Patrick’s Stage 2 PMBCL Non-Hodgkin’s Lymphoma Story
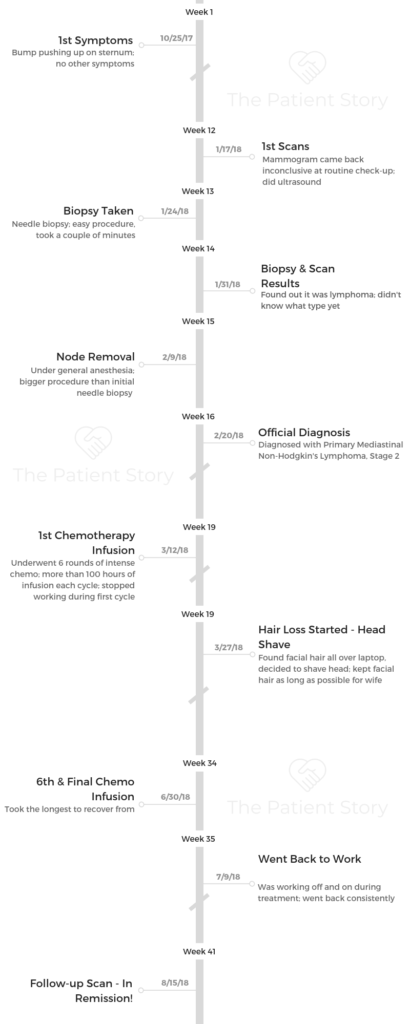
Patrick was diagnosed with stage 2 primary mediastinal B-cell lymphoma (PMBCL), a subtype of non-Hodgkin’s lymphoma.
He shares his story of undergoing hundreds of hours of chemo, advocating for himself as a patient, parenting with cancer and his survivorship journey since remission. Thanks for sharing your story, Patrick!

- Name: Patrick M.
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Primary mediastinal B-cell lymphoma
- Staging: 2
- 1st Symptoms:
- Bump pushing up on sternum
- Treatment:
- Chemotherapy
- 6 cycles of dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (DA-EPOCH-R) at more than 100 hours each
- Total of more than 600 hours of chemo infusion
- Diagnosis
- Treatment
- What do you wish you had known going into treatment?
- Describe the mass doctors found
- What was your experience with chemotherapy?
- What were the chemo side effects?
- How did you handle the hair loss emotionally?
- What was the worst thing you experienced during treatment?
- Were there any surprises throughout your treatment?
- Support & Life Outside Treatment
- Survivorship
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Every day I wake up, and that day is a gift. I have to take advantage of my days and give back to others. I am lucky to have each day.
Having that realization each day you wake up is quite inspiring.
Patrick M.
Diagnosis
What were your first symptoms?
The first symptom was interesting. I had noticed for a couple of months that I had this bump right on my sternum. That was it. It felt like a bone was popping out, but nothing else of concern. I didn’t have any other symptoms. I was going to the gym a couple times a week, and I was living life normally.
When I went for my routine checkup to my doctor, I got a clean bill of health. At the end, I said, “By the way, I have this bump on my chest. I’m not really sure what it is. Can you look at it?” He looked and wanted to get it examined.
We did a mammogram, and that came back inconclusive, so we did a biopsy. They knew that it was a form of lymphoma. They had to remove the actual node, and then they were able to diagnose it as a specific type of lymphoma.
»MORE: Read more patient experiences with first symptoms of lymphoma

What was your biopsy like?
The first one didn’t take very long at all. You just lay down, and they stick this needle in you. The second one where they had to remove the actual node, they knocked me out completely for that.
At that point, they did a trifecta. During the same operation, they knocked me out, they removed the node, they put in a port for chemo, and they removed some bone marrow.
The results from the biopsy took about a week to come back.
How did you react to your diagnosis?
It was a day like any other day. I knew I was getting test results back, but I tried not to worry about it. There wasn’t anything to worry about until there was something to worry about. I didn’t know it was going to be something that was life changing.
The day itself, I remember going to Starbucks in the morning. It was weird. It’s the first time in my life that I was in line and someone ahead of me paid for my drink.
I thought, “Oh that’s really nice.” I didn’t know it at the time, but I needed to be reminded that there’s still good out there.
I went in for the follow-up with my doctor, and I wasn’t expecting anything heavy as far as news went. I had let some family members know that I was going in for this thing they were looking at, but I wasn’t going to worry about it until I had to.
The doctor told me, and I remember not even knowing what lymphoma was. I thought it was a bad cold. I was googling it as he was telling me what lymphoma is. He explained it a little bit more, and I just didn’t get it at all. I remember texting my family and calling my wife and my mom.
