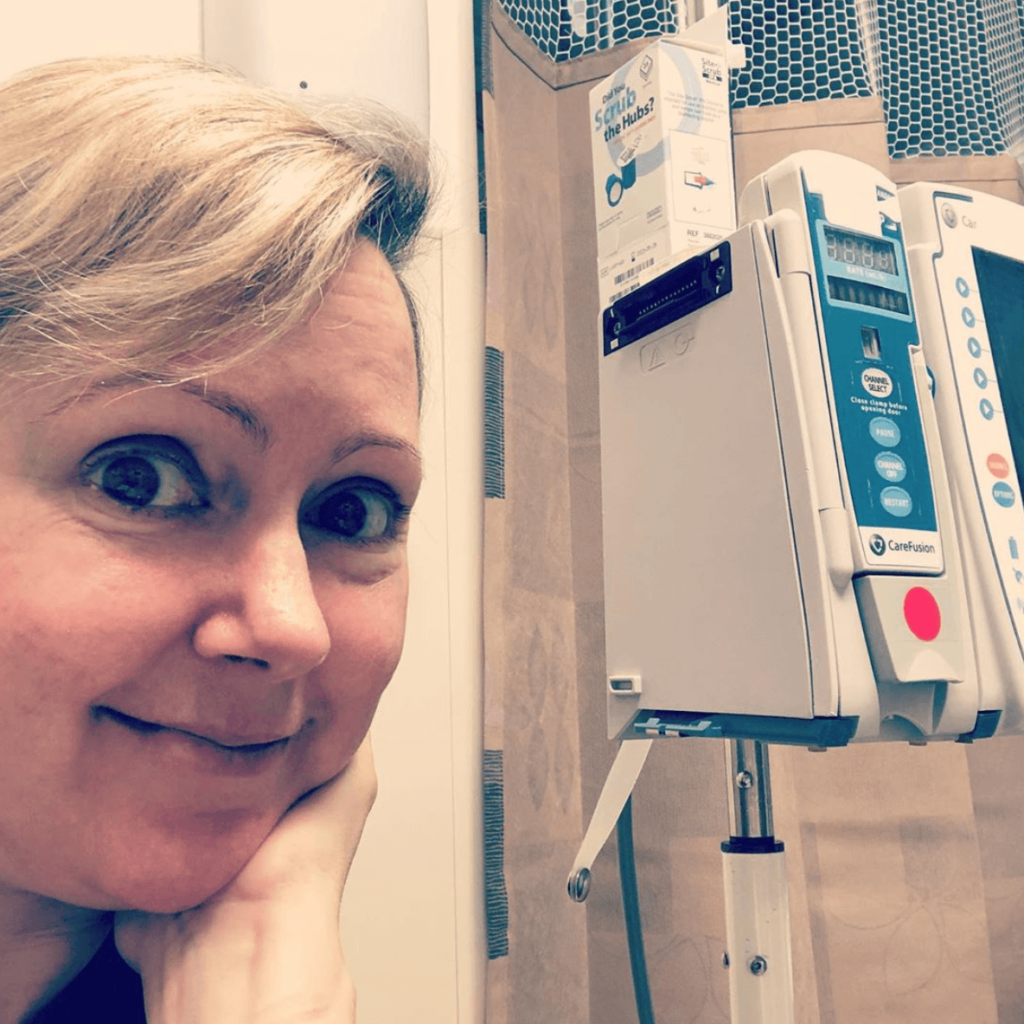
Erin’s Stage 2B-4 Relapsed IDC Triple-Negative Metastatic Breast Cancer Story
Erin shares her metastatic triple negative breast cancer (TNBC) story, one that started after she felt aching in her left breast. She details getting through surgery, chemotherapy, and radiation therapy.
In her story, Erin also highlights important quality-of-life topics, including how the diagnosis impacted her relationship, the importance of patient self-advocacy, and what support helped her most.

