Kimmie Ng, MD, MPH
Colorectal Cancer Treatment
Kimmie Ng, M.D., MPH, started her career with research in mind, but after working with patients, she realized her passion was in helping people directly.
A gastrointestinal oncologist, Dr. Ng also founded the center at the Dana-Farber Cancer Institute that focuses on research specifically for young-onset colorectal patients, people under 50 years old, a growing patient population.
In this interview, Dr. Ng talks about the role of the microbiome, the latest on colorectal cancer treatment in targeted therapy, and gives general guidance to patients and caregivers on questions they should consider at diagnosis.
- Name: Kimmie Ng, MD, MPH
- Specialty: Gastrointestinal cancers and young-onset colorectal cancer
- Roles
- Oncologist
- Co-Director, Colon and Rectal Cancer Center
- Director, Young-Onset Colorectal Cancer Center
- Director of Clinical Research, Gastrointestinal Cancer Center
- Associate Professor of Medicine, Harvard Medical School
- Experience: 15+ years
- Dana-Farber Cancer Institute
- Spends most of week on research, one day a week with patients
- Introduction
- Colorectal Cancer Focus
- What's behind this trend of younger colorectal cancer patients
- What is driving the increase in young-onset CRC patients
- How many colorectal cancer patients are under 50
- Patients get bombarded with diet and lifestyle recommendations. Where should they turn for reliable information?
- The benefits of Vitamin D
- The Role of the Microbiome
- Growing Focus on Targeted Therapies
- Guidance to Cancer Patients and Caregivers
Introduction
How did you shift from research to patient care
When I started in college, I actually majored in the molecular mechanisms of biochemistry and really thought that I was going to be in the lab, delving into the intricate complexities of how cells divide and how cancer works and how it spreads.
But as I progressed through my training, going to medical school, and having increasing interactions with patients, it really struck me that I wanted my work to be more directly relevant to patient care.
I wanted the research that I was doing to be able to have more of an impact on the patients I was meeting and treating than I could do from the laboratory bench.
With that, I shifted more to a clinical and translational type of research where I would work on patient samples and analyze tumors, look at diet and lifestyle factors, and see what of those, in combination or singly, could help to make people’s survival better and help them get through their treatment better.
Describe the work you do at Dana-Farber
When I started in medical oncology,I knew from a very early stage that I wanted to focus on gastrointestinal cancers. Specifically, colorectal cancer because there was still so much to do in terms of improving the outcomes and finding new treatments for patients with these diseases.
Very early on in my training, I decided to specialize in gastrointestinal cancer and colorectal cancer. Currently, I see patients one day a week and the rest of my time is spent running the Young Onset Colorectal Cancer Center, which really focuses on young people under the age of 50 who are diagnosed with colorectal cancer, as well as conducting research on the diet and lifestyle factors that may impact how long a patient lives with colorectal cancer.
I also study what some of the risk factors are for why more and more young people are developing colon cancer at younger and younger ages. That is still a mystery. We don’t know in the vast majority of patients why it is they became diagnosed with this disease.
Colorectal Cancer Focus
What’s behind this trend of younger colorectal cancer patients
It isn’t purely a screening effect.
Just to review the overall numbers, colon cancer is the third leading cause of cancer in both men and women in the United States.
When you combine men and women in the U.S., it’s the second leading cause of cancer death. It’s a very big problem that affects thousands and thousands of people every year.
Fortunately, we do have very effective screening programs for people over the age of 50 currently, where they’re able to catch cancers at an earlier stage and also before they become symptomatic, often at the polyp stage where you can completely prevent the cancer.
As a result of those successes of screening, the incidence of colorectal cancer in people over the age of 50, as well as death rates from colorectal cancer have been steadily declining over the years.
Unfortunately, that same improvement has not been seen in people under the age of 50 who are not being routinely screened.
It’s occurring at about two-percent per year in the rise of people, in both men and women, under the age of 50. It’s happening for both colon and rectal cancer, and it’s actually happening in most states in the U.S., as well as many countries around the world.
They’re predominantly higher socioeconomic status countries, and the reasons for these trends are still unclear, but it is a global phenomenon.
