DLBCL in 2023
What Patients & Caregivers Need to Know Now
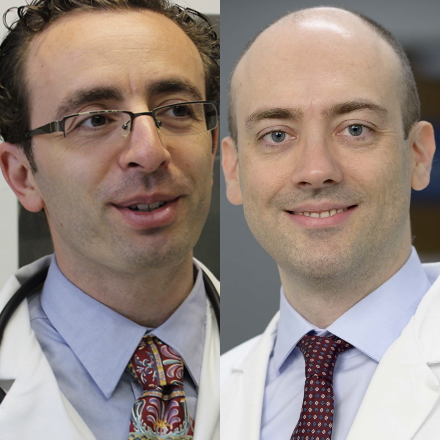
The Patient Story founder and DLBCL advocate Stephanie Chuang leads this conversation with Dr. Josh Brody, who leads the Lymphoma Immunotherapy Program at Mount Sinai’s Tisch Cancer Institute, and Dr. Lorenzo Falchi, an oncologist at Memorial Sloan Kettering Cancer Center with special research focus on immunotherapies for B-cell non-Hodgkin lymphoma.

Thank you to Genmab for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Immunotherapy for DLBCL
- CAR T-cell therapy in earlier lines of treatment for DLBCL
- Bispecific antibodies in the treatment of DLBCL
- Bispecifics in clinical trials
- Cytokine release syndrome (CRS)
- Deciding whether to give bispecific antibodies or CAR T-cell therapy
- Bispecifics given as single agents and in earlier lines of treatment
- Epcoritamab for transplant-eligible patients who didn’t do well post-transplant
- Importance of patient-reported outcomes
- Breakthrough therapies for DLBCL offer hope
- DLBCL Patient Stories
Introduction
Stephanie Chuang, The Patient Story: I was diagnosed with cancer when I was 31 years old and, like many people, I was completely overwhelmed [and] freaked out. I thought, Am I going to die? I think that’s a pretty common thing to think when you’ve been diagnosed with cancer. I was really thankful to learn that there was a standard of care treatment in chemotherapy that seemed to have a pretty good impact on cancer and DLBCL.
I underwent dose-adjusted R-EPOCH — a little bit different from the usual R-CHOP. I remember my doctor telling me, “Look, Stephanie, if you can hit two years after treatment is done and the cancer is gone, you’re still in remission. That’s a really good sign.”
It’s great news that I was able to get through treatment and get into remission. But that wait was really hard. Lots of anxiety and scanxiety as it’s known. I was able to hit two years and, in fact, most recently I celebrated my five years. But so many people cannot say that.
That’s where the problem is. There’s a really great need for more options in treatment. If that first treatment fails, when cancer comes back or if it never responded, [relapsed/refractory cancer] and that’s what we’re talking about.
What are the treatments out there? What are the options? What should you know to ask your doctor in terms of the research that’s going on out there?

There’s good news. There [are] a lot of different things happening in clinical trials, whether it’s new drugs or new combinations, new tactics, and a lot of immunotherapy using your own immune system to fight cancer.
I’m really excited to bring together two top DLBCL specialists and, hopefully, shed some light for you, especially during what is a very difficult time.
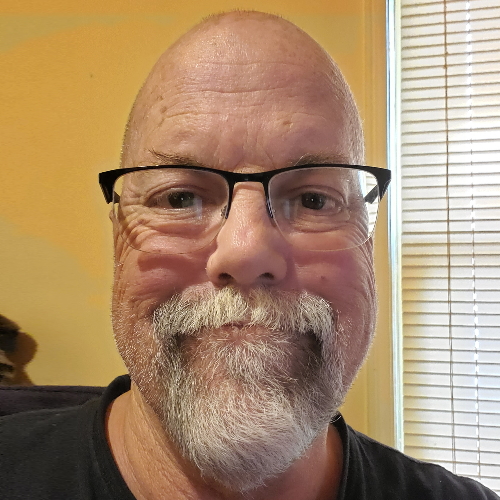
Dr. Josh Brody leads the Lymphoma Immunotherapy Program at Mount Sinai’s Tisch Cancer Institute.
