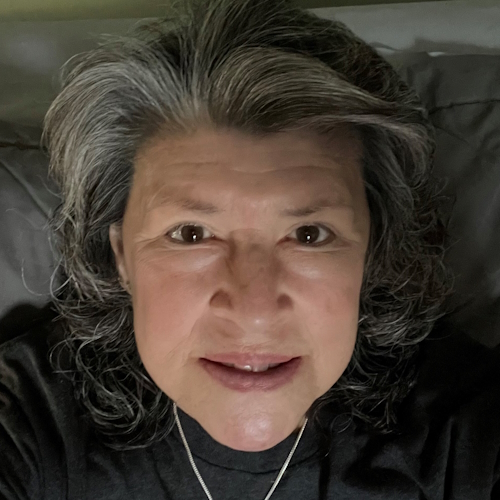
Alesia’s Diffuse Large B-Cell Lymphoma (DLBCL) Cancer Story
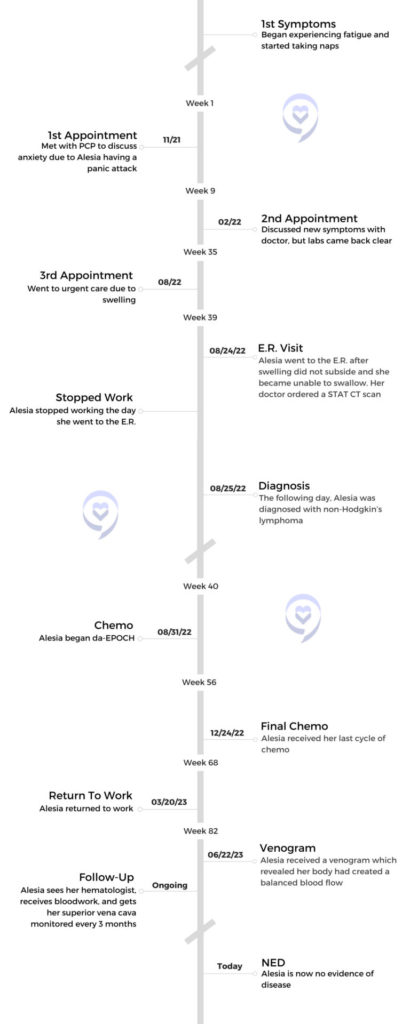
As a kindergarten teacher, Alesia assumed her fatigue, shortness of breath, and swelling around the face and throat were work-related symptoms or simply allergies. It wasn’t until her throat became swollen to the point of being unable to swallow that she visited the E.R.
At the E.R., doctors discovered a 10-centimeter tumor in her chest. Alesia was shortly thereafter diagnosed with diffuse large B-cell lymphoma (DLBCL). She began chemo cancer treatments immediately.
Now 4 months in remission, Alesia shares her cancer story with us, including her side effects from dose-adjusted EPOCH and rituximab, struggling with hair loss, coping with the mental toll of a cancer diagnosis, and her advice to those on their own cancer journeys.

