Kelsey’s Stage 2A Hodgkin’s Lymphoma Story

Kelsey was diagnosed with stage 2A Hodgkin’s Lymphoma at a young age. She shares her story of going through chemotherapy, why she decided not to freeze her eggs, and how important it is to speak up and advocate for yourself.
She also shares how getting into fashion and style and discovering comedy helped her at a time when she felt like she was losing her identity.
- Name: Kelsey R.
- Diagnosis:
- Hodgkin’s Lymphoma
- Stage 2A
- Initial Symptom:
- Bad leg itching with no rash
- Enlarged lymph nodes
- Treatment:
- ABVD chemotherapy
- Radiation
It is single-handedly the most important thing that’s ever happened in my entire life. Good and bad but mostly good, honestly, in terms of what I’m doing with my life now.


The Patient Story retains full editorial control over all content. This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Pre-diagnosis
- Diagnosis
- Treatment
- Advocating for yourself
- Taking a more active role in your care
- No evidence of disease
- Fertility treatment
- Self-discovery during cancer
- Survivorship
Pre-diagnosis
Tell us a little bit about yourself
I am originally from Arkansas, from a town called Bentonville. I’ve lived in Austin, Texas, for almost a decade. I moved down here after college.
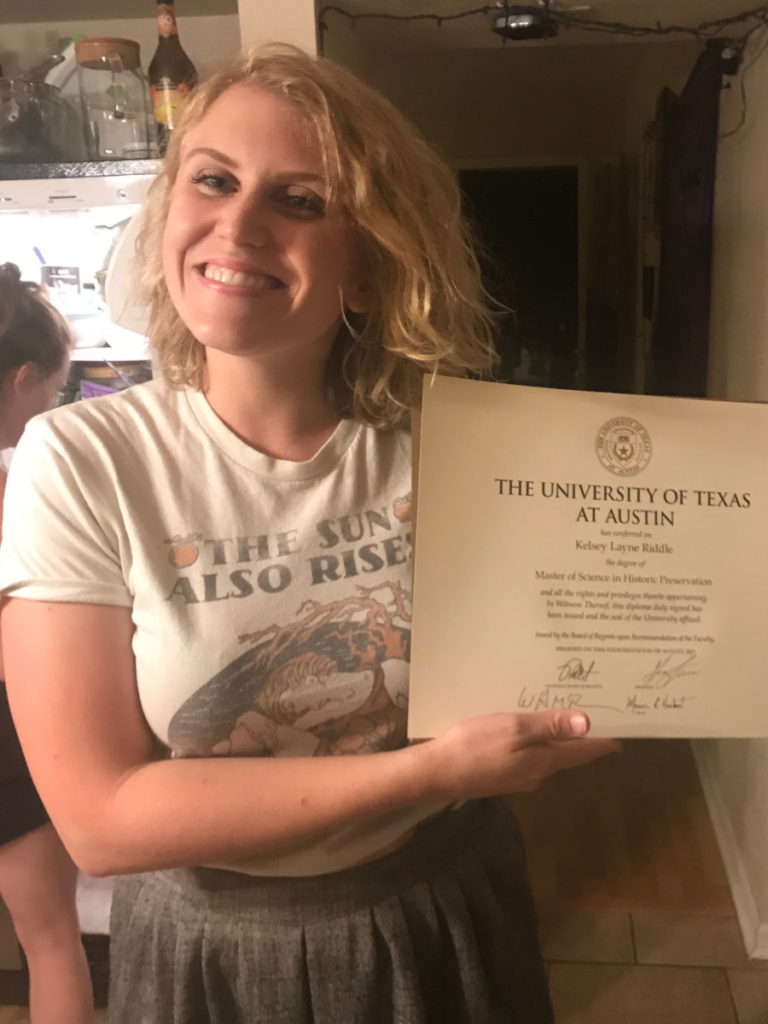
I’m a historian. I have a master’s degree in historic preservation. I work with buildings and objects.
I co-own a vintage furniture store with my sister. We mostly sell online and that’s really fun.
I’m also a writer. I do some work with The Patient Story. I’ve done some comedy writing in the past with different outlets like CollegeHumor and dabbled in stand-up a little bit.
I have a lot of jobs. I’ve also been an architectural historian. I do survey work and things like that.
The doctor comes in and he just turns ashen-faced immediately when he feels my neck. He leaves and I know something’s up.
What were the first symptoms?
It was August 2017. I was finishing up my master’s degree at the University of Texas. I was spending all summer writing my thesis, super exhausted, stressed out, [and] not feeling too great. I was having a lot of allergies. If you’ve been to Austin, you probably had some flare-ups so it’s not uncommon.
I had a lymph node that started growing on the back of my neck, about the size of a quarter. I went to my primary care doctor to get some routine medications filled and was like, “By the way, I got this thing. Probably nothing.”
I’m kind of a natural hypochondriac. I trained myself to be the opposite. I was like, “It’s probably nothing,” and they got me some antibiotics.
It didn’t do anything so I came back. Another round of antibiotics didn’t do anything. My primary care doctor said, “If this [lymph node] wasn’t moving, I would be worried this was cancer.”
When I went back for the last time and it hadn’t done anything, they referred me to an ENT. They had me do some blood work, which came up clear essentially and I did a little celebration. I went to the ENT and he prescribed me more antibiotics.
