Nicole’s Stage 4 Classical Hodgkin’s Lymphoma Story
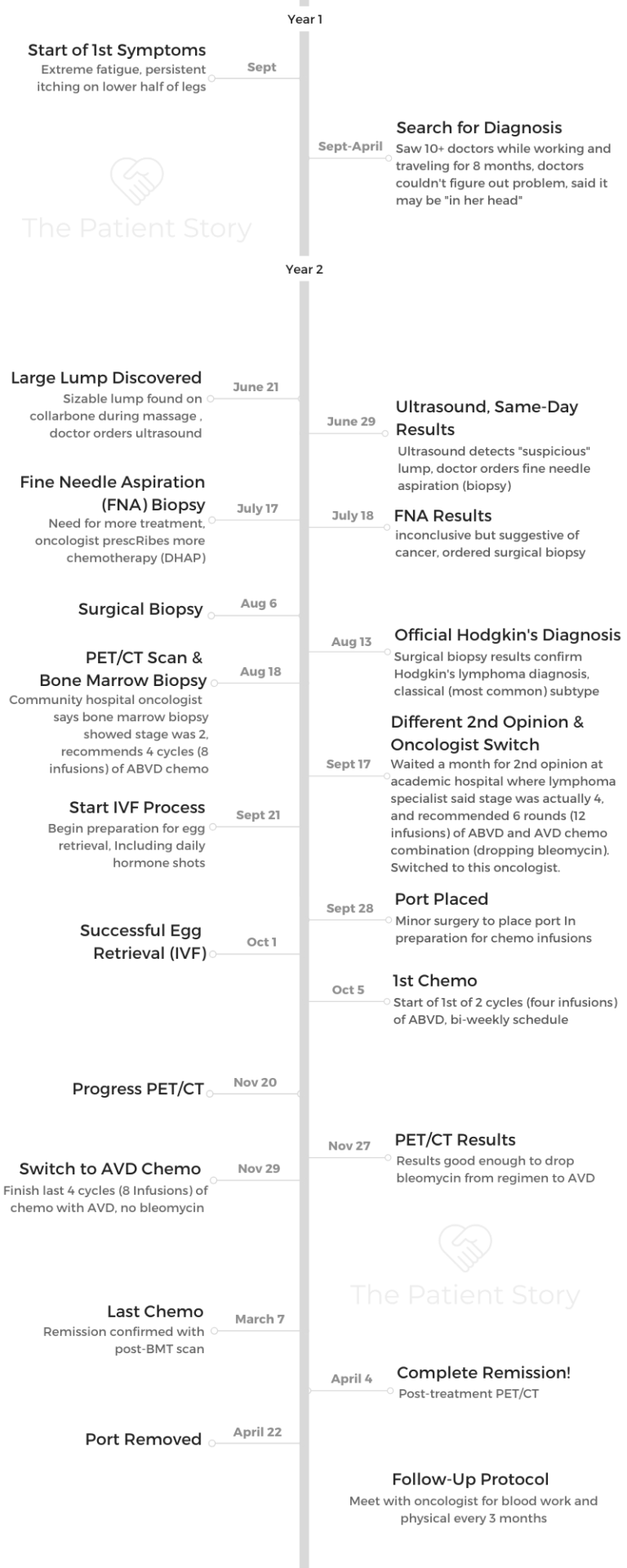
Nicole shares her stage 4 Hodgkin’s lymphoma story, one that began with 8 months of no diagnosis and her determination to self-advocate for answers. She describes undergoing chemotherapy — ABVD then dropping bleomycin to AVD — and managing through side effects.
In her story, Nicole also highlights how a second opinion changed the course of her treatment, turning to integrative medicine to fight side effects and taking care of her mental health.

- Name: Nicole M.
- Diagnosis (DX):
- Hodgkin’s lymphoma
- Stage 4
- Age at DX: 26
- 1st Symptoms:
- Extreme fatigue
- Persistent itching on lower half of legs
- Treatment:
- 1st Symptoms & Search for Answers
- The Path to Diagnosis
- Describe the ultrasound
- Describe the fine need aspiration (biopsy)
- Next steps: surgical biopsy
- How did you get the initial cancer diagnosis?
- A family of medical experts
- Describe the surgical biopsy
- When did you get the full, official cancer diagnosis?
- How did you process the Hodgkin's lymphoma diagnosis?
- How did you break the news to loved ones?
- Treatment Decisions
- Chemotherapy and Side Effects
- Integrative Medicine Practices
- Turning to holistic treatment for side effects
- What was the plan the integrative medicine doctor gave you?
- Describe the personalized nutrition plan
- Acupuncture for fighting nausea
- The mind-body connection
- Using guided imagery
- Additional holistic practices are part of your routine
- What was your follow-up protocol?
- Hair Loss
- Quality of Life Reflections
- Describe how you approached fertility preservation
- Describe the IVF egg freezing process
- Were there moments you had to advocate for yourself?
- Taking care of your mental health
- How important was it having caregivers?
- Were you able to keep working through treatment?
- How has it been navigating survivorship post-treatment?
- What's your last message to other patients and caregivers?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Symptoms & Search for Answers
How did you know something was wrong?
It was September, and I had begun a 4-month trip in which I planned to travel through Europe before settling in Rishikesh, India, to volunteer for 3 months.
My first symptom began as a slight itch on the lower half of my legs and feet. After just a few weeks, the itching grew more intense. Following the advice of numerous doctors and pharmacists, I treated it with over-the-counter topicals, but nothing seemed to work.
By month 2, the itching was almost unbearable. It kept me up all night and consumed me during the day. I was desperate for relief. I visited a local doctor, who performed a thorough examination and ordered numerous blood tests.
He ultimately attributed the itching to scabies, for which he prescribed me the gold standard treatment.
Unfortunately, no matter how many times I applied this harsh medication, the itching remained. It wasn’t scabies.
You turned to holistic medicine for answers
Frustrated that I had no answers, I decided to pursue holistic medicine options. I was in Rishikesh, after all, also known as “the yoga capital of the world.”
I worked with a yoga teacher, met with a healer and tried various ayurvedic practices on a weekly basis. I learned a lot about holistic treatments during this time, but unfortunately, nothing worked to rid me of my discomfort. I was miserable.

