Bethany’s Stage 2 ER+ Breast Cancer Story

When Bethany was in her late 20s, she used to find lumps in her breasts that turned out to be either swollen lymph nodes or cysts and would eventually go away. But when she was 33, she neglected to get one lump checked and it turned out to be cancer.
She shares her journey of how she went from not believing in medicine to blending the natural healing world with Western medicine and how the fear of recurrence pushed her to make big life changes.
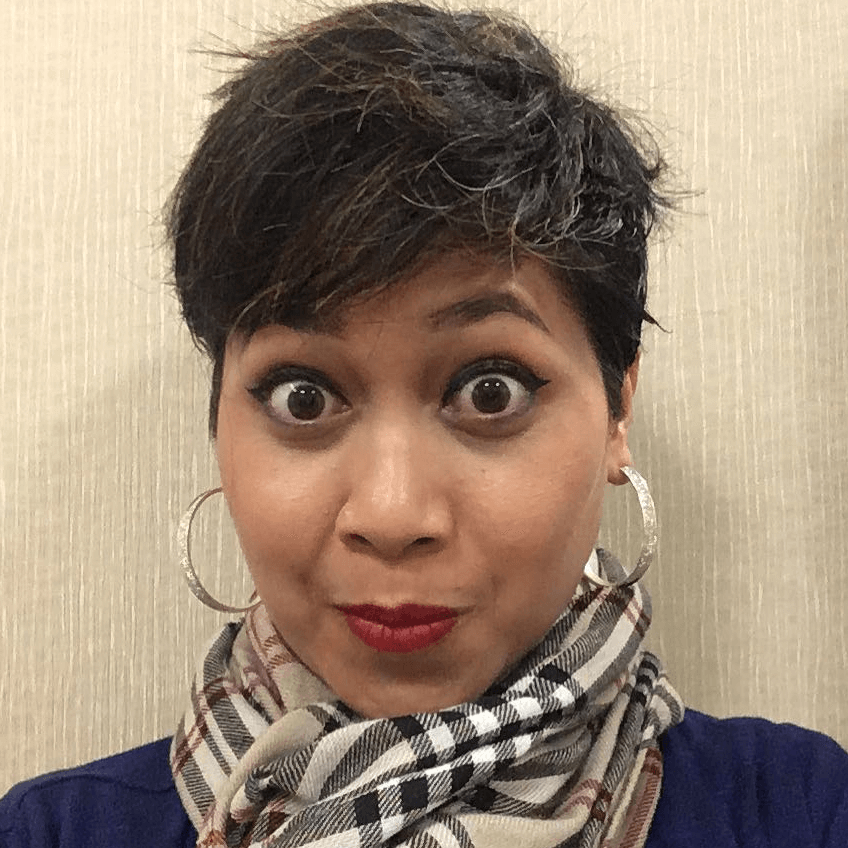
- Name: Bethany W.
- Diagnosis:
- Breast Cancer
- ER+
- Staging: 2
- Initial Symptoms:
- Lump in breast and armpit
- Treatment:
- Adriamycin (Doxorubicin)
- Cytoxan (Cyclophosphamide)
- Taxol (Paclitaxel)
- Double mastectomy
- Radiation
Here I am studying all these ways to be present, to be mindful, to embrace life, to learn, [and] to grow. What if that’s cancer? What if cancer is something that can be a teacher in some way and even improve my life or maybe help me appreciate life more?

- Pre-diagnosis
- Tell us about yourself
- When did you start to feel something may be off?
- How much time had passed before you had the lump checked?
- Getting the initial scans via thermography
- Finally getting an ultrasound and mammogram
- What was that moment when you said you needed to see what this is?
- Getting the biopsy
- Dealing with “scanxiety”
- Going in for the biopsy
- Diagnosis
- Treatment
- Remission
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-diagnosis
Tell us about yourself
I live in a small town just outside of Boulder, Colorado. I’m pretty obsessed with nature and adventure. Colorado just offers so many options for that. I’m so excited [about] ski season, hiking, nature walks, kayaking, [and] paddleboarding. It’s a new life for me out here. I’ve been here [since 2019]. I love anything outdoors. I love movement. I love life and the people in it.
I enjoy whatever is in front of me, whether it’s [a] delicious cup of coffee and chatting or sitting in the infusion chair for treatment.
[I’m] a lover of life and an inquisitive person as well, someone who challenges traditional belief systems, ways of living, or ways of looking at things. I get a little extra excited when someone’s like, “Oh, this is the only way.” I’m like, “Hmmm. Really? Okay, well, maybe we can challenge that a bit and see how there are just so many ways to live life, to enjoy life, to heal, [and] to be with people.”
I was [previously] in Texas. I was in Dallas and a little bit in Austin. Before that, I grew up in Florida. Florida, Texas, [and] Colorado are my three main homes.


