catheter in my neck specifically for T-cell collection and then immediately after, they would take it out.
We hit our first stumbling block. My neck catheter wasn’t working so they had to stick my veins. Luckily, I had a good team of people who were able to find a vein and complete the T-cell collection.
The T-cell collection day is pretty long. You’re sitting in a chair and can’t move because you’re connected to the machine. My advice is to bring snacks, your tablet or laptop, and be prepared to watch a lot of Netflix. I was living day to day, so I knew I could get through it.
I didn’t experience any side effects after the T-cell collection other than being a little bit tired. During the collection, you might feel that your body or lips are tingling, which has something to do with the calcium level in your body, so they will give you some calcium to help supplement but it’s not uncomfortable or painful. It’s just a weird feeling.
It was a little bit crazy for me but, again, through the journey and the experience, I told myself I could get through this. All’s well that ends well. I was focused on the mission and the mission was to get my T cells and send them out.

[I had] to get special permission from the drug manufacturer to use my T cells, which put my CAR T-cell therapy in jeopardy of being pushed back.

CAR T-cell Infusion
CAR T-cell infusion day came. Unfortunately, there were some delays in the schedule, which was very stressful. The drug manufacturer has to test your T cells. My T cells were considered too robust or too healthy and were labeled as out of range so that required me to get special permission from the drug manufacturer to use my T cells, which put my CAR T-cell infusion in jeopardy of being pushed back.
They were able to have a meeting and they approved for me to use my T cells. But then they were mislabeled so during the shipping process, they had to be sent back and then re-shipped, which was very stressful because my CAR T-cell infusion date was pushed back. I was very worried because this was happening in May. I wanted to at least have a summer and go to the beach so I wanted my CAR T-cell treatment over and done with as soon as possible.
Mentally, I was prepared for the process, but I didn’t prepare myself for the potential setbacks. While that was very stressful at the moment and I advocated a lot for myself to make sure that everything was going to turn out okay, I eventually ended up getting my CAR T-cell infusion done at the beginning of June.
You first receive three days of lymphodepleting chemotherapy, which is a low-dose chemotherapy done in the hospital as an outpatient. I was able to go back to the hotel that I was staying at nearby.
After three days of chemo, they gave me two days to rest before the infusion. I felt crappy after. It made me much more nauseous. I did not feel good. At points, I thought I could faint or lose consciousness. I felt pretty crappy during those two days that I wasn’t receiving anything. They do their best to give you what you need, such as anti-nausea drugs.

When they were pushing the CAR T cells in, I felt a garlicky or cream corn taste in my mouth, which is something that happens.
By the time infusion day came around, I was feeling much better. I went to the infusion center and the CAR T cells were brought in a little cooler. It wasn’t an infusion bag that they held. It was a syringe.
I had a PICC line where they would give me chemo through so they pushed the CAR T cells through my PICC line for about five minutes. They monitor you very closely in terms of your vitals. Beforehand, they pre-medicate you with diphenhydramine (Benadryl) to prevent any allergic reaction.
When they were pushing the CAR T cells in, I felt a garlicky or cream corn taste in my mouth, which is something that happens. It was fine though. I didn’t mind or anything.
Overall, the CAR T-cell infusion was not a big deal. They monitor you for the rest of the day. The infusion itself took less than 30 minutes. They monitored me for a few hours and upon discharge, I went back to the nearby hotel that I was staying at.
You have to come back to the hospital every day for regular blood work. They’ll ask you a bunch of questions because CAR T-cell therapy has two main side effects: cytokine release syndrome (CRS) and neurotoxicity.
CRS is noted by high fevers and other symptoms. Neurotoxicity is when your handwriting gets messed up, you’re not able to answer questions, your speech is jumbled, etc., so they were testing me for those things.

While it certainly wasn’t easy, I wouldn’t say that anything that happened was unexpected. They prepared us for the side effects that I could experience.

Side Effects of CAR T-cell Therapy
When I went into the hospital on day one, I was fine. They did blood work. I looked okay, so I went back to the hotel. I couldn’t be out in public, but we were able to take a walk outside and get fresh air.
That evening, I started to develop a fever, which they expected. I went to the ER and they put me in a room where I spent about five days dealing with high fevers and a general feeling of unwellness. I was weak and tired
My main side effect from the CAR T-cell therapy was on-and-off fever. I received a few doses of tocilizumab, which is what they give to control CRS, and one dose of steroid. The steroid knocked me out. I took the best nap of my life. For four hours, I was finally able to sleep. I was struggling with the fevers so with the help of the medications, I was able to recover.
After five days in the hospital, they were able to discharge me. I went back to the hotel because I still had to be monitored closely before I could be sent home.
While it certainly wasn’t easy, I wouldn’t say that anything that happened was unexpected. They prepared us for the side effects that I could experience. The most anxiety-inducing was waiting, being in the hospital, and not knowing how bad it was going to get.
I remember focusing hard on the tests that they would give me in terms of assessing my mental status because I was really scared that, at any minute, I could be losing it. But they assured me that I would be okay and, luckily, everything was so.

The first thing my fiancé and I did coming from the doctor’s office was go to the beach. It was a wonderful moment and a real first moment of victory where we were able to breathe for the first time in a little bit.