I was in complete shock, and so was everyone else. I didn’t know how to react to news like that other than to just try to stay positive. Trying to wrap your mind around what that means and the uncertainty that would follow was a lot to think through. I didn’t know how to react emotionally.
I wound up going back to work for a few hours and tried to keep going. Then I realized I should probably go home and have some time to myself. It was definitely a shock.
»MORE: Reacting to a Cancer Diagnosis
How did you break the news to your loved ones?
With my extended family, it was over a text very quickly. Then I called my mom.
With my direct family – we have 3 kids, who were 2, 5, and 7 years old at the time. We gave it a little bit of time before we talked with the kids. We wanted to wait and get more information and be more stable emotionally before we talked with them.
It was really difficult because we actually had a nephew pass away 6 months earlier from a rare form of brain cancer. He was 2 years old. We were fresh off of that experience, and the kids had that fresh in their minds. We knew we wanted to be careful about how we had that conversation with them. We sought out some help from the hospital to figure out how to talk to them about it.
We did it right. We spent an evening when they got home from school all together. We talked them through what cancer is – the spectrum of it. We explained to them what I had been told that I had.
We didn’t promise them anything. We just said, ‘We have some very good doctors who are going to be working with dad.’
Because we were emotionally calm, they were able to stay pretty calm. Plus, we told them after we talked, we were going to go out to dinner and have some ice cream.
They were fine once it was over. Throughout the entire process, I don’t think one of my kids shed a tear, and that’s okay. I don’t think they fully understood the gravity of what I was going through.
When they’re older and better able to understand the details of it, I’ll explain it to them then. They knew as much as they needed to know. They took it all very well.

Treatment
What do you wish you had known going into treatment?
Your mind is just spinning. You just wish you knew the whole story. You get it in chunks. You’re told what a certain type of treatment is supposed to look like.
My wife is phenomenal. She was on the computer researching the details of a lot of this very quickly.
In the process, you’re just anxious to know what all the treatments are going to be like. The outcomes are just going to be uncertain. To some degree, I just imagined getting on a rollercoaster and getting ready for the ride. I just had to let go of me trying to control everything. I just let the process be.
In the beginning, the rollercoaster was just starting to go up that first hill. I had to let the doctors around me and things around me take care of themselves.
At that point, I wish I would’ve known more information, but you just have to let go.
Describe the mass doctors found
I had a removal of the node, and really what they found was a huge mass pushing up next to my heart. It was pushing forward. That mass of cancer was actually pushing up toward my sternum, so that little node was just the tip of the iceberg. It was part of the huge mass underneath that we needed to address.
It was inoperable because it was so intertwined with everything else. It wasn’t something I was going to be able to have surgery on and remove, so chemotherapy was my option.
What was your experience with chemotherapy?
I didn’t have any radiation or any other type of treatment. It was straight-up chemo, but it was a very intense dose of chemo. I had 6 cycles of dose-adjusted DA-EPOCH-R at more than 100 hours each cycle.
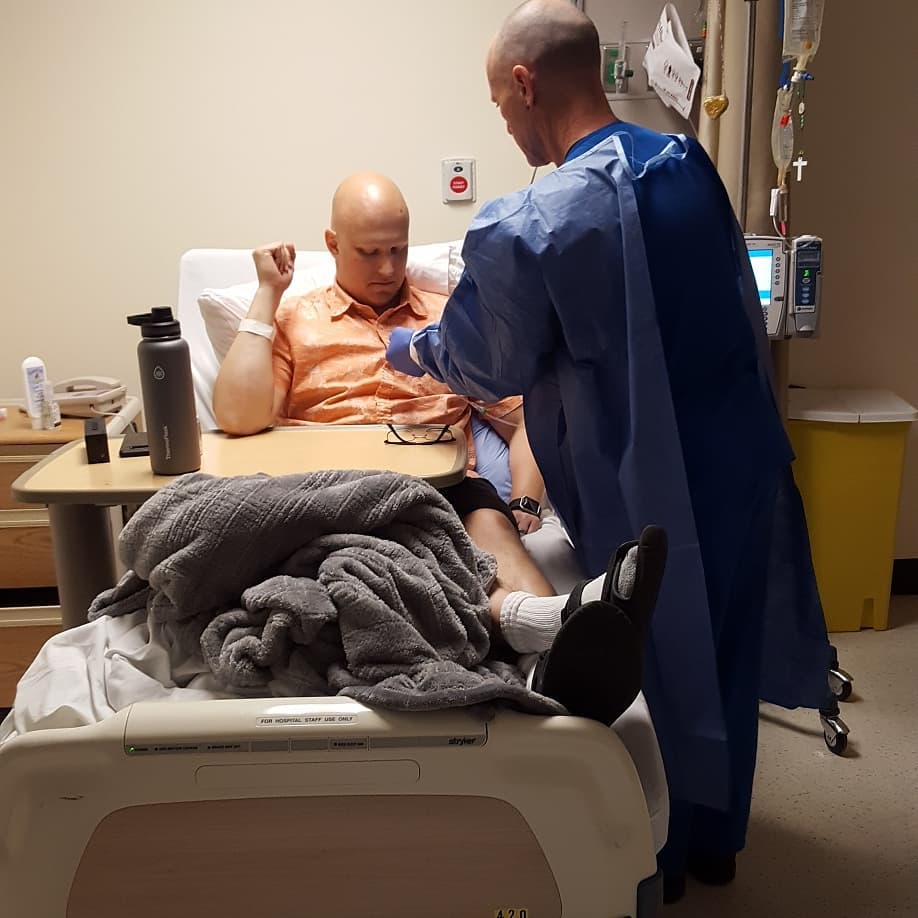
