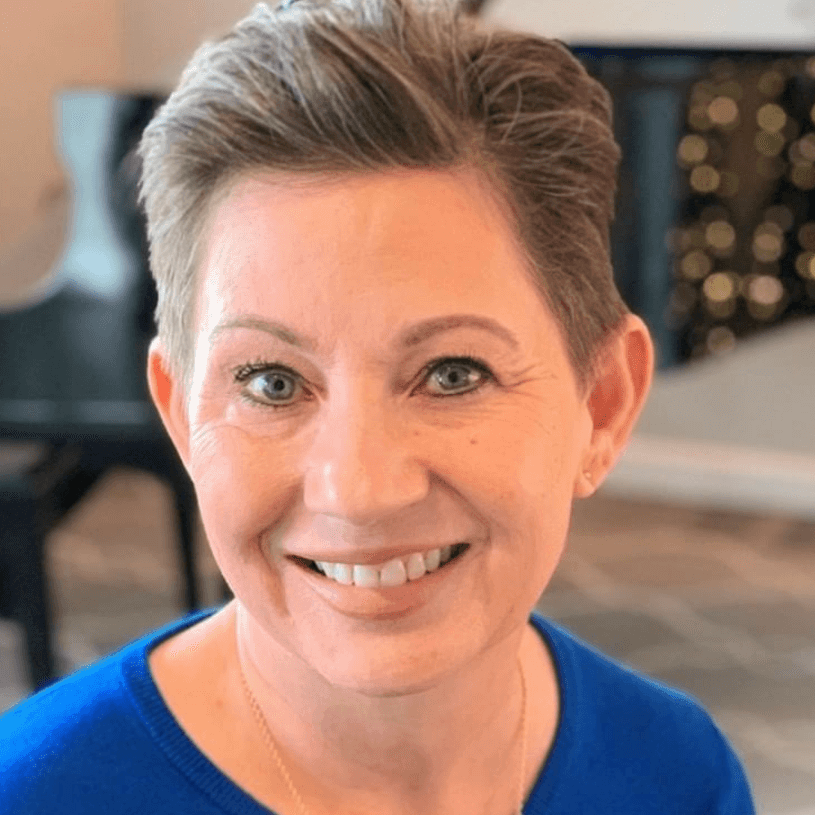
Chance’s Stage 2 Triple-Negative Breast Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Chance, who has a family history of cancer and tested positive for the BRCA1 gene mutation, was diagnosed with stage 2 triple-negative breast cancer at 24.
She discovered a lump in her chest during a beach trip. Despite having no other symptoms, she acted promptly and sought medical attention. After various tests, she received the official diagnosis of triple-negative breast cancer, the most aggressive form of breast cancer with limited treatment options.
She navigated chemotherapy, facing severe side effects like nausea, fatigue, and hair loss, and encountered unexpected complications while healing from her double mastectomy. Radiation therapy also presented difficulties, preventing her from undergoing breast reconstruction.
Despite the challenging journey, Chance emphasizes her gratitude for being alive. She highlights the importance of making choices that benefit one’s well-being and encouraging openness with loved ones for support.
In addition to Chance’s narrative, The Patient Story offers a diverse collection of breast cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Chance O.
- Diagnosis:
- Triple-negative breast cancer (TNBC)
- Staging:
- 2
- Initial Symptoms:
- Lump in breast
- Treatment:
- Chemotherapy: doxorubicin, cyclophosphamide, paclitaxel, carboplatin and olaparib
- Surgery: double mastectomy, radical hysterectomy (preventive)
- Radiation
Introduction
I’m 27 years old and work full-time as a social worker in foster care. I’m the regional director for Louisiana and South Carolina. I love my job. I’ve been working in foster care since I graduated college and I don’t see myself doing anything else.
When I’m not working, I’m outside. I don’t care what the temperature is or what the conditions are. I’m barefoot if I can be and if it’s safe to do so, which my friends think is crazy.
I rock climb and mountain bike a lot. I go hiking. I like lying in the grass and looking at the sky.
I have a dog, a five-year-old mutt who’s the best. I’ve been in a relationship for three years. I started three months before I was diagnosed; talk about diving right into a relationship. I travel full-time with my partner. She’s a respiratory therapist so we go wherever her work is and I work from home full-time.

I looked down at my chest hesitantly and could see a lump sticking out of my chest. It felt like it happened overnight, which is so cliché.

Pre-diagnosis
Finding a Lump
I was 24 at the time with a very extensive family history of cancers. I tested positive for the BRCA1 genetic mutation years prior so I was hyper vigilant as is. I was getting scans and tests done every six months preventatively.
In January 2021, I got my MRI and everything looked great. In February, I was in Florida, having a great time. I was lying on the beach and as I went to flip over to tan the other side, I felt a sharp, surface-level pain in my chest. I thought I laid wrong or laid on a seashell or something so I went about my business. It happened again so I lifted my towel to check if something was poking me and there was nothing there.
I looked down at my chest hesitantly and could see a lump sticking out of my chest. It felt like it happened overnight, which is so cliché.
Other than that, I had no symptoms. Sometimes people look back and say, “Oh, now that I think about it, maybe this and that.” I had nothing else.
The lump was big enough for me to know that it wasn’t a cyst, a bump, or a bruise. The best way I can describe what I saw was a lot of defined edges. It was the strangest thing I’ve ever seen on my body.
Because of my family history and my BRCA1 genetic mutation, in my gut, I immediately knew. I didn’t panic. I wasn’t in denial. I knew I needed to do something about it.

My nurse practitioner took me seriously. She said, ‘I’m going to get you scheduled for an ultrasound. Let’s rule out the worst-case scenario.’

Appointment with Nurse Practitioner
I didn’t tell anybody besides the family I was with on that trip. I handled it in private for a little bit.
I called my nurse practitioner and said, “I want you to look at this. I don’t think it’s anything, but let’s take a peek.” We scheduled an appointment two weeks after I found it. Thankfully, she took me seriously and said, “We’ve got to get this looked at. It could be a cyst, but let’s double-check.” From there, I went about all of the testing and imaging that would take what felt like forever after that.
I feel like testing for breast cancer is different for everyone and, honestly, I’m going to go out and say it’s different depending on where you live and who your doctors are. Unfortunately, not everyone has access to the same scans and imaging.
My nurse practitioner took me seriously. She said, “I’m going to get you scheduled for an ultrasound. Let’s rule out the worst-case scenario.”
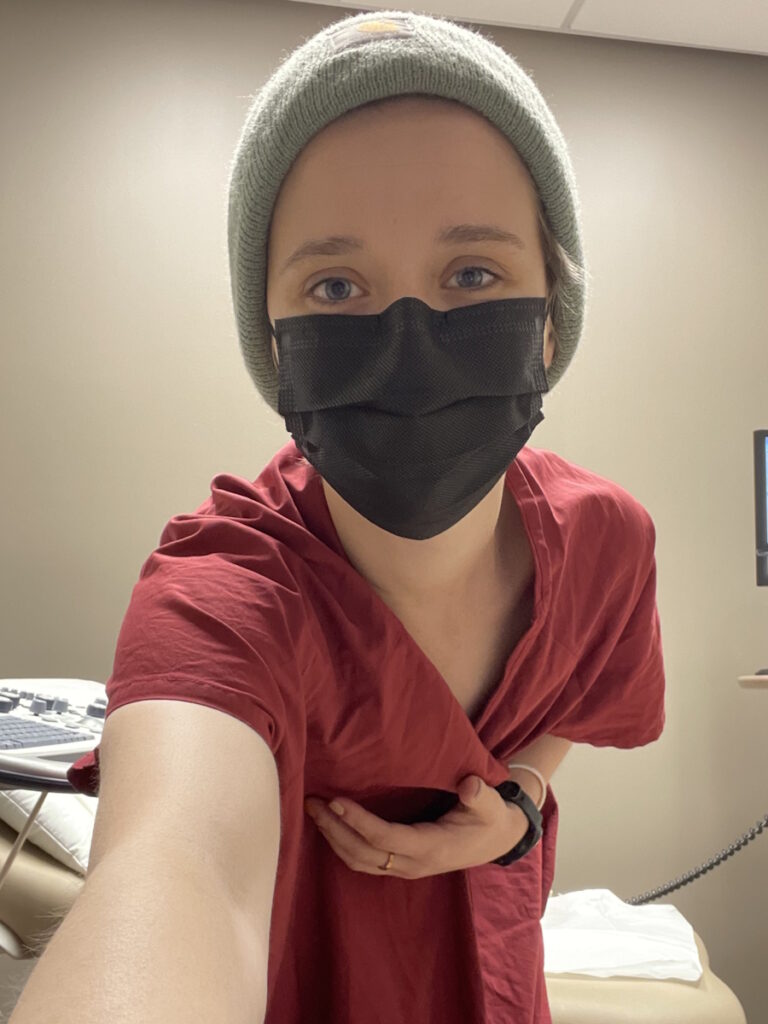
Testing for Breast Cancer
I went to the same imaging center where I get my scans every six months so they knew me and were familiar with my history. Usually, when I would get an ultrasound, they say, “Have a great day! We’ll see you in six months,” or, “Hey, we want to take a peek at this quickly.”
It was significantly different this time. It felt like I was the only one in the facility. It went silent. After my ultrasound, they immediately took me back for a mammogram. Then after, they immediately took me back for an MRI without even waiting for insurance approval. They said, “We’ll figure it out later,” which I thought was crazy.
I had all of those tests in one day, which is not common. You usually go about a week between each one. After I had all of those initial imaging done, three days later, I was lying on a table getting a biopsy. It’s not common for everything to happen that quickly so in my gut, I knew something wasn’t right.
I always thought that breast cancer is the most treatable cancer among women… I didn’t realize that there were so many subtypes of breast cancer and I got the worst one.

Diagnosis
Getting the Official Diagnosis
I had the biopsy on March 10, 2021. Five days later, on March 15, 2021, at 2:21 p.m. — I will never forget that time — while sitting in my grandparents’ living room, they called and said, “I have good news and bad news.” I said, “There’s no good news. What’s the bad news?” They told me I was diagnosed with stage 2 triple-negative breast cancer
At 24, and to date still, I am their youngest patient ever who’s been diagnosed with triple-negative. Now, there are people younger than me who have been diagnosed, but in my specific city, I’m still the youngest one that they’ve seen.
Learning About TNBC
I didn’t know anything about triple-negative breast cancer. As I was growing up, with my mom and her sisters having cancer, to me, cancer is cancer. Breast cancer is breast cancer. You either have breast cancer or you don’t. That’s the way that I approached it up until it happened to me.
I thought, Oh, triple negative. That’s amazing, right? Three negatives. We want that. We want negatives. I was then informed that triple-negative breast cancer is the most aggressive form of breast cancer with the least amount of treatment options. That’s the moment when I thought, Okay. This is real. My life is on the line here.
I was naive. I always thought that breast cancer is the most treatable cancer among women and all these other things you see online. I didn’t realize that there were so many subtypes of breast cancer and I got the worst one.

My breast surgeon sat with me for three hours and went into detail about everything I needed to know about triple-negative breast cancer.

I owe learning about triple-negative breast cancer to social media and my medical team. I say social media and not Google. If you’re newly diagnosed, please stay off of Google. I went straight to Google and I saw crazy stuff no one wants to read.
I turned to social media and found the Triple Negative Breast Cancer Foundation. I dove in head first and connected with a lot of people. I connected with Kelly Thomas instantly and she’s been like my big cancer sis. Five years out is the goal we want to reach. She and the whole community have been informative.
The Triple Negative Breast Cancer Foundation has great resources that I’ve utilized to learn about triple-negative breast cancer. At the end of the day, if I have a question, I go to my doctor first before anything else and then reach out if I’m unable to get the answers that I’m looking for.
Treatment
Discussing the Treatment Plan
I went in naive. I thought, Oh, it’s a tumor. You can see it. Just cut it out, right? No, not at all.
My very first appointment after being diagnosed was with an angel in human form, who is also my breast surgeon. She is the best thing that happened to me through all of this. I walked into her office scared and she sat with me for three hours and went into detail about everything I needed to know about triple-negative breast cancer. She told me I was going to need chemotherapy first and then she would do the surgery.
Then I went to my oncologist and met with the nurse practitioner. I got “chemo education” where you learn about all of the side effects, the what-could-happens, and the what-might-happens.

I feel very thankful for a team that cares about my life as much as I do.
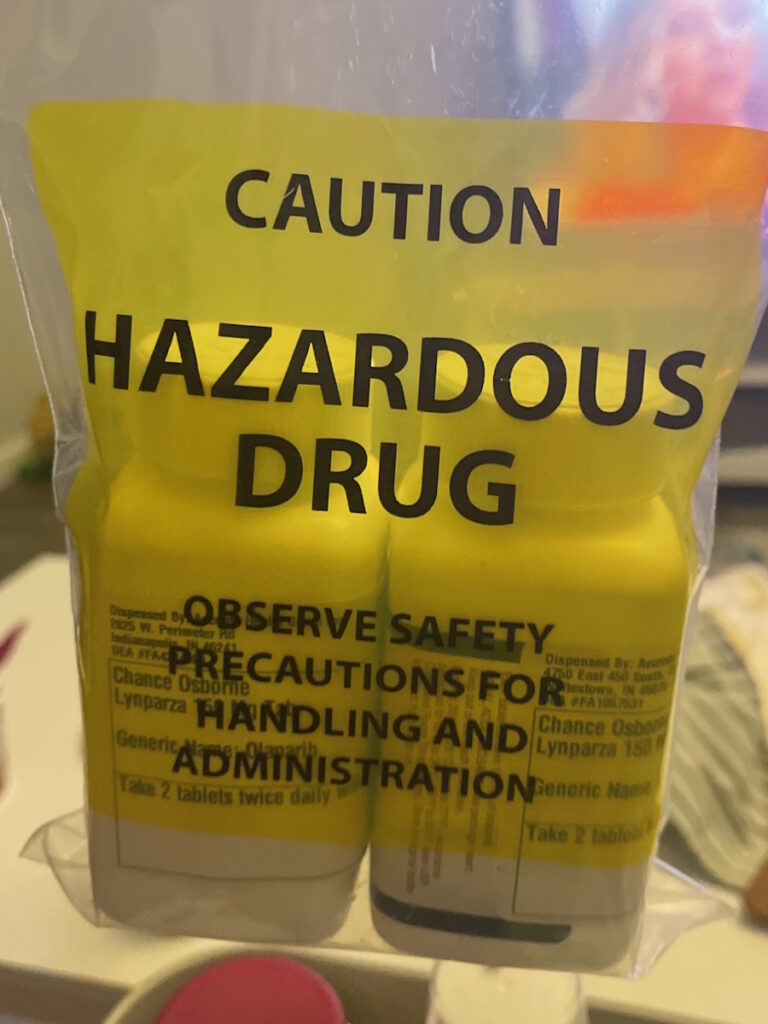
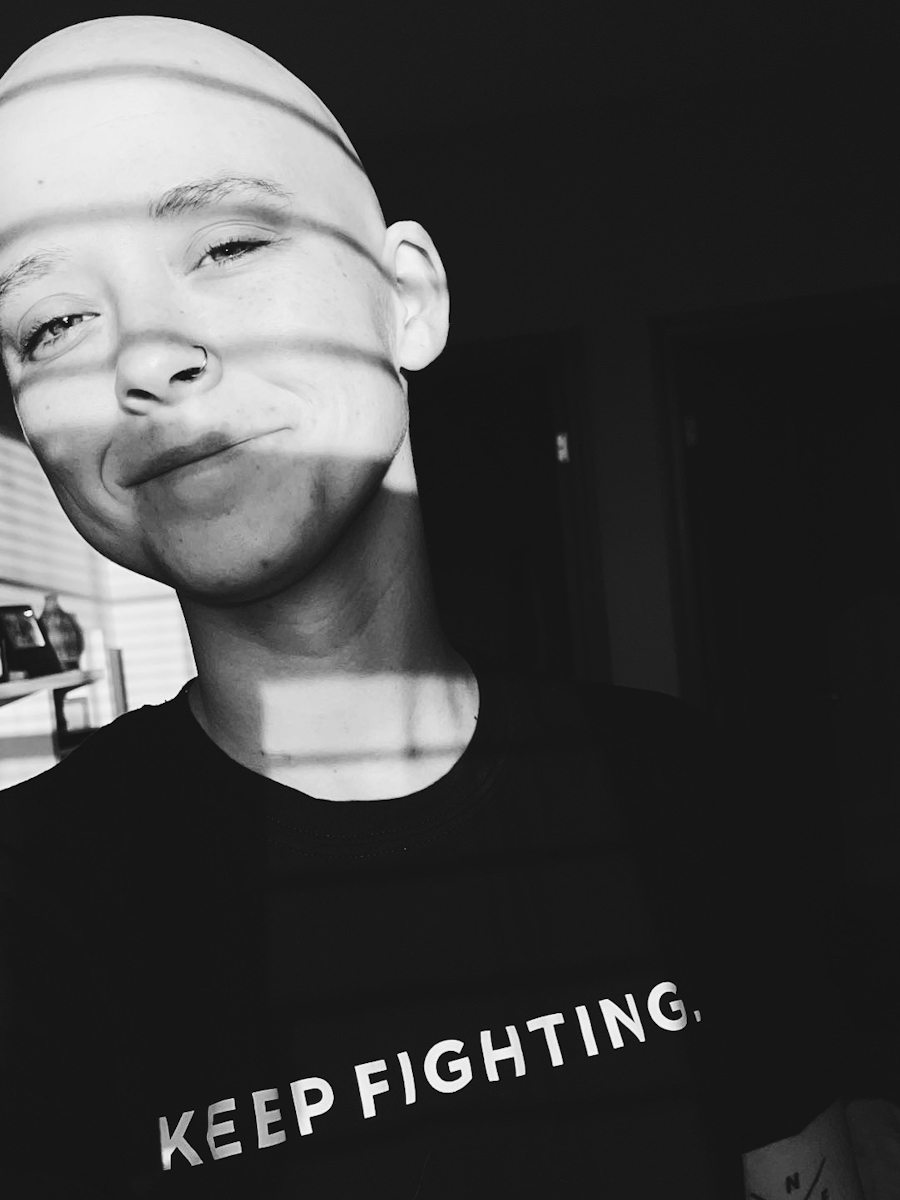
Chemotherapy
The Tuesday after my oncologist appointment, I started my first round of chemotherapy. Thankfully, they acted very quickly with me. From the date of diagnosis to my first chemotherapy was 16 days, which is very, very uncommon. I feel very thankful for a team that cares about my life as much as I do. I have been so privileged with my medical team.
With chemotherapy, a lot of it was based on some preliminary tests. You have to get an echo to make sure your heart is strong enough. I also had a full body scan to make sure the cancer wasn’t anywhere else. I had a scan of my brain to make sure it wasn’t there. That was going to determine my chemotherapy approach.
Once they found out there was no lymph node involvement and nothing involved anywhere else, we decided to do what was considered the gold standard of triple-negative breast cancer at the time. Saying at the time makes me feel like it was so long ago but that is no longer the standard.
My regimen was four rounds of CYTOXAN (cyclophosphamide) and ADRIAMYCIN (doxorubicin), which you may hear as the Red Devil in the cancer community. I don’t refer to it as that, but some people do. I did that every other week and I thought that was going to be the end of me. It was hard on me. Thankfully, I made it through and this is when it starts to get a little tricky.
Side Effects of Chemotherapy
After those four rounds, I was supposed to move on to 12 rounds of TAXOL (paclitaxel) once a week. About four weeks in, while having an infusion, my heart started doing some crazy stuff. I thought it was a panic attack. My vitals showed otherwise and they immediately had to stop treatment.
My port sits on either side of the chest and goes into the aorta. My port catheter had migrated into my tricuspid valve. If you know anything about hearts, nothing should be in there. That’s what triggered the Afib (atrial fibrillation). But they thought it was the chemotherapy so they stopped the Taxol and switched me to carboplatin. I did that every three weeks for four weeks.
My plan didn’t go as planned, but I was still able to get a substantial amount of chemotherapy within about 16 weeks. Once the experience happened with Taxol, I had to get my port removed.
I was able to finish chemotherapy. Unfortunately, I had to have the rest of my chemo through my veins so I had to get poked every single time.

Towards the end of that round of chemo, I was at a point where I had to crawl to the bathroom because I had nothing left to give.

I want to make it very clear that these side effects are my side effects and they may not be your side effects. Every experience is significantly different. I, unfortunately, felt like I had the worst experience possible, at least with the first four rounds of chemotherapy. Adriamycin and Cytoxan is the most lethal form of chemotherapy and I felt every sense of that.
I had extreme nausea, constipation, bone pain, fatigue, low blood pressure, dizziness, and vomiting. It honestly felt like the worst hangover of your life for eight weeks straight. There were very few things that could resolve it. I couldn’t walk. I was very weak and frail.
I’ll never forget one of the most vulnerable moments for me and it makes me emotional to this day. Towards the end of that round of chemo, I was at a point where I had to crawl to the bathroom because I had nothing left to give. It broke me down.
Some things helped, thankfully. During my last infusion, I figured out to receive a different form of nausea medication and have more fluids at the time of infusion. Taking an allergy pill also helped with bone pain.
Baths helped. Anyone who knows me is going to laugh when I mention taking baths. I probably took 5 to 7 baths a day. The warmth on my body was the only thing that made me feel like I could survive.
Honestly, sleep helped. There were days when I would take a Benadryl or my sleeping medication in the morning because being asleep felt so much better than having to be awake and endure what I was enduring.

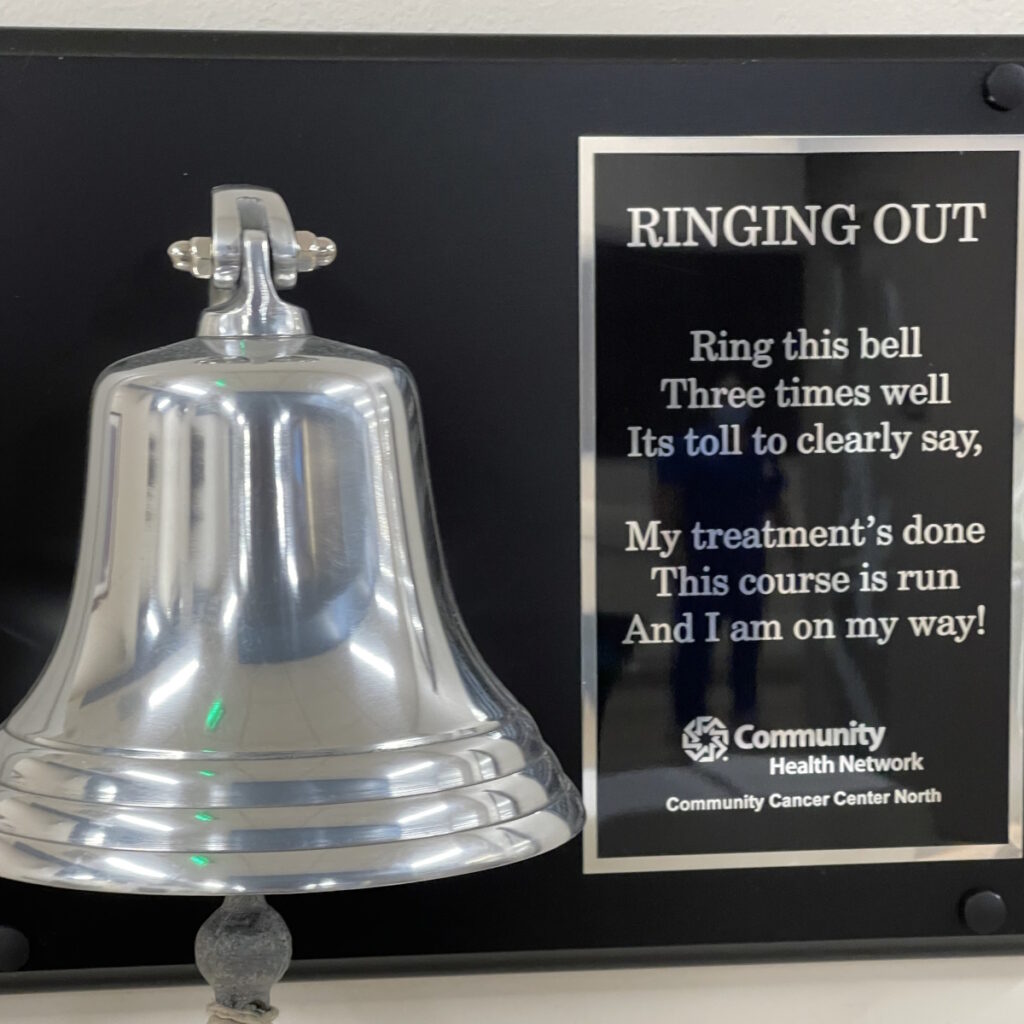
I rang the chemotherapy bell on August 8, 2021, and I thought the hardest part was behind me.
The second cycle of chemotherapies was night and day. I was able to work full-time. My hair started growing back. I was dizzy and I didn’t feel great, but for having chemicals pumped into me, I felt pretty good so that was a huge relief.
I didn’t have to change anything. I didn’t have to seek out any additional measures to feel comfortable and maybe it’s because I was comparing it to the first round. The second round felt like a breeze.
I didn’t look great. I was incredibly skinny. I was very pale and had big black circles around my eyes. I was bald pretty much, but I felt a lot better than I did initially.
I rang the chemotherapy bell on August 8, 2021, and I thought the hardest part was behind me. That’s what you see online. Chemotherapy is the hardest and if you can get through that, you can get through anything. I wish that’s how my story went.
Surgery
Double Mastectomy
After chemotherapy, I went in for surgery on August 30, 2021. The plan was a double mastectomy, lymph node dissection for testing purposes, and expanders to stretch out my skin to eventually get implants.
All went to plan. Everything was looking great. I had to stay in the hospital overnight.
Complications from Surgery
When I woke up the second day, my chest was black. My skin was black. It was actively dying.
My team came in and explained that there was a dye that was used called methylene blue dye, which allows your surgeon to trace the cancer or for testing purposes. What ended up happening was that I was allergic to it.
We had to take the expanders out. On September 4th, I went back in for surgery. I was flat, which I was okay with. I was thinking I’ll get my expanders eventually. We needed to let my chest heal. It was black. There was no guarantee that my skin was going to recover. Thankfully, it did.

I feel comfortable in my body. It doesn’t look the way that I imagined it would at 27 years old, but I’m alive.

On September 14th, I had to have a third surgery because I developed a hematoma, which is uncommon to develop 10 days later. It was big enough that it looked like I had breast tissue.
This is a testament to my medical team. I called my breast surgeon in the middle of the day, not thinking anything would happen. At 10 o’clock that night, a bunch of people volunteered to come in and do the surgery, solely because they knew I was uncomfortable.
It wasn’t an emergency and I wasn’t in medical distress. I overemphasized how uncomfortable it was and that was enough for them to rally the troops and do my surgery that night, which felt incredible. Again, I felt privileged. I thought, Okay, the worst is over. I’m good. It’s going to heal. I’ll get my expanders.
Where my skin turned black, a tiny little piece of my expander was able to break through the skin and that part of my chest never recovered. That was a long, drawn-out process of staples, stitches, glue, a wound VAC, and all of these other things. It eventually closed.
By the time it closed, it was time for radiation. We’re thinking we’ll do radiation and do the reconstruction after.
Radiation
Radiation didn’t go to plan either. It was really hard on me. Radiation can be different for everyone, but in the context of my surgery, the radiation affected my skin. The scar that we finally got healed broke open again. There were a bunch of delays and a bunch of little things that happened in between.
All that to say, I never got reconstruction because my skin was not in a position to do so. It may be in a few years, but to be quite honest with you, I’m very happy with what I have now.
Even if my surgeon called me and said, “You can get implants right now,” I would say no. I feel comfortable in my body. It doesn’t look the way that I imagined it would at 27 years old, but I’m alive, and being alive outweighs anything that my body could look like. It was a crazy experience.
Preventative Surgery
Total Hysterectomy
On October 12, 2021, I had a total hysterectomy. My mother passed away from ovarian cancer in 2011 so it was an option given to me as a preventative measure. Again, that’s a conversation that individuals need to have with their medical team, but that was a decision that I made for myself.
Thankfully, that healing was textbook perfect. I handled that very well and recovered very well.

There are plenty of babies in this world that need me and I need them. I just don’t know them yet.