When did you start to feel something may be off?
I found [the] first lump in my late 20s. At that time, I had a career as a yoga therapist, worked in wellness for many years, studied mindfulness and ate organic. I consider myself a really healthy person. I have no family history of cancer. But I did find a lump in my breast [so] I went and got it checked out. It was just a swollen lymph node or a cyst and it went away. I had very dense breast tissue. I had maybe four or five of those.
The first one [was] very scary. I didn’t realize there could be lumps that weren’t cancer. When you have dense breast tissue, it means it’s lumpy. Over time, those lumps would change and work themselves out so I learned how to monitor them, take them in and I felt I [had] a pretty good rhythm.
Fast forward to 33 [years old]. I found another one and decided not to get this one taken in and checked out. By that time, I already had enough of them and it’s always turned out to be nothing. I [didn’t] feel like going through that [whole] ordeal. I didn’t have health insurance at the time either. I was paying out of pocket for anything doctor related. I wasn’t very motivated to get that one checked out.
I first found the lump [in] November 2014. Over time, I noticed that it did start to grow. I talked myself out of it. I told myself that it was possibly a fibroadenoma. It’s just another swollen cyst. I’m so healthy. I don’t have a family history.
It wasn’t until the following summer [that] I felt another lump in my armpit and I’m like, Hmmm, that’s different. I had a really good girlfriend who was also a yoga teacher. Very healthy, lives a healthy lifestyle, has a great attitude about life, and she was diagnosed with a really aggressive form of sarcoma — stage 4 right off the bat — and it started as a pain in her hamstring, which she just thought was something from yoga. When she got diagnosed, that was definitely the wake-up call of, “Hey, you’re not immune to this. Young bodies get cancer.” I didn’t know much about it. I didn’t know many people. That really prompted me to get things checked out.
How much time had passed before you had the lump checked?
It was about eight or nine months in between. I found that lump, didn’t take it in, and then finally I did.
I considered myself a natural person. I would use nature to heal. Medicine was something I didn’t believe in at the time and [I would think to myself], “Oh, even if it was something serious, I wouldn’t use Western medicine to heal me. Are you kidding? That’s Big Pharma and I had all these beliefs about it.”
Getting the initial scans via thermography
When I did decide to get that lump checked out, I actually went for thermography. I was with a naturopath. I was in Texas at the time and had used it in conjunction with ultrasounds prior to that time. The results matched always. I was told with thermography that “there’s no radiation so it’s healthier for your body. It detects cancer six years earlier than mammograms.” It was just toted as kind of the better, healthier way to detect what’s going on in your breast tissue.
Those scans showed no signs of cancer in my breast or in the armpit so I was elated. The doctor gave me some homeopathic remedies, some other treatment options [to] flush my lymphatic system, and cleansing.
But in my time working with him, the lump started getting bigger in a matter of weeks. I asked him, “Are you sure I shouldn’t maybe get a mammogram? I don’t know. This feels weird.” We repeated [the] thermography scans two more times. Again, no signs of cancer.

You are not too young [or] too healthy to get cancer. It can happen to anybody.

Finally getting an ultrasound and mammogram
I still felt off. Finally, I was like, “I think I need an ultrasound or a mammogram.” And he said, “Okay, but just remember that mammograms cause cancer.” That’s a big story out there that prevents a lot of women from just going to a doctor and getting things checked out. I said, “Screw that. Maybe. I don’t know, but I have some big lumps here and I need to know what these are.”
I’m so happy I listened to that inner voice. I would have loved to turn her on nine months before when I first felt the lump, which is a big part of why I tell my story now. You are not too young [or] too healthy to get cancer. It can happen to anybody. Cancer loves bodies. It is just looking for a place to grow and thrive.
I did go the route of an ultrasound and a mammogram, which showed very suspicious activity. By that point, the lumps were protruding. You could see it coming out [of] my breast. A biopsy is what confirmed it.
What was that moment when you said you needed to see what this is?
I was driving home from my third or fourth appointment with the naturopath and I expressed my concern one last time. “I don’t know. I don’t feel comfortable with this.” His answer: mammograms cause cancer. I did respond, “I already have the lumps. Do you think they’re going to magically turn into cancer if I get my first mammogram? Do you think that that’s the case?” He [got] startled and [said], “Well, you do what you need to do.” I’m like, “I am.”
I actually kind of stormed out of that office, got in the car, and got my mom on the phone. My mom has a background in nursing. The whole time she’s like, “Go to the doctor. Who is this guy? Seems like a quack. Go to a doctor.”
I also felt really lost at that time, too. I knew I wanted one. I had no idea how. Here I am, I’m 33. I don’t have health insurance. I feel like an idiot. I’m beating myself up about not having health insurance in this situation. This was [at] the beginning of Obamacare. Health insurance for someone who is self-employed was so expensive. It was half my income for the month and I just couldn’t afford it.
Luckily, my husband at the time, his mother worked in a doctor’s office in Dallas. I reached out to her and I’m like, “Is there anything you can do to help? I need to get these lumps explored.” I’m so, so, so lucky because she just jumped right in. She got me [an] appointment with her PCP. I qualified for a charity grant for a mammogram and ultrasound.
Now, did I think it was cancer? No, but I wanted to rule it out. I need to know what this is just for my own peace of mind.
Luckily, with the Affordable Care Act, I was able to get health insurance in the middle of the year because I had just moved so I qualified for special enrollment. It was just this magical thing all coming together.
It really started dawning on me: Oh my god, this could be cancer. What if this is cancer?
Getting the biopsy
My insurance hadn’t kicked in yet. I could have waited a few weeks to get the biopsy, but I got a quote for it. I think it was $825 or something. Cue naivety. I thought, I can do that. That’s worth my peace of mind right now, honestly. I’ve just been in this already for weeks and I just need to know what this is.