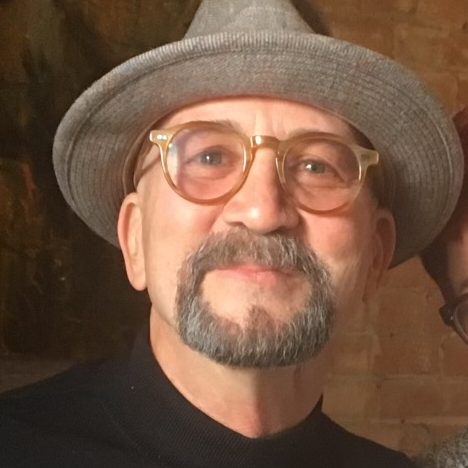
Dr. Lorenzo Falchi is an oncologist at Memorial Sloan Kettering Cancer Center with special research focus on immunotherapies for B-cell non-Hodgkin lymphoma.
There’s a lot of new information and updates coming out of the biggest meeting of top blood cancer doctors and researchers called ASH or [the] American Society of Hematology, which just took place.
Dr. Brody, a lot of people wonder — I certainly did when I was diagnosed — why me? What did I do to get this? This is something you hear a lot from your patients as well.
There’s nothing you did. You got this for the same reason that people get hit by lightning. Nothing that they did.
Dr. Brody

Dr. Josh Brody: In the very beginning, when patients get diagnosed, a lot of questions [are] coming out of a place of fear, [which is] very natural and understandable. How did I get this? What did I do? As though someone wants to blame themselves for this. I guess it’s natural.
Our first thing is to go and say, “There’s nothing you did. You got this for the same reason that people get hit by lightning. Nothing that they did. You got this, primarily for most patients, because of one cause and one cause only: bad luck. That’s why you got this.”
Then we say, “In context, it could have been worse luck because there are worse things you could even have.”
Of course, the questions are, “What can I eat to make this get better? What vitamins can I take?” The answer is you should eat [healthily] and be healthy. Being healthy is not just about eating; it’s about physical activity and exercise.
We have a ton of data that physical activity and living healthy improves outcomes for cancers, for lymphomas. But we don’t micromanage and have a specific, “Oh, you need these blueberries, this green tea, this antioxidant.” Healthy eating [and] healthy living is critical, but the details [are] probably not critical.
Being healthy is not just about eating; it’s about physical activity and exercise. We have a ton of data that physical activity and living healthy improves outcomes for cancers, for lymphomas.
Dr. Brody
Immunotherapy for DLBCL
Stephanie, TPS: What can be critical is how much we know, as patients and caregivers or care partners, to make sure that we’re getting the best care.
The standard of care has been R-CHOP as a first-line [treatment] for people in aggressive chemotherapy. But if that doesn’t work for the patient, then there’s that gap. What can we go to?
There’s been this big focus on immunotherapy and we’ve heard about CAR T-cell therapy and that’s been approved in DLBCL. What was really exciting at [ASH 2022] is bispecific antibodies and that’s really had a lot of progress in research, too.
Dr. Brody: We were already lucky in lymphoma to have more progress than before. [In the] last couple of years, I would say the rate of progress has only increased.
If there’s a unifying theme of things that are being invented in labs by companies [and] in academia, it’s immunotherapy [or] using our patients’ immune systems to kill their own cancer.
People thought this was a bunch of hocus pocus 15 [or] 10 years ago. We’re going to use your immune system to fight this problem. But now, it is a real, measurable, making-people-live-instead-of-die thing.
The progress in DLBCL immunotherapy has been unprecedented, especially [in] the last couple of years. The most obvious examples are CAR T-cells. When I describe this science-fiction-like immunotherapy to my patients, they say, “But that’s not a real thing.” I say, “No, it’s real,” and then we describe it. It’s quite remarkable.
[There is] even this somewhat-simpler type of immunotherapy that I think will actually have [a] greater impact overall than CAR T-cells, which is this class of medicines called bispecific antibodies. [It’s] another immunotherapy that gets your immune cells to kill cancer cells.
The progress in DLBCL immunotherapy has been unprecedented.
Dr. Brody
CAR T-cell therapy in earlier lines of treatment for DLBCL
Stephanie, TPS: To be clear, the idea of using your own immune cells to kill cancer is an idea that’s been around but in the last few years is when we’re really seeing the impact of this.
Before we dive into this big buzz of bipecifics, let’s talk about CAR T. As some people may or may not know, there have been three CAR Ts that have been approved in DLBCL, but they’ve been approved for third-line of treatment. Again, the first treatment didn’t work, [the] second treatment didn’t work, [and] now we’re going to the third one.
Dr. Brody, as you mentioned, CAR T has been able to put many patients into deep, complete remission, which is what we’re looking for. But the last year has shown that CAR T can be promising even earlier on. Is that right?