Fertility Preservation Before Cancer Treatment
Fertility was one of the first conversations I had with my medical oncologist. Being so young, he said, “We need to get you started on fertility treatments. You’re so young,” and I stopped him mid-conversation. I said, “I don’t want to proceed with that.”
He said, “This is a lot. Go home. Think about it.” He said this all out of kindness and stepped into dad mode. “Sleep on it. We can talk about it. We can educate you on it.”
There’s nothing to think about. Ever since my mom died, since I found out that I was BRCA1 positive, and since I’ve worked in foster care, I’ve never wanted to have children of my own. There are plenty of babies in this world that need me and I need them. I just don’t know them yet. It’s never crossed my mind.
I will say though, in a moment of vulnerability, do I grieve the loss of having my own children? Absolutely. But I know what it’s like to lose your mom in childhood and I’m going to do everything I can to prevent my children from enduring that same thing. If that means not having them biologically, then count me in.
Follow-up Protocol
November 2023 puts me at almost three years since diagnosis, which is crazy to me. I see my medical oncologist every 3 to 4 months, which seems to be on par with the community. I don’t get any scans unless there’s a reason to do so.
I get a Signatera test. It’s a very new development. It’s a cool test. They take your initial tumor DNA, draw your blood, and match it to your current blood DNA to see if there’s any circulating tumor DNA in your blood.
I’m not convinced that I trust it 1,000%, but for me, the reason we do that is that my tumor markers are not reliable. When I was diagnosed with cancer, it was a 9 and it’s been 9 ever since, even though I currently don’t have cancer so it doesn’t provide us accurate information to use it for determining reoccurrence.
I get a bone density test every two years because I had a hysterectomy and estrogen is what fuels healthy bones. I still see my gynecologist once a year to make sure that the fluid in that area is free of cancer.
I see my breast surgeon every six months or once a year to check on scarring. She does an exam and checks my chest wall, my armpits, and my neck. She is a true angel.
I see my team often and I plan to do so until I hit the golden five-year mark in the triple-negative breast cancer community.

Not having my mom with me to experience all of this was hard, but I was surrounded by my grandparents, my partner, really good friends, and my family. I felt very, very privileged to be loved so well.

Words of Advice
My biggest piece of encouragement is something that I’ve had to learn and now learning: there’s no wrong choice in your treatment. Sometimes you think of making the right or the wrong choice. I want to encourage you to understand that there’s no wrong choice. You may have to make a different choice if you don’t like the choice that you made at first.
I don’t like using the words right and wrong. There’s so much pressure with that, especially when it comes to your life. Instead, I encourage you to say, “What choice can I make right now that benefits me in this moment?” You have the autonomy and the privilege to make another choice if that choice doesn’t work out.
I was surrounded by amazing people. Not having my mom with me to experience all of this was hard, but I was surrounded by my grandparents, my partner, really good friends, and my family. I felt very, very privileged to be loved so well.
As time passed and as we had more open conversations about my journey, I asked them if there was something I could have done differently.
The only thing they said was that they wished I didn’t try to save them while I was saving myself. I withheld a lot of hurt, pain, and diagnosis information from them because I wanted to keep them as blind as possible to what was going on.
It wasn’t lost on me that that was just as hard for them. They watched my mom die and I’m sure that it was very triggering for them. I look just like my mom. I talk and act like my mom. I’m sure there were a lot of moments where it was like, “Oh no, is this going to repeat itself?”
If you’re newly diagnosed or in the thick of it, I encourage you to let your people in. They want to hurt with you. They want to be scared with you. I promise you, it’s way less scary if you allow people to be scared with you.


Inspired by Chance's story?
Share your story, too!
More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Alison R., Partially Differentiated DCIS, Stage 4 Metastatic
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in underarm/breast
Treatment: Chemotherapy, surgery, radiation, targeted therapy
Cancer Details: Only 1-4% of breast cancer cases also includes Paget’s
1st Symptoms: 2cm lump found in right breast
Treatment: Lumpectomy, double subcutaneous mastectomy, hormone therapy
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Cancer details: Both ductal and lobular, estrogen receptor positive. Different than breast cancer Tina’s mom was diagnosed w/ twice.
1st Symptoms: Sunken in nipple of right breast
Treatment: Double mastectomy, chemotherapy, radiation, hormone therapy
Cat L., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast radiating from lump
Treatment: Bilateral mastectomy, chemotherapy