When I went in, I would go in on a Monday, and I would spend about 6 hours in the infusion center getting one type of chemo. When I was done, I would go home. I would come back Tuesday morning, and I would check in for the rest of the week.
I started at 8 a.m. on Tuesday morning. They would plug me in, and I’d get going. I wouldn’t check out until Saturday afternoon. During one of the cycles, I didn’t leave until Sunday.
The entire time I was there, I was hooked up and being infused with chemo. Every cycle, it was more than 100 hours I was being infused with chemo in a hospital room.
What were the chemo side effects?
Hair loss. That’s what everybody goes through, I guess. It’s funny because I’ve always lived my life not having any hair. Ever since I got out of college, I just started shaving my head or keeping it really short because I’d been balding.
When I got diagnosed, I was like, “I’m not going to be denied this opportunity to lose my hair.” With what time I had, I grew some of the stubble out just so I could lose my hair. I lost my hair after the first cycle.
I definitely experienced neuropathy after the first or second round. That stuck around for quite a while. That was more annoying than anything. I’ve always had this sensitivity with my hands where they’ll get too dry, and I need to lotion them up.
With the neuropathy, the numbness was impacting my ability to notice the dryness. Frequently, I would be putting on lotion just because of the sensation that it gave me. I wasn’t able to do some of the fine motor skills I should be able to because of that.
After getting out of treatment every cycle, there were a couple of days where I just was not feeling well at all. Every day progressively got better. It wasn’t while I was there getting the treatment necessarily. The following days were worse.
Hair loss, neuropathy and generally not feeling well were the big ones.
I lost a lot of the color in my face. Nothing too terrible like getting dramatically sick or anything. During my last round, I did come down with a fever at one point, which had us torn deciding if I should go back to the hospital or not.
You’re supposed to go back in if you get sick after treatment just because your immune system is shot. We were wavering on that, but I ultimately ended up not doing that because I got some good sleep, and the fever went away.
»MORE: Cancer patients share their treatment side effects
How did you handle the hair loss emotionally?
I’ve always worn my facial hair a certain way. I was sitting in my office one day thinking about something, and I was scratching my chin. As I looked down, on my laptop there was just a pile of hair. At that point, I realized it had started.
Shortly after, I shaved what little stubble I had on my head because I wasn’t about to make a mess with that. My wife insisted that I had to keep my facial hair as long as I could. That was a slow process, but eventually I lost all of that. I lost my eyebrows. That was weird.
I started to not recognize the person in the mirror. Beyond that, it was a great reflection. The person in the mirror isn’t just the person you see – it’s the person inside.
Really, when I looked at myself in the mirror and I was pale with no hair at all, I only recognized myself by my eyes to a certain degree.
It was a great reminder that I was more than my looks. I still saw the person I am inside when I looked in the mirror, but it was certainly not the person I was used to seeing on the outside.
»MORE: Dealing with hair loss during cancer treatment
What was the worst thing you experienced during treatment?
The worst thing I experienced would probably be the time I missed with my family. I knew that everyone was rallying around me and supporting me any way the could.
For my kids, things still took place. My son still played baseball, and they still had school. Life went on for them.
It was difficult to be missing out on that. I remember the first time that my kids came to visit during my first round of treatment.