- Name: Alesia A.
- Diagnosis (DX):
- Non-Hodgkin’s Lymphoma
- Diffuse large B-cell (DLBCL)
- Primary mediastinal
- Diffuse large B-cell (DLBCL)
- Non-Hodgkin’s Lymphoma
- Symptoms:
- Fatigue
- Shortness of breath
- Swelling around the face and throat
- Night sweats
- Anxiety
- Age at DX: 31
- Treatment:
Feel your feelings. Take hold of your thoughts. Find support groups, whether it’s family, friends, or community online, and definitely be an advocate for yourself because you need you.
Alesia A.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Scans
Tell us about yourself
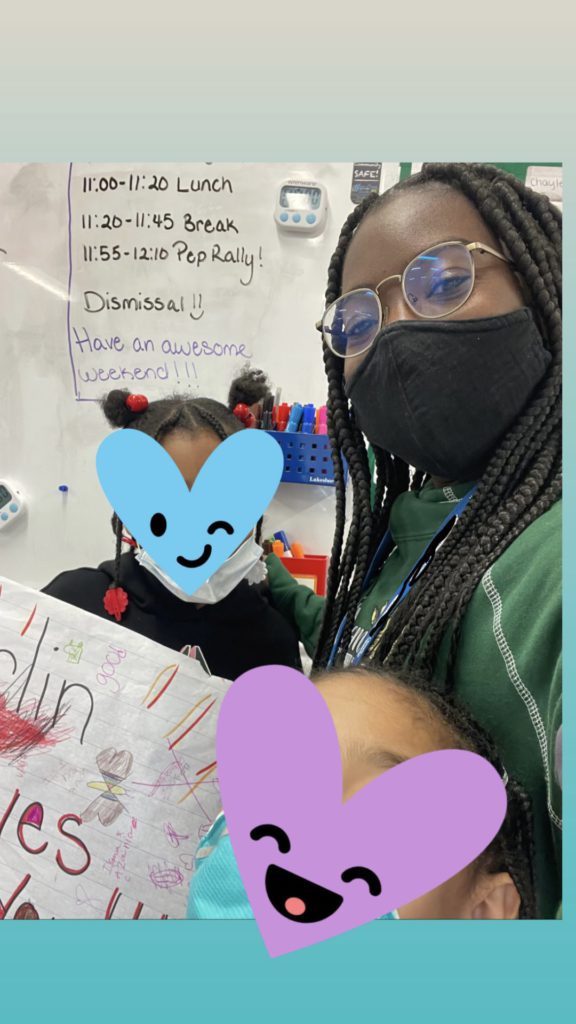
My name is Alesia. I’m 32 years old from South New Jersey. I am a kindergarten teacher. I work as a teacher in Philadelphia, and I really enjoy that. I’ll be going into my fourth year of teaching, so I’m really excited. In my free time, I like to do photography, be with friends and family, get ice cream, enjoy the summer, go to the beach, and things like that. The simple things.
What were your first symptoms?
I just brushed it off like I’m stressed, I’m working, I’m tired, I’m not exercising enough. Maybe that’s why I’m getting shortness of breath.
It all started during my second year of teaching. I didn’t really start experiencing symptoms until around November of 2021. My main symptom was fatigue. I would get really tired.
I also noticed a little bit of shortness of breath. At my school, we would have to take the stairs to go up. Usually going up the stairs, I’m like, this is great, this is exercise. Then after a while I’m like, why do I feel like I’m getting winded after only the second staircase? But I didn’t think anything of it. I was like, maybe I just need to exercise more. Those were the 2 main symptoms that I started to experience.
I just brushed it off like I’m stressed, I’m working, I’m tired, I’m not exercising enough. Maybe that’s why I’m getting shortness of breath. Being an anxious person, experiencing panic attacks, feeling chest pains, maybe it’s COVID. That’s what I was experiencing all of that year, and it was unexplainable things.
It started to gradually increase as the year went by. From springtime into summer, I found myself taking naps. I was a person that never did naps, but I did naps and the naps would take 4 hours. Even my family was like, “This is odd. Are you okay?” I’m like, I’m just really tired. I would sleep 8 hours and wake up. I remember being in a church service and dozing off. I was like, oh my gosh, what is happening to me?
It wasn’t until July of 2022, I started getting moon face swelling in my throat and in my face. It started in my eyes, but then it got even worse, to the point where I couldn’t swallow. I was like, okay, this isn’t good. All this time I’m thinking maybe it’s allergies, but now that I can’t swallow, I need to go to my doctor. Those were all my symptoms, especially having night sweats.
Were night sweats common for you?
No, I never had night sweats like that. Waking up and having to change my bed sheets and my pajamas. It was very odd. It’s springtime or summer so it’s in the 80s and I was like, it’s really hot.
Did you have any indication that it could be cancer?
My primary doctor took me in, and right away, she did not like what she saw.

I honestly had no clue. I thought it was allergies. Crazy enough, when I couldn’t swallow, I still went to work. Confessions of a workaholic. My principal and co-worker were like, “Please go see your doctor,” so I did. I left work and they took me. My primary doctor took me in, and right away, she did not like what she saw. She ordered STAT CAT scans of my neck and everything. She said in the meantime, “I’m going to order you an EpiPen. Change your sheets if it is allergies because we don’t know what this is, but let’s take all the necessary precautions.”
Getting further tests and scans to reach a diagnosis
Doctors and fellows were constantly coming to me like, “This is mostly likely a tumor, and the size of it is crazy big.”

