Nicole’s Hodgkin’s Lymphoma Story

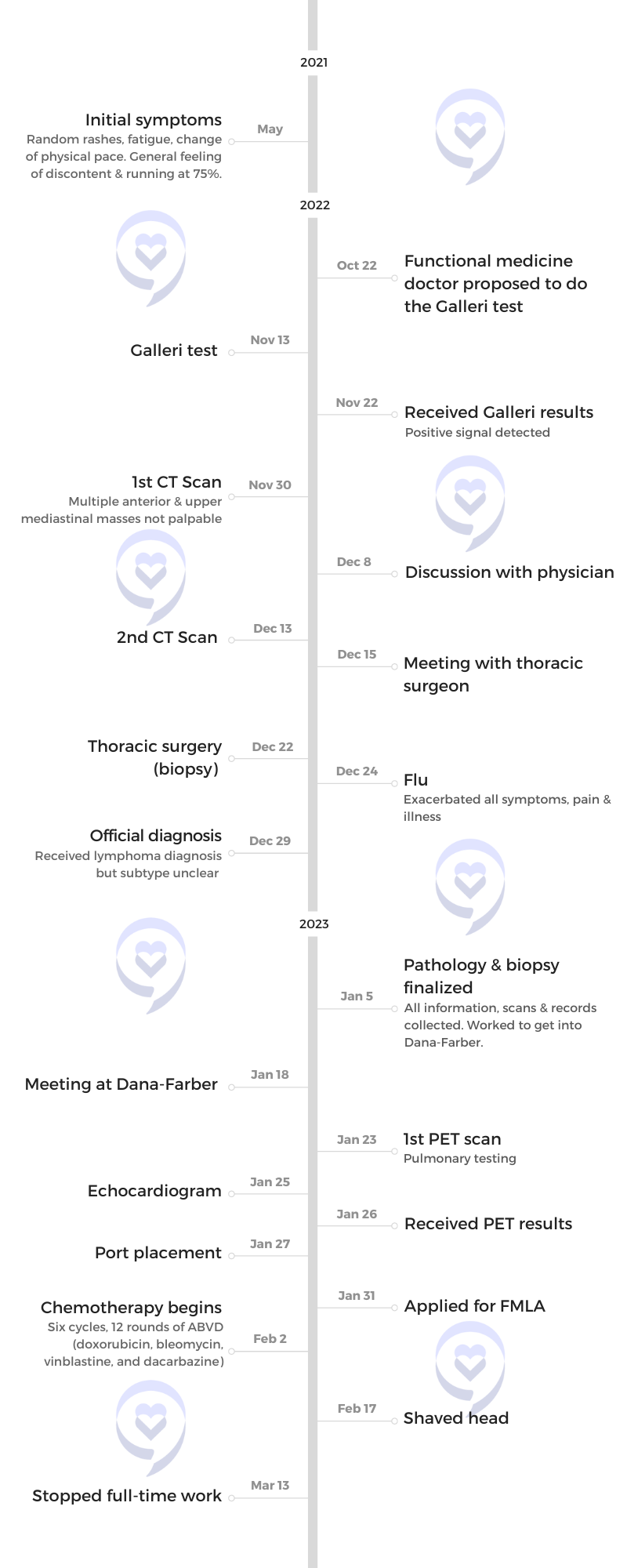
Nicole, wife and mother of three, was diagnosed with classical Hodgkin’s lymphoma in November 2022.
She only experienced general malaise and had a rash appear randomly throughout a six-month period. Desperate for answers and without any discernible symptoms, she turned to a functional medicine doctor who decided to give her a multi-cancer early-detection test.
Testing positive for cancer through a Galleri test got the ball rolling and got her started on her journey. Throughout her experience, Nicole faced challenges, including the mislabeling of her symptoms as anxiety and the need to advocate for herself with each doctor she encountered. To feel less alone, Nicole sought out online support groups and found comfort in The Leukemia & Lymphoma Society.
In addition to Nicole’s narrative, The Patient Story offers a diverse collection of Hodgkin’s lymphoma stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Nicole D.
- Diagnosis:
- Hodgkin’s Lymphoma
- Initial Symptoms:
- Fatigue
- Random rash
- Treatment:
- Chemotherapy: ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine)


Introduction
I’m married. I’m a mom of three. I live in New Hampshire.
I love gardening. I love arranging flowers. I don’t own a business but would like to, in my dreams.
I’ve done digital marketing for 20 years.
I love my friends, hanging out, and the idea of going back and doing that all.