- Name: Erin C.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma, triple negative
- Staging: Originally 2B, then stage 4 metastatic
- 1st Symptoms:
- Ache in left breast
- Treatment:
- Surgery to remove tumor
- Chemotherapy
- AC-T
- 4 rounds, infusions every 2 weeks
- Taxol
- 12 weeks, infusions once a week
- Carboplatin
- 12 weeks, once every 3 weeks
- AC-T
- Radiation
- 28 sessions over full breast
- 5 sessions just over the tumor
- 1-time brain radiation
Give yourself time to heal. Give yourself time to feel scared and sorry for yourself, but then you have to choose life.
Erin C.
- Diagnosis
- Chemo & Radiation
- What was your chemo regimen?
- What side effects did you experience from the chemo?
- What was the worst part of chemo for you?
- What’s your advice for someone who’s about to start chemo?
- What was radiation like?
- Did you experience side effects from the radiation?
- How did you feel when you were done with treatment?
- Relapse
- Reflections
- What was the lowest point for you mentally or emotionally?
- What helped you through the lowest times?
- How has your experience affected your work?
- Do you have a support system?
- How has the whole experience changed your perspective on life?
- Can you describe what it’s like to live with cancer?
- How has your cancer affected your relationship with your partner?
- Do you have any advice on self-advocacy?
- It can be hard to ask for help. What are some practical ways people around you can offer support?
- What would your advice for someone who has just been diagnosed be?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis
What were your first symptoms?
I noticed that I would get this little ache in my left breast right underneath my armpit. It was just a twinge. It wasn’t a big deal. Then, I noticed any time I fell asleep on the couch on that side, it would hurt a little more.
Of course, I went on the internet to find out what was going on. It says categorically that breast cancer does not cause pain.
It said it was most likely a cyst, muscle issues, or from my period. It was a different pain than I get from my period, but I still just kind of ignored it.
I talked to my gynecologist about it. She did a breast exam, and she said they didn’t feel anything. She said that if it didn’t go away in a couple of weeks, we’d see what we could do. That was October. That was a long time before my May diagnosis (the next year).
What made you go to the doctor?
I finally went to get a mammogram when I noticed that the pain was worse one night. When I went to feel it, there was some irregularity in the skin. It just felt like there was a cavern or indentation. I went and looked in the mirror and saw what I now know is called a dimple.
I went online again, and it said 100% it was cancer. That really scared me. I ended up having the mammogram and sonogram the very next week.
What were those first tests like?
That was a bit of a blur. The mammogram came back clear, but I knew that there was something wrong. When I got the sonogram, I pointed very specifically to the place where I was feeling it.
They spent a lot of extra time there with the wand, and they wound up finding something right next to the chest wall.
The mammogram doesn’t pick that area up, so I really had to advocate for myself. If you have small breasts especially, you really need to speak up about where you think something is going on.
After these 2 scans, they said they needed to get me a biopsy right away. I was going to my brother’s wedding 2 days later, so I waited on the biopsy. That was scheduled for when I got back.
What was the needle biopsy like?
That was very traumatic for me because I was deathly afraid of needles. I called my doctor before I left for my trip and when I got back, and no one would give me any Xanax or Valium.
I got there the day of the biopsy, and I said, “Is there anyone here who can prescribe something for me?”
No one could. I just ended up having a panic attack in there, which I knew was going to happen.
When you tell someone you have panic, they don’t listen to you when you tell them you have pain. They think it’s just the panic talking.
I don’t respond to anesthetic like most people do. I feel pain much earlier than the majority of people would. They didn’t give me enough anesthesia, so I could feel them taking the sample with excruciating pain. I could feel the blood dripping down from where they went in.
It was really difficult, and the doctor sort of made fun of me. He was like, ‘You were really difficult, weren’t you?’
How did you process the diagnosis?
They called me on the phone. I didn’t know they could give a cancer diagnosis over the phone, but that’s what they did. The radiologist called me and gave me his cell phone number to call him back.
I was about to go into a rehearsal. It was a Friday evening, so I called him because I didn’t think anything serious would be delivered over the phone.
He answered and said, ‘Your results came back positive. You have cancer.’
It was absolutely shocking. I couldn’t really speak, but then I had rehearsal. I had to bottle everything up and get through it.
I didn’t want to tell anyone because I didn’t know anything. The rehearsal was in my home. I run a theater company, and I was the lead in the play. I couldn’t step away.
I turned to my boyfriend, who was standing there waiting to see what was going to happen.
I mouthed to him, ‘I have cancer.’ The temperature of the room changed.