I had been in the hospital for a few days, so I hadn’t seen them. Everyone else had been by to visit, but when they came, I lost it. I couldn’t believe how much I missed them.

I had to leave the room because I was losing it emotionally. It had only been a couple of days, and previously, I’d been traveling a lot and would be gone for days, so logistically it didn’t seem like a big deal since I was just at the hospital down the street.
For some reason though, that had a huge impact on me emotionally – not getting to be part of their regular life.
I really missed the normalcy of family life. That was the biggest challenge. I know everybody’s journey is different, but for me, the emotional part was much more difficult than the physical.
I’m not saying the physical parts of it were easy, but the emotional aspect took its toll on me.
Were there any surprises throughout your treatment?
When you’re a kid growing up, you never imagine that one day you’re going to get cancer and imagine what that will look like. It’s hard to say what was a surprise and what wasn’t.
I was extremely blown away by the amount of support people were showing me. People I worked with, people I hadn’t talked to in 10 or 15 years, my family – everyone was reaching out to me.
I’m the youngest of 4 boys, and then I have a younger sister. Everybody wanted to help. My mom pretty much moved in with us for 5 months. She dropped everything and came up to support. As much time as I spent in the hospital, I didn’t have that much time where I was alone. I had a constant rotation of people with me.
Before treatment, you’re thinking, “Man, I can watch a ton of movies because I’ll have all this time.” Leading up to treatment, I had the intention of writing a book, so I thought I’d have all this time alone in a hospital room to write.
It was actually not like that at all. There wasn’t a whole lot of time where I was by myself. When I was, I was pretty much sleeping.
I was blown away by the amount of support and the number of cheerleaders I had near and far. That was the biggest surprise of all.

Support & Life Outside Treatment
Did you work through treatment?
As I was able, I went back to work. When I went in for treatment, I would go in a week at a time for each cycle. Typically, the following week, I would spend several days recovering. The third week, I would always go back to work.
I work in education, and that’s tough because kids are germy. Schools are germy, and I needed to not be in schools. Luckily, I have an office that’s not located in a school, so when I went back to work, I would be at work but not necessarily in schools.
My employer was awesome in being understanding. I contributed how I was able. I actually did a couple of conference calls when I was sitting in the hospital with the chemo being infused. I tried to stay as involved as I could, and that was a good distraction.
I have the luxury of being in an occupation where I get to give back and help other people, and it helped me in the process to still be engaged in that.
Instead of thinking about how difficult my situation was, it helped me to still mentally be engaged in what was going on at work. I still had the opportunity to give back in some capacity.
»MORE: Working during cancer treatment
Is there anything that might have helped you handle the financial process?
In the beginning, it was one of the stressors because we didn’t know how it was going to affect our family. I guess I wish I would’ve known that that part was going to be okay.
Looking back, the most important thing was my health. In the grand scope of things, the financial stress was unnecessary. The most important thing is figuring out how to take care of your health. I wish the finances hadn’t been a concern in the beginning.
What helped you through times of great stress?
Knowing that anyone was a phone call away was helpful. The number of people that were there with me was incredible. The staff at the hospital were phenomenal as well. They were the nicest people you’ll ever meet. They kept me busy.
You’re in there for a long period of time, but they’re coming in every half hour taking my blood pressure, checking in, asking about my appetite and all that, so they helped a lot with breaking up my time in the hospital. I was surrounded by so many supportive people who were beyond giving.
Were there moments you had to advocate for yourself?
My wife did a really great job of advocating for me. One of the biggest pains was the insurance company. My wife went to bat for me.
One of the things I had to do after each round of treatment was to have a specific shot every day for about 8 or 9 days. That meant I’d have to go back to the hospital after being there for a week. I’d have to go back literally every day just to get a shot. When you’re not feeling well, that’s not really what you want to be doing.
There was a separate shot that I could get that would only have to be once instead of going in every single day. It was the insurance company that was saying no because it was cheaper to go in every day.
It was frustrating that the insurance company was dictating part of the treatment. My wife went to bat and said, ‘No, he shouldn’t be going back to the hospital every day when he’s feeling terrible.’
Ultimately, the insurance company won. My wife was awesome, though, and figured out how to administer the shot herself. She would pick it up from the pharmacy, and every night she was my nurse and would give me the shot. It wasn’t my favorite part, and I’m sure it wasn’t hers either, but she was a great support.

Raising kids while going through cancer treatment
I was honest and open with them about it, but we handled it in such a way that let them know we didn’t want them to worry about it.
We made sure that life went on.
They still went to school every day. We got them into before and after care. On the weekends, if I wasn’t feeling well, my mom would take them out and keep them busy.