Pre-diagnosis
Initial symptoms
After my last baby in 2021, I didn’t come back the way I [did with] my other babies. But I was over 40 [and] had thyroid issues. Everything I was feeling could be attributed to my thyroid. I was trying to see [an] endocrinologist. It was around COVID so it was impossible to get in.
I had a weird rash on my arm. It goes away [and] comes back. I couldn’t figure it out. Did I have wine? Did I have cheese? Did I have bread? What’s happening? Did I get too much sun? I had no idea. Other than that, I was pooped.
They wouldn’t see me for six months. My physician kept attributing it to lack of sleep, thyroid, anxiety, and random things I knew weren’t right.
I knew something was wrong. I didn’t have the B symptoms, night sweats, itching, and temperatures. I was checking everything. I was looking for anything because the minute I had something, I could be seen by someone else. At that point, my cycles were off and I was feeling so shot and really sad, frustrated, and lost.
I [went] to see a functional medicine doctor. She’s my neighbor so I walked across the street and said, “My thyroid is busted. I can’t get in until December.” This is in the middle of the summer. I’m sweating. I can’t leave my house. I have a baby, the kids, everything. She said, “I’ll take your blood work.”
She started seeing me as a patient. She fixed my thyroid, by the way. It was off the charts. That wasn’t the problem, but my thyroid was to blame for some of these things.
I spent a couple of months with her going through everything and trying to make changes in my diet, my sleep, [and] my lifestyle.
Everyone always puts “anxious” on my chart. It’s [been] on every chart ever since I started seeing doctors. Generalized anxiety disorder, I think
She said, “I know you’re really anxious. I had a pharmaceutical person come in for something called Galleri. It screens for 50-some-odd cancers. Why not do it? It’s for 50 & older, but I’m your physician so I can get it approved. This will ease your anxiety. You think something’s wrong with you. I don’t see anything wrong with you. Your labs are perfect. We’re working on your thyroid. We’re getting your weight down.”
I thought I was feeling better, but I was pushing so hard to change everything so some of it was psychosomatic.





Putting the blame on anxiety
I’ve spent a lot of time with different doctors. I’ve been able to speak to or change doctors because of how I relate to them. I explain that I know about my anxiety. I’m very, forthcoming about my anxiety and it’s very specific to [my] health.
But I also have [my] gut and I haven’t been wrong a lot in my life. I’ve had things happen. [With] my third child, I had HELLP (hemolysis, elevated liver enzymes, and low platelets). I just felt weird. My baby and I wouldn’t be here if I didn’t say something.
I preface a lot of my first appointments with, “I understand that this might appear as anxiety or that I’m tightly wound.” I idle high. They either get it or they don’t and I explain that I know it.
In this process of lymphoma, I’ve told every single doctor, “I know I’m not your only patient and I get that. I’m not minimizing myself, but I’m also aware that you’re running around. But you have to understand, I’m here with you now.”
I started being very forthcoming [with] doctors [at] around [age] 20 or so. Along the way, I learned how to talk to them and if it doesn’t work, it doesn’t work.
Getting a blood test that screens for different cancers
I was ready for any test. My functional medicine doctor said, “It’s a blood test. It screens for certain cancers. It has a ton of false positives so be aware of that.”
I believed that this would change my anxiety. When people take your blood, you start to feel better because everyone always banks on blood.
It’s not cheap so I had to find the funds and dive right in.
I read my little pamphlet. I went to the site, but it was all very new. I read as much as I could about it.
I hadn’t seen my PCP in a while. I haven’t fired her because I need her for my insurance because a functional medicine doctor isn’t covered; it’s an extra.
I waited for two weeks. Every time I went to her or any specialist, everyone kept asking, “Are you going to finally be satisfied when you find out you don’t have cancer?”
I wasn’t sure it was cancer. I don’t have the words to explain what I know. I kept thinking to myself, I don’t know where everyone’s going here, but I haven’t got my results yet.