When I went for my follow-up, I had this lymph node — my supraclavicular lymph node on my right side — grow to about the size of an egg, literally overnight.
I went in [and] I remember I had no air conditioner in my car. It’s Austin in August. I’m melting. The nurses are like, “Oh, you poor thing.”
The doctor comes in and he just turns ashen-faced immediately when he feels my neck. He leaves and I know something’s up when the nurse comes in and hands me an ice-cold bottle of water. She’s like, “I figured you’re hot.”
My doctor came back in and he was very concerned. He said, “I want to do a needle biopsy.” It was just this moment. “Wait. What? Whoa, whoa. Where’s the antibiotics? Give me more of those.” Totally not on my radar.
Getting a biopsy
He did an ultrasound. He did the needle biopsy and it didn’t hurt at all. I said something along the lines of, “But aren’t cancerous lymph nodes not supposed to hurt? Because this one hurts pretty bad.” He was like, “Well, I just stuck a needle in it and you didn’t feel it.” I was like, “Oh.”
Then he was talking to me about results and when I’d get them. I just remember looking at him, “But tomorrow’s my birthday,” like that was going to make him not diagnose me with cancer. He looked at me and just went, “Uh, happy birthday…” like he was trying to be nice. He had no idea what to say. He’s fantastic but I’ll never forget the look.
The next morning, I woke up to a phone call from the nurse that they thought it looked like lymphoma and they wanted me to do a neck dissection biopsy.
It was horrible. I woke up on my birthday [to a] 9 a.m. phone call. I just sat there and bawled in my bed for a couple of hours [and] called my husband — or my fiancé at the time. My fiancé had called my two roommates and let them know what was going on.
When I walked out of the room, I just fell into their arms. It was very sweet. They’d gotten me [food] for my birthday. They tried to make it fun.
I remember thinking, “This is actually a relief,” because lymphomas are typically pretty treatable. I remember that was part of it.
I’m a hyper-paranoid person. I’ll just go down a rabbit hole. By the end of that night, I knew what every lymph node was called, what it drains to, and what it could possibly be. I knew that this one swelling was really, really not a good sign. He had told me he was thinking lymphoma would be the most common thing and that was what I really had dug into.

Honestly, that’s such an anxiety-inducing time. The wait is the worst.
Diagnosis
Did you have anxiety waiting for results?
Yeah, it was horrible. Honestly, that’s such an anxiety-inducing time. The wait is the worst. Not the worst in terms of how you’re feeling but emotionally it’s horrible.
It took them a really long time to get me diagnosed. I went in for one surgery and it was inconclusive. Then I went in for another neck incision.
I was laying after in recovery. This nurse comes in and I learned my ENT was super adamant about getting a good sample. He made sure there were conclusive results before he woke me up.