Meeting with a surgeon
The radiologist was very kind in that he had scheduled an appointment for me with a surgeon the next day, which was a Saturday. She opened up her office for me because I was so young and had no family history. They wanted to get on it really fast.
I did a lot of research the night before. I knew what questions I wanted to ask. She was very kind and took her time with me. She couldn’t give me my staging just yet. They needed to do surgery first.
We talked about my timeline. They gave me the option to do surgery first and then do chemo and radiation. Most people start with chemo, then do surgery, and finally do radiation.
My tumor was supposedly 9 mm, so maybe that was why she decided to do surgery first. Maybe she thought she could get it all and not have to do chemo. I don’t know.
Describe the surgery
During surgery, she found out what she thought was a 9-mm tumor was actually 2.3 cm. I went from what would’ve been stage 1A to a 2B in a matter of a conversation. One of my lymph nodes was also involved.
I went home after surgery to heal, and she told me the pathology and staging at the follow-up. I was shocked about that size. She didn’t handle my shock the way I wanted it to. The person I had in my consultation was not the same person who was giving me my test results.
I had the opportunity to switch surgeons at that point, and I did. The surgeon, at that point, was the one in charge of all my care and appointments. I just didn’t feel comfortable with her anymore, so I made the switch.
Switching medical treatment centers
I had a consultation with an oncologist and radiation oncologist. Both of them were at different hospitals. They sent me to Mount Sinai for my medical oncology. I went to a radiologist that was a little bit farther away.
When I went back to the medical oncologist, I asked him if I could change my radiation to the same place. Then the oncologist referred me to the surgeon there to do my port placement.
Then I had everything in the same place, so that was nice. Plus, the staff at Mount Sinai are all so great. They all worked so well together and with me. They have a breast center there, too, and that made everything so easy.
Chemo & Radiation
What was your chemo regimen?
I did AC-T. I had Adriamycin, which they call the “Red Devil” because it’s literally red. Then I had cyclophosphamide. I did 4 treatments of each of those with treatments being every 2 weeks. That took 2 months.
Then I switched to Taxol and carboplatin. I did Taxol once a week for 12 weeks, and I got carboplatin once every 3 weeks for those 12 weeks.
»MORE: Read patient experiences with AC-T chemo
What side effects did you experience from the chemo?
During the infusions, things went pretty smoothly. From the steroids, I gained weight. That was totally not fair. Most everybody on breast cancer treatment gains weight because of the treatment, unless you have nausea and vomiting.
I had limited nausea. I experienced some neuropathy, especially in my feet. That made it hard to wear high heels because I couldn’t feel my toes.
I also felt like I had the flu. I was tired and achy. I wasn’t much fun to be around. I tried really hard to keep my energy and mood up, but it wasn’t working all that well.
I did lose my hair. I was using a special service called cold caps. I had difficulty with them. They worked to keep about 50% of my hair, but I’m a bottle blonde. I dye my hair, so it was dry that it broke off. I needed to get a wig anyway.
»MORE: Cancer patients share their treatment side effects
What was the worst part of chemo for you?
Losing my hair, for sure. I had all the emotional junk you get from losing your hair without the physicality of it. I only lost half of my hair, but I still didn’t get what I wanted from the cold caps.
What I wanted was to keep my long hair. I’m an actor, so my hair was everything. All the sudden, I was rethinking everything. That was very, very hard.
What’s your advice for someone who’s about to start chemo?
I’m a fan of reading and researching, but you just have to know where to draw the line. Read what you can handle, don’t believe everything you read, take what you cant to your doctors, and ask questions based off of what you read. Don’t take information off of the internet as gospel.
Advocate for yourself. If you’re not good at it, grab a friend who can do it for you and take them with you. If you don’t pay attention to your body and speak up, your doctors won’t know what they need to do for you.
Get a port if you can manage it. I had 2 infusions via my veins, and it was awful. If you can at all get a point, do it.
Don’t listen to all the fears you read on the internet. Just discuss it with your doctor as an option because intravenous chemo collapses your veins and is just terrible.
What was radiation like?
I had 33 radiation sessions. I did them every week day. Of those, 28 were over my breast. They tattooed me under my arm. The last 5 sessions were boost sessions. They did that right where the tumor was, just on the tumor.
It was challenging more than anything. When you get radiation to your chest area, they obviously don’t want to irradiate your lungs or heart. You have to do these breathing exercises and hold your breath for certain amounts of times during the session.
They had this special test that measured the rise and fall of my chest. I would have to breathe in far enough for the machine to be able to radiate.
My mind was on the breathing and not the radiation whatsoever. I would be anxious, and then I would focus on my breathing. That would keep me calm.