Getting the results of the cancer detection test
It came to her in the mail. They called me to schedule an appointment and I said, “I know why you’re calling me. Can we just get on the phone? We’re not going to wait till next week.”
I tested positive for a cancer marker. There [are] false positives so everyone went to the false positive conversation. Now we have to prove that it’s real.
Getting a CT scan
I wanted to know what was next. Like every other process, you have to prove you need certain tests. No one felt anything. I still don’t feel anything.
I had to go through all the steps of going to a PCP, showing this test, asking for a CT scan, getting that approved, and pushing it through insurance. I had to work with my employer, my PCP, my functional medicine doctor, and Galleri. I had to make sure I had everything.
This is where you learn self-advocacy and the fight. I don’t mean to be pessimistic, but it is a fight. You have to go all in with everything and push, push, push.
I finally got in to get a CT scan. Of course, it wasn’t covered because of all these things. They picked an area and there was a piece where they thought they saw something.
I had to go back, but I had to ask for all of those things again to get the rest of my area. They found a mass behind my chest. There’s no way anyone was poking anywhere. There were a few “friends” around it, but nowhere palpable.
Finally, I have the thing that I need to go somewhere.
Diagnosis
Reaction to finding a mass
This isn’t the one I expected because I didn’t know you could have something and not feel it.
I was also scared. All I thought about was my kids. Where do you go from here?
Now I’m really in the dark. You can say to anyone, “Don’t Google.” I’m in marketing. I’m a researcher. That was my reaction.
I knew I had a long road. I knew that because getting to that point took two and a half, three months.





Feeling something was off & no one was listening
I actually said to my doctor, “I told you so,” but she knows me well enough to laugh. I told my husband, “I told you so.” I wish I was wrong.
Ultimately, I was glad I was right, mad I was right, but I knew I had a road ahead of me. I didn’t know what that meant and neither did my functional medicine doctor.
Getting the mass biopsied
It turns out the CT wasn’t proof enough to get into a cancer center or a professional oncologist.
I found a thoracic oncologist. He had to reach out to a bunch of people because it was mediastinal, meaning it’s behind my chest near my heart. I got that done before Christmas and they had to send it out. I had to wait, of course.
I told my surgeon, “When you go in there, I open myself up to infection.” Sure enough, I got the flu. Then all of the symptoms came. I lost my voice, I got sick, I got [a] fever — all the things happened.
I lost my voice for months. That mass was starting to press on my vocal cords. Everything started triggering my immune system. They started moving me along fast. Everything started getting worse. Honestly, I felt worse after the biopsy than I did before.
Waiting for the biopsy results
While waiting, I had to get things approved, like the surgery, then I had to wait for the biopsy results. It was Christmas time so I had to get my head in the game.
Everyone thinks that it comes back quickly. Everyone will always say waiting is the worst. You expect it to happen fast. It doesn’t.
When my biopsy results came back two weeks later, it wasn’t conclusive.
They said some of it was crush biopsy and they had to send it out to another institution for another person to look at. I lost my mind. More time? Is it growing? Is it spreading everywhere? Where is it going?
Getting the biopsy results
I finally got [a] cancer consultation because I had proof on paper. [The] results of my biopsy came in through my portal, but no one called me.
The surgeon actually called me and apologized. There [are] so many things that go on that you just have to do all your work. You’re also pooped out and sick.
Even though I finally had an answer, I was still losing my mind. It was the loneliest feeling. I thought I was just being emotional.





Getting the official diagnosis
When I got my biopsy from Utah, it was diagnosed as Hodgkin’s.
I’m in a small segment. There [are] only 8,500 diagnoses of classical Hodgkin’s lymphoma a year in the United States. I’m in a different age range and it’s a smaller subset of people. As a mom, I felt extra lonely in a weird way because I couldn’t find anyone. I also didn’t know if I was overreacting.
I chose to go to Dana-Farber.
I didn’t get a PET until after my consultation and after they started planning my chemo. I had my chemo and my port dates before I even had my PET date.
Treatment
I got my port in then started chemo four days later. After my PET, they said it was between stages 2 and 3. They wanted to start pumping me with chemo to see what would work and what wouldn’t.
With lymphoma in general, staging is not nearly as important. Blood cancer staging is different. Nothing is more annoying than someone saying, “I’m sorry you have cancer. What stage is it?” It’s the third question everyone asks before, “How are you?”
ABVD chemotherapy
My treatment plan was ABVD for six cycles, which is 12 rounds.
Side effects of ABVD chemotherapy
In the first infusion, my side effects almost were all psychosomatic in terms of it was obviously anxiety. I asked for fluid so I’d be extra hydrated. It’s important to hydrate the day before.
I tried to go in as a good student. You meet with the nurse the day before and but I felt I almost knew as much as she shared in terms of what to buy, what to do, and what to expect. I had so much time. Why not prep? That’s my nature. I knew what was coming.
My first side effects were straight-up anxiety. They gave me three different anti-nausea prescriptions, but it was all anticipatory and panic. During and after my first infusion, my body was fair, my brain was not.
Over time, the side effects are dehydration [and] constipation from the anti-nausea meds.


I felt like I was in a chemo coma like someone was laying on top of me. It’s like the worst flu. I wanted to get up and do things, but I knew to lay there because the more I rested, the better I would bounce back.
My appetite was quite good. I was eating all my favorite, terrible foods. I know so many people go into health mode, eat really well, and do everything by the book. I admire them. I thought, I’ll eat because I’m hungry and I’m scared that one day I might not want to.
I took a lot of Epsom salt and baking soda baths. I drank a ton of water and liquid IVs. You feel crinkly and tight. I knew the more I could get out, the more I could start moving.
As you go on, it weighs on you heavier. I have a harder time bouncing back. I would say my third or fourth day is [when] I get really frustrated and force myself to really dive in. I know it’s not necessarily the best idea, but it does help in that what chemo does to your body. You start to get a little looser. You’re moving and doing things.
I’m so dizzy sometimes [that] I don’t even know what to do with myself. Sometimes I feel it coming. I’ve never passed out before, but I feel like that’s what happens.
My appetite is getting worse. I’m not as hungry for my favorites. I can’t eat as much. I still eat mac and cheese. Why not? I already have cancer. Let me have mac and cheese. I used to be able to eat the bowl, but now I’m slowing down.
People imagine what they see in the movies. You’re going to be puking and basically hugging the toilet. I look very, very frail and unable to eat. This may happen [to] some people.


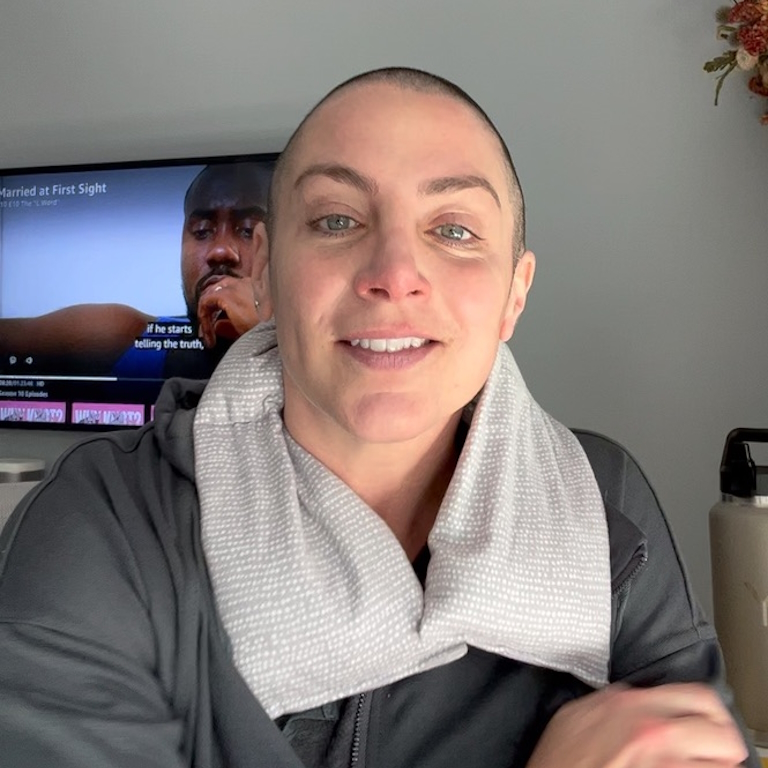
Hair loss from cancer treatment
Prior to starting chemo, I already cut my hair shorter because it was falling out. I did that in anticipation. I was working my way up. I already felt less feminine. I hate to say it, but I did. My son said, “Mommy, you look like a boy from the back.” Ugh, but it’s fine. It was just funny.
The day after my second treatment, I leaned over the sink and had a hot flash. I said to my husband, “Kevin, get the buzzers.” All the kids shaved and Kevin helped. Everyone got a turn.
I was trying not to cry. He was shaving my head, saying, “You’re pretty. You’re pretty. You’re pretty.” I had to make it quick. I wanted the kids involved because I don’t want them to be shocked when they saw me again. I was just getting a haircut and it’d be fun.
I hardly wear a hat. I get hot. Now my perspective is a little different. I’m totally fine with it. I’m shocked every now and then.
My eyebrows and my eyelashes [fell] out.

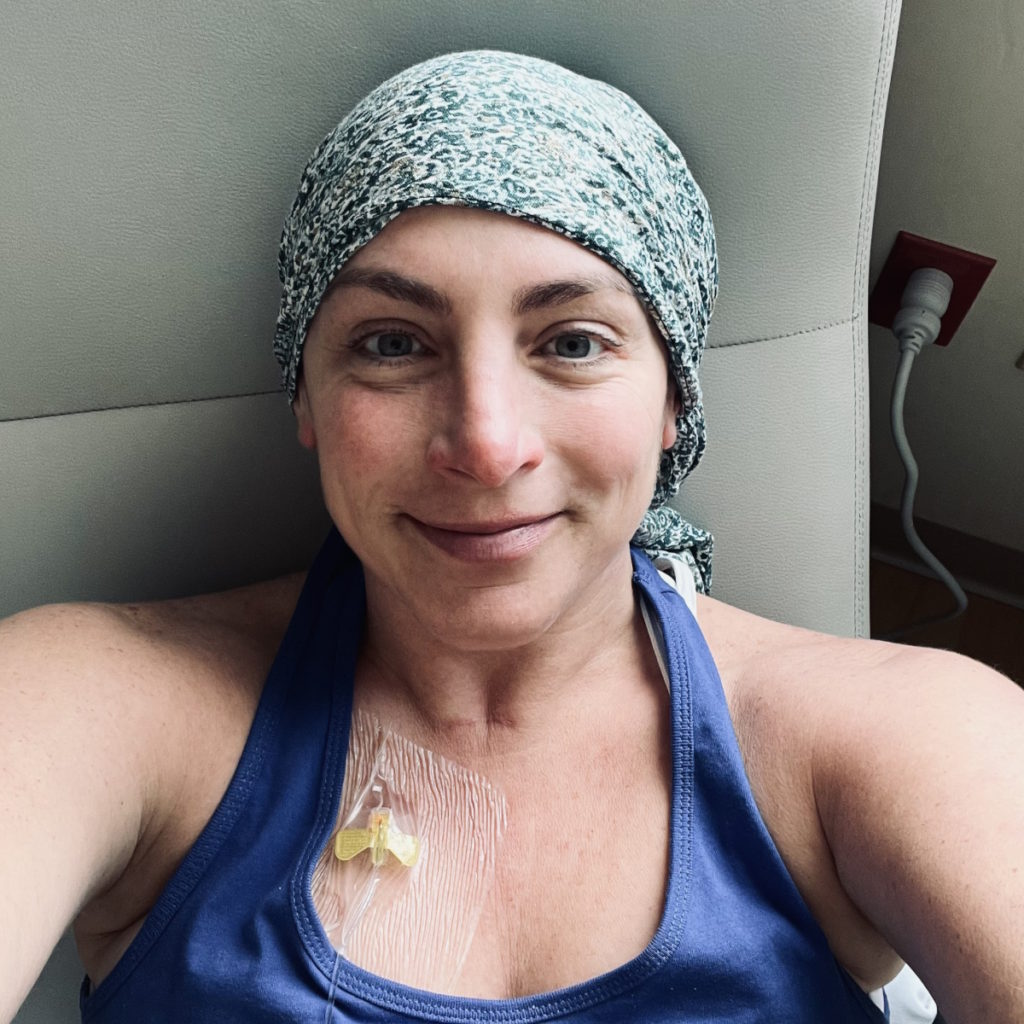
Mid-treatment scan
I’m trying not to look at it as an endpoint.
I had another PET scan. My ABVD is working on the “friends” and slowly on the big mass. I’m staying with ABVD. My body is receptive.
The point of the next PET scan was: is this cocktail working for your body? There are people that just are resistant to it.
There are many first and second lines of lymphoma cocktails. I wasn’t nearly as anxious as I thought I would be going into the PET scan.
The Leukemia & Lymphoma Society is a great resource for learning. It’s good to know there are other lines of treatment, even for the subsets of non-Hodgkin. They didn’t know which one I had when they sent it out to Utah so I was looking around.