I knew then.
Then there was the PET scan that would show the spread. When I think of some of the worst days in my life, the day I had that PET scan was just horrible because not only are you jacked up on a weird carb-free, caffeine-free diet, but you’re just sitting there while something is telling you how bad it’s going to be. I’ve never felt that way. It was horrible.
At that point, I had already been through so much analysis. I had been through so many different tests and still had tons to go before I could start chemo. I was just exhausted. My parents were there and they were emotionally exhausted.
Something about having a machine analyzing me for an hour or so and telling me my chances of living. It was just really difficult for me to handle. I remember they were putting me in the machine and that version of Despacito with Justin Bieber came on and I made them change the music for me. It was a big party song that summer. “Please turn this off.”
I remember leaving the PET scan upset and just collapsing in my dad’s truck and having an upsetting conversation with him. He was always the one that had the answers for me and he didn’t have them this time. It was just one of those things where I think we were just so emotionally exhausted that we just kind of collapsed.
Getting the official diagnosis
Once I was staged, it was just a matter of getting going. My anxiety was so much better. I think the worst part was knowing and then knowing what I had, but not how bad it was.
I had a friend recently with Hodgkin’s lymphoma and his was refractory. He’s fine now but it was a very scary ordeal. That was my only experience with lymphoma was his experience.
Once I was staged, after that it was just a matter of getting going. My anxiety was so much better.
Breaking the news
I told friends pretty much as soon as I knew because I don’t hide things very well and that’s huge. It’s not a little thing that I’m hiding. People were trying to see what I was doing for my birthday so people were already texting me a lot. I was filling people in.
Processing the diagnosis
I’m a go-getter. It was pretty much, “All right, let’s do it. Let’s get it over with.” That was kind of my immediate reaction.
Looking for an oncologist
Once I got a preliminary diagnosis, my ENT referred me to an oncologist in town [who] he refers a lot of people to [and] that he really liked. I was a little hesitant.
We live two and a half hours from Houston. We were close to MD Anderson. They were on my insurance and they had saved my grandmother’s life. We already had a relationship with them. I was pretty adamant about getting a second opinion there.
I know that with my diagnosis, it probably wasn’t necessary but I don’t regret going and getting that second opinion. I told my ENT that I was going to do that and he was like, “Yeah, you do what you need to do. I’ll just let you know that I have referred lots of people to this person. I had a really good friend who went to MD Anderson and then came back and ended up sticking with this person because they just liked his bedside manner so much more.” I was like, “Okay,” and that is what actually happened.
He was a really fantastic doctor who was really optimistic and very, very knowledgeable and listened to me. My doctor at MD Anderson, while brilliant and lovely, just felt very impersonal. I don’t really feel like I got much out of that. I did end up doing my radiation there, which I don’t regret at all.
I came back to Austin after I got my second opinion and stuck with [the] doctor that I originally had seen. He is the doctor I still go back [to] for my checkups.
When someone is in charge of saving your life, you want them to actually care about your life and find it interesting and important.

Importance of a good patient-doctor relationship
I wanted someone that was willing to answer my questions and actually take time with me. But also I think that the thing that still draws me to this doctor or any doctor I’ve had is interest in me as a person. When someone is in charge of saving your life, you want them to actually care about your life and find it interesting and important.
Like I said, MD Anderson, lovely doctors, lovely researcher, but she didn’t care what I do for a living. She didn’t care about me at all.
My doctor knows me very well and all the nurses and everyone there knows me very well. I think, for me, that was really important because it made me feel like they would actually respond to my concerns because I wasn’t just another test in a tube or something.
I went to Texas Oncology. They have lots of different branches in Texas. There was one that was about five minutes from my house, which is great. It rocks.