Everything happened so quickly. After that initial CAT scan my doctor ordered, I did it right away and she got the results back fairly quickly. She told me, “There’s some type of mass in your chest. I want you to go to the E.R.” I’m like, mass? Oh, my goodness. But I was still hopeful it was just a cyst or something. You don’t want to think anything bad.
I went to the E.R. and had constant communication with my family, letting them know what was happening. I got there around 4:00 or so. That night, I had another CAT scan. They did a bone marrow biopsy. Doctors and fellows were constantly coming to me like, “This is mostly likely a tumor, and the size of it is crazy big.” There were a good amount of tests that I had during that initial diagnosis.
Diagnosis

How did you process possibly having a tumor?
I really couldn’t. I was staring at the doctor, like, okay. It was just really hard for me to wrap everything around it until the actual chemo bag was hung like, oh, this is actually happening.
»MORE: Reacting to a Cancer Diagnosis
How soon after going to the E.R. were you diagnosed?
My diagnosis was the day after, August 25th.
What was your diagnosis?
My diagnosis came back as non-Hodgkin’s lymphoma diffuse large B-cell and my subtype was primary mediastinal B-cell lymphoma. I was diagnosed on August 25th, 2022 with a 10-centimeter-sized tumor in my chest.

How did you react to your cancer diagnosis?
It was just a sigh of relief. Literally, a sigh of relief. Like, I wasn’t crazy. Because like I said, all that school year, I thought something was wrong with me but I couldn’t pinpoint what it was. Having anxiety, panic attacks, being so tired. I was blaming everything on work, but I just knew my body was off and I felt like I couldn’t explain anything that was happening to me. It was scary. But honestly, it was just a sigh of relief. Like, there’s finally an answer and I’m seriously not crazy.
Did you have anxiety prior to cancer?
That’s something that I’ve had before.
Treatment & Side Effects

Losing my hair was very traumatizing. I didn’t think it would happen so quickly.
What cancer treatments did you undergo?
I was on the regular med search floor. The oncology team came to me and they’re like, “This is the plan. We’re going to move you to the oncology department and then we’re going to lay everything out. We’re going to start treatment right away.” They did that quickly. Then they came to me and had all the paperwork, explanation, and information about the type of treatment that they were going to start me on.

They started off with, “This is the type of cancer that you have and this is the type of treatment that will work well for you.” I was started on dose-adjusted EPOCH. What it looked like was, I would have to have treatment every 3 weeks, 5 days inpatient and it’ll be continuously running for 96 hours. It was a very, very intense treatment, followed by rituximab outpatient.
What side effects did you experience from cancer treatment?
My side effects were definitely nausea, hair loss, and extreme fatigue. I did have a short time of problems with edema, then we figured out what was happening. It was part of the prednisone treatment, so they had to cut back because I would swell a lot in my arms and in my face which was causing problems.
»MORE: Cancer Treatment Side Effects
How did you process your hair loss?

I was definitely worried about it. For me, my hair was part of my identity. I had very big hair. I was usually known for my hair. I loved doing my hair. I always had braids or kinky twists in my hair, different styles.
Losing my hair was very traumatizing. I didn’t think it would happen so quickly. It was after my first treatment. I had braids in, so I was planning on doing one last hurrah hairstyle. My mom was helping me and she was trying to tell me, “I don’t know if this is going to work out. There are chunks coming out, but we can keep trying.” It didn’t work out.

What would you say to someone experiencing hair loss from chemo?
It’s okay to grieve and you can grieve however long it needs to take. Because it was literally a part of you. It’s something that made you who you are or who you were. But there can be new beauty in it and a new level of trying to learn how to love yourself however you may look. Know that you are still you but you’re becoming someone better.
How did you cope with the side effects of treatment?
I took a lot of rest and tried to drink fluids. I didn’t do anything crazy, but I watched what I would eat and paid attention to what made me feel good and what made me not feel good. It was a little hard because I couldn’t eat as much. I had a loss of appetite. I took it easy and tried to move around as well.
There can be new beauty in it and a new level of trying to learn how to love yourself however you may look. Know that you are still you but you’re becoming someone better.
The mental aspect was hard because cancer in general is just a traumatic experience, let alone being in the hospital for 5 days just sitting in the room. I did make a point to take laps around the nurse’s station. I would bring things to help me feel better, like my Bible or my coloring books and crayons, my video game systems, and books. Anything that could help me deal with that space for a long period of time.
I’m not going to dismiss the fact that it was really hard. There were times when I lacked the motivation to participate in any of the things I had, like reading or anything, because the focus wasn’t there.
Sometimes it did feel lonely, but I did have and I still do have amazing support. My mom has been with me throughout my treatments. My brothers will make it a point to visit me. I’d have friends visit me and keep in touch with me. Those things helped me get through it, but the mental aspect was definitely hard because time kind of stops when life is still moving for your friends and family. That was just hard. It’s like, you’re getting treatment and you have to stop your life to undergo treatment. I came out of it and now I’m picking up where I left off.

