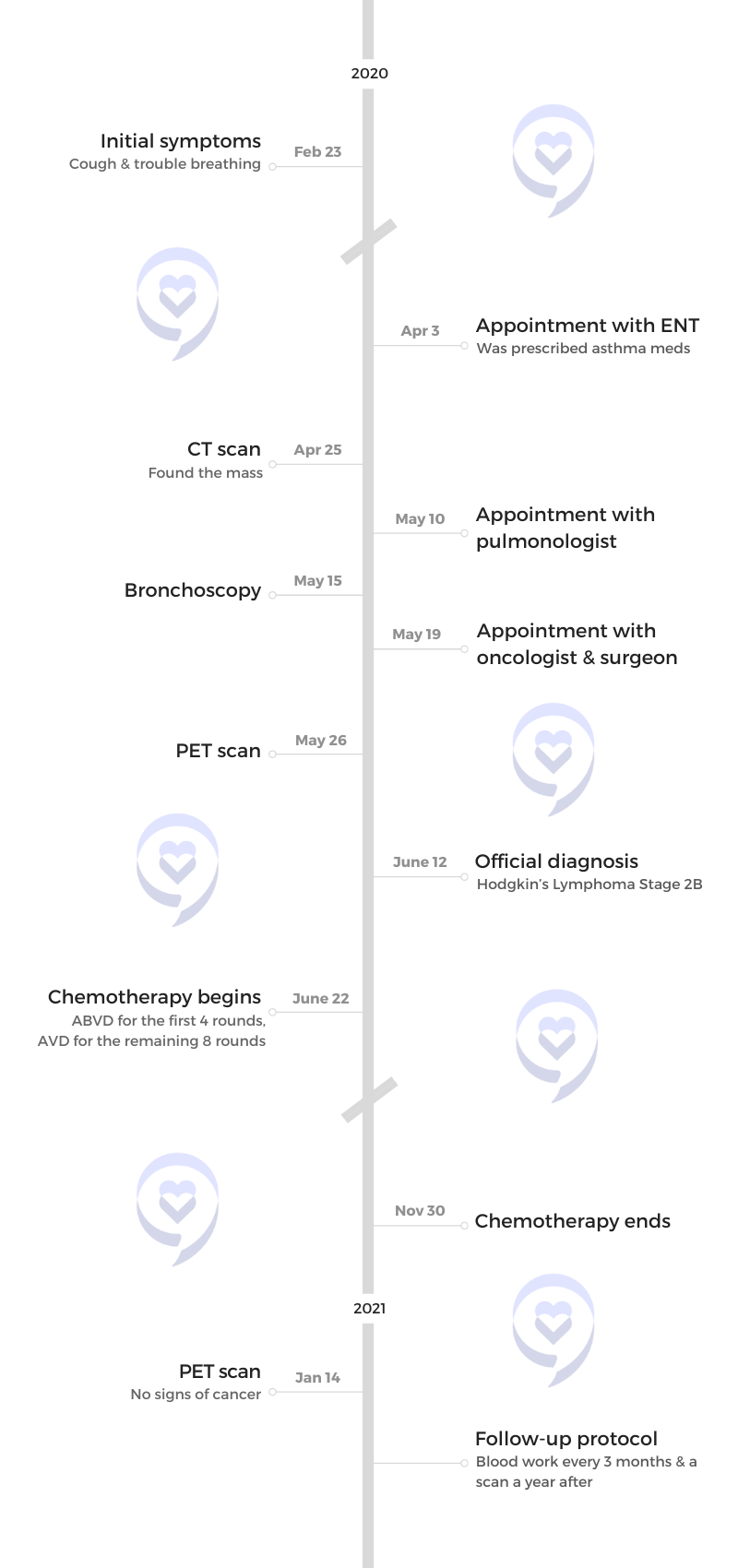
Patrick’s Stage 2B Hodgkin’s Lymphoma Story