Treatment
ABVD chemotherapy
I started ABVD in November. September 22nd was the day I got diagnosed. That was my birthday. I didn’t start until right before Thanksgiving. It was a two-month wait until my first round.
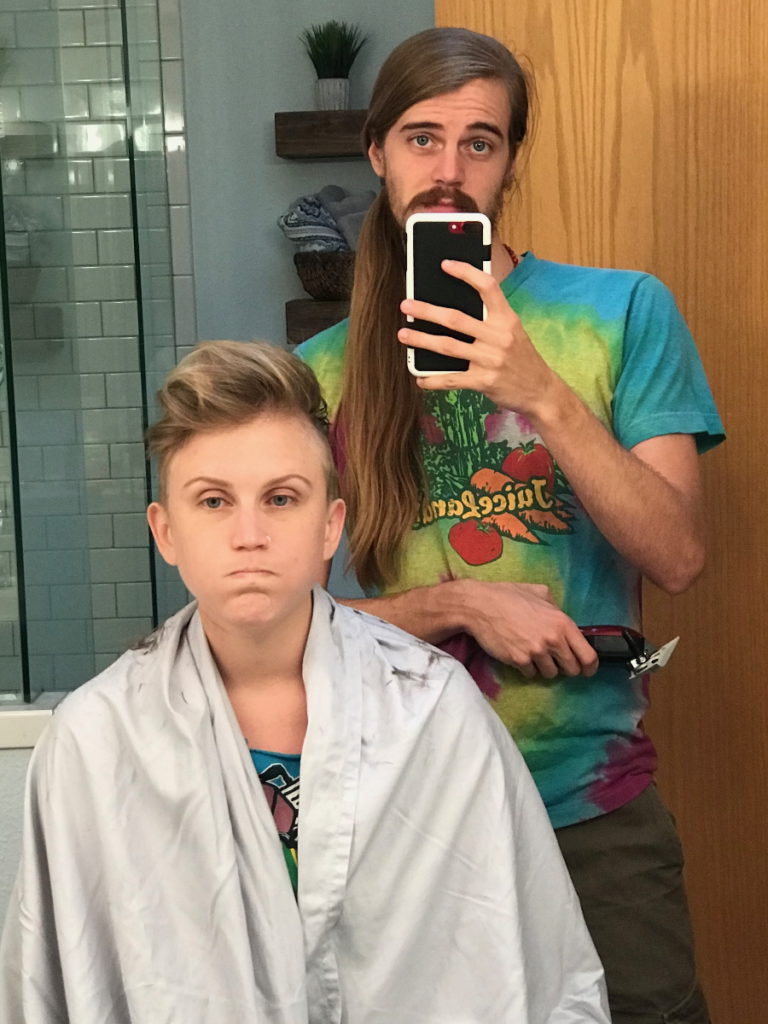
My first round, I was terrified, obviously. I started feeling improvement [in] my symptoms almost immediately. I was really lucky that I didn’t have an allergic reaction or anything to the chemo itself. My initial reaction was pretty mild. I lost a little hair. I ended up shaving it anyway after that.
I was mildly sick but my itchy legs resolved immediately. I think that that was also possibly because my immune system was being repressed. It was very crazy. I immediately felt better after my first round.

Side effects from chemotherapy
Hair loss
It was surprisingly not that emotional for me. I’d always had really long hair. The year before that, I had just chopped it all into a really short bob. I’d already made that leap and then when I found out I was going to lose my hair, I started dyeing it weird colors, having fun with it, and cut it into this really cute super, super short cut that I would never just do on my own.
After my first round, [my hair] was starting to fall out so I shaved it. I had fun with it. I don’t want to be bald again. I don’t think it’s a good look for me but I wasn’t super torn up about it.
My mom actually owns a wig shop. She owns a store that sells wigs and breast prostheses and bras for breast cancer patients since the 90s. I’ve been around wigs my whole life so she hooked me up with a couple that I would wear sometimes. I was more au naturel. I was also in Austin in the winter and it wasn’t really that cold so it was fine.
Did your grandmother inspire your mom to open a wig shop?
My grandmother actually opened a store first when she was going through cancer. She ran a hair salon and beauty supply store. She always sold wigs in Joplin, Missouri.
Whenever she started going through cancer, she realized there was nowhere for her to get breast forms — she had a double mastectomy — or bras or anything that wasn’t in a weird medical facility with dudes running it. She started selling those things. She became one of the only providers in the region for that.
Then, I believe, in 1997, she helped my mom open a similar store in northwest Arkansas, which is about an hour away. It was very successful.
Nausea
I got a list — I’m sure most people do — that’s about 20 pills long of, “If this doesn’t work, move here. If this doesn’t work, move here.” I was very on top of my anti-nausea meds. I think I had [Dexamethasone]. I had steroids. I had Olanzapine, which I didn’t like what it did to my head but it was so good. I had almost no nausea. It was actually pretty incredible.

[Olanzapine] made me feel really paranoid. I took a lot of Lorazepam for nausea, that was one of the main ones.
I had a friend send me some cartridges of medical marijuana from L.A. That made me such an advocate for medical marijuana. I was never anti-marijuana but when I’m taking this at a particular dosage for a particular reason, this cut through four different anti-nausea meds that I usually take, which are really messing with my head. It became one of those things where I was able to cut out certain meds just by substituting that. It was honestly pretty incredible.
He did it without asking me because he didn’t want me to be liable for anything. It showed up. I was like, “Okay. I’ll give it a shot.”
Neutropenia
After my first round, I went in for my second infusion and they did all the blood work. They were like, “Whew, that really knocked out your white blood cells.”
They were telling me that neutropenia is pretty common in Hodgkin’s Lymphoma patients, which weirdly went against what the MD Anderson doctor told me. But that was my experience, that it was common.
I had a really low white blood cell count the whole time and they could not give me Neulasta to up my white blood cell count because it would interact negatively with the Bleomycin — the B in ABVD — so I couldn’t have that. I just had to live with it. I was just careful and it was fine up until Christmas.
About halfway through my infusions, I got pneumonia and ended up in the hospital for almost a week in Arkansas. It was the lowest point in my cancer treatment. There was a man in the room next to me that was screaming in pain the whole time. And it was a really bad flu season. It was just very scary. It was horrible.
It made the whole ordeal way less scary once I was able to have some protection against infection.

Reading up on Bleomycin
When I got back to Austin, I had read a bunch of studies and research because that’s the kind of person I am. I had read something about how people who were going through a certain amount of rounds, which was slightly more than mine. If after two cycles they had no evidence of disease — which I had at that point, I had a clear PET scan, which was awesome — then you could remove the Bleomycin for the remainder to lower that toxicity because it’s very bad for your lungs.
I still have scars on my wrists from when I scratched myself when I was on it, like on my arms. The Bleomycin made me scar so easily. I just did it [lightly but] it would leave a permanent scar. [Then I thought,] “What’s it doing to my lungs? I don’t like this at all.”
I took that study to my doctor and said, “I know that I’m on fewer cycles but in this study, after two cycles they were able to remove the Bleomycin. Would I be able to do that so that I could take the Neulasta? I feel like my risk of ending up in the hospital again is more dangerous at this point than my risk of relapsing or having refractory disease from not being in the clear.” He agreed with me. He was very familiar with the study and he was like, “Yeah, I think that actually makes a lot of sense. We can do that.”
They removed the Bleomycin for my last two or three cycles and I was able to have the Neulasta. It upped my [blood count] really well and it was such a huge relief the rest of the time. It made the whole ordeal way less scary once I was able to have some protection against infection.
Do you think about what would’ve happened if the Bleomycin hadn’t been taken out?
I could have ended up in a worse situation in the hospital again because the infection I was in there for was not that bad. I was still there for a week. I think about my lungs. I don’t have any scarring and my lung capacity is fine so I’m really, really grateful for that.
The hospital was just such a wake-up call and I wanted to do everything I could to minimize side effects down the road. That was just really, really important to me.
Feeling vulnerable to infection
Most people got a taste of it during the beginning of the pandemic when we were all like, “Lysol everything. You can’t touch anything.”
I remember we were driving back to Austin after this hospital ordeal and my dad was sanitizing the McDonald’s cup that he went inside and got for me. It was like a containment chamber. He’s a little protective but that’s how it felt. It just felt like every single thing was a danger to me. I had to insulate myself in this little bubble.
It was also really scary. I was living with two roommates but they were really, really good about it, making sure they weren’t bringing stuff in the house or just letting random people come over, especially during flu season. But I think if they hadn’t been, I can’t control them. I’ve heard plenty of people have stories like this, so very similar.
Did having a friend who had refractory Hodgkin’s lymphoma impact the way you thought about treatment?
I didn’t think that because I don’t think that there was anything that the doctors could have done differently with his initial treatment. He had very bulky lymphoma in his chest and it was responding. Then the last couple of scans, it just stopped responding. He had a stem cell transplant. He’s doing great now, has a new baby, and life is wonderful. I’m really, really happy for him.
At the time, it wasn’t as much with the treatment. It was funny because I was talking to him when I first got diagnosed. He was already a couple of years past it and he was like, “You know, it’s weird. You eventually just stop thinking about it.” I was like, “No, there’s literally no way. I’m never going to not be thinking about this treatment.”
I was surprised that he hadn’t really done much research. He just let the doctors do what they wanted. For me, there is a point where I need to stop trying to fix the problem and let things ride because there is only so much you can do.
At first, it was, “Oh yeah, I’ll be fine, it’s Hodgkin’s.” All of a sudden, you’re in this very, very serious situation. My brain, of course, was like, “Well, what’s going to happen to me?” [That] was not good for my anxiety.

Advocating for yourself
I think that it’s hard to understand where the line is between complete holistic lunacy and advocating for yourself and knowing your body. In one vein, people are scared to introduce holistic medicine into their lives because they’re scared that that’s going to be the same thing as completely rejecting treatment, which I don’t agree with. But also I think that people get a little scared of advocating for themselves and looking at their treatment options.
Also, it’s one of those things where if you don’t have an interest in stuff like this in general, it’s hard. I have a big interest in academic studies. I read these kinds of things when I am curious about something. If this isn’t something you are already looking for, it might not even be something you think about. Maybe I can see what new research is out there that my doctor maybe hasn’t seen. When I brought this up, he said, “We literally just talked about this in a conference I just went to. This is a new study.” That was cool.
Don’t feel like you’re stuck with this situation of someone not listening to you advocate for yourself.

If you really feel strongly about something, at least bring it up to your doctor. Don’t be scared to ask them questions. If you have a doctor who is making you feel stupid or ridiculous for asking these questions and you have the ability to find a new doctor, find a new doctor because you do not have to deal with that.
I have actually told more than one person who has a doctor who won’t listen to anything that they’re saying or talks to them like they’re stupid or a child, “See if your practice has another doctor.” One girl I know did switch doctors and had a way better experience with her new one. Mine listened to me and was really great but don’t feel like you’re stuck with this situation of someone not listening to you advocate for yourself.
I do think that I’m coming at this from a place of privilege, of someone who knew what to look for in studies and had access. I was still in grad school. I had access to academic journals. It’s hard for me to say everyone needs to go do that but definitely ask for help because there are people who know a lot about this that can help advocate for you as well. I had just graduated in August. My access was still working for the rest of the year so I was able to do that.
With self-advocacy, it’s so difficult to talk about because I came from a place of such privilege. I grew up with a mom and a grandmother who knew how to navigate the system and it was still really difficult. You can talk to the social worker at the hospital and just say, “I don’t know this but this is what I’m trying to do.” People can help.
Taking a more active role in your care
I had grown up watching my mom and grandmother fight with insurance, fight with doctors, fight with billing, [and] fight with patients sometimes depending on the situation. I grew up watching my grandmother go through [a] very long and intense treatment regimen where her cancer had come back a couple of times. She really had to advocate for herself. There wasn’t any foundation or anyone. She started all of that in her town. She really had to advocate for herself. She was just so determined to survive even though her prognosis was really, really bad. I’m not saying that that’s the reason she survived because I don’t want to put that on anything. She dug it up. She made the phone calls she needed to make. She figured out who she needed to talk to. And watching her go through that…
I am the kind of person that I think my normal personality would be to listen to the doctor and be like, “Okay, yeah, you know best.” But because I’ve watched my mom and my grandmother go through that…
Ask for early results. I’ve gotten so lucky. If you’re a young cancer patient and you’re in a place where there aren’t a lot of young cancer patients, you get some special treatment. I’m not going to lie. They will rush things for you. Ask for your results the second they come in. Tell them you’re really worried. Make it very clear to them.
Build a relationship with your nurse, especially. That’s all stuff that has helped me get where I need to be. I’ve never been nasty and I’ve never had to because people do really want to help. They’re just overwhelmed as well.
No evidence of disease
Dealing with scanxiety
I get nervous about scans. Now, I’m almost five years out and I’m not worried about it anymore. But for probably three years, about a week before each scan, I just wanted to vomit. I already have very bad anxiety. I was always a hypochondriac. It was one of those things where I was proven right, my hypochondria was.
I just was really scared every single time. I would just go into this darkness for two weeks.
I definitely got much more in touch with spiritual stuff and self-awareness during cancer. I think that was a big part of it because you’re just so in your head all the time and you have to be. One thing that did make me feel better was not doing the insane research I’m always doing because that’s an anxious tic I have. It’s not a good thing all the time.
My husband would be like, “No, put the phone down.” My dad is the same way. I’d call him and be like, “Dad, I know what you’re doing. You need to put the phone down. You’re looking at articles right now.” He would say, “Okay, you have to put the phone down too.”
We would both be doomscrolling about what if it comes back. What if it doesn’t clear out the first time? What are my options then? What are other people’s stories?