Dr. Brody: Some big trials [are] showing remarkable benefit [with] CAR T-cells as second-line therapy — not as the first therapy, but as second-line therapy. They had to show that they were better than the standard in that place.
That standard for second-line was aggressive chemo and autologous stem cell transplant, which is just very aggressive chemo. It was focused on the highest-risk people, [those] with DLBCL who relapsed within the first 12 months. That meant a lot of people relapsed in month 3 [and] month 6. Some of them didn’t even relapse at all; they got no response at all from the front-line R-CHOP chemotherapy.
On these highest-risk patients, the benefit of CAR T-cells compared to the old standard was remarkable. Many more of them [are] staying in remission for months now. Now, at [ASH 2022], we have a year-and-a-half follow-up. One of those trials [shows] many more patients staying in remission.
[With] the old numbers with CAR T-cells, we thought maybe we were curing 35-40% of patients just with CAR T-cells. We’ll see if those numbers reproduce or might even be better now [by] using them in the second-line setting. That is for the highest-risk group of DLBCL patients that we’re talking about.
Bispecific antibodies are a real breakthrough class of medications for lymphoma and many hematologic malignancies… I like to refer to bispecific as the third big milestone in immunotherapy for lymphoma.
Dr. Falchi
Bispecific antibodies in the treatment of DLBCL
Stephanie, TPS: That’s really great. Let’s go into bispecific antibodies or bispecifics. Dr. Falchi, what is going on with them? Why are people so excited by them and how do they work?
Dr. Lorenzo Falchi: Bispecific antibodies are a real breakthrough class of medications for lymphoma and many hematologic malignancies, that is blood cancers. What makes them a breakthrough is they’re novel technology that really translated into very impressive clinical results and a real benefit for patients.
I like to refer to bispecifics as the third big milestone in immunotherapy for lymphoma. The first [is] monospecific antibodies, like rituximab that most people are familiar with in the field. The second [is] CAR T-cell therapy. I think the third would be bispecific antibodies.

Dr. Brody: Bispecific [antibodies are] actually very similar to CAR T. CAR T sounds so fancy. It’s hard to believe. We take some immune cells out of your blood. It takes a few hours, not too big of a deal. We put a new gene in them. The gene is called a CAR gene.
You put that CAR into the T-cells. Now they call them CAR T-cells. We take the blood out, mail this someplace — it used to be Santa Monica, now there [are] a few places — and then they mail it back to you. Then you reinfuse those CAR T-cells into the patient.
Bispecific antibodies [use a] very similar idea, just maybe a little simpler even. We don’t actually have to take T-cells out to make them recognize lymphoma. We put in a bispecific antibody.
Many folks have heard of rituximab. The regular antibody binds to one protein on one cell. [A] bispecific antibody binds to two cells. It binds to your lymphoma cell, binds to your T-cell, [and] brings them together. One of my colleagues said, “This is like the ‘Lady and the Tramp’ with the spaghetti in between them.”
At the very end of the spaghetti, in this case, it’s the kiss of death, because the T-cell kills the cancer cell. That “Lady and the Tramp” image is a pretty good one. I have to credit Dr. Matthew Lunning for the “Lady and the Tramp” metaphor. [With] that kiss of death, these T-cells are highly activated and able to kill. That immune cell kills that cancer cell quite effectively.

In folks where standard therapies didn’t work, where CAR T-cells weren’t working, it seems like more than a third of patients with these bispecific antibodies are getting complete remissions. Again, that’s the highest-risk group of patients. In the worst-case scenario, it seems like more than a third of them are getting complete remissions.
Even when the best things weren’t working, bispecifics, [and] epcoritamab in that case, [was] still highly effective.
Dr. Brody
Bispecifics in clinical trials
Stephanie, TPS: Let’s break down what we should be looking for in terms of bispecifics. As we know, these drugs are being developed in clinical trials. There are different phases where they’re bringing them to patients and seeing how patients do on them, studying dosages, and not just how effective they are in terms of how much more people can live without the disease but how well. What are the side effects? Which ones currently in clinical trials are expected to get approvals sooner?
Dr. Falchi: I think it emerged quite clearly that the two main actors in the world of bispecifics for patients with diffuse large B-cell lymphoma are epcoritamab and glofitamab. These drugs are both highly potent. Very, very powerful. In fact, before using them in patients, it was shown in experiments that their potency is exactly the same.