The search for answers
Upon returning home from the trip, I immediately dove into the daunting task of searching for a diagnosis. I visited at least 10 different doctors and specialists, sought advice from friends and family in the medical profession, and spent an inordinate amount of time researching my symptoms on the internet.
I prepared a thorough 3-page document listing all of my symptoms, the timeline of their onsets, and included photo evidence of everything visible. I brought this document with me to every appointment, hoping that if I could provide the practitioner with enough information, they would be able to diagnose me.
Unfortunately, after countless appointments and being told repeatedly that I was fine, I was still without a diagnosis. I was crushed and discouraged.
I finally gave up my search after one specialist told me that my symptoms were likely in my head. I decided instead to shift my focus to learning how to live with my symptoms.
In an effort to move on with my life, I accepted a temporary work opportunity in Tulum, Mexico, where I planned to spend my free time pursuing a healthier lifestyle that I hoped would help me to cope with my symptoms.
After a couple of months in Tulum, I went for a deep tissue massage. It was after this manipulation that a massive bump surfaced near my clavicle. It was alarming and prompted me to immediately book a flight home and schedule another visit with my primary care physician.
Describe the visit with your primary care physican
Upon meeting with him, it was clear that he was concerned. He informed me that the bump was actually a lymph node, and he said that he could feel at least 2 masses.
His tone had changed drastically since the last time I had seen him. It was during this appointment that I finally felt heard by a doctor and validated in my concern for my symptoms.
It was here that I realized the importance of becoming my own fiercest advocate.
I finally understood the hands-on role I would need to assume in my own diagnosis, which began with vowing to never silence my body or my instincts again. It wasn’t all in my head; something was very wrong.
The Path to Diagnosis
Describe the ultrasound
The first test ordered by my primary care doctor was an ultrasound of my lymph nodes. This was a quick and easy procedure, and to my surprise, I got my results back the same day.
Unfortunately, I still didn’t have any answers. Rather, these “results” indicated that I would need to undergo a fine needle biopsy of the largest clavicular lymph node.
Describe the fine need aspiration (biopsy)
This procedure was also quick, but not as easy as the ultrasound. It was more painful than I had expected, and it took the technician multiple attempts to get a good sample. The area was sore for 4 to 5 days.
Before I left the appointment, I was told I would receive my results in a week. This timing was perfect because I had a 1-week vacation to Cabo San Lucas scheduled for the next day and was looking forward to a break from this stressful experience.
However, before boarding my flight, I received a call from my doctor informing me that the results of the needle biopsy were inconclusive but indicative of a “more serious issue.”

