Kidney Cancer Specialist Dr. Christopher Weight Shares Insights
Dr. Christopher Weight is a urological oncologist who focuses on treating cancers like kidney, prostate, and bladder. Now at the Cleveland Clinic, Dr. Weight is a kidney cancer specialist who leads the Urological Oncology Center, managing his time between research and seeing patients.

- Name: Dr. Christopher Weight, MD
- Role:
- Urological oncologist
- Professor of urology
- President of Climb 4 Kidney Cancer
- Director for urologic oncology at Cleveland Clinic, Glickman Urological & Kidney Institute
- Experience:
- 15-20 years
- Approach with Patients:
- To help patients navigate the often confusing and scary world of a new diagnosis of cancer
The first thing to do is take a deep breath. Know that in the last 50 years, we have made tremendous advances.
Most patients have time to still do the things they love and spend time with the people they care about. Many cancers these days have been converted to chronic illnesses.
Dr. Christopher Weight
Introduction
Can you introduce yourself?
My name is Dr. Christopher Weight. I am a urological oncologist at the Cleveland Clinic, I direct our urologic oncology center, and I am the president of a non-profit organization called “Climb 4 Kidney Cancer.”
I’m passionate about telling and hearing patient stories and how cancer affects people. Part of the reason for that is, during my residency, my father got prostate cancer himself.
It was very educational for me to see that on the personal side and be on the other side of the knife so to speak.
Eventually all of us will end up in that spot, where we need care. It was a very life-changing, informative experience for me to be in the midst of my training as a doctor and have it all hit so close to home.
As doctors, we need to think of our patients as a wife, husband, daughter, father, and so on. We need to think of our own families and try to imagine what it’s like for their families. If you can put yourself in their shoes, I think it makes you a better doctor and communicator.
I specialize in several different types of cancer including: prostate, testicular, bladder, adrenal, and kidney. It’s hard to say I have a preferred area, but I do enjoy doing the kidney surgeries. Although, I like the others as well.
Can you talk about Climb 4 Kidney Cancer?
I derive strength and perspective from my patients and their bravery throughout everything they go through. We took that ideology and put that into Climb 4 Kidney Cancer. As you’re climbing that mountain, you’re going against gravity every step of the way. Then, when you get higher in your journey, your perspective changes, and you have a view you’ve never had before.
I started this organization with a patient and a friend of mine. We started it largely to address the underfunding of kidney cancer. It’s one of the top ten, but it’s just below a lot of people’s thresholds and radars.
Unfortunately, cancer funding in the US is very dependent upon advocacy and lobbying. The top four and breast cancer have been a model of how successful advocacy can be. They’ve proved that the funding can really break down barriers and produce better outcomes.
We recognized that need on the financial side, but I recognized something similar to what The Patient Story has recognized. Patient stories have so much power.
On top of that, kidney cancer is very related to lifestyle. We know that the three main risk factors are smoking, obesity, and high blood pressure. Those are all very controllable by lifestyle modification.
So, simultaneously, we thought if we could get people more healthy overall, we could reduce the number of people who get kidney cancer in the first place.
Or perhaps if they do get it, they would be more prepared to beat it if they were healthier overall. That’s where the physical aspect of it came from, and then we coupled it with some of those more symbolic aspects of climbing a mountain.
We integrated that all into C4KC where we advocate for healthy lifestyles, we draw on the symbolism of climbing, and use that as a way to raise money and fund research.
Kidney Cancer Diagnosis
What causes kidney cancer?
I can say, “The three main risk factors are smoking, obesity, and high blood pressure,” but I still have patients who come in with kidney cancer who have never smoked and who have always been active and healthy.
They want to know, “Why did I get it?” We don’t have an answer for that yet. We just know those three things alter your risk.
Like all cancers, kidney cancer is a combination of a whole bunch of problems. Somewhere along the way, things get out of balance. It’s frustrating for patients because we don’t have all the answers yet.
What I tell patients is, “If you hadn’t lived a healthy lifestyle, maybe you would’ve been here five or ten years ago,” because we know there are also predisposing genetic factors that make us more susceptible to it.
What are the types of kidney cancer?
There are two main types of kidney cancer. The most common type is renal cell carcinoma, which forms from the cortex or outside of the kidney. That accounts for about 85-percent of kidney cancers.
Another 14-percent to 15-percent is urothelial cancer. This is from the lining, the interior of the kidney that collects the urine. Under the microscope, it looks very similar to the most common kind of bladder cancer.