Dealing with “scanxiety”
At that point, I just got trained in this mindfulness practice of inquiry called The Work of Byron Katie so I have all these tools for dealing with stress. That’s literally my career at that time. During the diagnostic phase, when I still couldn’t figure things out, it really started dawning on me: Oh my god, this could be cancer. What if this is cancer?
I completely spiraled downhill. My mind was full of worst-case scenarios and all I could think was I have cancer. My life is over. All my dreams are done. My relationships are over. This is going to absolutely crush my family. I couldn’t see any kind of good or positive outcome in this situation.
I was just torturing myself for not getting things checked out sooner. Thoughts like, It’s my fault. I did something wrong to create this in some way. Obviously, I wasn’t healthy enough or good enough or a good enough person. I had all this self-blame going on and with my mind full of all of those beliefs, all those emotions, I just spiraled down and didn’t want to leave my bed. I was depressed. I was lashing out at people that were trying to help me. I’m like, “You don’t understand. You don’t know what this is like.” It felt so lonely.
I knew the mammogram and ultrasound were suspicious. I had a biopsy scheduled. The interesting part now is that that time period was so important to me and my journey because I really got to see the cause of [my] suffering and the cause of my pain [at] that moment because I had no idea if it was cancer.
Cancer could not have been the problem [at] that moment. We didn’t even know if it was real or not. But what was real was everything that was going on in my mind. My mind was full of it — not of cancer [but] just worst-case futures. I believed them and I went downhill.
I hit this moment where I was like, “Enough! This is enough! I can’t do this anymore.” I hit a level of suffering where it was just, “I have to try something else.” That moment, just like that inspiring moment to go get a mammogram, that inner voice kicked in again and it’s like, “Girl, you have tools for this. Let’s go back to them.”
I reached [into] my little healing toolbox and pulled out The Work of Byron Katie, which was the practice that I was just certified in. It’s a way to take those thoughts [and] get them all out of the mind. Write them down on paper. Beliefs like, “My life is over. Cancer will ruin everything. I’ll die young.”
I just started writing. Writing, writing, writing. Then I started questioning those beliefs and asking myself: “Is it true that my life is over? Can I really know for sure?” I’m like, “I can’t know for sure. It feels that way, but I don’t know. I don’t even know if it is cancer. Even if it is cancer, does that mean my life is over right away? I don’t know [the] cancer world well. Actually, there are people that are still around that have been diagnosed.”


Then another question of that process is, “How do you react when you believe that your life is over?” And that’s the depression, that’s spiraling down, that’s the lack of motivation to even take a walk around the block or eat [healthily]. I wasn’t motivated to do anything and [was] angry, rageful, and just lost.
Then I asked myself the final question of that process: “Who would I be in this same situation?” I have a biopsy scheduled at that point. Who am I in this situation? I don’t know what it is, but who am I without the thought my life is over? I had to sit and meditate in that space for a bit. Another thought would come in. I’m like, “Put out that thought. Who am I without that thought?” It slowed down my mind enough to come back to reality.
[At] that moment, [the] reality was there’s no proof there’s cancer at that moment. I have the next step, which is the biopsy scheduled. How grateful I am that I’m able to do that. I’m breathing. I actually felt really good physically without the thoughts. I have more energy. I’m not so tense. I’m seeing I have a lot of support around me.
Then I move into turning these thoughts around — My life is over → My life isn’t over — and looking for some examples of that. In reality, I’m alive. I’m speaking. I’m looking at this body. I’m moving. I’m breathing. I’m eating. I’m digesting, I’m showering. I’m alive. My life is not over. It’s happening right now. Then I started to look at even if it was cancer, how could it be true that my life isn’t over, you know? Or maybe my life is just beginning?
I started entertaining this possibility of, “Let’s play with this worst-case scenario, and how could that even be good.” I sat in that question, journaling, writing, and some really neat answers came out. I was like, “You know what? This could be a really amazing adventure. Here I am studying all these ways to be present, to be mindful, to embrace life, to learn, [and] to grow. What if that’s cancer? What if cancer is something that can be a teacher in some way and even improve my life or maybe help me appreciate life more?” That was already starting to happen.
Going in for the biopsy
When I went in for the biopsy, the nurse, her name was Joy and I just thought it was perfect. She was so sweet. I watched her walk me through all the details, put on the cozy socks, and she had a warm blanket for me. I’m just like, “Wow, there’s so much kindness here.”
The doctors came in. They explained everything and held up the giant needles that were going to be going [into] my body. They’re like, “Do you want to watch the procedure on the screen?” I was like, “Hell, no. Please put something over my eyes and thank you.”
I was really mindful through all of it and it was kind of fun. I talked with everyone and I was grateful that it was happening because these tests are what’s going to tell me what’s going on in my body. Therefore, I can know, stop living in that land of the unknown, and then know how to deal with it.