Patrick was diagnosed with Hodgkin’s lymphoma after experiencing trouble breathing and a dry cough.
Having always been athletic, his breathing started to get heavy while training for a marathon and he couldn’t continue to run. After an anniversary trip with his wife, his symptoms got worse. Something in his chest didn’t allow him to take a full breath.
After initially being diagnosed with asthma, an X-ray showed something in his chest that prompted a CT scan and then a PET scan, which eventually revealed a 3 cm lymph node.
Patrick underwent 12 sessions of ABVD chemotherapy over six months, experiencing side effects such as burning gums, nausea, and brain fog. Despite the challenges, staying physically active during treatment helped him stay positive and maintain hope. He shares how pandemic protocols affected his experience and how he manages scanxiety.
In addition to Patrick’s narrative, The Patient Story offers a diverse collection of Hodgkin’s lymphoma stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Patrick C.
- Diagnosis:
- Hodgkin’s Lymphoma
- Staging: 2B
- Initial Symptoms:
- Dry cough
- Trouble breathing
- Treatment:
- Chemotherapy: ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine)
Just because you’ve gone through something traumatic doesn’t mean your life is over. Do your best and the rest will come.

Introduction
I’m 43 and I’m married.
I’m a runner, marathoner, trail runner, weightlifter, and cyclist. Not really a cyclist anymore, but those are my hobbies.





Pre-diagnosis
Initial symptoms
I was training for a marathon and I was out running. My breathing was starting to get heavy and I couldn’t continue my run.
As someone that’s always been athletic, a cold or cough has never knocked me down before. I always trained through it. I always pushed through it.
But this was different. I had to stop and that’s never happened to me before. I didn’t know what was going on with me so it drew awareness.
I felt something in my chest, but I thought it was a cold or allergies. After just two miles, I have to stop.
It was [a] dry cough. Nothing was coming out. I’ve never had a dry cough in my life. When I was sick, there was always something there.
Reaction to feeling symptoms
I thought, I’m going to take a break and come back tomorrow. This is very, very strange to make me stop. This was February 2020, the day before my one-year anniversary.
The next day, I tried to run and just didn’t have it in me, which is rare. I hopped on my bike trainer and still felt breathing issues, but it wasn’t as bad so I said, “Maybe it’s just a bad cold or something.”
We celebrated our anniversary, went out to dinner, and caught a flight the next morning to Santa Fe, New Mexico, which has [a] really high altitude.
It got way, way worse. It felt like there was something in my chest that wouldn’t allow a full breath. It was scary in [that] this isn’t normal. But my stubbornness was putting in my head that it was a cold that needs to go away added on to altitude.
We came back to Houston. It’s not allergies because we went to a different part of the country that doesn’t have many trees so I thought it was our trees. It got a little better but it still never went away.


Being diagnosed with asthma
I finally caught the ENT doctor and he said I developed asthma. I just said, “Okay, I have asthma,” and went on to the next step.
My mom had asthma when I was a kid so I figured it’s asthma, let’s get it taken care of, give me the medicine. I need to get back to my life.
This was during COVID. The pandemic started as we were getting on the plane from New Mexico back to Houston.
The appointment was over Zoom. He said, “I’m going to give you asthma medicine. It sounds like it’s asthma.” He prescribed asthma medicine and it never did anything. I actually think it made it worse. I started getting gradually worse.
I called him again. He said, “I’m going to give you more medicine,” and it kept getting worse. By this time, he said, “They’re allowing us to see patients now. Can you come in? I’m going to give you an asthma test and an allergy test.”
He made me blow through a machine. He said, “I don’t think you have asthma.” Then he gave me an allergy test and said, “I’ll have these results to you in a couple of days, but I want you to go take an X-ray.”
He sent me to get an X-ray. I went home and got a phone call saying, “There’s something in your chest. It could be cancer. It might not be cancer, but I want you to take a CT scan.”
Hearing the possibility of cancer
I’m a very optimistic person. I thought, This is the ENT. He doesn’t know what he’s talking about. There’s something in my lungs. They’ll figure out what it is. I’ll be back on my feet in no time.
I didn’t think much of it at all. I was very positive. I called to make an appointment for a CT scan. Everything was backed up because of COVID so it took weeks to get in.
I went to get my CT and went to work. The doctor called and said, “This is serious. You either have lung cancer [or] a slight possibility of lymphoma. If it’s lung cancer, it could be stage 4.”
I used to smoke and I grew up in a smoky house. Everybody smoked in their houses back then. I said, “There’s no way I can have lung cancer. I run so much. I’m very active. It’s been 10 years since I smoked.” He said, “You’ll be surprised. It can affect you later on.”
I called my wife and said, “You need to come home. I’m on my way and we need to talk.” I told her and [said] we need to take further steps to figure out what’s wrong with me.
Breaking the news
It was the hardest thing I’ve ever done. When she walked through the door, she knew something was wrong. It was pretty bad.

Getting a bronchoscopy
He connected me to a lung doctor at Houston Methodist Hospital to do a bronchoscopy. It took two weeks to get that bronchoscopy.
He called me the next day and said, “I don’t think it’s lung cancer, but we can’t count it out. I do not find any trace of lung cancer in your lungs. But I’m pretty sure it’s lymphoma.”
Hearing the possibility of lymphoma
I heard of lymphoma. I just never knew what it was.
I started doing research. My grandmother passed away after battling leukemia 10 days before I started feeling my cough and my shortness of breath.
He didn’t tell me what kind of lymphoma it was. I was 39. They said Hodgkin’s lymphoma usually affects people 35 and under. I thought, Oh, so I might have non-Hodgkin’s lymphoma. The chance of living is a lot less than Hodgkin’s lymphoma. That was going through my head.
Meeting with an oncologist & cancer surgeon
He set me up with an oncologist and a cancer surgeon at Methodist in case they have to do biopsies and whatnot. I met up with the surgeon and the oncologist at the same time. It took about two weeks again for that.
The whole process was pretty long. They did a PET scan. When I met with my oncologist and the surgeon, the surgeon said, “Do you feel this? That’s your lymph node. I’m pretty sure you have lymphoma.”
It was on my right side, 3 cm. You could see a little bit, but I was so lean that I thought it was part of my muscle. After looking at it, I thought it was my traps (trapezius muscle). I really didn’t think much of it.
My oncologist said, “We can’t cancel out lung cancer or even testicular cancer because, statistically, cancer can come up and raise lymph nodes in your lung area.” They set me up to do a biopsy. I never had a swollen lymph node in my life so I didn’t think anything of it.
I went down the Google wormhole. This was on a Friday and he said, “I want to have this surgery on Monday morning, Tuesday morning at the latest. You’ve been getting the run around with this for too long now. We need to get you in.”


Having your doctor advocate for you
I knew COVID was an issue then, but I was a little bitter. They’re pushing back cancer patients for COVID.
I really like what the surgeon did. COVID tests were taking two weeks. They didn’t have [the] rapid COVID test yet. This was [the] end of May 2020.
They said, “He needs a COVID test, but it can take a week for the results.” He said, “I don’t want it. I need him in.” They said, “We need to have a COVID test.” He said, “I don’t want him to have a COVID test and wait that long.” He got me in. That would be my third test within a month they made me take.
Getting a biopsy
He did the biopsy. I was already out, but he told my wife, “I think it’s Hodgkin’s lymphoma,” just by the biopsy, which is a good thing. That was some relief that it was Hodgkin’s lymphoma, very curable.
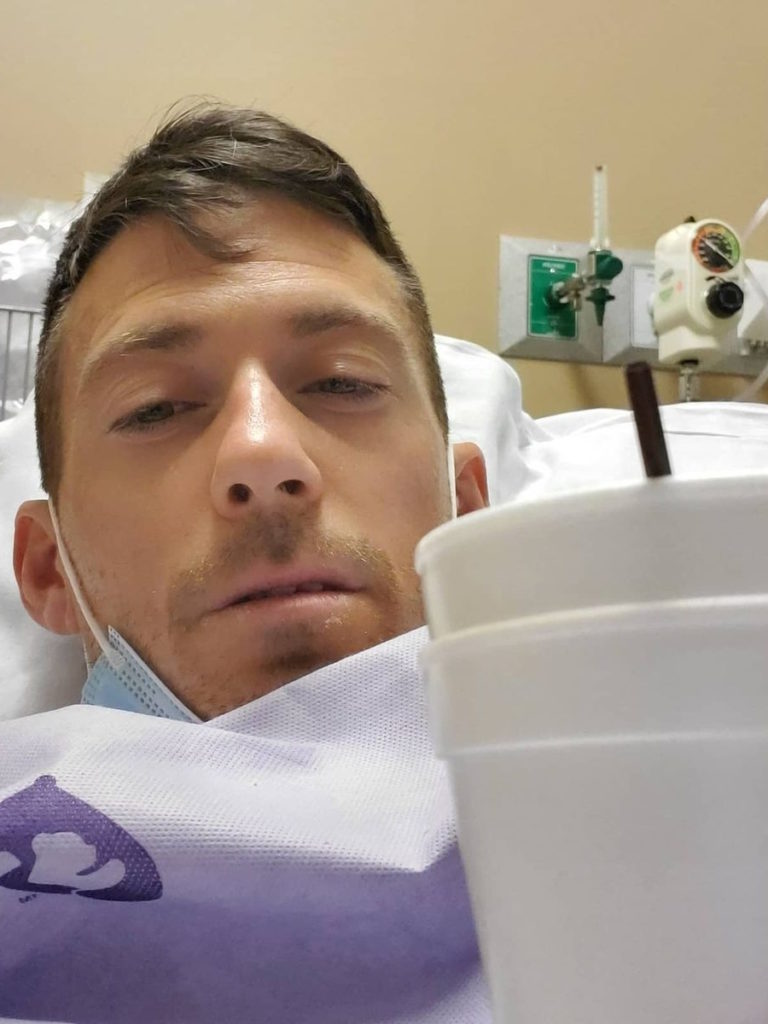
The appointment was at 8 o’clock and they made me get there at 5:30 for check-in. They put me in a room and gave me drugs. I actually had an allergic reaction to the anesthesia so they gave me Benadryl to calm that down. Then they put me into a surgery room and I was out.
It took about 2.5 hours. I woke up in this room and said, “What’s going on here?” Then they pushed me back and that’s that. For three days, it hurt pretty bad. I had a big scar.
Diagnosis
Getting the official diagnosis
He knew instantly that it was Hodgkin’s lymphoma but they couldn’t officially diagnose me. I had a follow-up appointment with my oncologist four days later.
My wife and I were a nervous wreck. My oncologist is a very young, very smart, and very positive doctor. We were sitting there and she opens the door really fast with a big smile on her face.
She said, “It’s really good news it’s Hodgkin’s lymphoma not non-Hodgkin’s lymphoma, lung cancer, or testicular cancer. It’s stage 2B Hodgkin’s lymphoma. We’re going to start you on chemo the following Monday.”
Discussing the treatment plan with the oncologist
She said [with] stage 2B, you usually go through 12 [sessions] within six months, every two weeks. ABVD for the first four and they take out the B, the bleomycin. She was really adamant to get me off bleomycin because I run a lot and I was a smoker in my 20s.

Shared treatment decision-making
I told her, “I need to run the Houston Marathon. If I finish chemo, it would put me at the end of November. Would I still be able to run?” She said, “Yes.” I said, “Yes!” And then my wife said, “No, you’re not.” She knows how I am. It was canceled anyway because of COVID.
I told her, “It’s very important that I stay active and still work. I want my life as normal as possible.” Running, cycling, and lifting weights is my therapy. She said, “Then we need to try to get you off the bleomycin after number four.”



Treatment
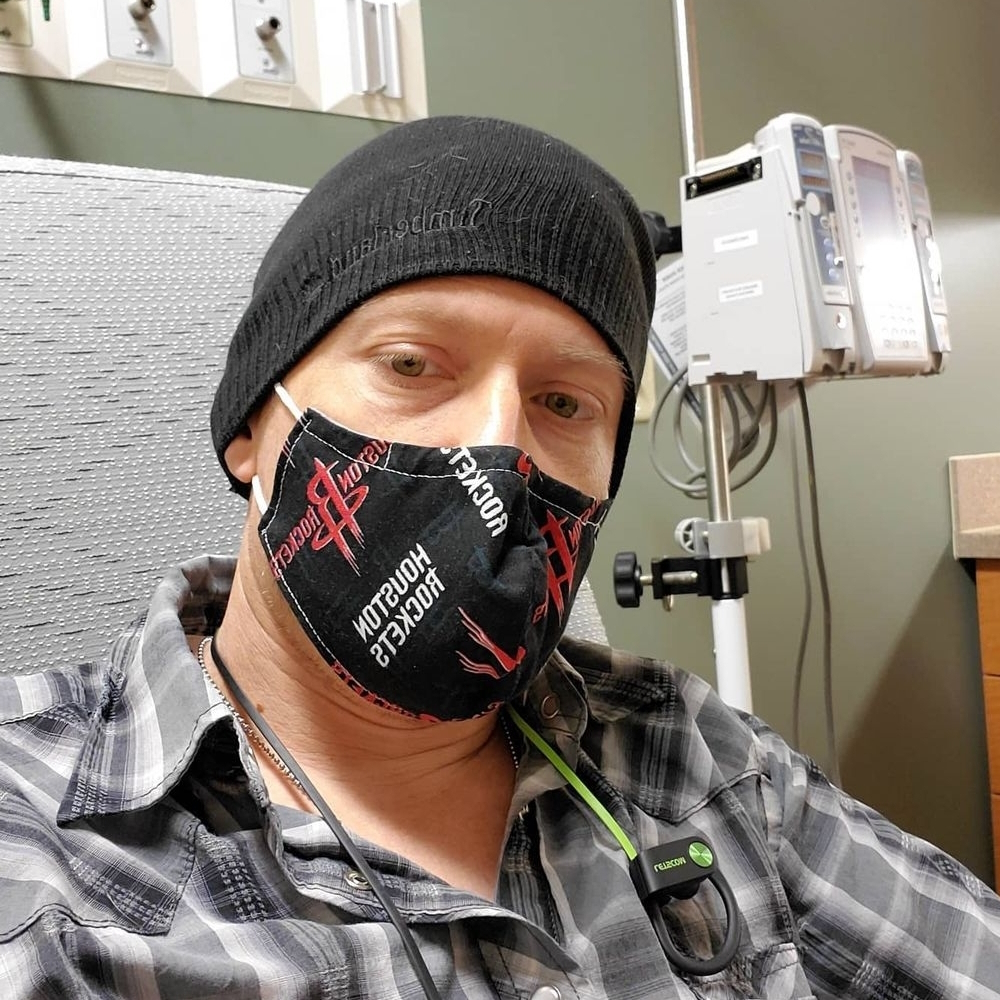
I’m not going to lie and say I wasn’t scared. Your whole life, you’re taught chemo patients are high risk. I was nervous, but I was very positive. I said, “I’m going to crush this thing. My life is going back to normal. I’m going to do my best to do what I do daily and not let this put me down.”
I walked in with a positive attitude. The nurses love me. They said, “You are the happiest person here.”
ABVD chemotherapy
They let my wife come with me because COVID cases just dropped a little bit, which was great. She sat with me [for] the whole five hours.
They took my lab work. They gave me the pre-meds. As soon as they hooked the chemo up, I felt it instantly. “Oh, this is not fun.”
I got there at 7 o’clock and I was there till 11:30. They would come in every hour and replace the chemo bag with something new.
Every two weeks for six months. The second treatment was pushed back a week because my lab work was off. They wanted to make sure the chemo wasn’t messing up my liver. My liver enzymes were really high because I was taking valerian root, a sleep herb. That was the only one that got pushed back.