Survivorship
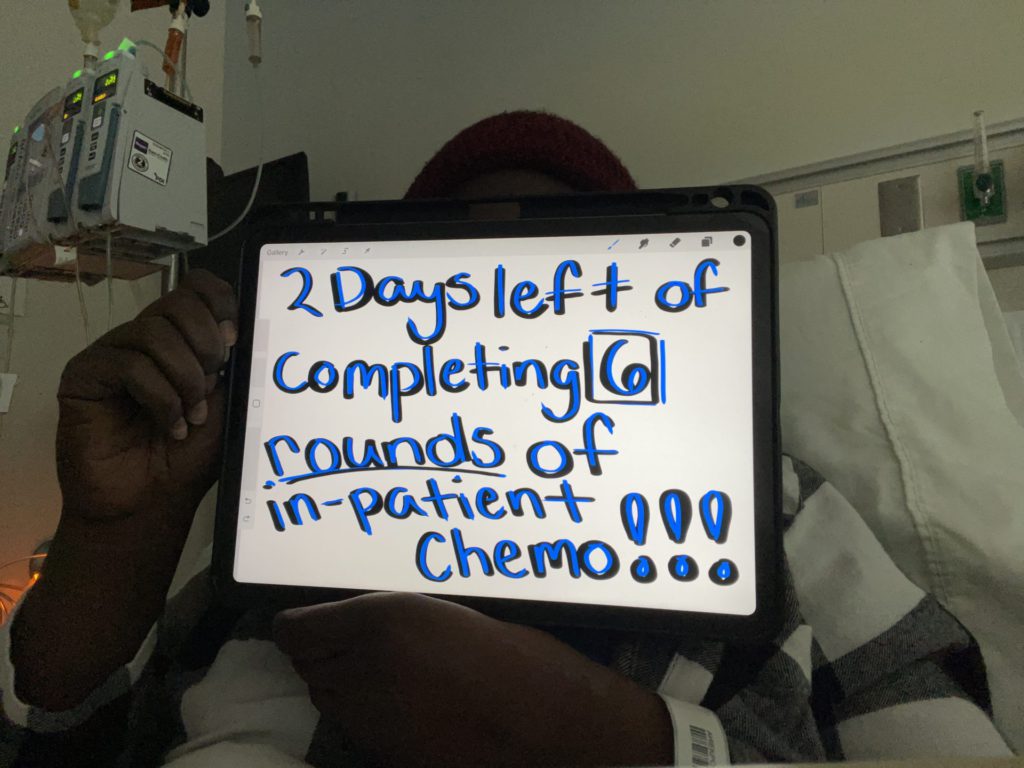
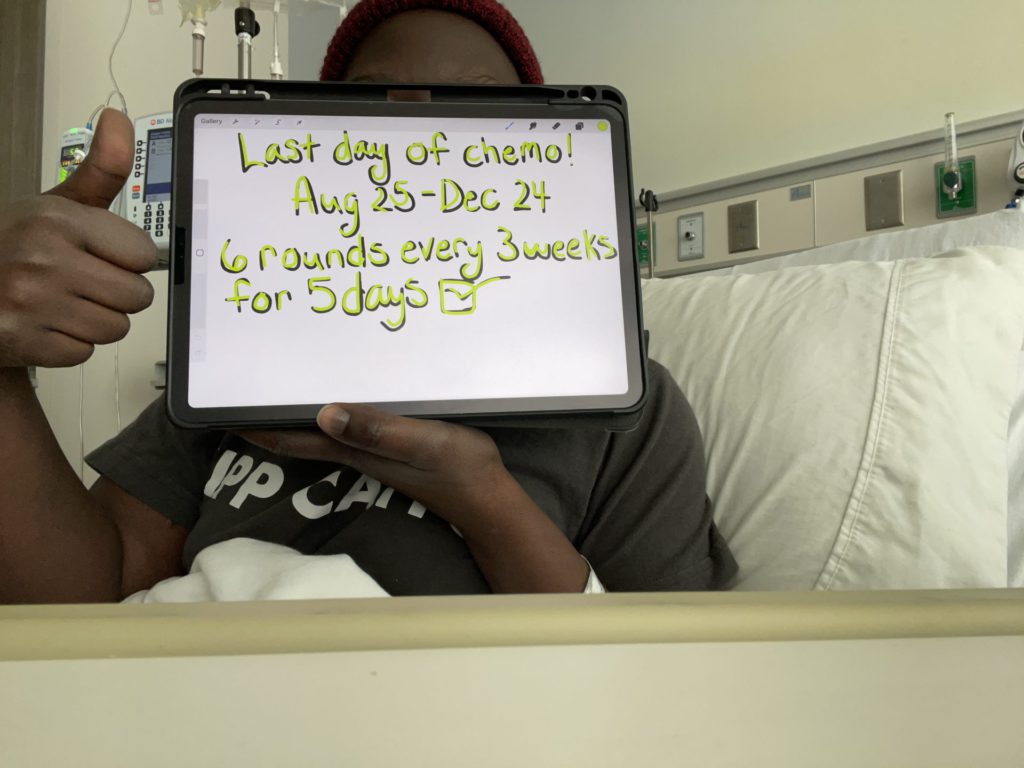
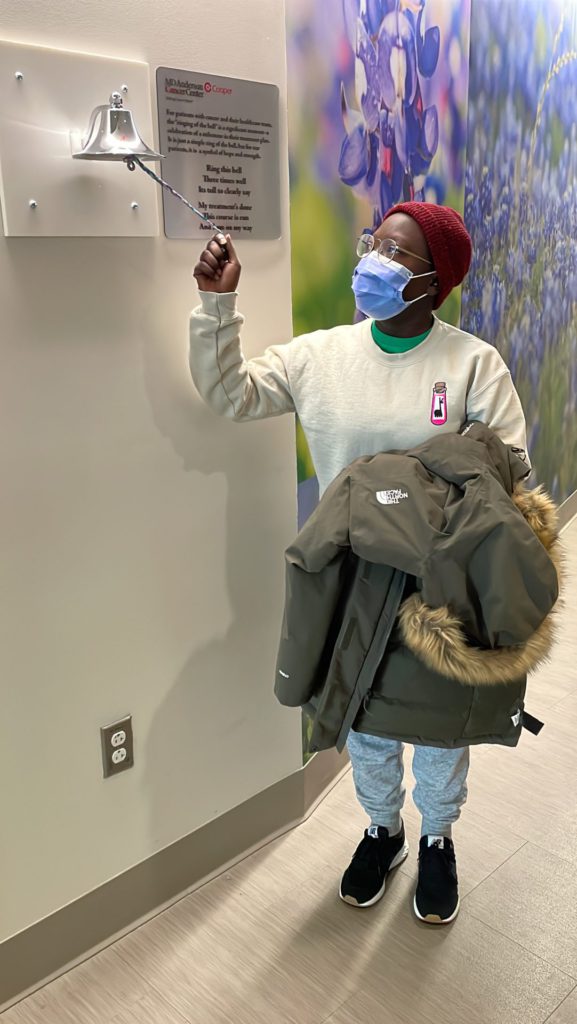
Did you finish your cancer treatments?
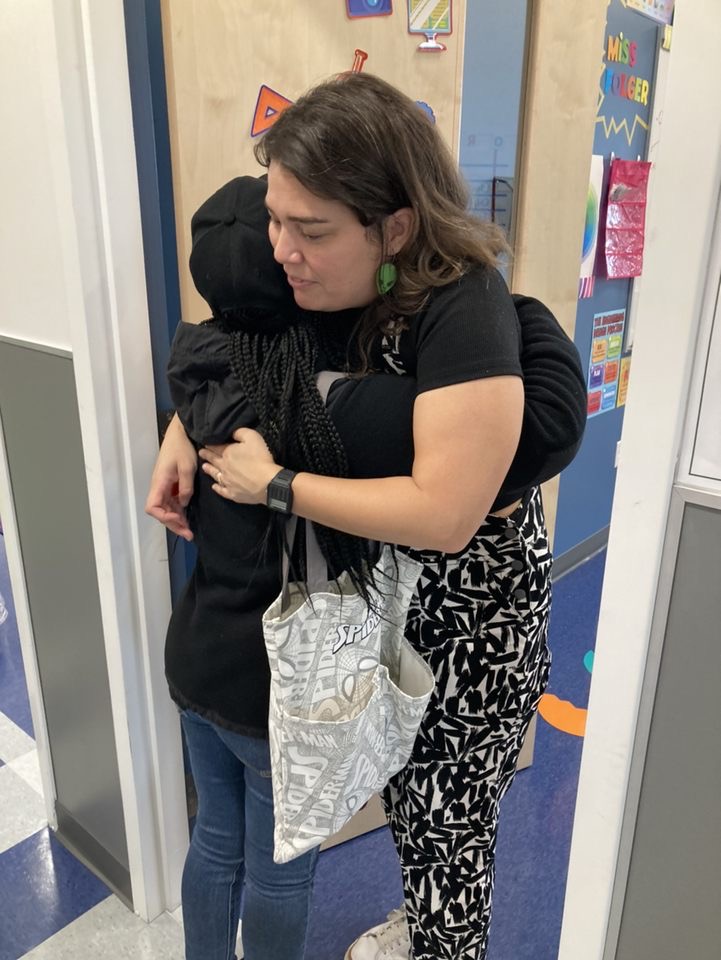
I finished treatment the week of Christmas and I took off about 2.5 months. I went back to work at the end of March which was good for me. I wasn’t sure how long I should wait to go back to work, but I figured around that time would be good because it will only be a short amount of time before summer break.
Did you have follow-up scans after your treatments ended?
After treatment, my doctor wanted to wait a few weeks for the treatment to, as she says, marinate within my body to get its last work in before my PET scan. It’s about 2 or 3 weeks out before I had my PET scan. Then a week in between when I saw my doctor. At about 3 weeks, I had my PET scan, and then in a week, I saw my doctor which was nice. The PET scan was part of my medical [procedure] at the hospital. So when they got the results, my doctor was able to see it and message me, “These are the results. Don’t worry about it. I’ll see you soon and we’ll talk about it.” So that was nice.
What were the results of that last PET scan?
The tumor had shrunk significantly to the point where I’m no evidence of disease, so I was good to go. She’s like, “I will not see you again until your next checkup,” which was nice.
How does it feel to have no evidence of disease?
It’s just a breath of fresh air. It’s just like, I don’t have to deal with this anymore.
How frequently do you get scans now?
Not as much, because my doctor doesn’t want me to get a lot of scans for risk of any kidney problems.
I just pray, take breathing techniques, and try to think of the positives instead of the negatives. Or think more positively than negatively, because I’m still going to think negatively.

Post-cancer swelling issues

I’m still having issues with my swelling. My tumor was in my chest and encased the superior vena cava vein, so it scarred that vein shut, which is my major vein that causes the blood flow to go through my arms and circulate through my head. That was the reason for the swelling. Since that scar shut, now I’m having superior vena cava syndrome, or SVC for short. I’m still experiencing some swelling like I did before the diagnosis.
I, unfortunately, did have to go to the E.R. again because I did feel a little bit of that swelling in my throat. But everything is still good. No relapse or anything, but I did have to get a CAT scan and potentially stents. I had that procedure about 2 weeks ago, which, good news, I didn’t need stents because my body made new pathways for the blood to circulate. But it’s something that will have to continually be followed up on. So the next scan, unless my doctor says anything else, will be 6 months out.
Do you experience scanxiety?
The scanxiety is so real. It’s the thought of “what if.” I definitely don’t want to think that way, but it’s just that natural, normal thought and feeling. I just pray, take breathing techniques, and try to think of the positives instead of the negatives. Or think more positively than negatively, because I’m still going to think negatively.
It’s, unfortunately, something that I’m going to have to endure lifelong. It’s going to be a constant battle of stress and PTSD. But knowing that I’m good and continuing to believe that I’m good.
Reflections

Feel your feelings. Take hold of your thoughts. Find support groups, whether it’s family, friends, or community online, and definitely be an advocate for yourself because you need you.
What would you say to someone currently on their cancer journey?
The journey is definitely a hard one, and I don’t want anyone to feel dismissed for their emotions or their thoughts. Their emotions and thoughts are valid and you are able to express the way that you need to express yourself. If you need to get angry, get angry, get sad, feel all those emotions.
Find community. Community can be hard sometimes, but there is an amazing community within cancer support groups. A big support group online like Facebook and Instagram, I found and they have been helpful throughout the journey.


Family and friends, be real with them. It’s okay to be real with your loved ones and let them know that they will never understand. But for them to know how you’re feeling and to give them a chance to hear you and try to be in your shoes.
Don’t give up. Continue to believe and hang on to hope. And be an advocate for yourself. Don’t be nervous or feel like you’re bothering your medical team. Be on them. Take every note that the doctor says. Ask if it’s okay to record what they’re saying to you. Ask if there are any other options.
Feel your feelings. Take hold of your thoughts. Find support groups, whether it’s family, friends, or community online, and definitely be an advocate for yourself because you need you.
How did you advocate for yourself with doctors?

I’m the type of person that wants to make sure I understand. On my dad’s side, my brothers always ask questions and they always repeat questions like, “Did I hear you right?” It’s kind of like that. Especially since they’re that way, they want to know all the answers, especially if they’re not there in the room with me. That was one of the things.
It was helpful that my medical team said, please ask questions. Knowing that they will sit there with me to answer all those questions, [made me] feel at ease. I know not everybody will get that opportunity or have that type of medical team that will sit with you. But it’s like, no. This is my body. This is what I’m experiencing, and if you’re going to be on my medical team, I want you to answer my questions. I want you to help me understand so that this journey can be easier. That’s what I did. It’s definitely a partnership.
How are you feeling post-cancer?
I’m just happy to be 4 months in remission and continuing to go strong and learning this new normal post-treatment.
More Diffuse Large B-Cell Lymphoma Stories
Lena V., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 1
Symptoms: Blood in urine
Treatment: Surgery, chemotherapy (R-CHOP), radiation
Cindy M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Itchy skin on the palms and soles of feet; yellow skin and eyes
Treatment: Chemotherapy (R-CHOP)
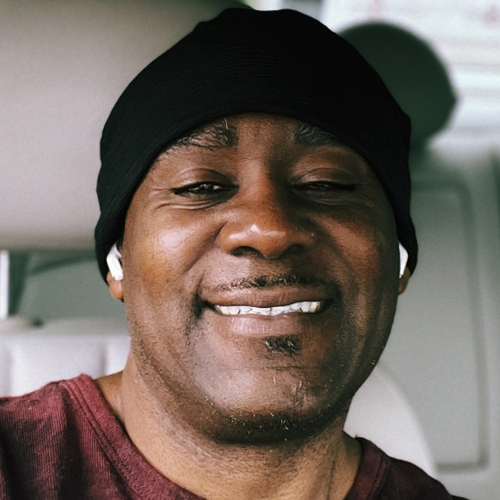
Tony W., Relapsed T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL)
1st Symptoms: A lot of effort needed cycling, body wasn’t responding the same; leg swelling
Treatment: R-CHOP chemotherapy, CAR T-cell therapy
Jonathan S., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Severe shoulder pain
Treatment: 6 rounds of R-CHOP chemotherapy, 10 rounds of methotrexate, 12 rounds of focal radiation, autologous stem cell transplant
Leanne T., Follicular Lymphoma Transformed to DLBCL, Stage 3B
1st Symptoms: Fatigue, persistent cough
Treatment: R-CHOP chemotherapy, 6 rounds
Paige C., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Weight loss, extreme fatigue, swollen lymph nodes in the neck
Treatment: R-EPOCH chemotherapy
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
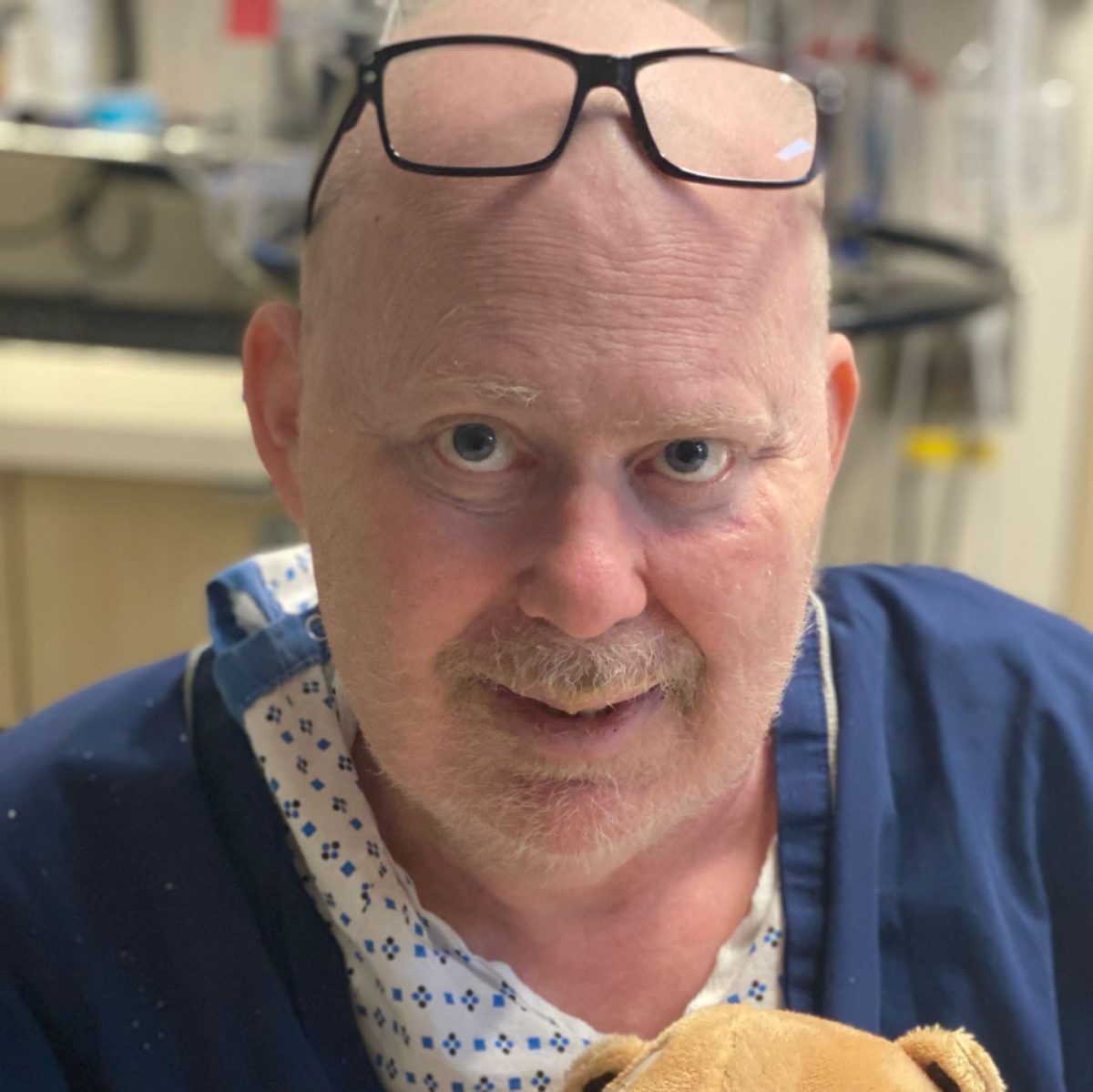
Kris W., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
1st Symptoms: Pain in the side of the abdomen
Treatment: R-CHOP chemotherapy
Robyn S., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL), Stage 2E
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: R-CHOP, R-ICE, intrathecal, BEAM; autologous stem cell transplant, head and neck radiation, CAR T-cell therapy
Barbara R., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Abdomen and gastric pain
Treatment: Chemotherapy R-CHOP, CAR T-cell therapy, study drug CYT-0851
Luis V., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Persistent cough, fatigue, unexplained weight loss
Treatment: Chemotherapy R-CHOP and methotrexate
Nina L., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Hip and lower extremities pain, night sweats
Treatment: Chemotherapy R-CHOP
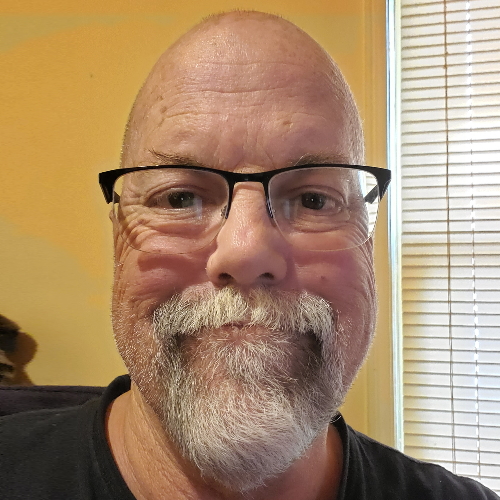
Richard P., Relapsed/Refractory Follicular Lymphoma & DLBCL
1st Symptoms of relapse: Swelling in leg, leg edema Treatment:1st line - R-CHOP chemotherapy, 2nd line - clinical trial of venetoclax-selinexor
Shahzad B., Refractory Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Extreme fatigue
Treatment: R&B, R-ICE, R-EPOCH, CAR T-cell therapy (cell-based gene therapy)
FDA approved: October 2017
Erin R., DLBCL & Burkitt Lymphoma, Stage 4
Cancer details: Characteristics of both subtypes
1st Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatment: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
Emily G., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Pain in left knee
Treatment: R-CHOP chemo (6 cycles), high-dose methotrexate chemo (3 cycles)