Diagnosis
Official diagnosis
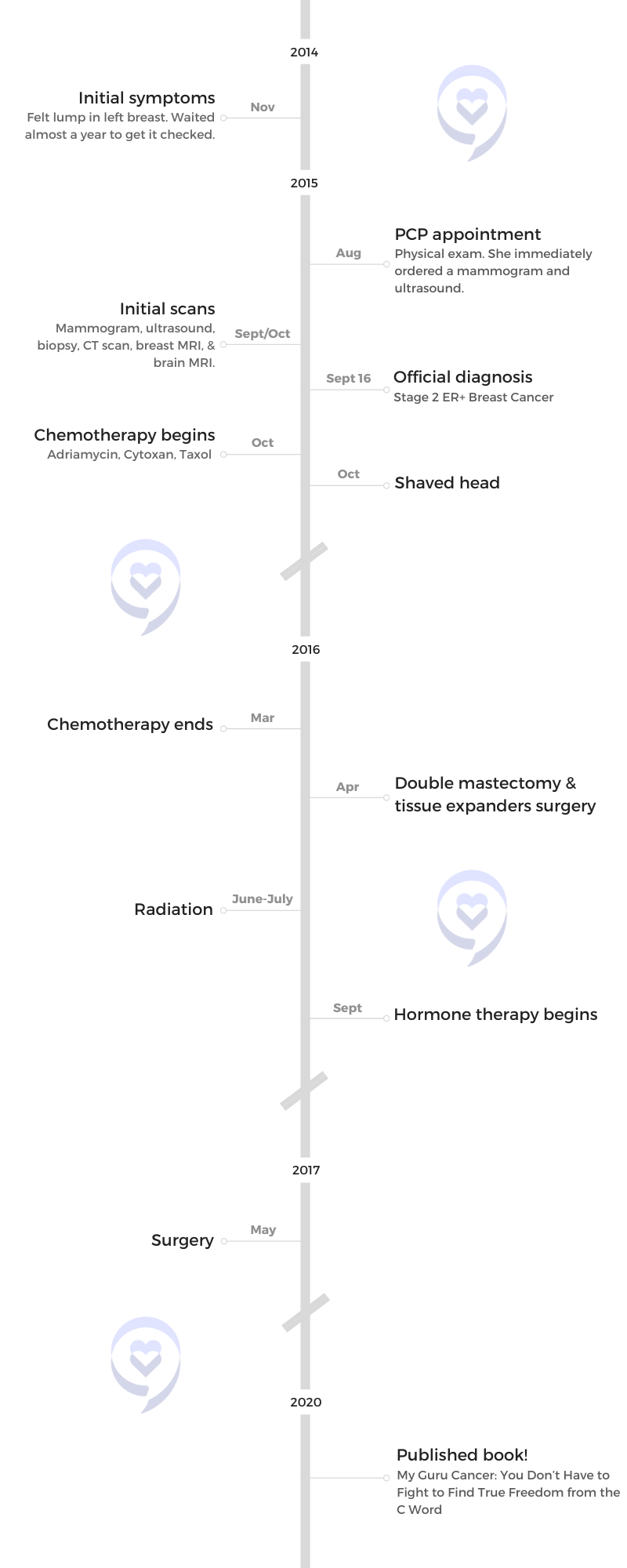
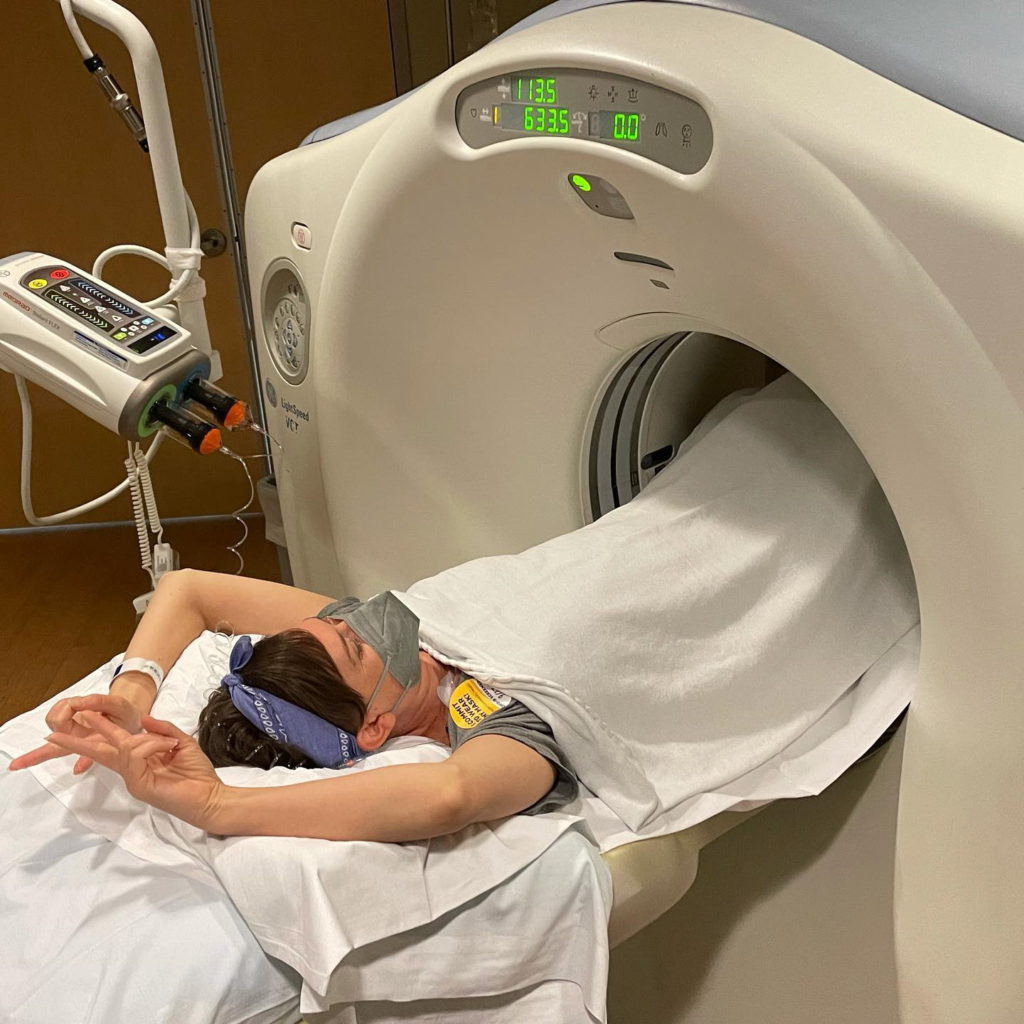
The official diagnosis of breast cancer was September 16, 2015. I had done a full body PET scan [and] brain MRI just to confirm it hadn’t spread to other places. Getting those results that it hadn’t was very nice to hear. Very relieving.
I had hormone-positive cancer, ER-positive. It loved estrogen. My body was really good at making it in my young 30s.