Dr. Brody: Because they have so many patients now, they really got to parse out the patients with high risk, super high risk, and all the different risk factors.
As we said, CAR T is very promising but a year or two ago, if CAR T failed, the options were not great. About a third of the patients in both the epcoritamab and glofitamab trials already had CAR T. CAR T didn’t work because it’s not a guarantee. It’s great, but it’s not a guarantee.
Epcoritamab or glofitamab — at [ASH 2022], we’re talking more about epcoritamab in that parsing of the data — [were] still giving complete remissions in more than a third of patients. Even when the best things weren’t working, bispecifics, [and] epcoritamab in that case, [was] still highly effective.
Glofitamab so far has some advantage in that all the recipes for them have been written as time-limited. You get 12 cycles and you’re done. Nine months of therapy and then you get a break.
Epcoritamab studies have been written so far to be continuous therapy, as long as it’s helping you and not hurting you. Whether we need to keep giving it for a long time, we don’t really know. At least, it’s a difference so far.
The other big obvious difference is that [with] epcoritamab, the way we [give it] is different. It is a subcutaneous injection, so it’s a quick little shot and you’re done. You’d almost think you could just get it at home, but we haven’t worked on that yet. Glofitamab is an IV infusion still.
Rates and severity of CRS for bispecific antibodies appear to be, at least at this stage, quite substantially different compared to what we see with CAR T-cell.
Dr. Falchi
Cytokine release syndrome (CRS)
Stephanie, TPS: We don’t have any FDA-approved bispecifics in the DLBCL space yet. The hope is that maybe there will be approvals sometime in 2023. This is information based on these research studies.
A very important topic is side effects and quality of life. We can extend life by X number of months or someone’s in remission for this amount of time. But we also truly want to understand: are we going to be able to live well while on this treatment or even once we get off of the treatment? Can you set the stage for what kind of side effects we’ve seen so far in the studies with bispecifics?
Dr. Brody: We talked about all the promises. We do not want to oversell this. There are also side effects of these medicines. The most significant or maybe concerning side effect of all of these bispecifics, really all these immunotherapies, is the risk that we push your immune system too hard and you get a reaction as though you had an infection, but there is no infection. It’s just that we pushed your immune system to react.
One version of that is a side effect [is what] we call CRS: cytokine release syndrome. CRS can be significant. [It can] make you get a high fever [and] make you get low blood pressure. If you get a [really] bad version of this, you have to be in the hospital for observation and sometimes for treatment of that.
With CAR T-cells, those high-grade CRS events were pretty common. They’ve gotten better as we’ve gotten more experience using them. With bispecifics, the numbers are better but that risk is still there.
For both bispecifics, epcoritamab [and] glofitamab, the standard today is that people have to get hospitalized for at least one day just to observe them after they get the first higher dose of that infusion.
Dr. Falchi: Both administrations are given usually without side effects. The main side effect that ensues a little bit later is something called CRS or cytokine release syndrome. For those who have experienced CAR T-cell, this is a very well-known adverse event.
It’s an inflammatory reaction where people can have fever [and] chills, their blood pressure could decrease a little bit, [and] there can be some confusion. It can be scary because it comes up quite suddenly and it may become quite apparent quite early. Very rarely, it requires hospitalization and may need care.
For the most part, we were very pleased to see, in both the epcoritamab study and the glofitamab study, that the percentage of patients who have a severe cytokine release syndrome is much less than 5%. The majority of patients will have some fever [and] chills, and generally, these will resolve within a day or two.
These rates and severity of CRS for bispecific antibodies appear to be, at least at this stage, quite substantially different compared to what we see with CAR T-cell, particularly Axi-cel, which is one of the most utilized products for diffuse large B-cell lymphoma.
In the CAR T-cell studies, we’re looking at [a] double-digit percent of higher grade CRS. For that reason, most patients, particularly those who are a little bit more advanced age, need to be hospitalized for several days after receiving CAR T-cell.
For bispecific antibodies, we’re looking at a 24- to 48-hour hospitalization. We’re confident that in the future, as we gain more experience, there is a possibility that these drugs — [which are] off-the-shelf products so [they are] immediately accessible — can be given on a fully outpatient basis without having [to be] admitted to the hospital.
Although none of these [bispecifics] are currently approved by the FDA, it is hoped that one or more of them will be approved in the near future because of such promising results.