Radiation
After the T-cell collection, I immediately went to radiation, which is a whole other process. They had to do a CT scan of my chest to understand where they had to radiate. They gave me tiny little tattoos that nobody else would notice except me to mark the areas.
During radiation, I was doing breath holds to lift the area that they had to radiate. I needed to lift it away from my lungs and my heart as much as I could so that there was no scatter to my other organs, which is something that they tried to avoid. They want to do their best to radiate just the area that they have to.
The breath holds were tougher than I thought because you have to hold your breath exactly right for them to radiate the exact spots. It felt like a hard yoga class where you have to breathe a certain way and hold your breath. It was tougher than I initially imagined.
I did ten rounds of radiation and ten rounds of radiation with those breath holds made me very tired. Honestly, I wasn’t expecting to be so tired from radiation. Luckily, I didn’t have any other side effects.
Follow-up Protocol
After my CAR T-cell therapy, which was a month total from the time I got my infusion to when I was allowed to go home and started seeing the doctor on a less frequent basis, they determined that I was safe to go home. I took it easy and took things day by day.
I had a PET scan scheduled at the 60-day mark. The results showed that I was 100% in remission. There was no evidence of disease.
The first thing my fiancé and I did coming from the doctor’s office was go to the beach. It was a wonderful moment and a real first moment of victory where we were able to breathe for the first time in a little bit. We were sitting by the ocean, having lunch, and then we saw dolphins jumping. You don’t see that often in New Jersey, so we took it as a good omen for things to come.
It was a turning point and the biggest moment for my mom, honestly, who was my main caregiver during the entire time. She said the last time she was this happy was the day that she gave birth to me, so it was an emotional moment.

I didn’t know who I was anymore. I was still me in many ways, but in other ways, I wasn’t.

Cancer Survivorship
Survivorship is honestly very difficult. In a way, it’s more difficult than going through cancer. Once you’re able to pick your head up, everything else starts to come into focus again. That’s tough sometimes because you finally start to take stock and understand what was lost in a way. For me, a big part of it was my identity.
I didn’t know who I was anymore. I was still me in many ways, but in other ways, I wasn’t. Honestly, I don’t know if I’ve found myself again even at this point, but it’s a continuing journey and I’m still on the ride.
Words of Advice
Honestly, what helped me was taking things day by day, moment by moment, whatever time increment to get through difficult moments. I would tell myself, “I just need to get through these 10 minutes. If I can get through 10 minutes, I can get through 20 minutes. If I can get through 20 minutes, I can get through the next hour.” During those tough times, when I was in pain and wasn’t feeling well, and when I was struggling, that’s what helped me get through.
It’s important to have a good support system. I had a lot of cheerleaders in my corner, mainly my family, my fiancé, and my fiancé’s family. They were there for every step of the way. Being able to lean on those who are there to support you is huge.
If you don’t have people close to you to support you, definitely lean into the resources that are provided to you. There are a lot of cancer centers that provide free social workers for cancer patients. I saw a social worker and she was very helpful. She had a lot of experience and, based on her experience with cancer patients, understood what I was going through. She helped me through some of the tougher moments as well.
Connect with others who are going through the same experience as you. It doesn’t have to happen all at once. It’s certainly a journey. Upon diagnosis, I wasn’t ready to talk to anyone, do anything, or reach out to anyone. But as I went through the process, I became more and more comfortable about reaching out and it was a huge help to me. Don’t be afraid to reach out and ask for help where you need it.

Being able to lean on those who are there to support you is huge. If you don’t have people close to you to support you, definitely lean into the resources that are provided to you.

Inspired by Daniella's story?
Share your story, too!
More PMBCL Stories
Arielle R., Primary Mediastinal (PMBCL)
1st Symptoms: Swollen neck lymph nodes, fever, appetite loss, weight loss, fatigue, night sweats, coughing, itchy skin, trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Keyla S., Primary Mediastinal (PMBCL), Stage 1
1st Symptoms: Bad cough, slight trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Donna S., Primary Mediastinal (PMBCL), Stage 1-2
1st Symptoms: Visible lump in center of throat, itchy legs, trouble swallowing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Patrick M., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Bump pushing up into sternum
Treatment: 6 cycles of DA-EPOCH-R (dose-adjusted) chemotherapy at 100+ hours each
Crystal Z., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Chest pain
Treatment: 6 cycles of R-CHOP chemotherapy
Stephanie C., Primary Mediastinal (PMBCL), Stage 3
1st Symptoms: Visible swelling around the jaw and neck area, major fatigue
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
Mags B., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment:(1st Line) R-CHOP chemotherapy, 6 cycles
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatment: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
CAR T-Cell Stories
William Y., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Extreme fatigue, achey hands
Treatment: Chemotherapy, CAR T-Cell therapy
...
Jacqueline Barrientos, MD
Role: Hematologist, researcher
Focus: Chronic lymphocytic leukemia (CLL), lymphoma, 17p Deletion (Ibrutinib, Acalabrutinib, Venetoclax), IgHV mutation
Provider: Northwell Health (NYC)
...
Tim Fenske, MD, MS
Role: Hematologist-Oncologist
Focus: chronic lymphocytic leukemia (CLL) & leukemia and lymphoma | CAR T, targeted therapy
Provider: Medical College of Wisconsin
...
Shahzad B., Refractory Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Extreme fatigue
Treatment: R&B, R-ICE, R-EPOCH, CAR T-cell therapy (cell-based gene therapy)
FDA approved: October 2017
...
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
...
Robyn S., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL), Stage 2E
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: R-CHOP, R-ICE, intrathecal, BEAM; autologous stem cell transplant, head and neck radiation, CAR T-cell therapy
...
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...
Theresa T.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: IgG kappa Light Chain
Initial Symptom: Extreme pain in right hip
Treatment: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
...
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
...