What was your reaction to the diagnosis?
By the time I heard those words, “You have cancer,” it was a few weeks after my 34th birthday. I was at home sitting on the couch, watching TV. I had known the results could come in any time. While I say I could find peace with cancer, I was still stalking my phone like crazy. I remember thinking, Should I get a car wash? Eh, no, I’ll just stay. I’ll just stay here.
My husband had just come home. I saw the number on the phone. [It] was the PCP’s office and it was just like, “Oh my god. Oh my god. This is it!” [My] heart rate goes up and he’s sitting next to me.
She was so kind. She said, “You know, I wanted to tell you as soon as possible. I know you’ve been waiting on the results and this is the part of my job I really don’t love. This is the hard part of my job.”
They found cancer in both breasts and the lymph node. Hearing those words, it was just like time stopped. I think I could have described every nanosecond. My hand was on the couch, the other one was on the phone. We had our foreheads touching, just leaning over, and we were just frozen.
Then she went on to share, “People get through this. I just had a patient who’s in her late 20s. She made it through. She just had her first baby.” I love that she was being a human on the phone with me and very caring. I still was like, “Are you… Really? Cancer? This is cancer?” It took moments to settle in. I was like, “What?”
We hung up the phone and I looked at my husband. I was like, “What do I do now? What do we do?” Then he just grabbed me, pulled me in, and we just started sobbing. While that was such an intense moment, I felt so much love, too.
I stood up and got really hot. My body started sweating. I had to take my shirt off. I was just pacing. I’m looking down and I’m like, “That’s cancer? What?”
Then it began — meeting with the breast surgeon [and] oncologist, and getting more tests done. My insurance kicked in finally and that biopsy bill turned out to be $8,000 instead of $825.

It was so much all at once. Just the emotions of my life just changed forever. With all the mental practice I was doing, I was trying to stay present with it. “Okay, it’s go time.”
It’s also heart-crushing how quickly your life changes. In my 30s, everyone else is growing careers, growing babies, and I’m growing cancer. I’m just like, “What? What the heck?”

