Theresa’s Relapsed/Refractory Multiple Myeloma Story
Interviewed by: Stephanie Chuang
Edited by: Katrina Villareal

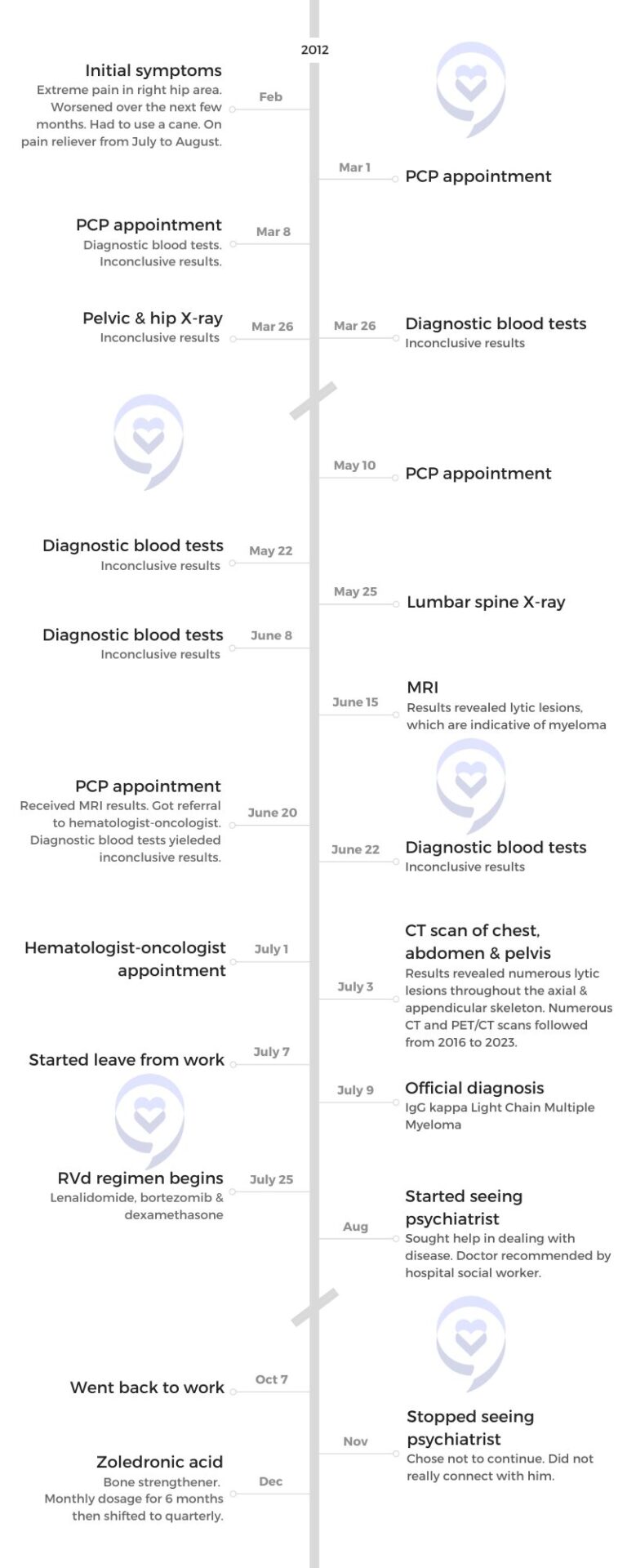
Theresa’s myeloma journey is one marked by resilience, determination, and a profound sense of hope. Her life took an unexpected turn when she began experiencing severe hip pain in 2012. Despite numerous tests and consultations, it took several months to arrive at a diagnosis of IgG kappa light chain multiple myeloma.