Next steps: surgical biopsy
He urged me to schedule a surgical biopsy as quickly as possible. I pressed him for more information. He finally informed me that the results indicated that it could be cancerous, but that I would need a surgical biopsy to know for sure.
Hearing this was shocking and terrifying. I immediately called to schedule a pre-op appointment with my surgeon. The earliest opening wasn’t for nearly 2 weeks, so I decided to still go on the trip with hopes that it would take my mind off of this uncertainty.
I didn’t feel that my doctor was being totally transparent with me, so I signed a medical release form before departing the country, which authorized my mother to pick up copies of my test results.
How did you get the initial cancer diagnosis?
3 days into my trip, I received a call from my mom. With my permission, she had shared my fine needle biopsy results with my uncle, a neurosurgeon.
His interpretation was less ambiguous than my doctor’s had been. “Uncle Barry says it’s Hodgkin’s lymphoma,” she told me over the phone. “He says you’ll definitely need the surgical biopsy for a full diagnosis of the subtype but that the pathology is pretty conclusive.”
That was how I learned that I had cancer. From my mother, while on vacation in Mexico.
A family of medical experts
To many people, this might seem like a strange way to find out that you have cancer, but it actually felt fitting to me, especially given my family’s history.
My grandfather was one of the top physicians of his time, and many of his children and their children went on to become doctors, too. My extended family includes a neurosurgeon, an oncologist, a radiologist, 2 psychiatrists, a general surgeon and 2 primary care physicians.
This was a huge blessing and gave me the invaluable advantage of always having someone capable and willing to double-check my doctors’ work. Their support was truly invaluable.
However, coming from a family of medical doctors also led to some harsh realizations. I learned rather quickly that doctors do not have all the answers. Yes, they may be in charge of your care, but they do not know everything about your cancer, about your treatment, about your body or even about the side effects you will inevitably face.
I was made painfully aware of this when neither my personal physicians nor my family members could answer many of my most pressing questions about my diagnosis:
- How did this happen?
- Why did this happen?
- How can I change my lifestyle to make sure it never happens again?
- What is the optimal diet to best support my recovery?
- Will acupuncture help?
- Will holistic medicine hurt?
My mind was reeling and full of unanswered questions. Realizing and accepting early on that doctors don’t know everything allowed me to take ownership of my healing journey and motivated me to seek my own answers, answers that would help me make sense of this nonsensical thing.
This mindset helped me tremendously throughout my treatment and further reinforced the need to be my own fiercest advocate.
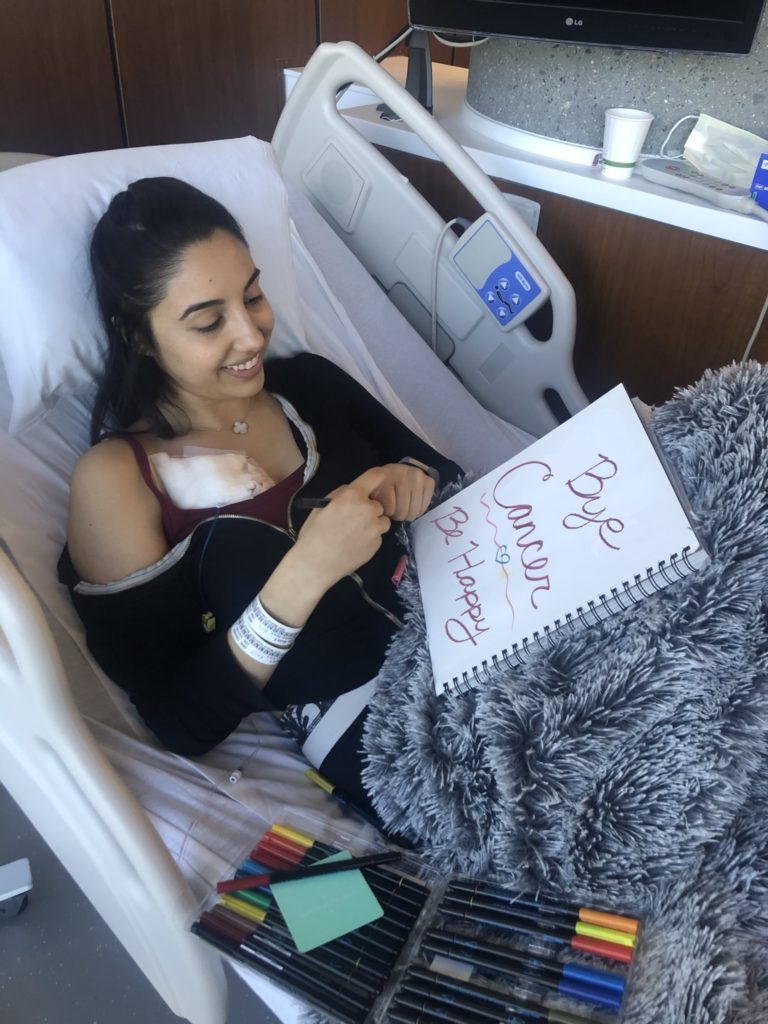
Describe the surgical biopsy
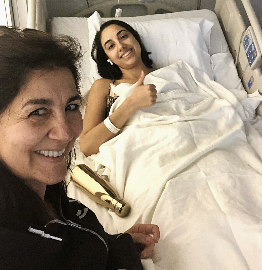
Upon returning from the trip, the days leading up to the surgical biopsy felt surreal. It was as though I was going through the motions of someone else’s life.
I was living in limbo and felt completely paralyzed from making any sort of forward progress.
When I arrived at the hospital on the day of the biopsy, I had a defeated mentality because I already knew what the outcome would be. During the biopsy, they removed an entire lymph node from my clavicle.
For the next 3 to 5 days, I slept about 18 to 20 hours every day — more than I had ever slept before. Removing that single lymph node resulted in a level of fatigue that I couldn’t have even imagined.
When did you get the full, official cancer diagnosis?
5 days after my surgical biopsy, on August 13, 2018, I received my official diagnosis: Classical Hodgkin’s lymphoma, nodular sclerosis subtype.
That same day, I got my first PET-CT scan in order to determine the stage of my disease.
How did you process the Hodgkin’s lymphoma diagnosis?
Initially, I was in complete and total shock. All I could bring myself to do was sit on the couch and watch reruns of the television show “Friends,” because my brain was unable to process how a healthy, active, 26-year-old like myself could suddenly develop cancer.
It certainly didn’t help that society’s interpretation of the word “cancer” is both dire and alarming. I quickly found myself questioning my mortality and all of my life choices.
Was there something I could have done to prevent this? It was all very overwhelming and felt like an impossible emotional mountain to climb, so I didn’t. I just sat on the couch and watched “Friends” until the shock wore off.
Surprisingly, there was also an element of relief. For 8 long months, I had been suffering from this intractable itching. It drove me crazy, adversely affected my mental health, and prevented me from living any type of normal life.
Not knowing what was wrong with me was much worse than knowing I had cancer. Because of that, I actually found gratitude from my diagnosis.
Yes, I had cancer, but at least my pain now had a name. At least no one thought it was all in my head. It was real, and it was treatable.
I realized that my circumstances could be worse in so many ways. With that profound realization and newly developed gratitude, I found hope.
How did you break the news to loved ones?
Breaking the news to all my loved ones was an extremely exhausting process, both emotionally and physically.
By the time I received my full diagnosis, fatigue had become a major symptom, and I found that each emotionally draining conversation I endured would physically exhaust me as well. I began the process of telling my loved ones but found that each conversation was more tiring than the last.
Repeating myself over and over, while simultaneously trying to address the fears and concerns of my loved ones, became extremely daunting. Eventually I realized that I needed to stop.
After the most important people knew, I shifted my approach to waiting to tell people whenever they happened to reach out to me. Surprisingly, this experience taught me a very important lesson in how to protect my energy.
The more I expended my limited energy on emotionally difficult conversations, the less I was able to conserve and utilize on my own internal healing.
I learned to honor my energy levels and the limitations that they presented.
Treatment Decisions
How did you decide where to get medical care?
Based on the recommendations of my doctor and surgeon, I met with a highly regarded oncologist who worked at a publicly-funded hospital in the suburb where I grew up.
During our first visit, after reviewing my PET/CT scan, she determined my cancer to be somewhere between stage 2 and stage 4. She explained that in order to get a definitive staging, I would need to complete a bone marrow biopsy. I agreed to the procedure right then and there in her office.
Describe the bone marrow biopsy
I underwent the most painful procedure I had ever experienced. She had certainly downplayed what I should expect, and I resented her a bit for that.
The good news was that results of the bone marrow biopsy came back negative, resulting in a stage 2 diagnosis.
What was the stage 2 treatment plan?
The oncologist then presented me with the following treatment plan:
- First, 4 rounds of ABVD chemotherapy
- Next, a PET-CT scan to determine if I had achieved remission
- Finally, possible radiation afterwards (depending on results of the PET-CT)
Did you get a second opinion?
I was quite thrilled with the stage 2 diagnosis and relatively short treatment plan laid out by the oncologist, because I was terrified of chemotherapy and wanted as little of it as possible.
However, it was very important to my family that I get a second opinion, so I used every resource available to me and was lucky enough to secure an appointment with one of the best local specialists.
Unfortunately, because he was in such high demand, his first available appointment was a month away. I decided to delay treatment and wait for the appointment because my research informed me that Hodgkin’s lymphoma is a slow-growing cancer and that a 1-month delay wasn’t cause for concern in a stage 2 case.
The diagnosis changed from stage 2 to stage 4
By the time the second opinion appointment arrived, I was feeling sicker than ever and eager to move the process along.
After his team reviewed all the same test results and scans ordered by my first oncologist, they definitively determined that I had stage 4 cancer.
This came as a huge shock. I found myself trying to argue my way into a stage 2 diagnosis, but the doctor remained firm. In his opinion, it was an absolute stage 4 despite the negative bone marrow biopsy, and his reasoning was thorough and well founded.
In fact, he believed that the bone marrow biopsy had been an unnecessary procedure altogether, and he apologized that I had to endure it. Stage 4 wasn’t what I expected or wanted to hear, but he was confident and firm in this diagnosis.
I now had 2 highly regarded oncologists offering me 2 very different paths. The new diagnosis was 2 stages higher, and the treatment plan was 2 months longer than that of the first oncologist.
Despite how badly I wanted to take the easier route, I didn’t. This was primarily due to the unique and dynamic treatment plan proposed during my second opinion appointment.
He wasn’t simply following the status quo of how most doctors treat Hodgkin’s lymphoma. The thoughtfulness of his plan made me more confident in what laid ahead, so I switched oncologists immediately.
Without a doubt, I believe that delaying my treatment by a month in order to get a second opinion was the best and most significant medical decision I made during my entire cancer journey.
Describe this different treatment plan
Regardless of staging, nearly every case of classical Hodgkin’s lymphoma is treated in the same way: the ABVD chemotherapy regimen and possible radiation, if necessary.
The ABVD regimen has been the standard first-line course of treatment for Hodgkin’s since the 1970s. Unfortunately, there have been few medical advancements made in the 40 years since then.
What impressed me about my new oncologist’s unique approach to this standard treatment was its dynamicity.
It involved a mid-treatment PET-CT scan to determine if it was possible to downgrade the chemo regimen from the classic ABVD to a less intense AVD, thereby dropping the “B” (bleomycin) after just one of the 6 cycles.
His reasons for using this approach were scientifically founded and backed by recent studies. Additionally, they were logical to me, the layman.
Bleomycin is one of those “nasty” chemo drugs that can have detrimental long-term effects on your lungs. The less of it your body has to endure, the better, and his treatment approach was very mindful of that.
He felt the same way about radiation and informed me that it was his intention to avoid using any radiation during treatment unless it was the last remaining option. It was clear to me that he was extremely knowledgeable about the negative effects of Hodgkin’s lymphoma treatments.
As such, his treatment plan balanced the important task of destroying the cancer cells with the additional goal of avoiding as many long-term chemo side effects as possible.
»MORE: Read more patient experiences with bleomycin
How was your medical team?
Unlike the first oncologist I met with, the one I ultimately chose worked at a university research hospital. Being a patient at a research hospital meant that my medical care team had expanded.
It wasn’t just me and my one doctor anymore. I now had an entire care team assigned to my case, which included my primary oncologist, an oncology fellow, a symptom nurse, a pharmacist and a psycho-oncologist.
The entire team was located in the same office, which also housed the chemo infusion center and the blood analysis laboratory. It was a one-stop shop, and the team-based approach gave it a much more collaborative feel than that of the publicly funded hospital.
Chemotherapy and Side Effects
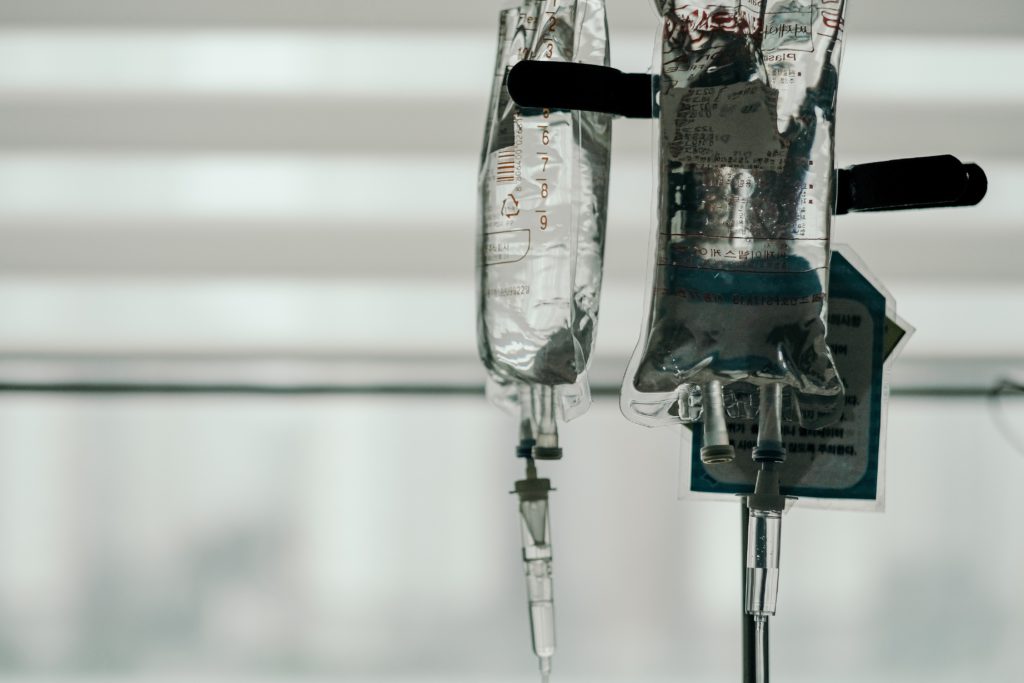
Describe getting the port pre-chemo
Having a port inserted in my chest was one of the pre-treatment procedures required by my oncologist. Initially, I tried to convince him otherwise, because I wanted to avoid any unnecessary procedures. My prior oncologist hadn’t required that I have one.
However, he explained that 6 months of chemotherapy involved a lot of IV insertions, and the small veins in my arms would likely become weak over time. I hesitantly agreed.
Inserting the port was a more difficult procedure than I was expecting, primarily because I was not fully sedated. Towards the end, the medications had worn off completely, and I was fully awake as the doctors applied a great amount of physical force to move the port into the correct position.
I was sore for 3 days following the procedure, and it took me several weeks to get used to having a foreign device under my skin.
With that said, over the next 6 months, I grew to genuinely appreciate my port.
I believe it made every individual experience at the infusion center more pleasant not only for me, but also for the nurses who were responsible for inserting my IVs.
Getting the port removed 8 months later was a very simple and painless procedure, not at all like the insertion procedure.
All in all, I would recommend getting a port or similar device for anyone facing a lengthy chemotherapy treatment.

Describe the ABVD and AVD chemo regimens
My first ABVD chemo infusion was on October 4th, nearly 2 months after my diagnosis. The plan was for me to undergo 6 cycles over 6 months, which totaled 12 individual infusions, 1 every 2 weeks.
My chemo day was Thursday. For the first 2 rounds, I received the ABVD chemo regimen. Then I did an interim PET-CT scan, which luckily showed that the treatment was making enough progress to downgrade my ABVD regimen to an AVD regimen for the last 8 infusions.
»MORE: Read our comprehensive ABVD chemotherapy info page
What were the cycles like?
In the beginning, I didn’t know what to expect, and Google was no help. I approached the situation feeling unprepared and emotionally unstable.
However, the first infusion surprised me in a couple significant ways. First, I was shocked to realize that the itching symptom, which had been tormenting me for 13 long months, was suddenly gone. It disappeared that quickly, after just 1 infusion.
Experiencing this relief helped shift my perspective from ‘chemo is poison’ to ‘chemo is medicine’ for the first time.
The second surprise was that I didn’t feel the effects of chemo right away. Upon returning from the first 6-hour infusion day, I felt tired and a little nauseous, but I was otherwise okay.
However, this didn’t last long. The next morning, I could feel the side effects getting worse, and I was overwhelmed with nausea and other discomforts. These side effects continued to worsen in the days following.
Eventually, the side effects peaked about 3 to 4 days after the infusion and then progressively got better. About a week after each infusion, I would wake up feeling ‘recovered,’ which I referred to as ‘climbing out of my chemo hole.’
It was the best part of every round because it left me with approximately 7 blissful days of feeling “normal” before the next round began

What were all the different side effects you felt?
My side effects came in waves and got progressively worse over time. My primary side effects were:
- Extreme nausea
- Stomach pains
- Fatigue
- Sensitivity to light
- Shortness of breath
- Strong aversions to certain smells
- Mouth sores
- Disorienting dizziness
How did you combat the side effects?
After the first infusion, I began to experience extreme nausea, stomach pains, fatigue and sensitivity to light. I combatted the nausea with acupuncture and by preventatively taking anti-nausea medications around the clock, before the nausea even began.
I decreased the stomach pains by following a strict diet and supplement plan. I addressed the fatigue by sleeping as much as possible. I dealt with the sensitivity to light by wearing extremely dark oversized sunglasses whenever light caused me discomfort, including inside.
»MORE: Read other cancer patient experiences with chemotherapy
By the second infusion, I was immunocompromised, which means that my immune system was compromised. I had to be extremely careful not to catch a cold or flu, because my immune system did not have the strength to fight off even the tamest of invaders.
I protected myself by wearing masks in public, applying hand sanitizer regularly, and limiting the number of people I came into contact with. I also developed shortness of breath, which was likely caused by the bleomycin.
By the third infusion, I was experiencing a nauseating metallic taste in my mouth and had developed an extreme aversion to certain smells. I sucked on ice cubes and sniffed essential oils to combat these discomforts.
I also developed a strong aversion to saline, which is the fluid the doctors inject patients with every time they insert an IV prior to starting a round of chemotherapy.
Though most people can never taste or smell saline, the aversion made me feel instantly nauseous every time I was injected with it. Strangely, I could even taste it in my mouth as it was being injected into my port.
Sniffing essential oils while the saline was being injected helped tremendously with this, although initially I made the huge mistake of only using one scent, lavender. Because of this, I slowly developed an aversion to lavender.
Even to this day, too much lavender can make me feel nauseous. After developing the lavender aversion, I realized that rotating essential oils was the best way to handle the saline aversion so that I wouldn’t develop any more new aversions in its place.
By the fourth infusion, I was experiencing mouth sores and had begun to feel dizzy whenever I stood up too quickly.
Following my dentist’s instructions, I used Biotene mouthwash for the sores and switched to a dentist-prescribed sodium fluoride toothpaste.
As for the dizzy feeling, I simply had to learn to get up very slowly. The more mindfully I moved, the less disoriented I felt. The yoga, meditation and breathwork practices helped me tremendously with this.

Did the cycles get better or worse?
By the end of the first 2 infusions, or the first cycle, I began to notice a pattern occurring in each 14-day round. Every round seemed to be similar, though more intense, than the last one.
By figuring out this pattern, I realized I could proactively work to decrease certain symptoms before they arrived.
This was when I began to build a holistic treatment plan with the intention of preventatively combatting my chemo symptoms. The goals of this holistic plan were to:
- Decrease the severity of my chemo side effects
- Keep my immune system strong throughout my 6-month chemo journey
- Remove all miscellaneous toxins (i.e. sugar, alcohol and stress) for the duration of my treatment to allow all of my healing energy to be focused solely on combating the cancer cells and coping with chemo
I followed my holistic treatment plan closely and mindfully, and I truly believe it made a significant impact on the outcome of my journey.

Integrative Medicine Practices
Turning to holistic treatment for side effects
Establishing and following a strict holistic treatment plan was the method that helped me the most, but building the plan was a journey in itself.
While I had some basic knowledge of holistic remedies from my time in India, my biggest concern was that holistic treatments would negatively interfere with my chemotherapy treatment.
What was the plan the integrative medicine doctor gave you?
Unfortunately, my oncologist wasn’t able to answer any of the questions I had on this topic.
He referred me to my hospital’s Integrative Medicine Center, where I was able to meet with an MD who was also trained in holistic practices.
She reviewed my oncologist’s entire treatment plan, as well as my scans, and then proceeded to answer all of my questions about the safety of holistic remedies in conjunction with my specific treatment. The topics we discussed were:
- Nutrition and supplements
- Acupuncture
- The mind-body connection, including guided imagery
Describe the personalized nutrition plan
First and foremost, she provided me with a personalized nutrition plan that would meet my goals of minimizing chemo-induced side effects while simultaneously working to combat cancer.
She also helped me build a comprehensive supplement plan, including vitamins, mushrooms and teas that would help keep my body’s immune system strong.


I asked her about Essiac tea, which had been recommended to me as “something that helped chemo patients exhibit as few symptoms as possible,” and she informed me that it was not only safe to drink daily, but incredibly healthy in general.
To this day, I still drink Essiac tea every day and can feel a noticeable difference when I miss a few days.

Acupuncture for fighting nausea
Next, we discussed acupuncture. Someone had suggested it to me as a good way of combating the extreme nausea I experienced in my first cycle.
I was surprised to find that not only did she fully support my desire to incorporate acupuncture into my treatment, but she strongly encouraged it.
She compared acupuncture to getting your car serviced before a long road trip. “Getting your car serviced won’t make the car brand new,” she explained, “but it will help the car run as smoothly as possible, despite the bumps you’ll surely hit along the way.”
Together we decided that doing acupuncture sessions one day before and one day after each chemo infusion (or medical procedure) would be a thorough and reasonable plan.
The mind-body connection
Lastly, we spoke in depth about the mind-body connection. I shared what I had learned about it thus far, and she encouraged me to continue deepening my understanding on the topic.
She recommended 2 documentaries, one called “Heal,” and the other called “Radical Remission.” These documentaries became staples in my holistic healing journey, and even now, whenever I feel down or discouraged about my health, I rewatch them as a reminder of the significant role that the mind-body connection can play with regards to physical health.
Using guided imagery
In alignment with this topic, she also recommended that I use guided imagery to help increase the effectiveness of the chemo, a phenomenon that is supported by scientific evidence but is seldom taken advantage of.
She referred me to an audio recording called “A Guided Meditation to Help You With Chemotherapy” by Belleruth Naparstek. I purchased the recording off iTunes and listened to it during every chemo infusion.
With the help of this recording, I would visualize the chemo drugs entering my bloodstream and attacking the cancer cells. Not only did it help me to relax during the infusions, but it also helped me feel like I was productively contributing to the chemo’s effectiveness.

Additional holistic practices are part of your routine
My single meeting with this doctor revolutionized my cancer journey. It helped to bridge the gap between my medical treatment and my desire to implement holistic healing practices as well.
However, the journey did not stop there. After meeting with her, I continued to build upon my holistic team of experts. I found an acupuncturist who was deeply knowledgeable in Chinese medicine and willing to commit to treating me consistently in accordance with my chemo schedule.
I also found an oncology exercise specialist, or cancer exercise specialist, who helped me build a plan for safe physical activity during treatment.
Through this specialist, I was able to get into a medical research study being conducted at my hospital called “Yoga for Chemotherapy,” in which I worked with a private instructor, who helped me to integrate yoga, meditation and breathwork practices into my healing journey.
»MORE: Read other patient experiences on yoga and meditation
With the help of all these experts, my holistic treatment plan began taking shape, and by the third chemo infusion, I felt like I had established a holistic routine that was perfect for me, my symptoms and my situation.
It should be noted that all of these services were provided for free or covered by my medical insurance. There are lots of free services to support cancer patients, and I believe utilizing them is hugely advantageous.
What was your follow-up protocol?
My oncologist does not believe in intermittent follow-up scans. His belief is that PET-CT scans are high in radiation and generally not good for anyone.
He also explained that the chance of a Hodgkin lymphoma relapse is lower than the chance of receiving a false positive from a PET-CT scan.
So instead of getting intermittent scans, our follow-up protocol is simply to meet every 3 months for a full blood panel, physical examination and thorough discussion of any symptoms or concerns that have arisen.
If there is cause for concern, only then will a scan be ordered. I was the only cancer survivor I knew who wasn’t getting regular scans during the first year of remission.
At first, it bothered me, but as time passed, I learned to appreciate my oncologist’s approach. Now I highly recommend that every cancer survivor inquire with their oncologists as to whether recurring follow-up scans are truly necessary in their case.

Hair Loss
How did you prepare for hair loss post-chemo?
My oncologist informed me that the chemotherapy regimen would cause my hair to fall out, and I was definitely having trouble coping with that.
Like many women, I believed that my hair defined my physical identity, and I was terrified to see myself without it.
I spoke to a lot of people who had been through the experience and decided on a plan that felt right for me.
I would cut my hair short ahead of chemo and then allow the short hair to fall out on its own. I had been told that shortening it would decrease its weight, and therefore it would fall at a slower pace.
I was also told that there would be a clear moment when it was time to shave it off, marked by clumps of hair falling out simultaneously and painful hair follicles that felt like they were on fire.
I purchased a shaver in preparation for that moment, and in the meantime, I purchased silk pillow cases because they are more gentle on hair than cotton ones, as well as a new shampoo and an at-home hair treatment, both of which were specifically formulated for “sudden, temporary hair loss.”
I also began accumulating wigs, wraps, hats, etc. I didn’t know what was going to work for me, so I got a little of everything. As with every other aspect of this journey, getting prepped definitely helped me cope with the looming fear.
When did you start to lose your hair?
I began losing hair after the first chemo infusion, but it was evenly distributed and wasn’t falling out in clumps, so I decided not to shave it right away.
With each infusion, I lost slightly more hair, but the even distribution of it made it less noticeable than I was expecting, and I kept waiting and waiting for the moment that clumps began to fall.
To everyone’s surprise, after the first 3 months of chemo I had only lost 15% of my hair. After all 6 months of chemo, I had only lost 30%. It truly felt like a miracle.
Hair loss is extremely common for the chemo regimen I underwent, and many of the infusion nurses commented on how shocking it was that I still had hair.
I had spent countless hours worrying and agonizing over what losing my hair would be like, and for me this was a reminder that I should not waste time and energy worrying about things that haven’t happened yet.
Getting prepared was necessary, but in this case, too much preparation was emotionally trying. I don’t know why or how I didn’t lose my hair; perhaps it was discontinuing the bleomycin, perhaps it was the holistic therapies, perhaps it was the Essiac tea, or perhaps it was simply my genetics.
The truth is I will never really know, but I believe that life gives you the challenges that you are in need of overcoming, and apparently losing all my hair was not on the agenda for me.
»MORE: Patients describe dealing with hair loss during cancer treatment

Quality of Life Reflections
Describe how you approached fertility preservation
Deciding whether or not to freeze my eggs prior to chemotherapy was a difficult decision to make. I had already delayed treatment by a month in order to get a second opinion, and I was told that freezing my eggs would result in another 2- to 4-week delay.
However, my oncologist informed me that I would be required to undergo a number of pre-chemo baseline tests and procedures, so he suggested that I work on completing those whilst simultaneously undergoing the hormone treatments necessary for egg retrieval. I decided to go for it, and to my surprise, the entire process only ended up taking 11 days.
»MORE: Fertility preservation and cancer treatment
Describe the IVF egg freezing process
In my experience, the egg freezing process was quite easy and seamless. The hormone injections didn’t bother me, the daily blood draws and ultrasound check-ups felt efficient, and the egg retrieval procedure was quick and resulted in a successful outcome.
I remember sitting in the waiting room and flipping through a large booklet of testimonials from past patients. Each page was filled with words of encouragement and empathetic advice about how to handle the physical and emotional challenges of fertility procedures.
I remember thinking how foreign those words felt to me. For me, getting my eggs frozen felt like a tiny hurdle in an extremely difficult marathon.
I plowed through the experience while remaining laser-focused on the much bigger challenge that was waiting for me just around the corner. The truth is, in my case, I was too busy worrying about my own survival to be concerned about the lives of my unborn future children. Because without the former, the latter wouldn’t even have the opportunity to exist.
Now that nearly 2 years have passed, I am so grateful to have gotten it done and out of the way. Cancer has a way of derailing the life plans of its host, and I was certainly not spared from this reality.
From start to finish, I lost about 2 years of my 20s to cancer. As I try to play catch-up in many areas of my life, it’s nice to know that I don’t have to worry about having children in accordance with my biological timeline, because my eggs are already frozen.
It preemptively lifted a weight off my shoulders, which hadn’t begun to weigh me down.
»MORE: Read a patient’s detailed IVF journal
Were there moments you had to advocate for yourself?
Being a self-advocate was of the utmost importance every step of the way, and I simply cannot stress that enough.
Whether it’s:
- Standing up to your doctors regarding the validity of your pre-diagnosis symptoms
- Doing your own independent research to be able to challenge your doctor with informed questions about your treatment
- Seeking alternative solutions to your issues when your doctor has no input
- Learning to ask for help, learning to accept help
- Simply learning to say no to social invitations because of a compromised immune system
Not only does self-advocacy help ease the challenges of the journey, but it also helps ensure you will receive high-quality medical treatment.
»MORE: How to be a self-advocate as a patient

Taking care of your mental health
Without question, it was the teachings related to the “Yoga For Chemotherapy” study that helped my mental health the most.
Practicing yoga and meditation daily helped me maintain control over my mental health, and whenever I began to lose control due to fear, pain or discomfort, it was the breathwork practices that helped me regain it.
‘I can breathe my way through anything’ became my personal mantra.
Although I had prior experience with all of these practices from my time in India, I was never able to feel the magnitude of their powers until I was facing a true emotional (and physical) crisis.
How important was it having caregivers?
Having support from caregivers is vital, and learning to accept that support is equally as important. The latter was the more important lesson for me to learn.
Being a cancer patient often made me feel like a burden on my loved ones, but in learning to surrender to the situation, I also learned to accept help when it was offered.
I reminded myself that I wouldn’t need help forever and that I would be doing myself a disservice if I chose not to accept the support that was being offered.
For those who are struggling to receive the support they need, I recommend expanding your search. There are so many amazing resources and programs to support cancer patients free of charge.
Research them, ask your doctors about them, ask other cancer patients about them, and take advantage of them. Remember that even if you feel alone, there will always be someone willing to help, if you can just find the courage to ask for it.
Were you able to keep working through treatment?
When I received my diagnosis, I stopped working in order to focus full-time on my healing. I am a firm believer that your body heals best when your mind is at rest.
While many cancer patients consider their treatment period to be an unfortunate “pause” in their regular lives, I found that I was able to spend my free time educating myself on what it means to be truly healthy.
Without this experience, I’m not sure I would have ever found the time, opportunity or motivation to do such pivotal internal work. I feel so fortunate to have had the financial means to accomplish this.
With that said, 4 months into chemotherapy, I was spontaneously offered a job on the founding team of a health and wellness conference series based in Kaplankaya, Turkey.
At the time of the offer, I had already established a harmonious rhythm with regards to my medical and holistic treatment plans, and I was feeling physically and mentally strong enough to take on something new.
As such, despite being in the middle of treatment, I decided to accept this new position. It should be noted that performing this work served as a continuation and reinforcement of the personal healing work I was already doing.
Had it been a job offer that didn’t reinforce these values, I would have certainly declined. Focusing on my own personal healing and health education were my only priorities during this time, and I was extremely fortunate to find an opportunity that supported and deepened that work.

How has it been navigating survivorship post-treatment?
Now that nearly 2 years have passed, I am able to look back on the experience with a deep sense of gratitude. Though it was the most difficult hardship of my life, it set me on a new path of health and wellness, which has become my new normal.
Not only did it shift my daily habits in a more positive and healthful direction, but it also helped me to acquire the underlying knowledge to support a career transition into the health and wellness industry. This allowed me the privilege of continuing to deepen my personal healing practice through my regular daily work.
Overall, my cancer journey represented the first time I was truly able to turn a personal hardship into an absolute triumph of lessons learned.
I now understand that I am capable of approaching all of life’s hardships in a similar manner, and I am so grateful to have learned this lesson in the earlier stages of my life. It has already served me in so many ways. Not only do I prefer my new normal to my old life; I am eternally grateful for it.
What’s your last message to other patients and caregivers?
To anyone facing a medical hardship, I say this: Our doctors can support us in our healing journey, but the journey itself is ours and ours alone.
Nobody knows your body better than you do, so listen to your body and your intuition first and foremost. Don’t mistake your doctor’s word as being the ultimate word. Only you are entitled to that.

Inspired by Nicole's story?
Share your story, too!
Classical Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)