Treatment
My first chemo was [at] the beginning of October. Within mid-October, I was bald.
They staged it at a late stage 2, early 3. There was a large mass in my breasts, a few little satellite nodules, and my left armpit had a tumor [that’s] 4.8 cm. That was the one that I felt. Some other ones were looking positive as well.
I asked — of course, Miss Natural Me, was very naive — and I’m like, “Oh, so we could just scoop that out in a little surgery and I’ll be cancer-free by the end of the year, right? That’s how this works.” And no, that was not how that worked.
I showed up to the office and again, my breast surgeon — so kind — is looking at me like a human. I know not everybody gets that experience and I was just so grateful. She’s holding my hand. She’s walking me through everything.
We couldn’t do surgery right away. She said, “If we did [the] surgery, it would be very mutilating to your body, especially in the armpit area, because you might lose the use of your arm. With that, I think we should do chemotherapy first with the goal of shrinking everything and then be able to have less invasive surgery.” That sounded like a great plan because I’m like, “I love my arm. I very much would like to use it.” So that was clear.
Then she said, “Five to six months of very aggressive chemotherapy, then surgery, then six weeks of radiation, and then five to 10 years of hormone therapy.” And that’s where I was like, “Are you kidding?” I just looked at her stunned.
I remember her drawing the graphs of how cancer cells multiply and divide in the breast ducts. I just was like, “That’s my body? You’re talking about my body right now? This is so confusing to hear all of this because I feel so healthy. If I didn’t have those lumps, I just felt on top of my health, on top of the world. I felt great.”
I love this moment. She grabbed my hands, looked me right in the eyes, and said, “You feel healthy because you are healthy.” I was just like, “Dang, you’re awesome.” Because that’s true. You think, “Oh, now I’m a cancer patient and now I’m sick.” No, I’m also a really healthy person. I just happen to have some cancer growing in my body. And that’s a totally different perspective than what we hear out there. Very empowering to hear as well. I am healthy. I am strong. And then you know what? I got this.
Starting chemotherapy
I dove right into that treatment plan. I thought of it in phases. It was too much to wrap my head around everything.
[I got] Adriamycin and Cytoxan, so AC. Four treatments every other week and that’s known as more aggressive, go after it really quickly, so a little bit more intense on the body. Then 12 weeks of Taxol so that took me into finishing in March. There were some times [when] my numbers were too low to be able to continue treatment so I’d have to take a break and come back so it extended it a little bit, which is normal in the process, too.


The stories I heard about chemo [and] what I saw in movies are my reference points of chemo being poison. I actually challenged some of those beliefs, specifically that chemo is poison to my body and that it’s poisonous to me. I found the opposite. Chemo is healing my body when I took it through that process.
You read the side effects, it’s terrifying. Imagine this future of bald, vomiting, gray skin. No quality of life is where my mind was going at first. Then as I started walking through it in inquiry, it was like, “I don’t know if it’s poisonous to me. I’ve never had it. I don’t know how’d my body react. I’m young, healthy, and strong. There’s a lot of complementary natural ways to support side effects and I’m actually pretty excited to learn more about that stuff.”
I started blending the natural healing world with this Western medicine world. [I] also looked at my other beliefs about Western medicine. You hear, “Oh, Big Pharma is only in it for money,” or “Doctors aren’t human. They’re just trying to make you sick.” These were the things I was hearing at the time in the natural world. I laugh at a lot of it now. Maybe that’s true in some cases but I’m looking at my doctors holding my hand, looking me in the eye, and crying with me. That’s a human right here. And you know what? They want what I want: to be cancer-free and live a good life. It doesn’t really look good on them if I’m dying next week. They’d run out of patients really quickly. It was just seeing this other world of medicine.
I became so grateful. It became a privilege. I’m so lucky I have treatment options.
Here’s this thing I’m going through. How can I make it better and more fun? Because whether I like it or not, I’m going through it.
When I went in for chemo, I nicknamed it. I changed the name to see love. I did this for a lot of things. I changed the name to something super cheesy, but it made me feel better.
I’d go and get all plugged in with my port. I’d see the kindness in the nurses. I’d make friends with my neighbors. I’d bring all my movies, coloring books, or whatever to entertain myself and I would have fun. There was this baseline of here’s this thing I’m going through. How can I make it better and more fun? Because whether I like it or not, I’m going through it.
How did you deal with hair loss from chemotherapy?
I loved my hair. My hair and my breasts, I considered my two best assets. I love them. My hair was touching my butt — long, curly mermaid hair — so that was really emotional. I hadn’t had a haircut in forever either so I knew that would be hard.