Dr. Falchi
Deciding whether to give bispecific antibodies or CAR T-cell therapy
Stephanie, TPS: To be clear, we’re not saying that with bispecifics being so promising if they are approved, they’ll erase the need for CAR T-cell therapy. But what we’re talking about is there are details that are coming out in this research that will help doctors, patients, and care partners determine the best treatment path for each individual.
Some of those factors include what is available [and] what is quicker to get because sometimes, time is going to be a big factor. What are the side effects? How long would someone need to be monitored in the hospital or the clinic for side effects that are more severe, like CRS, the way you’ve both described?
Is there anything else that you would consider in making the treatment decision about whether someone should go on a bispecific or CAR T?
Dr. Falchi: On a logistical basis, CAR T-cell therapy is quite an involved therapy. It needs to be administered by specialized centers.
In the US, there [are] many such centers, but they’re not everywhere so it’s important to know where these centers are [and] who can administer those therapies. Doctors have to be certified. Centers have to be certified. It is not a therapy that everyone can give.
They require hospitalization for the majority of patients. Some patients can receive CAR T-cell therapy on an outpatient basis but for now, I would say, that’s a minority of patients. The majority will require hospitalization and monitoring. Even after discharge, oftentimes patients will be required for a period of time to stay in the area where [the] CAR T-cell therapy was administered.
In the post-CAR T-cell therapy period, there’s periodic monitoring where the doctors will want to look at blood counts, other blood work, or scans multiple times in the months ensuing CAR-T cell therapy.
As far as bispecific antibodies are concerned, these are drugs that are administered either subcutaneously or intravenously for the most part, on an outpatient basis. And this is important because although none of these drugs are currently approved by the FDA, it is hoped that one or more of them will be approved in the near future because of such promising results.
Therefore, it’s important for us as academic clinicians and for our colleagues to become very familiar with this product. I think, really, the point to make about these drugs is that they can be safely administered as outpatient therapy. Their main side effect, which is cytokine release syndrome or CRS, is something that is to be expected in a certain percentage of patients and we all will need to become familiar with it and how to manage it promptly.
Management of CRS from bispecific antibodies has not been as “complicated” as it has been for CAR T-cell therapy in the sense that drugs like acetaminophen, drugs like steroids including prednisone or dexamethasone, which are drugs that we very commonly use and most patients are familiar with, are the mainstay of therapy for most cases of CRS related to bispecific antibodies.
Only rarely will patients treated with bispecific antibodies need [a] higher level of care that includes hospitalization and other drugs that are used to calm down a more severe CRS.
With these easier-to-use bispecifics, the next step is how we can combine them with some standard therapies.
Dr. Brody
Bispecifics given as single agents and in earlier lines of treatment
Stephanie, TPS: Bispecifics right now [are] being studied both as single agents, meaning just the bispecifics alone, but also in combination with other treatments that are already being used. We’ll have to see how those turn out.
As we’re also talking about different bispecifics, we know that they’re being tested for later lines — third, fourth, fifth — and then typically what happens is the research tries to move them earlier.
Dr. Brody: The real future of that is not just how good they are alone because we never really cured any cancers alone. We don’t cure some DLBCL patients with C; we cure them with R-CHOP. Combinations are the basis of oncology.
With these easier-to-use bispecifics, the next step is how we can combine them with some standard therapies. That’s already being done. We have some data about that at the ASH [2022] annual meeting and those response rates are extremely high. That is the future.
For now, it’s third-line patients where everything else has failed, but they are very quickly moving up into the second line. We have some data about the second line.
We’ve already started studies bringing them into the first line in combination with standard therapy. It’s a rate of progress. We’re very lucky.
The luckiest thing would be to have no cancer at all, but if you had to have something, [it’s] better to have something where the progress is being made this quickly.
Dr. Falchi: As single agents, I think what we’ve seen is that now, with longer follow-up for these studies, some of those individuals who had a very good response early on tend to maintain that response. There is a suggestion that some of these patients may become long-term disease-free. In other words, being alive and well without evidence of disease at a relatively long follow-up time.
We’re all very cautious toward the word cure, but we certainly believe that there is a potential for these people not to have a recurrence.
[The goal of] adding epcoritamab to that second-line platinum chemotherapy [was] just trying to get complete remission rates up high enough that the transplant would work better.
Dr. Brody
Epcoritamab for transplant-eligible patients who didn’t do well post-transplant
Stephanie, TPS: Thank you, Dr. Falchi. One example is a study that was presented on patients who are eligible for transplant but didn’t do well after the transplant so they’re studying epcoritamab or epco for these patients. What was the main takeaway there?