Finding support
Feeling alone
I felt different before and after. Before, no one was listening. Even my own family is used to me saying, “I feel like something’s wrong.” Not hypochondria but they probably view me that way now.
You work hard just to be heard. I was feeling very alone because no one was listening. Then when everyone had reason to listen, I felt alone because the minute I finally had the diagnosis, I didn’t fit in. When I looked up what I had, I didn’t fall into the early or late diagnosis.
That made me wonder: What does that mean for how I’m treated? What does that mean for how my life is? Are you going to treat me the same way you would treat a 20-year-old? I don’t think I can take it. I remember being 22. I had more energy.
I even posted [on] social media. Are there any people between the ages of 35 and 45? Looking for cases similar to mine, maybe just a little. That’s where that loneliness fell into play.


My oncologist helped point me in the direction of The Leukemia & Lymphoma Society and social workers. I had my therapist.
The more I reached out to others, it helped, even though they could be in another country. Simple advice of MiraLAX the day before or this lotion because of rashes. The loneliness subsides a little bit when you know that you can reach out or get advice.
I’m not sure how I got through that loneliness before I was diagnosed because no one was listening until I got the results. I had to get the results to prove it was time to actually do something about it. I really had to fight the first portion of the loneliness.
This portion that I’m in now is like the world is happening without me and the whole world is living. It comes day to day, person by person, or connection by connection. Having a regular conversation will carry me through the next few days.
My therapist is hardcore. She does not like crying. “What if it doesn’t work?” She doesn’t like any of that stuff. Pick your therapist how you want, but I needed a drill sergeant because I could go down a rabbit hole.



Joining support groups
I’m on Hodgkin’s and non-Hodgkin’s Facebook groups. I’m also on refractory/re-occurrence because they have great advice in regard to [the] post-first line of treatment.
I’m proactively reaching out to moms who are in a panic. No one understands. Your sleep schedule’s off and you’re panic writing just to write back or have someone write back to you.
I didn’t even go on Reddit because I thought it was for the young folk, but there is a huge lymphoma community there. They are very supportive considering the vast age range. I can’t believe the number of 70- and 80-year-olds on there.
There are a lot of moms saying, “I don’t even know what to do. I’m going to lose my mind,” so I reach out. People really do keep cancer private, which is interesting. There could be a million reasons why, but I want to be very, very out there about it.
I was very, very self-conscious about the hair. I look pretty sick. Someone tried to help me with my bags at the grocery store. She was 70 and I just had that moment of I’m not sure if I’m grateful or, “Oh my, I’m that person.”
I put myself out there because I know that I might be triggering some moms. I see moms looking at me with their kids. I see the slow down when [they] see me.
I went to get my hair cut before it was shaved. There were moms in the barbershop with their kids. I was so scared I was going to trigger these moms like, “Whoa! That could be me. She’s my age. She’s got a kid. She’s got a kid younger than me.”