I decided to throw a hair party. I had a friend, a yoga client, who had a hair studio. He opened it up on a Sunday. I brought friends and family in and we had champagne and sushi. It was a really fun day and a special moment.
I had so much hair come out. I also was able to donate it. I found an organization that makes wigs for young children who have been affected by cancer. I just thought if I can’t have this hair, the thought of little kids running around playgrounds wearing it just made me smile. So I did that.
I started chemo with a little pixie cut and I really thought that I would bypass any emotions about actually losing my hair. I was like, “Yeah, I got this.”
Day 16 was the morning I actually did. It was exactly when they told me it would be. I started feeling like my scalp was really tender. I woke up at 6 a.m. I looked [at] the pillow and there were clumps of hair. I had heard about that when I was starting to read books. I was like, “Okay. This is it. It’s happening. Okay. Okay. We can do this.”
I leave my husband in bed and I go to the shower. I had read that you could rub it out when it was wet in the shower so I’m rubbing it out more and more. I’m looking at the floor and [there are] clumps. They look like little wet hamsters all over the shower floor. I’m trying to build myself up like, “Okay, okay, you’re good. You’ve got this.”
The steam got to be so intense that I thought I might pass out in the shower so I stumbled out. The moment that I was not prepared for was looking in the mirror. These patches of hair and zigzags. I had no idea who was looking back at me in the mirror.
I lost it, just started screaming. My husband came in and I was just like, “Get it all out now! Get your shaver!” And he’s like, “But my shaver won’t work on heads. It’s only for faces.” And I was like, “Go buy one!” I grabbed scissors. I started cutting this part [in front]. I was a disaster. I can laugh about it now because it’s one of the funniest stories but at the moment, it was so dramatic. Finally, a few hours later, he had gotten the shaver. I charged it and just shaved it all off.
It was so interesting to look at the pain behind being bald [and] eventually, losing my breasts or having my breasts replaced. I did have a double mastectomy. These are what make me a woman and beautiful. Those are my beliefs. I looked at them, like, “Is that really what beauty is?” In reality, I know it’s what I think it is but is it? Can I find it anyway?
I started loving being bald. It’s so freaking easy after having hair down to my butt for years. Warm things like the shower felt so good on my head, like a little scalp massage. All senses were heightened. Then it was fun. I’d walk around really proud. I would go to fancy restaurants in Dallas, totally bald but with a really cute dress on. I was like, “I’m going to own this. Whatever. It’s happening. I’m going to own it.”


I think I have this pattern of “It’s so hard” right in the beginning, I freak out, and I let myself freak out. Those emotions are natural and they’re meant to flow. Then eventually, I’ll make peace with it and be like, “How can I make this fun? What can we do here?” I took that mindset to each phase of treatment.
Deciding on breast cancer surgery options
After chemo, then the surgery decision. Chemo shrunk my tumors. It was amazing. It was like magic. It shrunk them down to microscopic level. [There were] barely signs of cancer come Christmas that year.
I had all surgery options — a lumpectomy, a single, or a double. I completely tortured myself [during the] decision-making process because I loved my natural breasts. But, at the same time, I saw that my breasts are very dense. They’re very good at growing lumps. Now, would I have cancer again? I don’t know, but I’d have a lump again and that would mean I’d have to go through ultrasounds, mammograms, and biopsies over and over.
I also had very large breasts for my body. They yanked on my neck and shoulders and I had headaches frequently [so] I was entertaining the idea of what might it feel like to not have [them]. After torturing myself for a long time around the decision, I did choose a double mastectomy for my long-term peace of mind and that felt good for me.
I know it’s always a personal decision. All treatment really is so I don’t judge people. Everyone’s just doing what’s right for them. I’m really happy that I made that decision.
I had my double mastectomy and had tissue expanders put in place. Those are like temporary breasts that go through radiation better than implants. They hold their place better because when you go through radiation, your skin will tighten and shrink.
That surgery was my cancer-free date. They got clear margins. They removed some lymph nodes as well.
Remission
I didn’t hear the news right away. I heard the news in the car with my mom. We were on our way to a park downtown to have lunch. We had just gotten some vegan pizza. The doctor called and [we] pulled over right away. It was funny. She said it in a very sterile voice. She’s like, “The pathology results came back and there is no evidence of disease.” I was like, “I’m sorry, what? What? What are you saying? Are you saying that… Is the cancer gone?”
It was really weird. As soon as I got around, we hung up the phone. We’re sobbing and then we went to the park. [At] that time, I was still healing from surgery. I had drains hidden in a fanny pack underneath my clothes and my breasts were taped up — literally a bra full of tape holding everything together. I’m sitting there at this park in downtown Dallas eating pizza with my mom.
It’s exciting to get that news but, at that point, I still had so much more treatment, too, so you don’t feel cancer-free. I had so much more to come at that point.