My son was going through his first holy communion prep while I was going through treatment. Toward the end of my treatment, he had his first holy communion. That whole process continued.
We just made sure that their lives weren’t interrupted and that they had the opportunity to spend time with me.
One tradition we’ve had for years is pizza movie night on Friday nights. When I was in the hospital, we still did it. My wife would get the kids, they’d go pick up a pizza, come to the hospital, and we’d sit in my room and watch a movie on my laptop.
As much as possible, we made sure their lives were as normal as they could be. They still had a lot of things to look forward to.
»MORE: Parenting with cancer
Survivorship
How did your cancer affect your relationship with your wife?
It brought us together in many ways. When you have 3 kids, you rarely have any time to yourself. You rarely have any time to do anything or talk about anything. When she’d come see me in the hospital for these extended lengths of time, we’d do a mad libs book or random stuff like that.
We just had more time together than we previously did. That part was nice. I always knew that I married the right person. I knew I had married a phenomenal person.
Nancy Reagan once said, ‘A woman is like a tea bag. Only when things get hot do you realize how strong she is.’
I would say that’s true for my wife. She was absolutely incredible during the entire process.
Both of us had times where we found ourselves in an emotional state, but she took on so many different roles throughout the process.
She supported me and made sure the rest of the world kept going. She had to continue orchestrating our kids’ lives and schedules, and she still had a full-time job to tend to. She is just an amazing person. I wish cancer on no one, but some of the joys I’ve gotten from it, I wish for everybody.
The way in which it brought my wife and I closer together was amazing. It was a stress, and it was difficult, but we got through it together. I couldn’t have done it without her. Her support was nothing short of amazing.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

Describe your “new normal” following cancer
I finished my sixth round. It had the biggest impact and was the hardest to recover from.
After the fact, it took a while for my hair to grow back, but other than that, I went back to work pretty quick and got back into some of my old routines.
My new normal is a little paranoid any time I have an ache or pain or something come up, because I worry that it’s cancer. I’m a little more paranoid than I used to be. Going through the process, my wife and I were trying to figure out anything that could’ve potentially caused the cancer.
Was it the weed killer we used on the yard? Was it the type of pans we were using? Now we’re super particular about anything that has any potential cancer-causing agents and are always being watchful of that.
The other side of that is that every day I wake up, and that day is a gift. I have to take advantage of my days and give back to others. I am lucky to have each day. Having that realization each day you wake up is quite inspiring.
Advice for someone going through something similar to what you’ve gone through?
Keep going. Know that your attitude is going to be half the battle. Keep going and stay positive. Believe in yourself. It’s a journey that has its ups and downs, but you just have to keep going.
Sometimes you can’t see the light at the end of the tunnel – you might not even know that there is a light at the end of the tunnel – but you have to keep going and trust in the process.
The entire time, you need to recognize that while you’re going through this, everyone else around you is going through this as well. There are many people that love you and care for you, and they’re concerned.
Many people don’t want to overburden with questions, but they are scared to death for you. I would err on the side of over-communication and share as much as you can. Keep people updated, and as you do, allow them to be your cheerleader.
Many people in this process feel helpless and don’t know what to do. They don’t know what to do, but they want to help. Let them help. If people are offering to help, let them help because to some degree they’re suffering as well.
No, they’re not going through what you’re going through, but they’re very concerned, and they just want to know what they can do.

Inspired by Patrick's story?
Share your story, too!
Primary Mediastinal B-Cell Lymphoma (PMBCL) Stories
Arielle R., Primary Mediastinal (PMBCL)
1st Symptoms: Swollen neck lymph nodes, fever, appetite loss, weight loss, fatigue, night sweats, coughing, itchy skin, trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Keyla S., Primary Mediastinal (PMBCL), Stage 1
1st Symptoms: Bad cough, slight trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Donna S., Primary Mediastinal (PMBCL), Stage 1-2
1st Symptoms: Visible lump in center of throat, itchy legs, trouble swallowing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Patrick M., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Bump pushing up into sternum
Treatment: 6 cycles of DA-EPOCH-R (dose-adjusted) chemotherapy at 100+ hours each
Crystal Z., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Chest pain
Treatment: 6 cycles of R-CHOP chemotherapy
Stephanie C., Primary Mediastinal (PMBCL), Stage 3
1st Symptoms: Visible swelling around the jaw and neck area, major fatigue
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
Mags B., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment:(1st Line) R-CHOP chemotherapy, 6 cycles
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatment: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy