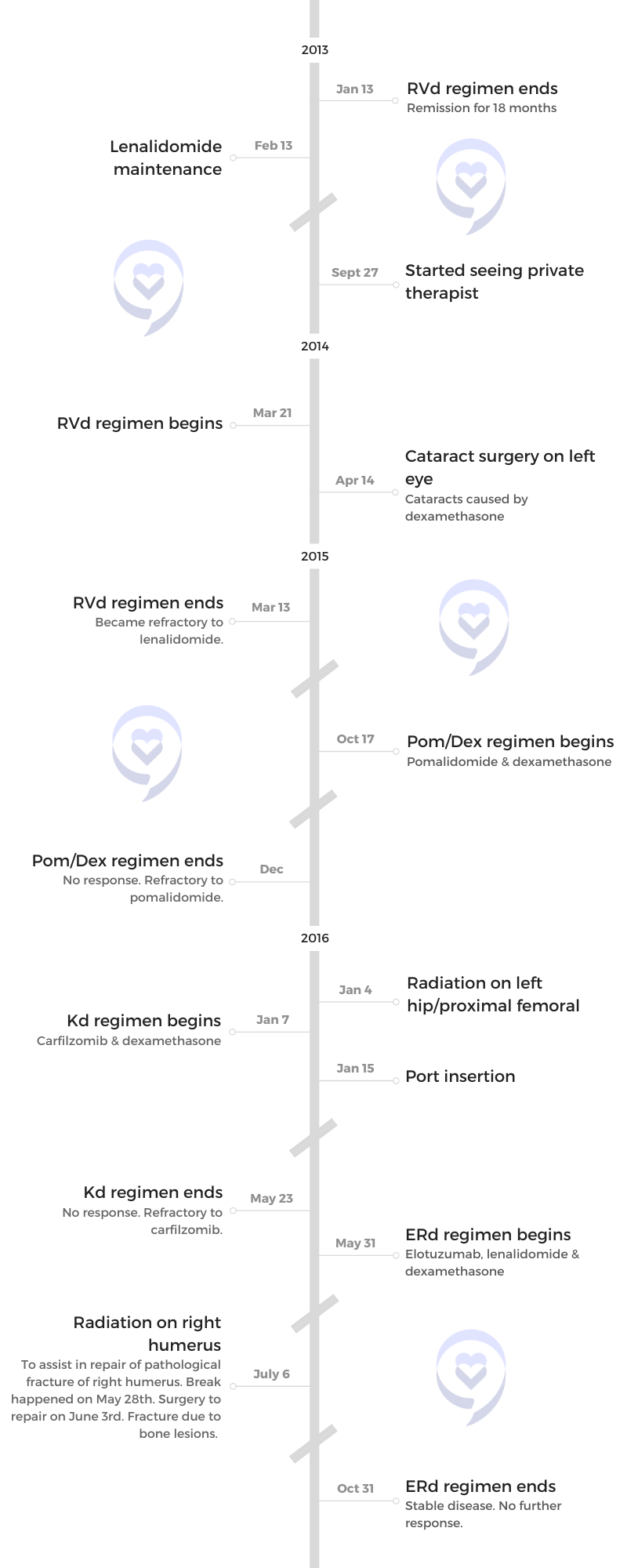
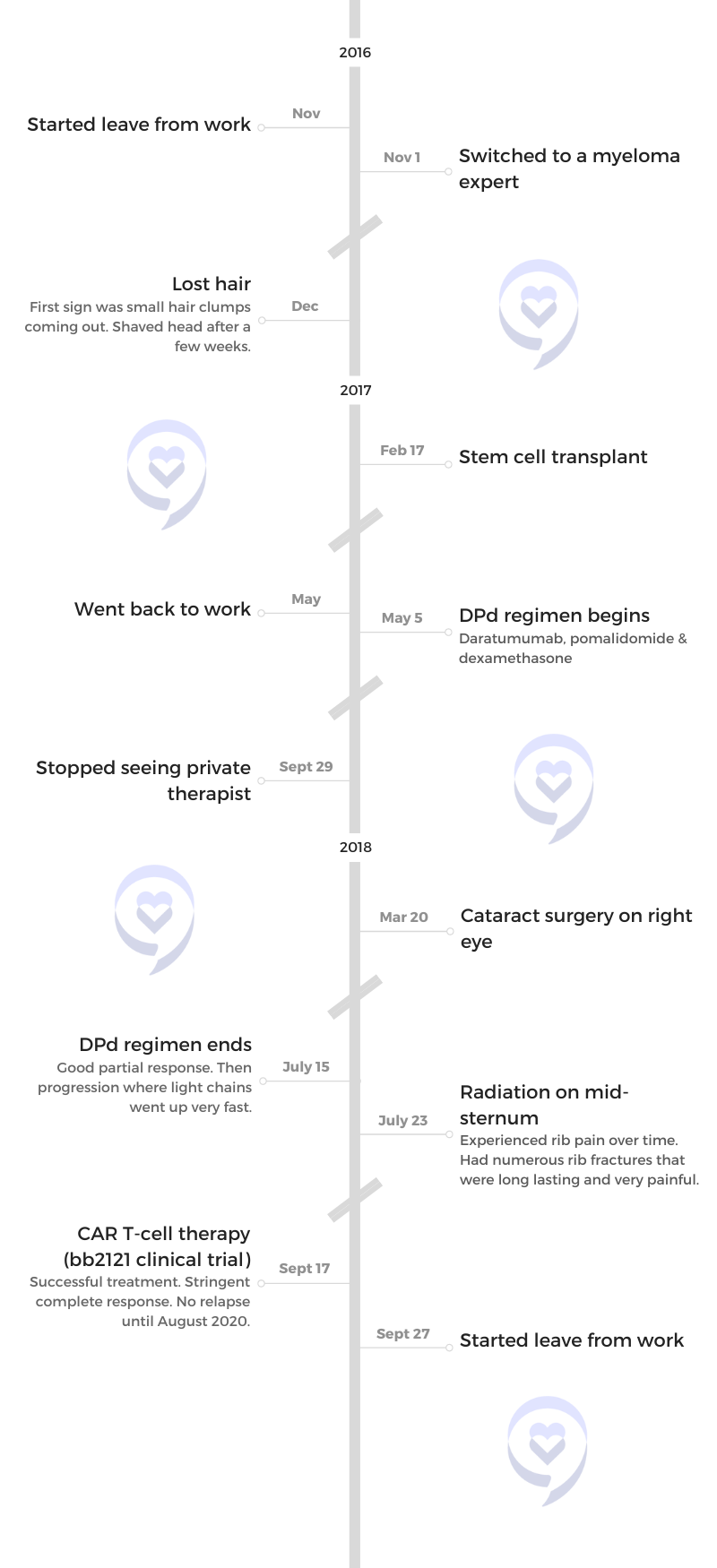
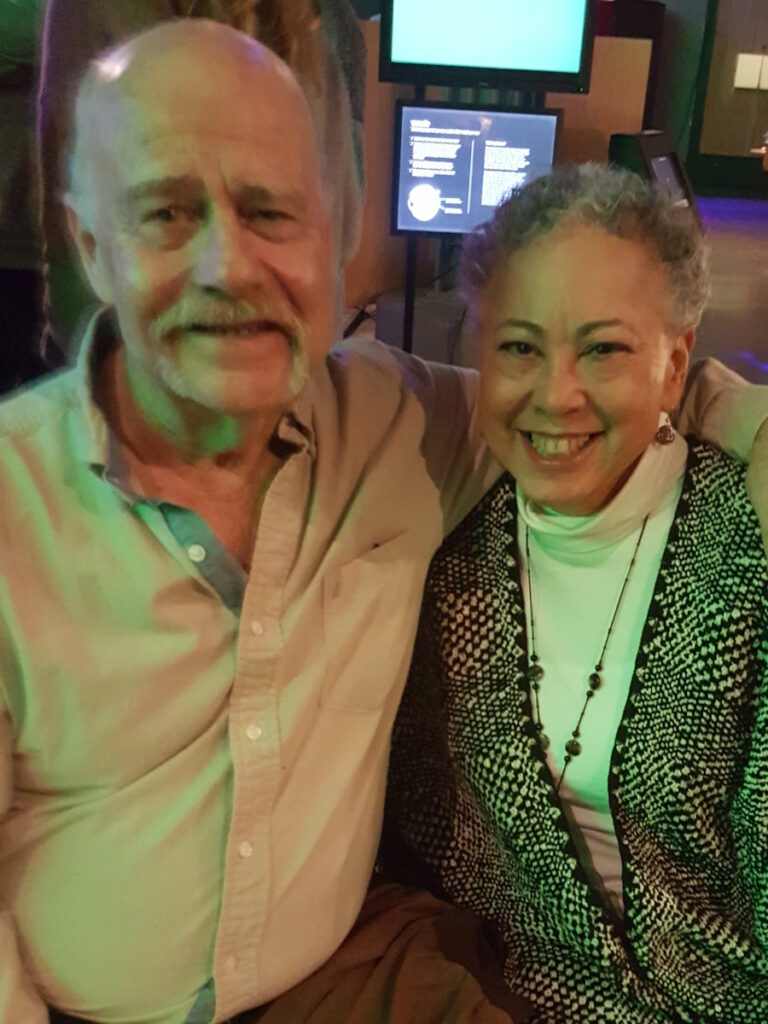
The initial shock of the diagnosis was met with a steely resolve to confront the disease head-on. Supported by her husband Tom and guided by her medical team, Theresa embarked on a treatment journey that included RVd chemotherapy, which initially showed promising results but eventually led to relapse. Undeterred, she enrolled in a clinical trial for CAR T-cell therapy, becoming one of the first recipients of this innovative treatment.