I was way more worried about letting the cancer progress. If I had seen that there was a really high chance that I would lose fertility, I would have probably frozen my eggs but I chose not to do that.

Fertility treatment
My doctor encouraged me to look into freezing my eggs. I did the research and looked into it. At that point, I was so ready to get treatment going because it would delay my treatment another few weeks.
The research showed me that ABVD is not super toxic. I found that most people were generally fine after the course of treatment that I would have. If I were to go on to a stem cell transplant, I think I would have definitely considered those options.
I decided it honestly just wasn’t worth it for me because I wanted to get going on treatment. I was way more worried about letting the cancer progress. If I had seen that there was a really high chance that I would lose fertility, I would have probably frozen my eggs but I chose not to do that.
It’s really hard because I was surprised that the doctors were all like, “You really need to look into this.” Because to me, I was just like, “Just get on with the treatment. I don’t want to die.”
I was 26 and I wasn’t quite at the point where I was thinking about the immediate reality of having kids. I’m about to be 31 now and if I were diagnosed, I think that it would be something I would consider way more intensely. But at the time, I couldn’t even see past tomorrow, let alone a future with kids.
I remember coming out of one of my surgeries for the biopsy. One of the nurses was telling me about her friend who’d had Hodgkin’s and has all these kids now and how it’s great. I’m like, “I don’t care. Good, good for her.” At that point, I was just so concerned about I have cancer.
I’d seen that my chances of remaining fertile were pretty high. If it had been different, I would have probably felt differently about it.
Self-discovery during cancer
Getting into fashion and style
I got way more into fashion and style and expressing myself through that when I was sick. I always enjoyed dressing [in] different ways but not every day. If I were going to a grocery store, I’d always be in shorts and a T-shirt. I wasn’t thinking about it and I still do that.
During cancer, it became one of those things where okay, I’ve lost my hair and losing my eyebrows. I’m gaining weight. I’m kind of puffy. I’m not healthy looking. I want to be able to present myself still.
I started doing my makeup every day and buying a lot more clothes. At first, it was a little bit [of] I want to feel healthier. Then it just became fun.
I took a photo every time I was at the doctor’s office. I would take my little fashion selfie because I had all these really fun outfits. I bought a lot of new, looser, comfortable clothes for chemo. I had this flowy, bohemian thing going.
Everyone would always comment on my style when I walked in and that made me feel really young. That was fun.
It helped me see past the blandness of my everyday surroundings like hospitals and my room in a time [when] I was feeling very numb because of medication. You’re dealing with a lot of anxiety and stress. I was feeling very numb in terms of who I was.
I felt like I didn’t belong to myself. I felt like I belonged to the doctors and to the people who are worried about me. My body was not mine at all. The self-expression came from trying crazy makeup colors and different clothes that allowed me to reclaim my body a little bit.
Re-establishing your identity
That’s exactly how you feel. You’re no longer you. You’re a cancer patient. I’d gone from being this young graduate student who worked in nightclubs on the weekends, worked at a rock poster museum, went out a ton, and did all this cool stuff to someone who was inside all the time and living at the hospital.
It wasn’t even so much of this is Kelsey. It was more of this is mine. This is something I can control. Not necessarily projecting this thing about myself to other people but more of projecting that I am here to other people. I’m making myself really visible [at] a time [when] my natural instinct is to really try to make myself invisible because I don’t like the way I look and I don’t feel good.
There was so much attention on me all the time at this point. I was someone that never had a ton of attention on me. I wasn’t someone that was big and loud and stuck out. I always went with the flow and blended in. All of a sudden, I’m walking down the street, bald… You’re going to notice the bald girl walking down the street.
It was one of those things where I was like I’m going to try all the crazy stuff I’ve always wanted to try but been too scared to. I already look like this and I’m going to reclaim the space for myself. It’s something that has stuck with me.
Honestly, I am not glad that I had cancer but I’m glad I had this experience and this awakening because I don’t think my life would be as colorful as it is now.

Getting into comedy
I had always been really into standup comedy. I’d done improv a little bit before grad school with this theater in town. I was just too scared to try standup, as many people are. I already had really bad stage fright.
I’d been writing but one day, I just sat down and was just feeling a lot of emotions but didn’t know how to get them out. I sat in my room, took a little yellow pad, and just wrote 20 pages. I wrote from start to finish everything I had experienced with cancer. I forced myself to go really deep into the parts that were really painful to think about.
Out of that came a lot of really funny stuff that made me laugh, came out of these very serious pages. I was able to put together a little standup set. I was on so many meds and on my anti-anxiety meds for my nausea. I was like, “Screw it. I’m going up.” I just started doing standup and I got really, really into it pretty quickly.
I was getting booked on shows and doing shows a little bit outside of town, going to San Antonio. I connected with a comedian who is a cancer patient as well in San Antonio, who runs a lot of shows, [and] who connected me to some really cool stuff. It was just tons of fun and I did that up until right before the pandemic.
I haven’t gone back because part of me associates it with that time. A lot of my jokes were about cancer. I am trying to re-negotiate my identity and my relationship with that. But that did launch me into screenwriting and humor writing, which I do with fervor now. I do it all the time and I really, really love it so that was very important.
I always joke it was the steroid-induced mania because I would get out of chemo, be on all these steroids, be on all these meds, and I’d be like, “I got to do something!” You got to do something. You feel really, really weird.
You get up there and you don’t care if people are throwing rocks at you because you will get crickets like 50% of the time when you start. It was just something. I don’t want to say it was all the meds or anything like that. It was a combination of just being in a place in my life where I was like whatever. What else am I going to do? I don’t even care anymore. I’m just going to do it.
It’s taken me a long time to deal with the fear and the emotions I was feeling then because you really do push a lot aside and just go into survivor mode.
Survivorship
What does it mean to you?
I’m still trying to discover what it means because I think I’m at the point now where I don’t think about it every day. Then when I remember it, that scares me a little because I’m like, “Whoa, that was me.” That was such a big part of who I am now.
It is single-handedly the most important thing that’s ever happened in my entire life. Good and bad but mostly good, honestly, in terms of what I’m doing with my life now. But also, it’s taken me a long time to deal with the fear and the emotions I was feeling then because you really do push a lot aside and just go into survivor mode. I’m still dealing with a lot of that.
The biggest, most important realization I’ve had in terms of survivorship is realizing that if my cancer comes back, I don’t know what’s going to happen. I am not automatically the same person I was when I got it the first time. It doesn’t erase any of the progress or changes I’ve made in my life. It doesn’t erase who I am. I’m a different person now and it’ll be a different experience.
Even if something happened or I had a bad prognosis, living with cancer, in terms of the everyday, is not something that you can be constantly mourning. Because right now, this very moment, I could have some horrible disease that’s going to kill me tomorrow but I don’t know that. I’m still just living life like this every day. The only difference is whether or not you’re panicking about it or not.

That’s easy for me to say now, but it’s just something I think about a lot because I do fear it coming back and in my mind, that would erase all the beautiful things that are in my life now. But I know that that’s not true and that there are a lot of people that live with chronic cancer that live beautiful lives. Cancer patients aren’t just zombies walking down the hospital hall. That’s not what we are.

Inspired by Kelsey's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)