What was the next step?
I had some complications [during] healing. I had this thing called cording in my armpit that showed up after surgery. It was weird. I did not read it in the very long list of side effects. These strings developed. Literally, they look like piano chords and they would go from [the wrist] all the way down through my armpit to my breast. I couldn’t lift my arm and it really hurt.
When I first brought it to the attention of my breast surgeon, she’s like, “You’re going to physical therapy right away. We have to resolve this before radiation.” Because when you’re in radiation for breast cancer, you have to hold [your arms up] for 10 minutes and be really still. She goes, “First of all, the cords? They don’t really know the cause of it.” They don’t know. They could last forever. They could be gone soon. There could be more. It was just very unknown. Of course, I freaked out about that.
I went into physical therapy and just loved my physical therapist. She was wonderful. It was like private yoga therapy for healing after surgery. I have a background in yoga therapy, but healing from a double mastectomy, I felt really nervous to push my body. This was unfamiliar territory to me. I tell everyone now, “If your insurance covers physical therapy, do it. Don’t wait for a complication.” I didn’t understand why everyone wasn’t just recommended to do it. I felt it was awesome.
I started healing really quickly. She would massage the cords. They would pop and break apart. It was creepy.
By the time I did have radiation, I had full use [of my arms] and range of movement. That took me into the summer. My tissue expanders were getting filled with saline every week and I literally watch my boobs grow a half size. That was hilarious. And painful as well as they would stretch.
I chose to do reconstruction. Some people choose to go flat. I still wanted to have breasts in some way. They stretched the pec muscle over on top of the implant or, at this point, the tissue expanders so it was painful. It was really intense.
They had to blow me up to a certain size before radiation and they had to blow me up [to] a bigger size on the radiation side. [In] the summer of 2016, I had a lefty super boob. It was just huge because it would eventually shrink more. The tissue expanders don’t move at all. It was weird, but it was nice to know they were temporary.
I had radiation that summer. That went great. As expected, your skin does peel and blister. It’s a really intense sunburn. Underneath was this baby butt-soft, brand-new skin that totally healed.
[The radiation] did some weird stuff like pulled [the] breast up and my nipple to the left a bit. Some women have their nipples removed with a double [mastectomy]. I was able to keep mine because there wasn’t any cancer near it. I got the set of googly eyes forever, but that’s okay.


Maintenance treatment
After radiation, all the big parts of cancer therapy were over. I got on a hormone pill called Tamoxifen, which is to basically block if there were remaining cancer cells floating around, microscopic ones. It would ideally bind the cancer cell’s mouths closed so [they] couldn’t feed on estrogen. That was a daily pill. That actually went great. It was very easy for me.
There I am just kind of released and they’re like, “See you in three months.” I had to wait about a year for that final reconstruction surgery, which is a big deal but it’s also not really cancer treatment. It’s working with a plastic surgeon.
It was a really interesting moment for me because here I am, physically cancer-free. I made it through the biggest parts of treatment and at first, it was exciting. Elating. Then I just got bombarded with so many emotions again: fear of recurrence.
I’m making friends in [the] cancer world and some of them aren’t here anymore. I’m just seeing these other possibilities. Big emotions were coming up.
That was a big lesson. Caregivers or partners have their own cancer journey, too. And to be honest, I think it’s harder at times.
How did cancer affect your marriage?
I was having a really hard time in my marriage. Cancer was connecting us in the beginning and then it started tearing us apart.
We had different views on healing. He was very much into the natural, alternative world and he saw chemo as poison. He thought it would kill me. He doubted everything the doctor said.
He also wouldn’t get help either. I was begging, “Please go to therapy.” It was about a year and a half into the process [when] he finally said yes.
That was a big lesson. Caregivers or partners have their own cancer journey, too. And to be honest, I think it’s harder at times because we’re all dealing with [the] unknown. Cancer is going to do what it does so that’s out of all of our control. But at least with me, I can be empowered in how I treat my cancer, how I choose to live, [and] how I react to things. I can affect that. But he can’t affect that either so it’s like [a] double loss of control. And of course, what’s underneath all of that is fear of losing me. What happened was he emotionally checked out a bit and I felt very unsupported.
Luckily, my mom, with her nursing background, was flying out. She lives in Florida so she was flying out for all the big parts of treatment. She was amazing. My partner was also amazing but he could not show up for me fully with the treatment part so I was just full of so much grief.

I was having a really hard time in my marriage. Cancer was connecting us in the beginning and then it started tearing us apart.

Here I was, cancer-free. And that birthed my whole philosophy of cancer that being cancer-free, true freedom from cancer, it’s a state of mind. It is not a diagnosis. It’s not a physical condition so I had to find cancer-free again in my life. That involved letting these emotions flow, letting the grief come out, and then questioning [the] thoughts [that] cancer will come back [and] the beliefs about my relationship.
Making life changes after achieving remission
I made huge changes in my life. I use the fear of cancer coming back in a different way where I don’t have to live in this constant fear.
It was really clear to me that I was done living in Texas. I’d actually been done 12 years earlier and just didn’t [leave] for many different reasons. But I was ready to go.
I had started spending summers in Colorado. I’ve always loved Colorado. I started writing. I wrote [at] the beginning of my journey. I shared my whole journey on a blog and on social media. It felt really good to write and that was very healing for me, so was sharing, and that connected me with so many amazing people in the cancer community as well.
Some answers became clear. I want to write a book about this experience. I want to help others. I could have fun in cancer. And so I did that.
My relationship was not working for me anymore. [In] the summer of 2019, I’m done treatment, in remission, feeling good, and I’m making big changes. I packed all of my belongings into my [car], separated from my partner, and drove to Colorado to start a new life to put [myself] first and see what I really want.
Bethany moves to Colorado to start a new life. There, she begins experiencing lower back pain. After being told that she didn’t need a scan, the pain worsened until she finally insisted on one. A lower back MRI revealed lesions all over her bones. She shares her story of finding out she had metastatic stage 4 breast cancer.
Read Bethany’s metastatic stage 4 breast cancer story here »

Inspired by Bethany's story?
Share your story, too!
More Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation