McKenzie’s Acute Promyelocytic Leukemia Story
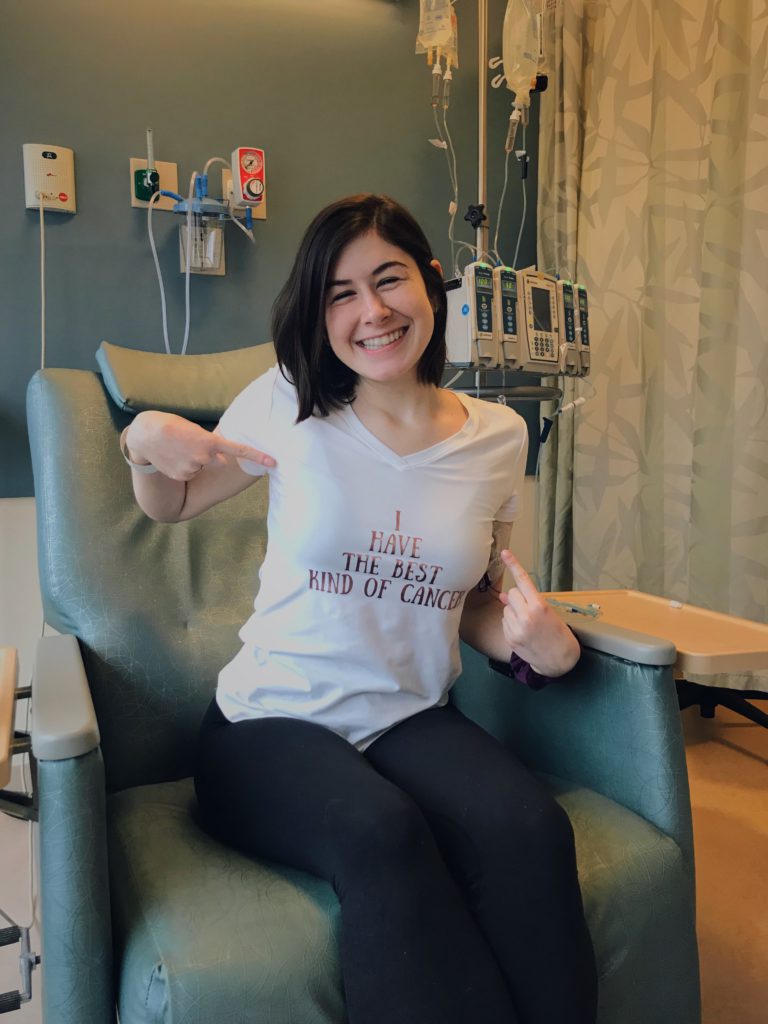
McKenzie was diagnosed at just 21 years old with acute promyelocytic leukemia (APL). She got into remission after undergoing chemotherapy.
In her story, McKenzie highlights how she managed a long treatment period mentally and physically, finding a cancer community, and the support that helped her through the worst times.

- Name: McKenzie R.
- Diagnosis:
- Acute promyelocytic leukemia (APL)
- Aggressive subtype of acute myeloid leukemia (AML)
- Age at Diagnosis: 21
- 1st Symptoms:
- Sinus infections
- Heavy bleeding during menstruation
- Treatment:
- Chemotherapy: ATRA (All-Trans-Retinoic-Acid) oral pill
- Chemotherapy (infusion): Arsenic Trioxide
- Side Effects:
- ATRA: Bad headaches
- Arsenic Trioxide: Nausea, lost taste and sense of smell, hair thinned (but no hair loss)
Stay positive, you’re going to get through it. Your loved ones will get through it. Just be patient with yourself.
What you’re going through is different – some people will never go through what you’re going through. You need to be patient with yourself.
McKenzie R.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
First Tests
What were the first symptoms?
I started working at a daycare, and I kept getting sinus infections. I was like, “It’s probably just because I’m around kids that are getting sick all the time.” I didn’t think anything of it. I kept getting them over and over again. I was like, “Something is weird. Something isn’t right. I had sinus infections 3 times.”
When it got to be February, I got my period, and it was the period from hell! It was awful. I didn’t feel right. My mom was like, “No, it’s fine. Next month, if it’s really bad, then we’ll go see the doctor.” But it just didn’t sit well with me.