Dr. Brody: There’s one abstract about epcoritamab plus this aggressive platinum-based chemotherapy. R-DHAOx or R-DHAC are aggressive, platinum-based chemotherapies that are usually a plan B.
Plan A [is] something like R-CHOP and if it doesn’t work, plan B for younger, healthier patients would be to get platinum chemotherapy [like] R-DHAC, R-DHAOx, [or] other similar ones. R-ICE is another similar one there. They’re all just platinum chemotherapies. If it works well, then [they] go on to autologous stem cell transplant.
Stem cell transplant sounds a little elegant because stem cells are involved, but it mostly involves tough chemotherapy. Folks are hospitalized for a while and out of work for a while.
[The goal of] adding epcoritamab to that second-line platinum chemotherapy [was] just trying to get complete remission rates up high enough that the transplant would work better.
In that trial, although patients intended to go on to stem cell transplant, some patients that got complete remission with just epcoritamab plus platinum chemo never did go on to the transplant and are still in remission at beyond a year now.
We cannot yet say if those patients are cured. They may be. A little more follow-up would hopefully confirm that. Epcoritamab is clearly making that chemotherapy work much, much better.
Dr. Falchi: We participated in that study and the early results on a relatively small number of patients appear very promising.
For those patients who are able to complete the program, their chance of response was 100% and the majority of them were complete response, meaning that lymphoma really disappeared. Obviously, we don’t know what’s going to happen in the long term, but there’s certainly a very, very good start.
Importance of patient-reported outcomes
Stephanie, TPS: That sounds so promising. One thing we’d like to highlight is that research relies so heavily on data, on the numbers, and that’s for a very good reason. Putting the numbers and percentages into context is really important.
Some of the research presented at the conference is called PRO or patient-reported outcomes. Very simply, it’s something I hope there’s a lot more of because it gives that context.
There was one report for epcoritamab on quality of life where 61% of interviewed patients reported [a] positive impact on their daily activities after being on the bispecific. Around 40% reported a positive impact on physical, emotional, and/or social functioning and 80% of patients reported being “very satisfied or satisfied with treatment.”
Now, again, [we] want to stress [that] this was a limited sample size. It was in this clinical trial of more than 100 patients. But I do want to ask you, Dr. Brody, why is this information so important to study?
Dr. Brody: Patient-reported outcomes are critical because the other version of that kind of data is so unfulfilling. It is just these kinds of graphs of adverse effect frequencies but that does not tell the story.
If someone had grade-3 toxicity for 20 minutes or for two years, it adds up as the same on the graph. It’s just they had a grade-3 toxicity.
A human experience is that 20 minutes [is] not so bad. Two years? I would rather have a grade-3 toxicity of many types for a day than have a grade-1 toxicity for a year. Grade-1 toxicity for a year, you maybe can’t go to work or can’t work well.
That’s why patient-reported outcomes [are important] especially, I think, for these immunotherapies, especially for bispecifics.
This main side effect for bispecifics, the most common one, is cytokine release syndrome. It can be bad. It can be serious. You can end up in the ICU from it.
The nice thing about it is people either have it or they don’t. Maybe 20% of people have a bad version of that immune overactivation and [for] those that do, [it] mostly lasts for about a day or two. Then they pretty much don’t ever have it again. That is a grade-3 toxicity, but for most people, it is two days, God-willing, out of their life.
The way we normally report these in meetings, abstracts, and publications falls short because the patient’s perspective is that a two-day side effect is not the same as a two-year side effect. It’s totally neglected in the way we present the data. That’s why the patient-reported outcomes are critical and why the numbers, I think, are very promising for these types of immunotherapies.
These are breakthrough therapies that offer hope to a substantial proportion of individuals, of people that would otherwise have very little outlook suffering from a recurrent lymphoma that can be unforgiving.
Dr. Falchi
Breakthrough therapies for DLBCL offer hope
Stephanie, TPS: Asking patients for their perspectives is so important and, again, something I hope will trend in that upward direction.
What is the general takeaway for DLBCL patients and for their loved ones as we go deeper into 2023?
Dr. Falchi: My general takeaway about bispecific is one of great excitement. It is my line of research because I truly believe that these are breakthrough therapies that offer hope to a substantial proportion of individuals, of people that would otherwise have very little outlook suffering from a recurrent lymphoma that can be unforgiving.