It’s not me against chemo and cancer. It’s me and chemo against cancer.
I’ve reached out to moms and other women because I see them saying, “How do you do this when you have a three-year-old?” I have one, four, and seven. If you’re married or you have a partner, they can help as much as they can, but you want to be part of everything.
People imagine the worst. They’ll never pick up their baby. They’ll never be able to breastfeed. Some women get diagnosed while they’re pregnant. Some women receive ABVD while they’re pregnant. It’s a testament to the strength of women.
When I reach out, it feels better. I don’t know anything, but I do know what my experience was. It does help even if it’s not the same.
One woman had all these stomach issues and it’s because she was taking stool softeners in pill form. They sit in your system, as I’ve learned, and they don’t go through your system like regular liquid. The pain is unbelievable.
You feel lonely and even though you might not have the same side effects, it’s better to know that there are other people and you can talk to them. That’s why I was all over The Patient Story even with people with different cancers because I was so desperate to not feel alone.



Words of advice
I highly recommend chewing ice during the A portion of your ABVD. Use baking soda and salt water as a mouthwash when you start and when you go through it.
When I was going through the beginning of my journey, I came upon The Patient Story and wanted to speak out about being your own advocate and speaking to the professionals with confidence and strength.
If you don’t trust someone, move on. Use your voice. Talk to professionals. Go to The Leukemia & Lymphoma Society. Reach out to whoever you trust.
Don’t lose hope. You’re not alone. I was an outlier in terms of the Hodgkin’s, my age, being a woman, a mom, and all that. That’s why I wanted to reach out to moms. You feel alone and you have a lot on your plate. You’re not alone.
While you have the time, breathe and do your homework. Look at it as the biggest project of your life. Put all of your effort into how you are going to handle it. You’re your biggest project.
The minute I knew something was up, I got a therapist that has cancer patients. I highly recommend that.
Not everyone could afford to do what I did and I don’t even really know if I should have done what I did. I hope one day Galleri won’t have to be out of pocket.


The earlier you get ahead of anything, you’re in control a little bit more. When you’re sick, you feel out of control and I think that that’s a huge thing.
You have those days where you just sit in bed and the whole world is outside. I can’t even tell you how many times I hear everyone outside, it’s a beautiful day, and I couldn’t even move. I was a wreck.
Change your overall environment. Instead of rotting in my room, I try to move to the porch for a little while so I can see or talk to people. I don’t like when people come up to me when I’m feeling really sick.
I don’t want to feel left out of the world because you do feel left out of the living world. As much as I want to say that it gets better, I don’t know if it will if I don’t proactively do something about it.
I have three kids and a husband and sometimes, I feel very, very alone in this house. They have to do things. They have to be happy. They have to live.
Remember that it’s up to you to reach out. Have a conversation. Find someone that has something similar. I haven’t done any in-person support groups, but I have loved The Leukemia & Lymphoma Society and its online boards. I can’t believe how many older people are on there giving really wise advice.
Loneliness is really tough when you’re sick because you don’t have the energy and you have to push yourself to solve it. Your brain can do some crazy stuff, especially if you sit on a computer or your phone.
You can drive yourself crazy and you can drive yourself sick. There is a mind-gut connection. People need to be a little aware of what they’re doing to their bodies when they are so sad or lonely.
I keep saying the word lonely, but it’s not necessarily lonely. You’re no longer part of the world you were. You will never be the same again, no matter what. You’ll never have the same life. I think that’s a really tough thing to get your head around.
It’s great to talk about it instead of pretending it doesn’t exist. If I didn’t talk, I wouldn’t be okay. Even though ABVD is currently working the guys in there, if I didn’t use my voice to help me fight it — find it, fight it, and then help solve it — I would be a mess.
You need to speak. Educate yourself. Always push a little further. Trust your gut.





Inspired by Nicole's story?
Share your story, too!
More Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)