Did you experience side effects from the radiation?
I had fatigue, but luckily no nausea. My only skin issue was just a slight redness on the actual area. It was like a mild sunburn. It wasn’t painful, and that’s pretty atypical.
Most people have quite a bit of discomfort and burns with that much radiation. I just didn’t. I did absolutely everything the doctors told me to, though.
I put lotion on it several times a day and all that stuff. I don’t know if that’s what made a difference, but I didn’t have any major issues.
How did you feel when you were done with treatment?
After radiation, that was it for treatment. I’m triple negative, which means I’m negative for 3 major causes of breast cancer.
For everyone else, they have the hormone therapies. With triple negative, you don’t have to do any of that.
I knew I didn’t have any evidence of disease after surgery. The radiation was preventative. Even though I knew I didn’t have any evidence of disease left, it was still so nice to be done with treatment.
I didn’t really have a ‘woohoo, remission!’ day, but knowing I didn’t have to go through any more treatment was great. It was just so nice to know that all the treatment I’d been through had worked.
Relapse
How did you find out you relapsed?
In September 3 years later, I started feeling sick. I thought that I had pneumonia. I got treated for that, and then in early October, I had another X-ray. They noticed there was something in my breast.
He said, “Just call your gynecologist. It’s probably just a cyst.” I was like, “Uh, you know I’m a cancer survivor, right?”

Still, I thought maybe it was a secondary cancer, and it was no big deal because I could get restaged and all that.
I went to go get my regular mammogram in October, and they didn’t find anything in the mammogram. I got the sonogram, and I pointed at the spot in the X-ray. They did a very long sonogram trying to see what was on the X-ray.
When they were done, they said they needed to do a biopsy because they did see something. At that point, I was just absolutely crestfallen.
Being in the mammogram, sonogram, and biopsy, there was a lot of PTSD because it transported me back to the first time around. I was very upset.
I was told that I did have breast cancer again when the results came back. They scheduled me for a PET scan to see if it had spread anywhere else.
I got those results in person. A younger doctor under my oncologist came in and told me I had growth to my lungs. Of course, I started crying.
It was a very surreal and upsetting experience. I couldn’t figure out how the X-ray to my lungs didn’t show the cancer there. I guess it was small then and very fast-growing.
Next steps for lung metastasis
He said he needed to do some testing. He needed to biopsy the lung tumor. That would tell him for certain that was breast cancer that had spread to my lung rather than lung cancer.
They opted to do surgery for that biopsy rather than a needle biopsy because of the location of the tumor. I did that within 2 weeks of finding out I relapsed.
They ended up taking out the entire tumor, which was fantastic. They hadn’t planned to do that, but they got in there and saw they could.
When they tested the tumor, they found out that it responded to androgen as a hormone. They said if they inhibited that, it should make the tumor shrink.
I started a 2-month protocol and did that through January 2019. It was just a daily pill I took in the morning. I didn’t really have any side effects from the medicine.
Then I started getting tired even easier. I had more and more symptoms from the lungs. I kind of just thought I wasn’t over the pneumonia yet.
But at the end of the treatment, they saw that the treatment hadn’t helped at all. I got that news in February, a few months later.
The tumor had grown from nothing to 5.7 cm in a matter of months. My oncologist was in a panic. He was like, “We have got to get you into something. A clinical trial or something.”
Then it was discovered that I had metastases to the brain. That put everything else on hold. I got radiation in my brain in March.

Describe the radiation for your brain metastasis
That was really freaky. The mask was scary. Your whole head is held down to the table. At that time, I was having a really hard time breathing because of my lungs and was coughing a lot. That, plus the claustrophobia, was not fun.
The session was divided into 2 parts. They were half-hour treatments, and I could take as much time in between as I needed.
I could even take the mask off if I needed to. Luckily, I only had to do that once, and it cleared it up. It took care of it.