Side effects of ABVD chemotherapy
My gums were burning. Nausea and my gums were my first side effects.
The steroids would keep me up at night. The first two nights, I would be wide awake with full energy because of the steroids, which they gave before the chemo.
I had brain fog.
Managing the side effects of chemotherapy
I tried to take the nausea medicine and it didn’t work. It made me feel a little worse. I took them one time and never took them again.
I stayed active the whole time. If I couldn’t lift weights or ride my bike, I would go for walks. My wife would go with me a lot of times.
The week of treatment, I felt bad. Then starting Friday afternoon, I will start coming back to life. My brain fog and nausea will start going away and I would start getting a lot of energy.
By Sunday, I usually felt back to normal. My life would be normal for a week. Chemo [on] Monday morning, a week of feeling bad, then a week of feeling good. It was a big cycle. Every treatment week got worse and worse and worse.
How being physically active helped
The day after my first treatment, my wife and I went for a four-mile walk. I don’t want to sit on the couch and feel miserable. I want to go and I felt it helped me.
It gave me more positivity [and] more hope. It put in my head, “I’m beating this.” I felt it was better for my mental being more than my physical being.
I stayed pretty positive. I did get upset a lot easier. I wouldn’t say lose my temper, but I was a lot more sensitive. My wife and I didn’t fight, but there [were] episodes where I would be snappy at her, [at] coworkers.
I think I had more episodes of depression before cancer than while I was going through chemo. In a way, it made me less depressed because it made me realize that I can still do almost everything I could have done before. I’m stronger than I think I am.
I decided to take the week off my last chemo and not be active. I wanted to take a break from everything and just relax. That last week was the worst I’ve ever felt.
I was sick the whole time. I was worse on everything and I think it’s because I sat on the couch and did nothing. I felt bad for myself.





Post-treatment
I had a PET scan after number four to see if I can get taken off the bleomycin. The doctor said no more bleomycin.
Then I had a CT scan after eight. There [were] no signs of cancer in me. They were going to determine if I needed radiation and I didn’t.
My insurance wanted to wait six weeks before I had my next scan. I had my PET scan six weeks [after] my last chemo and it was all clear.
No evidence of disease
We were in my car on a Zoom appointment with my doctor because they were back in COVID protocol. I was happy because my wife was able to be with me. She couldn’t go with me to doctor’s appointments before so it was a great moment.
I was in my truck outside of work, on my lunch break, with my wife, and it was such a great feeling. It was one of the best things I’ve heard in my life.
She teared up. She was really happy, of course. It was a journey.
Follow-up protocol
I got a scan after one year. Everything was good.
My oncologist said I just need blood work. Every oncologist has different opinions. Some want every year for the first five years. She said I don’t have to. I can if I want.
I opted out [of] my two-year scan because my blood work came back good and I feel great. I’ve heard [to] try to minimize scans because they’re not the best for you.
Managing scanxiety while waiting for test results
I would just go throughout my day. Go to work. There are moments I would forget about it then I would constantly check my chart after the scan. It gave me scanxiety but not where I couldn’t focus or knock me on my knees, which I’ve heard it does to some people.
[With] my first CT scan, I just wanted to get to the bottom of what was wrong with me so I ignored it. I wasn’t even nervous. I was three months in on this and wanted to find out what was wrong. My second scan before I was officially diagnosed [was the] same.
After chemo started, it started to get a little scarier [thinking] that, I hope I’m doing good. But the actual scans never really affected me.


Running the Houston Marathon after chemo treatment
After my last chemo, I started getting really, really active. The day she told me I had no signs of cancer, I went all out. I signed up for the next marathon. I completed the Houston Marathon one year and one day after she told me I was cancer-free.
It was a great feeling. I was mad at myself because I didn’t hit my goal. I’m very competitive, but deep down, it was one of my proudest moments. Besides marrying my wife, it was probably my proudest moment.
People think that their life is over after cancer and it’s not. I was 40 years old, got through chemo, and completed a marathon afterward.
I trained so hard that I knew I had it. It was more emotional for my wife. She posted Instagram stories and said, “I’m so proud of him. He went through a lot and he’s doing stuff that a lot of people are scared to do.”
Words of advice
Listen to your body. If your body tells you [to] get up and move, even if it’s a little bit, do it. It will bring up your spirits.
Just because you’ve gone through something traumatic doesn’t mean your life is over. Do your best and the rest will come.
When I push really hard, I feel my lungs are not as strong as before, but I ignore it.
I refuse to let it beat me down.




Inspired by Patrick's story?
Share your story, too!
More Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)