Opening avenues of hope for patients with diffuse large B-cell lymphoma that recurs after one or more lines of therapy, which is very, very challenging to deal with, is something that I think we’re all excited about. I’m personally just looking forward every day to what’s coming next and how many more people we can cure hopefully more and more each day.
Stephanie, TPS: Thank you so much, Dr. Falchi and Dr. Brody. So excited by the things that were discussed. We couldn’t cover everything that’s happening. We’ll definitely be putting on more conversations for people who are wondering more comprehensively what’s available out there.
The numbers are promising, but how soon are we going to see this at our hospital or at our clinic? Will it be accessible? What are the side effects? Will I be able to live life while I’m on this treatment?
With everything that’s happening right now, it is so important to be up to speed on the latest that’s happening so that you can ask those questions of your doctor and make sure that you or your loved one is getting the best care possible. Remember, you are not alone.

Thank you to Genmab for their support of our patient education program! The Patient Story retains full editorial control over all content.
DLBCL Patient Stories
Lena V., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 1
Symptoms: Blood in urine
Treatment: Surgery, chemotherapy (R-CHOP), radiation
Cindy M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Itchy skin on the palms and soles of feet; yellow skin and eyes
Treatment: Chemotherapy (R-CHOP)
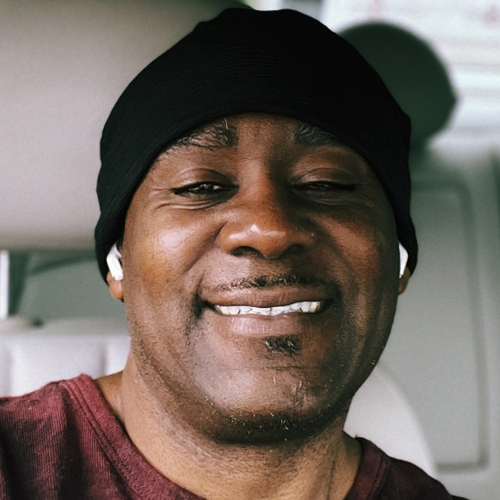
Tony W., Relapsed T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL)
1st Symptoms: A lot of effort needed cycling, body wasn’t responding the same; leg swelling
Treatment: R-CHOP chemotherapy, CAR T-cell therapy
Jonathan S., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Severe shoulder pain
Treatment: 6 rounds of R-CHOP chemotherapy, 10 rounds of methotrexate, 12 rounds of focal radiation, autologous stem cell transplant