New chemo regimen
I was going to start a clinical trial the week after brain radiation, but it turned out that there was a waiting period after getting radiation done if you were going to be in the trial.
My doctor cancelled it, and we started chemo that day instead because I had already waited long enough. I was suffering with the breathing issues. He just wanted to get me started.
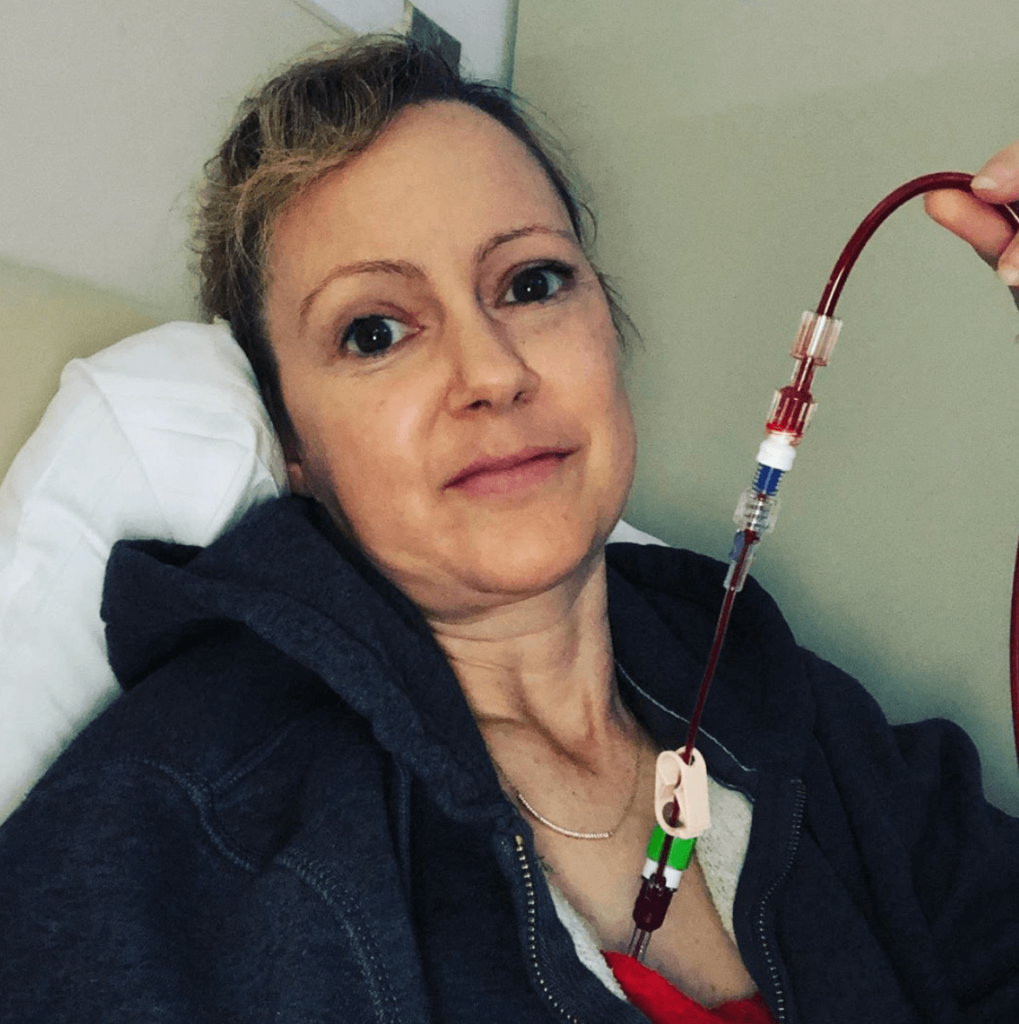
I’m on Gemzar and carboplatin right now. That’s ongoing. I’ve been doing that since March 2019.
I have chemo 1 day every 2 weeks, then I have a week off. I’ll be doing that indefinitely.
Gemzar and carboplatin side effects
I’m not having side effects this time around. When you’re early stage, they want to nuke you so it doesn’t come back. This is milder chemo.
This is like, “There is no cure, so we want to give you the best quality of life.” The amount of chemo is pretty small, so I’m very lucky.
What’s the check-up protocol?
I have exams every week. Then every 3 months, I have a brain scan, a bone scan, and a CT scan for my lungs to check in. The tumors have shrunk down quite a bit from this chemo.
The cancer itself caused me to lose my appetite, so from January until about early August 2019, I had severe issues with appetite and lost about 40 pounds.
I don’t know what it was about the cancer that was making me feel that way, but I know it was the actual illness because that was before chemo started. I’m better now because the tumors have shrunk, but it was rough for a while.
Reflections
What was the lowest point for you mentally or emotionally?
Right after chemo started, when I was at my worst in terms of my health. I just couldn’t breathe. I was sleeping on the couch. I was sleeping with a breathing machine.
I couldn’t walk anywhere. I have a 2-floor walkup. Stairs were a major issue. I couldn’t really leave the house at all.
It was just miserable. It really impacted me mentally as well. I was just depressed. I just felt so sick. I didn’t have time to feel anything except so sick.
What helped you through the lowest times?
Chemo, mostly. It has made me feel so much better. I also started taking Lexapro and Abilify. I had been on them prior to this whole thing, but I couldn’t even take my medication because I was so depressed and out of it.
Once I started taking my medication again, my appetite came back. That was interesting to see how that helped.
How has your experience affected your work?
With my theater company, we’ve kept going. I’ve been performing through all of my treatment. It just had to be done. I don’t know how I survived, but I did. It was not easy. The rest of my acting life was put on hold.

Do you have a support system?
I feel very lucky. I live with my boyfriend, so he’s like a round-the-clock caregiver. We have a huge friend group here in New York.
We have a lot of people who have been very supportive financially and emotionally and in every way. People have brought me food, which is wonderful.
My mom has also been amazing. She doesn’t live here, but by phone, she has been a huge support to me. I’ve been to out to see her 3 times since I was diagnosed, too, so that’s been nice.
How has the whole experience changed your perspective on life?
It’s really hard to realize that there is a life expectancy put on you. The average lifespan for my cancer is 5 years.
Now, I no longer get to think about growing old. I do think about it sometimes, but in a, “Well, that’s not going to be me,” way.
All the sudden, a bucket list becomes important. I run into issues with money a lot more now. How do I create enough money to do all the things I want to do before I die?
I’m just trying to keep a positive attitude as much as I can.
I say the things I want to say. I just try to live my life. It’s taken on a new quality to it. I don’t spend my time doing things I don’t want to do. I factor the value of my time into everything.
Can you describe what it’s like to live with cancer?
It’s really isolating. The amount of support I need to get through things makes me feel very guilty.
I feel like people are going to get tired of me. I end up feeling bad a lot when I have to ask for help. That is a pervasive feeling for me.
People have been very kind. I get no indication from anyone that they’re fed up with me or anything, but I still just feel that way sometimes.
»MORE: Read different experiences of a cancer diagnosis and treatment

How has your cancer affected your relationship with your partner?
We’ve had some ups and downs. It’s really scary for him. He didn’t know how to handle the diagnosis. He got thrust into caregiver mode, and he can barely take care of himself.
One time, he told me, “This is so unfair. This is not where we’re supposed to be in our lives.”
Things are really good, though. We’ve been lucky enough to go to counseling. It’s sponsored by the chemo center. I don’t have to pay for anything to go. That just helps us navigate the disease together so neither of us are by ourselves in it.
Do you have any advice on self-advocacy?
Take notes in your appointments. That will help you to know if something is different from time to time.
I would recommend bringing someone who is more of a bulldog about things if you would rather them advocate for you.
It can be hard to ask for help. What are some practical ways people around you can offer support?
Reaching out and saying hello is always welcome. If the sick person doesn’t get back to you right away, it’s no big deal. They’re sick and tired. Try again.
Financial help is obviously always appreciated. Everyone going through cancer should consider a GoFundMe or something similar. Even meal trains are so helpful. A lot of people want to help but don’t know how. Meals are a great place to start.
»MORE: What kind of support cancer patients say helped the most
Being able to talk about my situation with other people is great. I love when people comment on my posts and genuinely want to know how I’m doing. It makes me feel less isolated.

What would your advice for someone who has just been diagnosed be?
Give yourself time to heal. Give yourself time to feel scared and sorry for yourself, but then you have to choose life. You’re going to go through a lot, and it’s going to be really hard.
If you’re early stage, it’s very treatable, and the treatment will fly by. It doesn’t seem like it, but it will.
When you’re done with treatment, that’s when the real work begins. When your physical health is under control, that’s when you have to fix whatever was broken and couldn’t take priority as far as your mental health.
With stage 4, you have to go on with your life. This is the only life we have, so you have to just grieve and then just don’t feel guilty for one second about living your life.

Inspired by Erin's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation





















One reply on “Erin’s Stage 2B-4 Relapsed IDC Triple-Negative Metastatic Breast Cancer Story”
I have had cancer of breast two times. Last ductal carcinoma, one year later diagnosed with another cancer. Double mastectomy followed by chemotherapy and radiation. Infections on right implant and had to be removed. Left with lymphedema and severe numbness in feet. Thankful for treatment. I constantly remind myself that I will be well no matter. If my journey ended I am grateful for the kindness and hope given by healthcare providers, my caregiver and friends. Be well my friends.