Since the majority is renal cell carcinoma, that’s what is usually referred to when people say kidney cancer. The two types are treated completely differently, though, and respond to different medications.
Within renal cell carcinoma, there are three main subtypes. The most common is called clear cell renal carcinoma, the second most common is papillary, and the third is chromophobe. There are a whole bunch of rare cancers that can affect the kidneys, but those are the main types.
What determines what type of kidney cancer someone gets?
There are probably some genetic differences between the three. The real distinction comes from what they look like underneath the microscope.
We can’t tell by imaging alone. Although, one of the projects we’ve been funding with C4KC is using artificial intelligence to distinguish between those on CT imaging.
The types do behave differently and they do have different genetic changes, but we don’t know for sure if there are distinct risk differences between people.
For example, is one person more prone to one type or another because of some genetic factor, or if you’re obese, are you more prone to one or the other? Those are the details we’re still working on.
Kidney Cancer Treatment
Can you walk through your thought process of how to tackle a given kidney tumor or case?
Most kidney masses are identified incidentally now. What I mean by that is you go in for some other reason, get a scan, and you happen to find something abnormal in your kidney.
I recently had a patient who had a deer run out in front of her while she was driving. She got checked out, she looked fine, but they did a scan just to be sure. They found a big kidney mass, so she was very grateful to that deer for finding this cancer that was caught early enough to get treated without her having any symptoms.
Incidentally, there’s a lot of kidney abnormalities that look like cancer that aren’t–probably as many as 20- to 30-percent.
The first thing I focus on if someone comes to me with a kidney mass is telling them that. I try to determine the probability that it is cancer versus the probability that it’s a benign mass.
The easiest and biggest distinction to make right away after imaging is the size of the mass. The smaller it is, the more likely it is to be a benign process or a very slow-growing process of cancer. The bigger the mass, the more likely it is to be cancer and/or a life-threatening cancer.
The other thing we look at is actually the patient. The age of the patient is a factor. The younger you are, the less likely it is to be cancer. The average age that someone gets kidney cancer is 65 to 69. If they have smoked or have some of the risk factors, that increases the probability that it’s cancer.
Another important question right at the beginning is, “Is it confined to the kidney?” We scan the entire body, looking for masses or anything suspicious anywhere else. If they don’t have anything that’s spread, surgery is usually the best course of treatment for most kidney cancers.
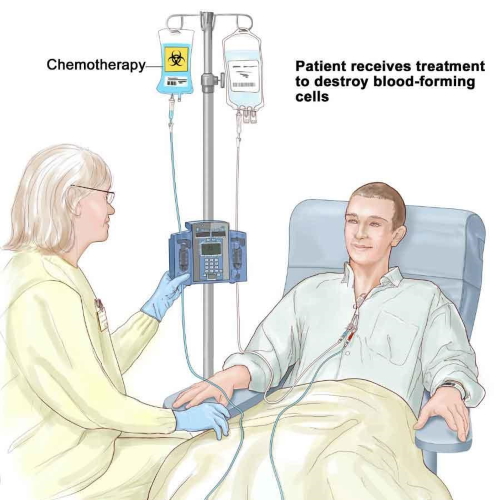
Is chemotherapy, radiation, or any other therapy ever necessary with kidney cancer?
Typically, we only use chemotherapy when the cancer has spread somewhere outside the kidney, and we don’t use it in the historical understanding of what chemo is.
You don’t lose your hair. Some are still infusions, but some are actually even pills you can take. It’s called targeted therapy or immunotherapy. It’s a combination of those medications only if it has spread outside the kidney.
Radiation therapy, we don’t typically use in kidney cancer because even though it would kill the cancer, it’s hard to deliver a high enough dose to the kidney without eating some of the surrounding organs. We use radiation more if it were to spread to the brain or some bone.
What is the role for clinical trials in kidney cancer?
It’s an exciting time. There have been a lot of advances in these targeted therapies, which were developed out of understanding the molecular basis of kidney cancer. They work based on those pathways. There have been a whole lot of drugs developed and approved for kidney cancer recently.
Even more recently, immunotherapy. There are big developments there as well.
Immunotherapy tries to harness the power of your own immune system to fight off cancer. They can often do that with limited side effects when compared to conventional chemotherapy.
I always encourage patients to get into a clinical trial if one is available to them. They help advance the science and knowledge, but they may very well benefit the patients themselves.