Leanne T., Follicular Lymphoma Transformed to DLBCL, Stage 3B
1st Symptoms: Fatigue, persistent cough
Treatment: R-CHOP chemotherapy, 6 rounds
Paige C., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Weight loss, extreme fatigue, swollen lymph nodes in the neck
Treatment: R-EPOCH chemotherapy
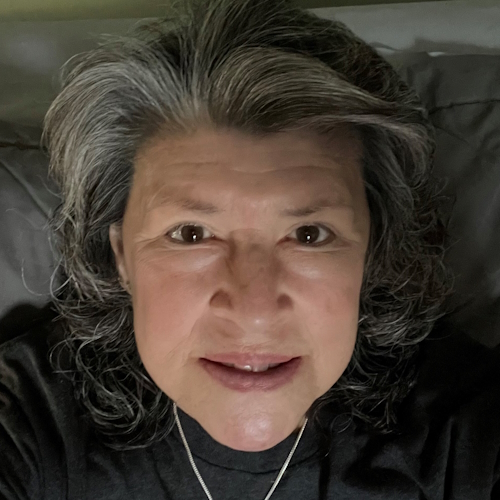
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Kris W., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
1st Symptoms: Pain in the side of the abdomen
Treatment: R-CHOP chemotherapy
Robyn S., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL), Stage 2E
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: R-CHOP, R-ICE, intrathecal, BEAM; autologous stem cell transplant, head and neck radiation, CAR T-cell therapy
Barbara R., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Abdomen and gastric pain
Treatment: Chemotherapy R-CHOP, CAR T-cell therapy, study drug CYT-0851
Luis V., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Persistent cough, fatigue, unexplained weight loss
Treatment: Chemotherapy R-CHOP and methotrexate
Nina L., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Hip and lower extremities pain, night sweats
Treatment: Chemotherapy R-CHOP
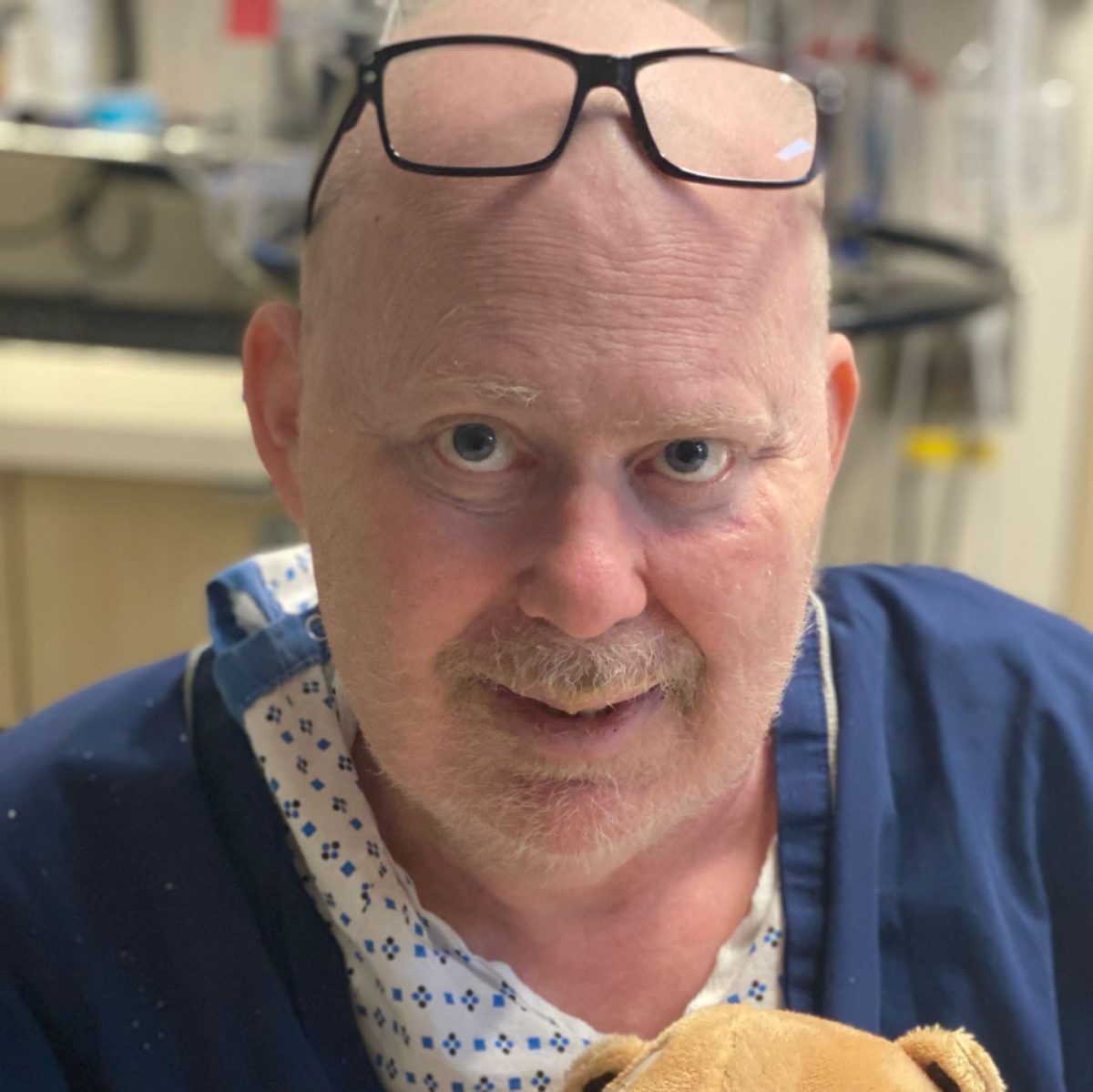
Richard P., Relapsed/Refractory Follicular Lymphoma & DLBCL
1st Symptoms of relapse: Swelling in leg, leg edema Treatment:1st line - R-CHOP chemotherapy, 2nd line - clinical trial of venetoclax-selinexor
Shahzad B., Refractory Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Extreme fatigue
Treatment: R&B, R-ICE, R-EPOCH, CAR T-cell therapy (cell-based gene therapy)
FDA approved: October 2017
Erin R., DLBCL & Burkitt Lymphoma, Stage 4
Cancer details: Characteristics of both subtypes
1st Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatment: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
Emily G., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Pain in left knee
Treatment: R-CHOP chemo (6 cycles), high-dose methotrexate chemo (3 cycles)