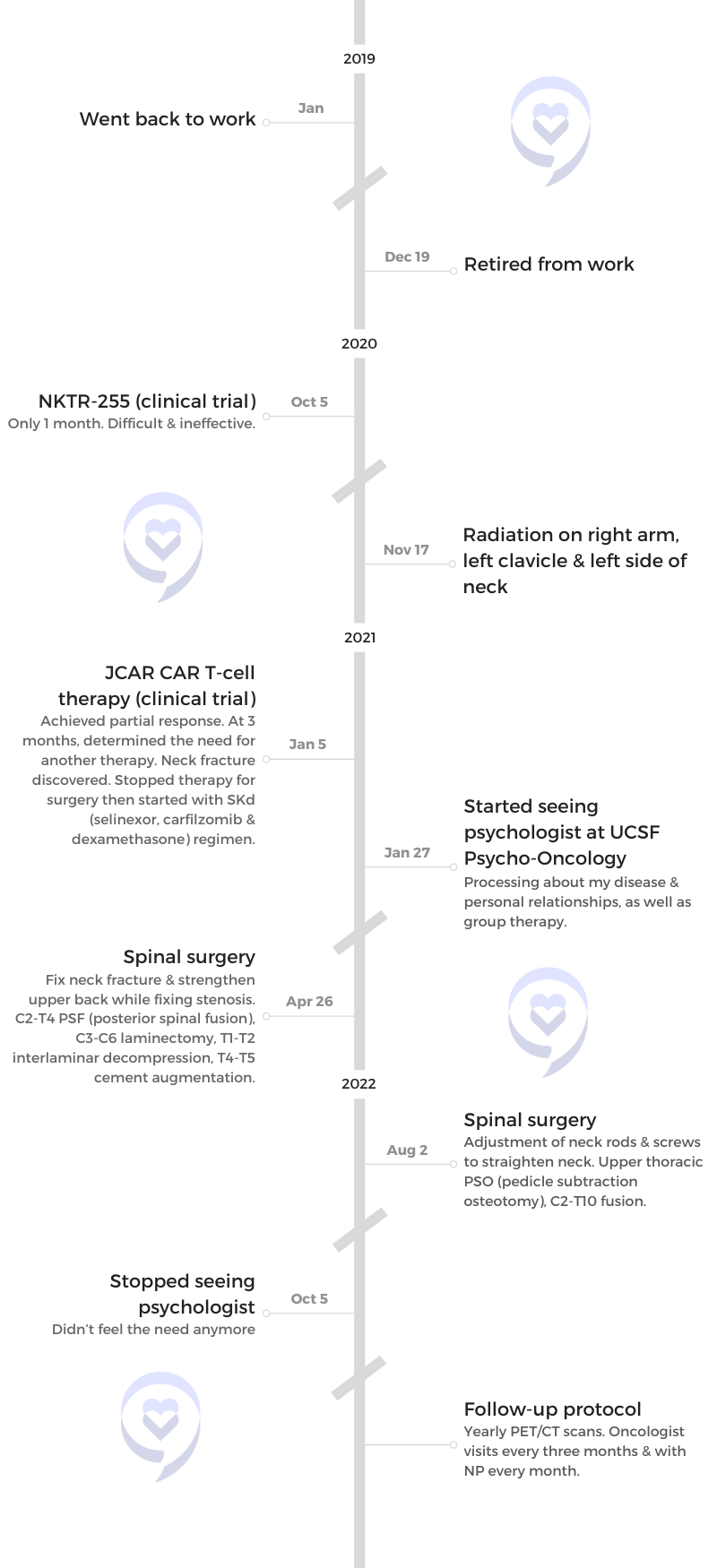
While the CAR T-cell therapy initially induced remission, the cancer eventually recurred, prompting Theresa to explore further treatment options. She participated in another CAR T-cell therapy trial and subsequently underwent treatment with selinexor, carfilzomib, and dexamethasone (XKd), which has been effective in managing the multiple myeloma.
Throughout her journey, Theresa has remained optimistic, actively participating in her treatment decisions, and advocating for herself. Her story is a testament to the power of resilience, hope, and the relentless pursuit of innovative treatments in the face of adversity. As she continues her journey with multiple myeloma, Theresa’s unwavering spirit serves as an inspiration to others facing similar challenges.
In addition to Theresa’s narrative, The Patient Story offers a diverse collection of multiple myeloma stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.

Thank you to Karyopharm Therapeutics for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Theresa T.
- Diagnosis:
- Multiple myeloma, relapsed/refractory
- Subtype:
- IgG kappa Light Chain
- Initial Symptoms:
- Extreme pain in right hip
- Treatment:
- RVd (lenalidomide [“len”]+ bortezomib+ dexamethasone [“dex”])
- Pom/Dex (pomalidomide [“pom’]+ dex)
- Kd (carfilzomib+ dex)
- ERd (elotuzumab+ len+ dex)
- DPd (daratumumab, pom+dex)
- CAR T-cell therapy (bb2121 clinical trial)
- NKTR-255 (clinical trial)
- JCAR CAR T-cell therapy (clinical trial)
- XKd (selinexor+ carfilzomib+dex)
- Zoledronic acid (bone strengthener)
- Radiation
It gives me hope that there are more treatment options out there. There are so many people working at different levels to help folks with myeloma be better-taken care of. They’re looking for a cure, so that’s very exciting. They’re getting closer than they have ever been.
Theresa T.
Introduction
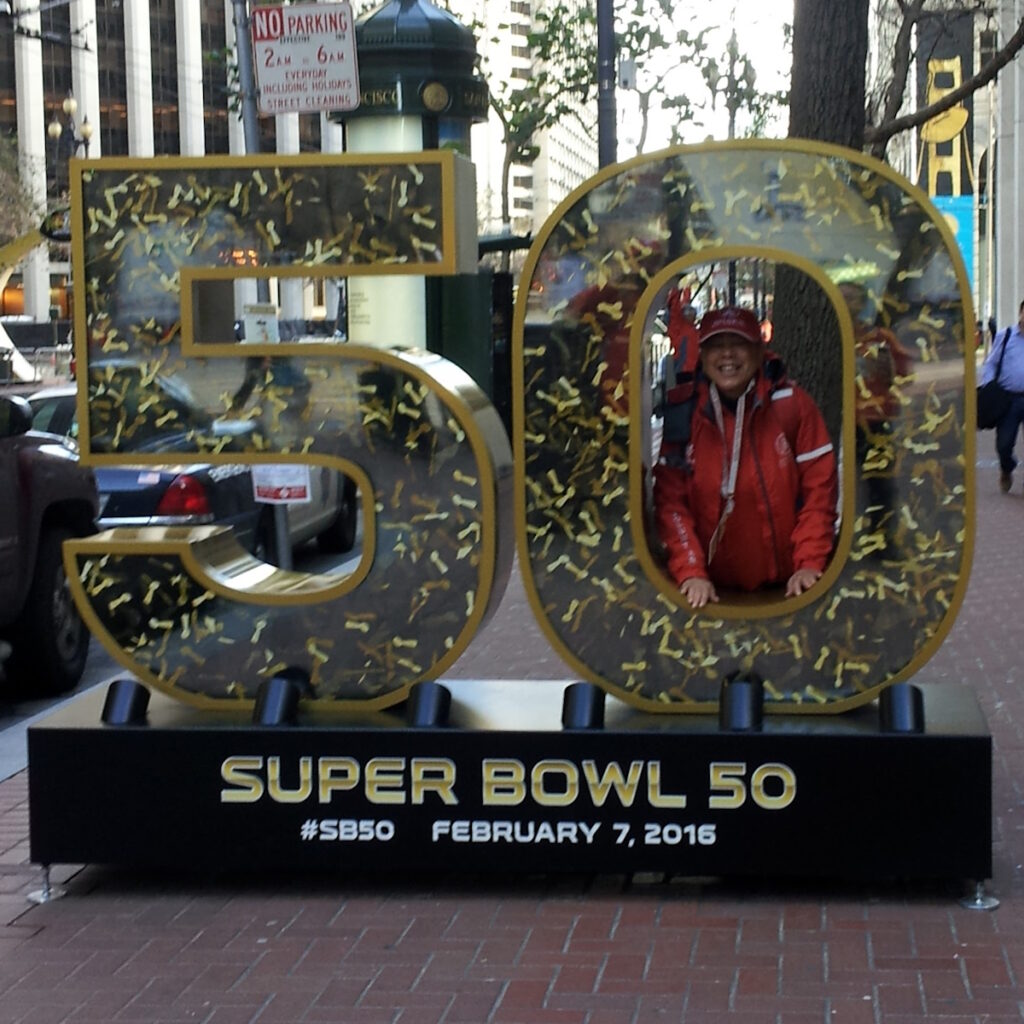
Theresa: I was born in New York City, grew up primarily in Connecticut, and currently live in San Francisco. I went to college in Boston, moved to San Francisco a month after graduating, and I’ve been here ever since.
I had a great career in human resources. I loved that because I love helping and training people. That helped me a lot in my myeloma journey. I’ve been able to talk to other people who have myeloma, help them, and provide information. It’s always good to extend a helping hand to other people. People have done that to me as well, so I want to give back.
I have three brothers and two sisters. It was great growing up with great siblings. We all get along, which is wonderful. I love my brothers and sisters.
I used to be a lot more active. I love to swim. I love to go to the beach. I wish it was a little bit warmer, but it’s close.
I’m full of energy, loving, funny, sometimes smart, and strong, which is interesting. It’s sometimes hard to take that compliment when you go through cancer. People say, “Oh, you’re so strong. I admire you.” Meanwhile, inside, you’re freaking out.
I’ve had people say that to me a lot, so I guess it’s true. I think it comes from being from a long line of strong women in my family. I have good role models. I don’t know any other way to be.


Pre-diagnosis
Initial Symptoms
Theresa: Around February 2012, I started having bad pain in my right hip, which kept getting worse and worse.
I went to my primary care physician who took blood tests and X-rays but didn’t find anything. We kept digging further. We didn’t know what was going on. It was rough, but I kept going. I probably had 6 or 7 different kinds of blood panels to try and figure out what was going on.
For a period of about 3 to 4 months, she went from working out once a week to being unable to walk on level ground without a cane.
Tom
Scans
Theresa: She sent me to an orthopedic surgeon for a spinal X-ray. He’s the one who suggested that I get an MRI, which revealed lytic lesions. Myeloma tends to create lytic lesions. It’s a cancer of the bone marrow, so it eats away at the insides of your bones.