How do you go about referring patients to clinical trials? Any advice?
No one can have all the information about all the trials in their brain. It takes a team, and I think computers could also be helpful in this area. We have, and so do many universities, a multidisciplinary oncology group.
I am a surgeon. I treat cancer with surgery, but we have doctors who treat patients with immunotherapy and chemotherapy. We have doctors who treat patients with radiation.
We have a meeting every other week where we come together and inform each other on what trials we’re working on and what’s going on. We also discuss challenging patients who aren’t following any of the norms. In those meetings, we often update each other on new clinical trials we’re aware of.
For patients, I want them to know there is an ever expanding pool of information and clinical trials. It’s important to know that and ask about that.
If your local team doesn’t have one available, keep asking. Usually, academic medical centers are great for that, but sometimes local centers are too.
The governments has a website that is supposed to have a registry of all the clinical trials. It’s called clinicaltrials.gov. I always encourage patients to check that. Although you would like to rely on your doctors, it’s nice to have someone else who can do some of that research for you. You, as a patient, don’t need to be doing it, but maybe a family member could go and look for you.
It’s important to feel empowered. There’s a lot of information out there, and it’s impossible for you doctor to be aware of all of it. Don’t feel obligated to stick with a doctor if they don’t have access to a trial or even just information you want.
It’s okay to get a second opinion. It’s okay to switch providers. You’re not going to hurt anybody’s feelings.
I’ve had patients come to me with information that I hadn’t known and was able to incorporate into my practice.
Support
How can family members of cancer patients help?
Be present. Show up to appointments. Cheer on your family members. I recognize the limits of medical care to meet all the needs of a patient with cancer. We can prescribe treatments and give information, but there’s also a tremendous amount of help that comes from the support network.
There’s quite a bit of data that suggests this to be true. The survival rate among married couples where one patient has cancer is higher compared to single individuals with cancer.
What that means for me as a doctor is I need to make sure the patient does what they can do and enlist the support of their family.
»MORE: What kind of support cancer patients say helped the most
Do you have any advice for a newly diagnosed patient?
The first thing to do is take a deep breath.
Know that in the last 50 years, we have made tremendous advances. Most patients have time to still do the things they love and spend time with the people they care about.
Many cancers these days have been converted to chronic illnesses. You may need to treat it, you need to pay attention to it, and you may have to go through surgeries, but you still are going to be able to lead a reasonable life.
For those of us who work with people who have cancer, there is a constant reminder of the temporal nature of life. Health is a gift. Every day that you have it is a benefit.
Of course, you don’t want someone to have to get cancer to come to this clarity, but the perspectives gained are not necessarily a drawback.
You are going to gain insight from this experience, and that can sometimes be a lever to you being able to live the most meaningful life and focusing on the relationships that really are most important.
It’s hard to say going into it because all you can see at the beginning is this horrible thing, but it’s something that many patients express at one point or another.
Things like The Patient Story and C4KC are so valuable. Reach out. It’s so reassuring to a newly diagnosed patient to see someone who has been where they are who is now doing the things they love to do again. It’s a breath of fresh air.

Oncologist Interviews
Dr. Christopher Weight, M.D.
Role: Center Director Urologic Oncology
Focus: Urological oncology, including kidney, prostate, bladder cancers
Provider: Cleveland Clinic
...
Doug Blayney, MD
Oncologist: Specializing in breast cancer | HER2, Estrogen+, Triple Negative, Lumpectomy vs. Mastectomy
Experience: 30+ years
Institution: Stanford Medical
...
Dr. Kenneth Biehl, M.D.
Role: Radiation oncologist
Focus: Specializing in radiation therapy treatment for all cancers | Brachytherapy, External Beam Radiation Treatment, IMRT
Provider: Salinas Valley Memorial Health
...
James Berenson, MD
Oncologist: Specializing in myeloma and other blood and bone disorders
Experience: 35+ years
Institution: Berenson Cancer Center
...
Jacqueline Barrientos, MD
Role: Hematologist, researcher
Focus: Chronic lymphocytic leukemia (CLL), lymphoma, 17p Deletion (Ibrutinib, Acalabrutinib, Venetoclax), IgHV mutation
Provider: Northwell Health (NYC)
...
Dr. D. Ross Camidge, M.D., Ph.D.
Role: Thoracic oncologist, Director of the Thoracic Oncology Clinical Research Programs
Focus: Lung cancer, small cell (Immunotherapy), EGFR (Osimertinib), ALK (Alectinib), ROS1 (Crizotinib), BRAF (Dabrafenib & Trametinib), NTRK
Provider: Univ. of Colorado
...
Edmund Tai, M.D.
Role: General oncologist, hematologist
Focus: Specialist in treating Chinese-speaking patients
Provider: Sutter Health (Bay Area, CA)
...
Irene Ghobrial, MD
Role: Clinical investigator and professor of hematological oncology
Focus: Multiple myeloma, Waldenström’s Macroglobulinemia, early screening, clinical trials
Provider:Dana-Farber Cancer Institute (Boston)
...
Tim Fenske, MD, MS
Role: Hematologist-Oncologist
Focus: chronic lymphocytic leukemia (CLL) & leukemia and lymphoma | CAR T, targeted therapy
Provider: Medical College of Wisconsin
...
David Miklos, MD
Date: Jan. 2021
Focus: Who benefits from CAR T, ZUMA-2 clinical trial, Stanford's CAR 22 Work
Provider: Stanford Medical
...
Kimmie Ng, MD, MPH
Role: Gastrointestinal oncologist
Focus: Young-onset colorectal cancer, microbiome
Provider: Dana-Farber Cancer Institute (Boston)
...
Farrukh Awan, MD
Role:Hematologist-oncologist, associate professor
Focus:Leukemias, Lymphomas, BMT
Institution:UT Southwestern
...
Kerry Rogers, MD
Role: Hematologist, researcher
Focus: Chronic lymphocytic leukemia (CLL), Hairy Cell Leukemia (HCL)
Institution: OSUCCC-The James
...
Nina Shah, MD
Role: Hematologist-oncologist, researcher
Focus: Multiple Myeloma
Institution: University of California, San Francisco (UCSF)
...
Rafael Fonseca, MD
Role: Interim executive director, hematologist-oncologist
Focus: Multiple myeloma, new drug development
Institution: Mayo Clinic
...
William Wierda, MD, PhD
Role: Hematologist, Med. Dir., Dept of Leukemia
Focus: Chronic lymphocytic leukemia (CLL), other leukemias
Provider: MD Anderson
...
Latest on CLL Treatment (2022)
Featuring: Nicole Lamanna, MD; William Wierda, MD, Ph.D
Hosted by: Michele Nadeem-Baker
Topics: Pirtobrutinib, new oral combinations, venetoclax updates, CAR T
...
David Miklos, MD, Ph.D
Role: Hematologist, researcher
Focus: How MCL treatments have improved, importance of clinical trials
Provider: Stanford Medical Center
...
David Miklos, MD, Ph.D
Role: Hematologist, researcher
Focus: Role of allogeneic BMT, response to graft versus host disease (GVHD)
Provider: Stanford Medical Center
...
CAR T Cell Therapy in Myeloma
Dr. Fonseca shares his insights on emerging T-cell therapies for multiple myeloma, describing the role T-cells play in our bodies and then focusing on chimeric antigen receptor (CAR) T-cell therapy and bispecific T-cell engagers.
...
Joseph Mikhael, MD
Role: Dir. Myeloma Research, CMO at International Myeloma Foundation (IMF)
Focus: Multiple myeloma
Provider: TGen/City of Hope
...
Ruben Mesa, MD
Role: Executive Director, Mays Cancer Center; Prof. of Medicine
Focus: Myeloproliferative neoplasms (MPN)
Institution: UT Health San Antonio MD Anderson
...
Srdan Verstovsek, MD, PhD
Role: Director, Clinical Research Center for MPNs at MD Anderson; Section Chief, MPNs; Prof., Dept. of Leukemia
Focus: Myeloproliferative neoplasms (MPN)
Institution: MD Anderson
...
Saad Z. Usmani, MD
Dr. Saad Usmani, Chief of Myeloma Service at Memorial Sloan Kettering, talks about CAR T-cell therapy, bispecific antibodies, novel therapies and combination therapies.
...
Vincent Rajkumar, MD
Dr. Vincent Rajkumar, a hematologist oncologist at the Mayo Clinic, talks about drug pricing and the impact of high prescription drug costs on patients and families.
...
The Doctor Talk w/ Dr. Gasparetto & Dr. Richter
Role: Dr. Cristina Gasparetto (Duke) and Dr. Joshua Richter Mount Sinai discuss latest relapsed refractory multiple myeloma treatments
...
Dr. Samuel Washington, MD, MAS
Role: Assistant Professor of Urology, UCSF
Focus: Treatment disparities in bladder cancer treatment
Provider: University of California San Francisco
...
Multiple Myeloma in 2023
Long-time myeloma patient and advocate, Jack Aiello, leads the conversation with Dr. Joshua Richter, Multiple Myeloma Director for Blavatnik Family Chelsea Medical Center at Mount Sinai and Dr. Muhamed Baljević, Plasma Cell Disorders Research Director for Vanderbilt-Ingram Cancer Center.
...
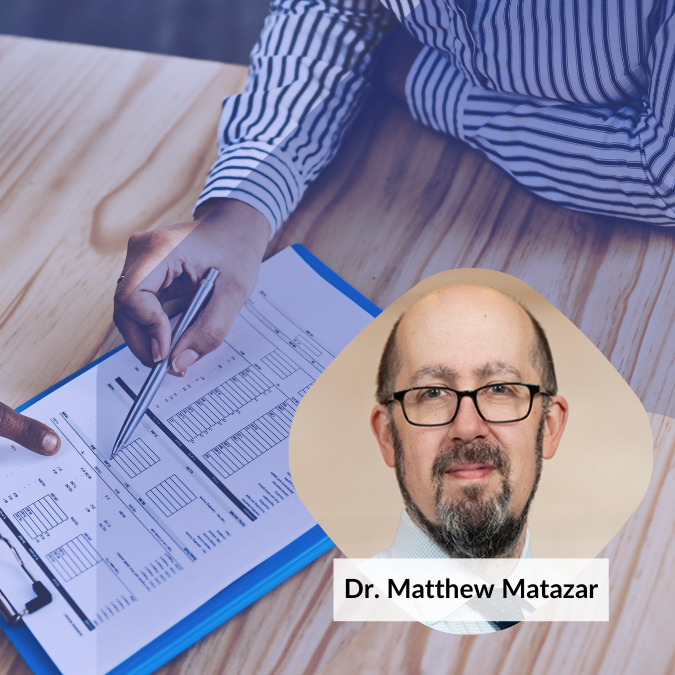
Matthew Matasar, MD, MS
Dr. Matthew Matasar, chief of blood disorders at the Rutgers Cancer Institute of New Jersey and RWJBarnabas Health, sat down with Dr. Samantha Spiegel, a Hodgkin’s lymphoma patient, to discuss some of the most exciting news coming out of ASH 2022.
...
DLBCL in 2023
The Patient Story founder and DLBCL advocate Stephanie Chuang leads the conversation with Dr. Josh Brody, who leads the Lymphoma Immunotherapy Program at Mount Sinai’s Tisch Cancer Institute, and Dr. Lorenzo Falchi, an oncologist at Memorial Sloan Kettering Cancer Center.
...
SABCS 2022 Highlights
Top breast cancer doctors Dr. Paolo Tarantino with Dana-Farber Cancer Institute and Dr. Lola Fayanju with Penn Medicine discuss the big highlights from this year’s San Antonio Breast Cancer Symposium.
...
Relapsed/Refractory Multiple Myeloma Highlights from ASH 2022
Multiple myeloma specialists Dr. Ajai Chari with Mount Sinai in New York and Dr. Sandy Wong with the University of California San Francisco discuss the big buzz at this year’s ASH: bispecific antibodies.
...
Myelofibrosis Highlights from ASH 2022
Dr. Serge Verstovsek and Dr. Naveen Pemmaraju discuss cutting-edge treatments and therapies, and combination therapy as a focus in treating myelofibrosis.
...
Newly Diagnosed Multiple Myeloma Highlights from ASH 2022
Dr. Caitlin Costello and Dr. Sagar Lonial discuss treatments for newly diagnosed multiple myeloma patients.
...
High-Risk Smoldering Multiple Myeloma Highlights from ASH 2022
Patient advocate Jack Aiello and hematologist Dr. Shaji Kumar discuss what high-risk smoldering patients can do to delay or possibly avoid progression to active myeloma.
...
DLBCL: The Latest in Treatment and Research
Discover the latest DLBCL treatments from two top lymphoma doctors and a diffuse large b-cell lymphoma survivor who is also a doctor.
...
Chadi Nabhan, MD, MBA
Dr. Chadi Nabhan shares how he got involved in the Monsanto trials, what he learned from the, and why he decided to write a book about the whole experience.
...