What is driving the increase in young-onset CRC patients
The reason for why this is happening is one of the mysteries of medicine, honestly. We know that diet and lifestyle seem to have a strong link to colorectal cancer no matter what age you are, so we suspect that perhaps it’s diet and lifestyle, perhaps it’s environmental exposures other than diet and lifestyle, such as antibiotic use, that may be influencing whether young people are developing this at younger and younger ages.

I will have to say that we’ve done a couple of studies that linked obesity and sedentary behavior to a higher risk of developing colon cancer under the age of 50 in cohorts of women.
But the vast majority of patients we see in clinic are not obese and they are active, they eat healthy diets, they follow very active and healthy lifestyles. So clearly, it’s really not just those factors that are leading to this.
How many colorectal cancer patients are under 50
Approximately 150,000 patients are diagnosed newly each year with colorectal cancer. About 18,000 of them are under the age of 50. So it is a small proportion of all colorectal cancer patients right now who are diagnosed at a young age.
But if the trends that we are seeing now continue, it is estimated that by the year 2030, 25-percent of all rectal cancer patients are going to be under the age of 50.
So this is clearly going to be more and more of a problem in young people if the current trends continue and if we don’t start to understand better what the risk factors and causes are.
Patients get bombarded with diet and lifestyle recommendations. Where should they turn for reliable information?
Your experience is exactly the experience of so many of our patients. I think part of the problem is that there isn’t a lot of rigorous research out there to really determine what the ideal diet and lifestyle should be for a person with cancer or to prevent cancer.
This is an area I started working on right out of fellowship and started during fellowship, to study this in a more rigorous fashion. It is true that most of the diet and lifestyle studies out there are still epidemiological. They’re observational.
For the most part, they can only conclude there’s an association between a certain diet and lifestyle factor and risk of developing a cancer or likelihood of surviving that cancer.
It has been something we’ve been focusing on to try and turn those observational studies into randomized clinical trials that will be able to establish causality, a cause and effect relationship, which is the gold standard for determining if something truly has an effect on cancer.
The benefits of Vitamin D
One example is I’ve been working on vitamin D for a really long time. There’s been a lot of evidence in the laboratory that higher levels of vitamin D have been associated with less risk of developing colorectal cancer.

The vitamin D pathways implicated in all kinds of mechanisms that are very relevant for cancer development, so it made sense from the laboratory side that vitamin D may have a role.
We then started to look at this in epidemiological studies. Very consistently, we saw that higher levels of vitamin D in the blood seemed to be associated with a longer survival in patients with colorectal cancer, especially those with more advanced stages of colorectal cancer, stages three and four.
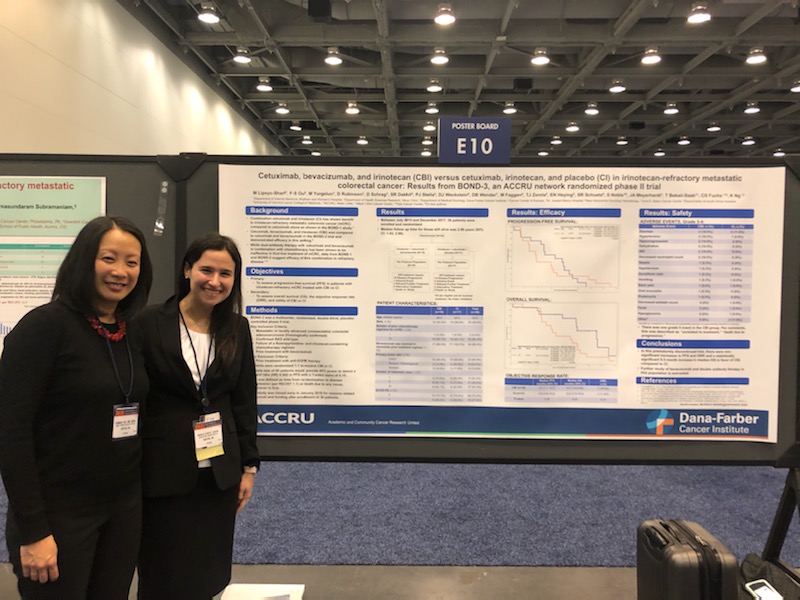
When we saw this and all the consistent evidence supporting such a relationship, we did decide to translate this into the first randomized clinical trial of vitamin D supplementation for treatment of patients with metastatic colorectal cancer.
This was called the Sunshine Trial and it was published in JAMA a couple of years ago. We found that adding high-dose vitamin D to standard chemotherapy seemed to allow patients to delay progression of their cancer for longer than a lower dose of vitamin D added to chemotherapy.
That was the first randomized clinical trial of vitamin D in colorectal cancer. The results were really encouraging and has now led to a National Cancer Institute-sponsored phase three clinical trial called Solaris, which is ongoing and enrolling, hopefully by the time it’s done, 400 patients with metastatic colorectal cancer to establish whether high dose vitamin D has a role in the treatment in patients with this disease.
It’s so important to understand the role of diet and lifestyle. These are easier interventions. They’re cost-effective. They’re things patients can do themselves that may perhaps impact how well they do. So it’s very important to study them very rigorously and to have evidence-based recommendations to give to our patients.
The Role of the Microbiome
What is the role of the microbiome in colorectal cancer
This led us to hypothesize that perhaps it’s the microbiome. The microbiome is the trillions of organisms that are living in all of our guts right now that have a profound impact on a variety of different chronic diseases and colorectal cancer is one of the ones that are probably most influenced but the microbiome because the cancer is developing right there in the gut where all the trillions of organisms are living.
We know that diet and lifestyle very closely shapes the composition of our microbiome and which organisms are in there.
It is therefore likely that diet and lifestyle factors, and environmental factors that may be affecting the microbiome in a way that may be leading to colorectal cancer, and also affecting how well our immune systems are able to either fight off or not fight off the development of a cancer such as this.
What are you hoping to gain in your newest study of the microbiome
I was very fortunate to get a three-year grant from the Colorectal Cancer Alliance to really study how exactly the microbiome may be influencing the risk of developing colon cancer in young people.
What we’re trying to do is understand how the microbiome is different in young patients depending on how young they are.
We know from clinical experience that it seems like the youngest patients under the age of 30, so in their twenties, even in their teens, may have a different type of colorectal cancer, one that might be a little more aggressive than the colorectal cancers we typically see.

Even compared to patients developing colorectal cancer in their thirties or in their forties are certainly different than those developing colorectal cancers over the age of 50.
We really want to delve deep into how the microbiome is different by what decade of age you’re diagnosed.
We also want to compare microbiomes of healthy, young people, who do not have a colorectal cancer diagnosis so we can get some hints on whether there’s some special microbiome signature that may predict who is at higher risk for developing colorectal cancer.
If it’s true that there is a specific signature or a high-risk microbiome that we can identify in healthy, young people, we’d be able to know who to target for earlier screening so that we can hopefully prevent the cancer from happening in these young people or catch the cancer at an earlier stage when it’s a lot more curable.
Because the microbiome has such an impact on our body’s immune system, as well, we’ll also be studying the effects of the microbiome at these different ages of diagnosis on different components of the immune system.
One very cool part of the grant is that we’ll be collecting stool samples from patients in their 20’s versus their 30’s versus over 50, as well as from healthy young people and actually transplanting and transferring these stool samples with their microbiome into mouse models of colon cancer.
We will see what impact each patient’s microbiome has on the development of colon cancers in these mouse models and study how exactly it is that it’s influencing the development of that cancer, and how it might be altering that mouse’s immune system to either lead to more aggressive growth or lead to less aggressive growth.
Our hope is that we better understand the mechanism of how the microbiome might be interacting with the immune system to lead to colorectal cancer.
Through that, hopefully we can discover a signature or model target that we can then develop a new drug against that would either decrease the chances of this happening in young people or better treat colorectal cancer that has already developed in a young person.
How will you conduct the study
There are two parts to the study. The first is just collecting a lot of stool samples from a lot of different patients at young ages, across the whole spectrum of young age, also from a large number of people with older onset colorectal cancer, above the age of 50, and then from a young cohort of people without colorectal cancer.
We want to analyze how the microbiome is different across these different ages and across cancer patients versus young, healthy patients.
The second part is to take a subset of these stool samples we’re collecting from these people and transplant them into mice to figure out what the mechanism and effect is on the immune system.
Has this study been done before
I don’t think so in terms of looking at young-onset colorectal cancer, specifically. It’s been done for other diseases to look at other variables and how the microbiome might be related to those variables.
As far as I know, this is the first study of its kind for young-onset colorectal cancer.
Who do you need as part of the study
We want to partner with as many patients as possible. Even though the rate of colorectal cancer happening in young people is rising, in terms of the overall colorectal cancer patient population, it is still a small number.
If we’re going to be able to get answers as to what these risk factors are and what the underlying causes are, we’re going to need thousands and thousands of young patients to participate in research studies such as this.
We all need to work together, partner with each other to get this work done quickly.
Growing Focus on Targeted Therapies
Targeted therapies have really revolutionized the treatment of patients with metastatic colorectal cancer in recent years.
We used to not understand which mutations may predict for benefit or lack of benefit from certain drugs, but with the advent of cutting edge technologies that are available now to really sequence tumors and understand the genetic profile of tumors, we understand more and more which mutations have a role in prediction what treatments may help to benefit a patient.

Microsatellite Instability (MSI)
The most striking example is the patients who have microsatellite instability (MSI) high-colorectal cancer. Among metastatic patients, it’s really a tiny proportion of patients.
Way less than five-percent of all metastatic colorectal cancer patients have this MSI high type of colorectal cancer, but if they do, it predicts a remarkable response to immunotherapy drugs.
These are patients who, if they respond, may have durable remissions lasting years, which is amazing for somebody with metastatic disease. So one of the biggest research priorities for us is to figure out for the other 95-percent of metastatic colorectal cancer patients, how can we get immunotherapy to work for them.
Here’s where the microbiome may actually have a role we’re just beginning to understand, as we were saying before, about how the microbiome interacts with the human’s immune system.
That could certainly be a factor in why 95-percent of colorectal cancers don’t respond to immunotherapy.
KRAS & NRAS
Other targets include KRAS and NRAS. KRAS is notoriously hard to target and develop drugs against. Approximately 50-percent of colorectal cancer patients do have mutation in either the KRAS or NRAS gene.
Where this knowledge has helped us in determining treatment recommendations for patients is if there is a KRAS or NRAS mutation in a patient’s tumor, then they are likely to not respond to drugs targeted the EGFR pathway.
VEGF
The other pathway that has been important for colorectal cancer is the VEGF pathway. These drugs that target the VEGF pathway we think work by targeting the mechanism by which tumors make blood vessels to feed themselves, so clearly trying to interfere with that may help to kill the cancer and perhaps help the patients not have progression of their cancer, and live longer.
Agents such as bevacizumab that are added to chemotherapy do seem to improve outcomes for patients with colorectal cancer.
HER2
We have a bunch of other targets, too, that have come on the scene. HER2, for example, has been a known target in breast cancer for a really long time. We’re now understanding that about five-percent of patients with colorectal cancer also have an overexpression of the HER2 gene.
In those patients, it seems like drugs that target the HER2 pathway, similar to the ones used in breast cancer, may also be effective in these patients with colorectal cancer and overexpression of the HER2 gene.
A lot of those trials are still ongoing, but they’re being increasingly incorporated into the armamentarium of drugs that we have to treat these molecular subsets of colorectal cancer.
BRAF
Finally, the other gene that’s very important to know the status of for a patient with colorectal cancer is the BRAF gene, which is present in about 10- to 15-percent of all colorectal cancer patients. We now have new drug combinations that target the BRAF pathway, whereas patients previous to these discoveries didn’t have many treatment options.
So there have been so many advances in the last few years in regards to these targeted therapies. It’s very important that all colorectal cancer patients with metastatic disease make sure to get their tumor profiled so that these decisions can be made and more precision medicine approaches can be recommended.
Guidance to Cancer Patients and Caregivers
What’s your guidance to patients going to community hospitals who may have less access to research
It’s a great question. While it is true that more and more centers, whether academic or community, are in fact doing this and sending patients’ tumor samples off to be profiled and sequenced, we do know that there are still many, many patients out there whose tumors have not been profiled.
I do recommend that patients be informed in terms of the status of their key genes. One is whether or not they have microsatellite instability, the KRAS and NRAS, the BRAF and the HER2, those are the ones right now that have treatment implications.
It can really affect the types of treatments that are recommended that have knowledge of whether or not these molecular alterations are present in your tumor.
If it is not offered that the patient’s tumor sample is going to be sent off for sequencing, patients should definitely ask their oncologist about it.
What are the basic questions patients should be asking their oncologists
It’s so important to be able to openly ask and talk to your oncologist about any question that may be on your mind. Even to ask, are there any questions I should be asking that I haven’t asked yet?
In general, the basic things to know are:
- What kind of cancer do I have?
- Where has it spread to if it has spread?
- What stage is it?
- What other tests do I need to be able to determine what stage it is or to help determine what type of treatment should be done?
- Are there any other types of doctors I should see?
- Is there a role for radiation, surgery, should I be meeting with those doctors?
- What are the treatment options?
- Often there are a few to choose from and so what are the data supporting each and which one would be recommended and why?
There are also clinical trials out there and a clinical trial is not for everyone, but it’s always good to know whether or not there is a clinical trial option out there that may improve your chances of having a good outcome or even if not, it just helps to advance the field of research and our understanding for future patients.
Other things are what are the side effects of treatment? So if you have decided on treatment what are the likely side effects? It’s important patients get good teaching about what to expect and if there are side effects, how to manage them.
It’s very important to know who to call in case there’s a problem. There has to be a good communication plan with the treatment team.
Then there’s still so much more than just treating the cancer, there’s everything else. Especially for our young-onset colorectal cancer patients, there may be questions about impact on fertility.
There are effects on sexual health. There are concerns about nutrition, diet, and lifestyle. Then psycho-social support is so important to help a patient and their family get through this.
It really takes a village to help comprehensively care for a patient with cancer and all of those resources should be used so you can get the best treatment possible.
What are your thoughts on the advancements of medicine and research, and what it means for cancer patients
The future is bright. There have been such discoveries in cancer research that were before unimaginable.
The example I always give is the example of immunotherapy and how well it does work for the under five-percent of metastatic colorectal cancer patients where it currently works right now.
Even in someone with metastatic disease, there is now a chance perhaps of long-term remission and cure, whereas that wasn’t always something thought to be achievable with someone with stage four cancer.
The hope in science is limitless and it has resulted in discoveries that have changed the way patients are treated and that has more than doubled the survival of patients with colorectal cancer.
There are advances being made everyday. The longer you are around, and thriving on treatment, the more new advances will be made. Definitely talk with your oncologist about whether there are research opportunities you can participate in, whether they be clinical trials or studies of the microbiome where you can contribute your stool, or diet and lifestyle questionnaires.
There is still so much to be learned that will benefit you and will also benefit all the other future patients out there.
Thank you, Dr. Ng!

Oncologist Expert Interviews
Dr. Christopher Weight, M.D.
Role: Center Director Urologic Oncology
Focus: Urological oncology, including kidney, prostate, bladder cancers
Provider: Cleveland Clinic
...
Doug Blayney, MD
Oncologist: Specializing in breast cancer | HER2, Estrogen+, Triple Negative, Lumpectomy vs. Mastectomy
Experience: 30+ years
Institution: Stanford Medical
...
Dr. Kenneth Biehl, M.D.
Role: Radiation oncologist
Focus: Specializing in radiation therapy treatment for all cancers | Brachytherapy, External Beam Radiation Treatment, IMRT
Provider: Salinas Valley Memorial Health
...
James Berenson, MD
Oncologist: Specializing in myeloma and other blood and bone disorders
Experience: 35+ years
Institution: Berenson Cancer Center
...