Between mid-February to the end of June is how long it took to get a real diagnosis. In the meantime, my pain kept getting worse and worse. I was using a cane and on pain relievers. It was frustrating to not know what was going on.
Tom: It was unpleasant and worrisome. We didn’t know what it was. For a period of about 3 to 4 months, she went from working out once a week to being unable to walk on level ground without a cane.
Diagnosis
Getting the Official Diagnosis
Theresa: I had an appointment set up at the end of June with my primary care physician. I had seen her several times since February to try to figure out what was going on.
The day before my appointment, I got an email from the doctor’s office referring me to a hematologist-oncologist. I was in denial as to what that meant. It was pretty shocking, but I wanted to wait until I saw my doctor.
They set up an appointment with the hematologist-oncologist for me to talk to. He was a lovely man and was very good. I got one of my first bone marrow biopsies. At the end of June, it was confirmed that I had multiple myeloma.
Tom: He said, “As far as survival is concerned, five years is easy.” My jaw dropped.
It was going to be a big part of her life from here on out, which meant it was also going to be a big part of my life from here on out.
Tom
Reaction to the Diagnosis
Theresa: My myeloma story started when there were a lot of emerging therapies for myeloma. I had always been pretty much healthy and didn’t have anything wrong with me specifically. I led a fairly healthy lifestyle while enjoying life, but I was shocked to get this diagnosis.
Tom: It happened pretty fast. I knew what it meant for her and it was going to be a big part of her life from here on out, which meant it was also going to be a big part of my life from here on out.
Theresa: I left his office better informed. It took me a while to absorb everything. I didn’t completely freak out. I was still in a bit of a denial.

As I talked to them, did more research, and got information about what the treatment was going to be, it slowly seeped in that I had cancer.
Theresa

Discussing the Treatment Plan
Theresa: When they discussed setting up the appointment for the first treatment, I said, “Maybe we’ll wait a few weeks.” He said, “Why are we waiting? We should do this right away.” I didn’t understand the impact of it right away.
As I talked to them, did more research, and got information about what the treatment was going to be, it slowly seeped in that I had cancer. It’s not the worst cancer, but it’s not good because it doesn’t have a cure, so that was a little shocking.
I came back the following week with Tom. The doctor very patiently and thoroughly went through what this disease was, what the treatment protocols were, and what we would do next. The good thing is they’ve developed new therapies.
RVd Chemotherapy
Theresa: The oncologist had a very specific treatment plan. He said, “The initial treatment you get is RVd (lenalidomide, bortezomib, and dexamethasone). This is the standard of care. This is the best that we can do for you.” At that time, there wasn’t a good alternative.
Tom and I talked about it. One thing that I appreciate he always says is, “It’s your body. You have to make the ultimate decision.” Over the years, we’ve talked about different treatment plans, what they’re going to involve, timing, and everything. But in the beginning, the timing was as soon as possible.

Subconsciously, I was doing things often because I couldn’t control this part of my life, so I would try to overcorrect by controlling other parts of my life.
Theresa

Side Effects of RVd Chemotherapy
Theresa: I had a fever. After my second infusion appointment, the fever got worse. They took me to the hospital, which at the time was at CPMC (California Pacific Medical Center). I stayed overnight for observation to make sure I was okay.
When you start a new therapy, your body tends to be shocked and you often have adverse reactions. Luckily, they didn’t continue.
My first reaction was itching. A couple of months later, I had a little rash, but it went away. It was nothing awful.
I had a lot of fatigue. I wasn’t sure if I was going to take time off of work. I took time off for all the appointments, but after that, I took a three-month leave of absence.
After about six months, my numbers went down. I have IgG kappa light chain myeloma. There are different kinds of myeloma. It’s so varied that it’s hard to pinpoint sometimes. I found out that what works for one person may not work for the next person.
I was on and off treatment for a while. That’s my story. It’s been a roller coaster ever since, going up and down, having longer stretches of relapse or shorter stretches of relapse depending on what’s going on.
I’ve gotten upset a lot during these 10 years, especially when I didn’t have control. That’s what affected me more than the why.
I don’t have any control over this disease. I can’t control the effects of the treatment. Even subconsciously, I was doing things often because I couldn’t control this part of my life, so I would try to overcorrect by controlling other parts of my life.
I ask questions and follow orders, so he thought I would be a very good candidate for the CAR T-cell therapy trial.
Theresa
CAR T-cell Therapy Clinical Trial
Theresa: [My disease] became refractory towards my line of treatment. It stopped working. They had a clinical trial available and he thought I was a good candidate. I asked him why he thought that and he said, “You’re in otherwise pretty good shape. You’re doing well. I know you pay attention.” I ask questions and follow orders, so he thought I would be a very good candidate for the CAR T-cell therapy trial.