CLL Highlights from ASH 2022
Patient advocate Andrew Schorr and hematologist Dr. Nitin Jain discuss the latest treatment and developments in CLL coming out of ASH 2022.
...
Research on Black Myeloma Patients, Access & Disparities
Patient advocate Valarie Traynham and Dr. Shakira Grant discuss the barriers many Black patients face, how it impacts their care, and what can be done to help improve their outcomes.
...
Testicular Cancer: What Patients Need to Know
Medical oncologist Alok Tewari, MD, PhD, who specializes in cancers arising from the genitourinary tract, discusses what patients need to know about testicular cancer.
...
Lynch Syndrome: What Patients Need to Know
Medical oncologist Michael Hall, MD, MS, discusses Lynch syndrome, what cancers patients would be more at risk for, and who should get tested.
...
The Role of Bispecific Antibodies in the Treatment of Multiple Myeloma
Hematologist Alfred Garfall, MD, MS, from Penn Medicine discusses with multiple myeloma patient advocate Jack Aiello the advancement of immunotherapy for multiple myeloma, the difference between CAR T-cell therapy & bispecific antibodies, and the role of bispecifics in the myeloma toolkit of immunotherapies.
...
How to Build a Strong CLL Team
Nicole Lamanna, MD, from Columbia University Medical Center, Spencer Bachow, MD, from Boca Raton Regional Hospital, and CLL patient Lisa P. discuss the importance of building a strong support system and collaborating effectively with multiple doctors.
...
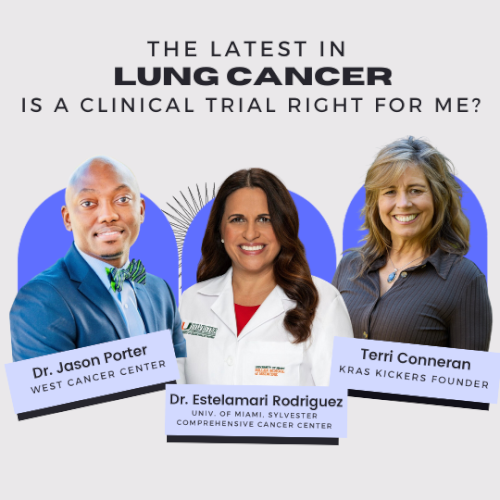
The Latest in Lung Cancer Treatments: Is a Clinical Trial Right for Me?
Leading experts Estelamari Rodriguez, MD, MPH, from the University of Miami Sylvester Comprehensive Cancer Center, Jason Porter, MD, from West Cancer Center & Research Institute, and Terri Conneran, founder of KRAS Kickers, discuss the latest in lung cancer treatments and ongoing clinical trials.
...
The Latest in Multiple Myeloma Treatments: What Clinical Trials are Available to Me?
Patient advocate Cindy Chmielewski, experts Dr. Carl Ola Landgren and Dr. Caitlin Costello, together with clinical trial nurse Christen Hawthorne uncover groundbreaking insights on the latest multiple myeloma treatments and clinical trials.
...
Clinical Trials and You: How to Navigate Treatment?
Patient advocate Ruth Fein Revell, experts Dr. Angela Fleischman and Dr. Ruben Mesa, together with clinical trial nurse Melissa Melendez delve into the cutting-edge realm of myelofibrosis clinical trials.
...
Let’s Talk CLL: Patients & Doctors Discuss the Latest LIVE
Patients, care partners, and a panel of CLL experts including Dr. William Wierda, Dr. Nicole Lamanna, Dr. Adam Kittai, and Jackie Broadway-Duren share the latest in CLL research, clinical trials, treatments, and comprehensive care strategies.
...
The Latest in Multiple Myeloma: Understanding Promising Treatment Options
Patient advocates Cindy Chmielewski and Jack Aiello, and experts Dr. Rafael Fonseca and Dr. Susan Bal discuss promising multiple myeloma treatment options.
...
The Latest in Hodgkin Lymphoma: Treatment Options in 2024
Dr. Matthew Matasar, chief of blood disorders at the Rutgers Cancer Institute of New Jersey and RWJBarnabas Health, discusses some of the most exciting news coming out of ASH 2023.
...
Optimizing Quality of Life: Reducing Toxicity in Hodgkin Lymphoma Care
Dr. Andy Evens from Rutgers Cancer Institute discusses how to reduce the toxicity of Hodgkin’s lymphoma treatments so patients can live their best lives after cancer.
...