I was enrolled in the bb2121 trial, which led to the very first FDA-approved CAR T-cell treatment [in myeloma]. I know my number is in there somewhere about my survival with that treatment, so that’s fun.
Clinical trials are a lot. You have to be dedicated. I remember talking to somebody who said, “Why are you doing this trial?” I said, “I want to help other people. Besides, I think it’s going to help me. It sounds really good.” You’ve got to do what you’ve got to do.


Deciding to Participate in a Clinical Trial
Theresa: I had been reading about CAR T-cell therapy and learned they had amazing results. People thought that this might be the cure for myeloma that everybody’s been frantically searching for, so it seemed like a good idea at the time.
There was a lot of paperwork to go through. There were 55 pages of study material that you had to sign your name on about 20-some-odd times, but it’s so worth it.
I trusted my doctor, Dr. Thomas Martin, who is a world-renowned myeloma specialist. I trusted his opinion and read everything.
I had some hesitation because it was still a trial, but the safety and efficacy had been already dealt with. This was a matter of figuring out the dosage, I believe. I felt it was safe and a good idea. I trusted the doctors and trusted what I read.
Within 30 days, I had a complete response. There was no myeloma detected in my system. That lasted for about 18 months.
Theresa
CAR T-cell Therapy Process
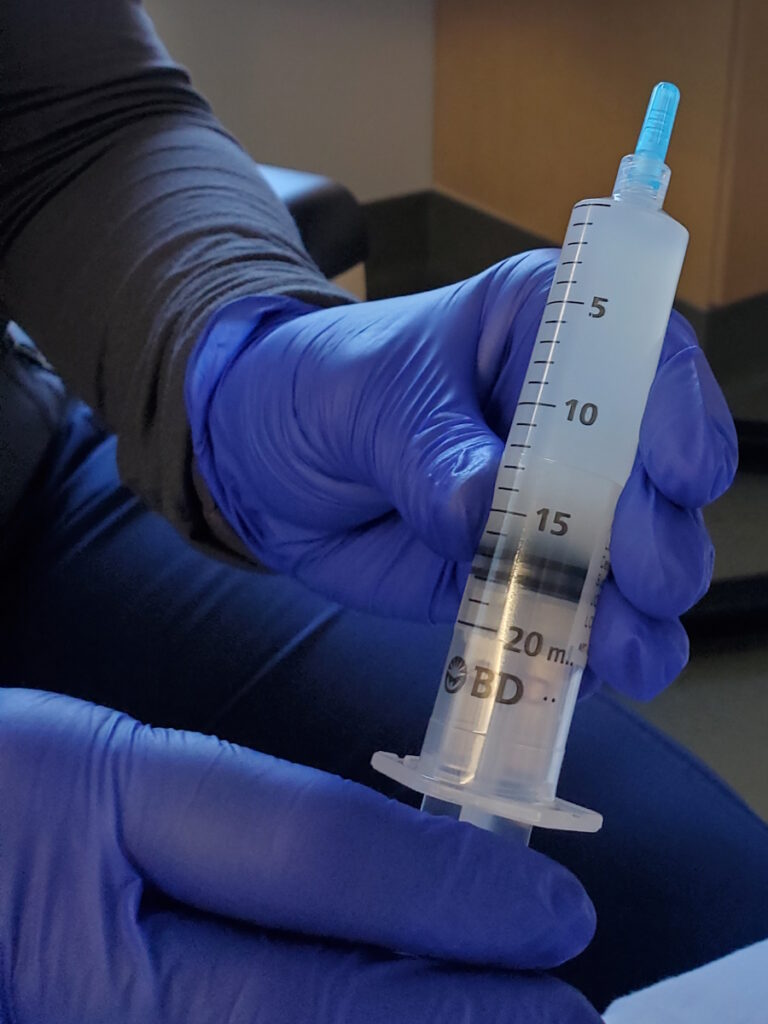
Theresa: First, they take your cells out. They had to send them to New Jersey and then back to California. Before that, there were three days of chemo. To get the CAR T cells, you have to go to the hospital. It’s like a short infusion.
I got them on a Monday and then I had what we like to call Loopy Tuesday. I did have cytokine release syndrome. I don’t remember most of that day at all. I said some strange things when they asked me questions.
After that, they hooked me up. They did so many things to make sure I was okay. I felt okay. They did tests. Doctors came every five minutes. They wouldn’t leave me alone. Everything was fine, except for that 12- to 18-hour stretch. It was otherwise being bored in the hospital.
Luckily, within 30 days, I had a complete response. There was no myeloma detected in my system. That lasted for about 18 months, which is better than the average of about a year or 13 months. I beat the odds, but it came back.

JCAR CAR T-cell Therapy Clinical Trial
Theresa: We talked about options. I didn’t go on treatment right away when I started relapsing. There was another trial that he wanted to try, which had a different target. I tried that, but only for a month. It didn’t do any good and it was hard.
Dr. Martin said, “I’ve got another CAR T trial we could try. It’s got a little bit of a different target, so maybe it’ll work.” I went on the second CAR T-cell therapy clinical trial. I did not have the bad CRS I had with the first one. I was only in remission for three months, so it wasn’t effective. That’s when we decided to go on selinexor.
Know that it could get better. If it’s your first treatment, give your body time. Talk to the doctors and the nurses. Ask them what to expect and what’s normal. Don’t be afraid to ask what’s going on. “What can I expect from this? What can I do to change this? Can I change the dosage? Can I change the timing?”
Selinexor, Carfilzomib, and Dexamethasone (XKd)
Theresa: I’m taking selinexor in combination with carfilzomib and dexamethasone (XKd). In the beginning, it was three weeks straight of carfilzomib infusions and selinexor every other week.
They said it would make me nauseous, so they gave me two anti-nausea drugs while I was getting the carfilzomib. I had two kinds of pills to take at home: one at night for three days and then another to take any other day that I felt nauseated.
It did usually present with some nausea for about three days. I experienced extreme fatigue, although we found out that it was due to the anti-nausea medicine that I was taking at night, so we changed it.
I take three pills in the morning before I get my infusion and on selinexor days. Five or six hours after I get my infusion, I take dexamethasone.
I’m very lucky to have responded to a lot of different treatments. Most of my treatments have been pretty good.
Theresa
Adjusting to New Treatments
Theresa: Know that it could get better. If it’s your first treatment, give your body time. Talk to the doctors and the nurses. Ask them what to expect and what’s normal. Don’t be afraid to ask what’s going on. “What can I expect from this? What can I do to change this? Can I change the dosage? Can I change the timing?”
With dexamethasone, sometimes, it depends on the dosing schedule because it can keep you awake. Work with your body to know the best time to take it and if you can make adjustments. Ask the doctor, “What else can I do?”
This is one mistake that I made in the beginning. I thought if I said something to my doctor, they would address it, but they don’t always do that. If you say something, they’ll listen and write it down, so you have to specifically ask them.
I’ve been on this regimen since September 2021. Again, beating those odds.
One thing I know is that I’m very lucky to have responded to a lot of different treatments. Most of my treatments have been pretty good. Maybe a quarter to a third of them didn’t work, but others have, so I’ve been very lucky to have that percentage work for me.


Future Treatments
Theresa: I don’t think about them specifically. I’ve already discussed what my next treatments would probably be. I have a choice between a bispecific antibody trial or another kind of CAR T-cell therapy clinical trial on a completely different target.
It’s likely that within some amount of time, maybe 3 to 6 months even, I’ll have to go on another treatment. Selinexor has worked for way longer than expected and it’s been well-tolerated.
I have hope. I’ll still be around. I still have stuff to do. I’m not ready to go yet.
Theresa
Words of Advice
Tom: When we got the diagnosis, I said, “Okay, we’re on our way. We got a name. We can pin this sucker down.” We’re getting closer to 10. Median survival rate was 7 ½ years and she’s beaten the hell out of that.
Theresa: I have hope. I’ll still be around. I still have stuff to do. I’m not ready to go yet. It gives me hope that there are more treatment options out there. There are so many people working at different levels to help folks with myeloma be better-taken care of. They’re looking for a cure, so that’s very exciting. They’re getting closer than they have ever been.
It’s about survival, doing the right things, getting support, and being tough.


Special thanks again to Karyopharm Therapeutics for its support of our independent patient education content. The Patient Story retains full editorial control.

Inspired by Theresa's story?
Share your story, too!
More Relapsed/Refractory Multiple Myeloma Stories
Theresa T.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: IgG kappa Light Chain
Initial Symptom: Extreme pain in right hip
Treatment: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
Donna K.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: None, found by blood tests
Treatment: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T, selinexor-carfilzomib
Connie H.
Diagnosis: Multiple myeloma, relapsed refractory
1st Symptoms: Chronic bone pain
Treatment: IV Chemotherapy, CAR T cell therapy
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
Beth A.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: Non-secretory (1-5% of myelomas)
1st Symptoms: Extreme pain between shoulder blades, sternum, head, burning sensation
1st Line Treatment: VAD chemo, radiation, stem cell transplant
RR Treatment: 8 chemo regimens, successful combo→selinexor+bortezomib+dexamethasone
Scott C.
Diagnosis: Multiple myeloma, relapsed/refractorySubtype: IgG lambda (majorityof myelomas)
1st Symptoms: Pain in hips and ribs, night sweats, weight loss, nausea
Treatment: Clinical trial, chemo, kyphoplasty, stem cell transplant