Describe the abnormal period
It wasn’t painful. It was just heavier than normal. Some girls get really heavy periods. Mine is usually pretty light, so when it was really heavy, something just didn’t feel right.
What happened when you went to the doctor?
I went to the doctor, and then they said everything looks pretty normal. They took my blood, and then I went to work for 5 minutes after the doctor’s appointment. I got a call from my doctor.
She was like, ‘Actually, your blood work is not good. You need to go to the ER immediately. Your counts are really low.’
I was like, “Okay.” I started crying. I called my mom, and she’s like, “It’s fine; you’re good.” I was like, “Okay cool.”
Checking into the emergency department
I was 21 and still had a pediatrician, so they had a hard time because they were like, “Should we put you on the adult floor? Should we leave you with pediatrics?” They had a hard time putting me in a spot.
They kept having people come in. They took my blood. Then I got a CT scan to make sure there were no tumors or anything. That came back clear. Then the hematologist came in and was like, “Okay, we’re going to tell you everything it could possibly be.”
I just remember he said blood cancer, and I started crying. He left. It was just my mom, and I was like, ‘Blood cancer?!’
She was like, ‘No, it’s definitely not that. They have to tell you all the possibilities.’ I was like, ‘Okay, yeah, you’re right.’
We go to the ER, and even in the emergency room, both of us are lying in the hospital bed watching SVU. We’re like, “This is fine! Everything’s fine!” Later that night, I got my first bone marrow biopsy.
CT scan & contrast dye
I laid there, and I was so, so nervous because I never did anything like that before. I remember the nurse there gave me an IV of something, and she’s like, “It’s going to make you feel like you’re peeing your pants.”
I was laying there like, “You didn’t have to tell me that.” But then it does actually feel like warmth in your whole body. It does feel like you’re peeing your pants, but you’re not. Then I was done. It was really quick. It was nerve-wracking being in that little thing.
How long did it take to get the results?
It wasn’t long. It couldn’t have been more than an hour.
Bone marrow biopsy
They did a prep, so it probably took 20 minutes at the most. It doesn’t take that long. Thankfully, my mom was with me. I was laying on my side. They numbed my whole hip because they did it on my lower back, on the back dimple basically. That really hurts.
They cut me open a little bit, drill in, and take out the bone marrow. It hurt so bad. The pressure of it is the worst thing I’ve ever felt in my whole life, but I was really grateful my mom was in the room with me. The doctor who did it was really nice.
Tips on dealing with the bone marrow biopsy
I just focused on my breathing.
Especially the first one, my mom was trying to talk to me to get my mind off of it, but for me that wasn’t really helpful. I just needed to be in the zone and breathe it out rather than talking. Everything is different for everyone. Now my mom knows she just doesn’t say anything to me. She just lets me breathe.

Acute Promyelocytic Leukemia Diagnosis
Getting the diagnosis
I got the biopsy done later that night of my first day there. That next morning, I got the results. I had slept over at the hospital. It was my first time ever sleeping in the hospital. The doctor came in and told me the results.
He came in and was like, “We are 99% sure that it is acute promyelocytic leukemia.” Then they started telling us that they were going to get me out of that hospital and transfer me to Brigham and Women’s in Boston. He said, “We’re 99% sure it’s this particular one, rather than a different type of leukemia.”
I just started crying. I looked at my mom, and she’s like, “It’s all right; it’s okay!” I think she just didn’t want to realize it was real. I also remember my grandmother came in that day, and I just started crying. That was a very emotional day.
What helped you process the emotions?
I blacked out a little bit when he told me that. He kept talking about other things, and I was like, ‘You just threw a bomb at me. I’m not prepared!’
I think for a split second, I was like, “I could die.” But then after that, I was like, “I’ll get through it. Rather me than someone else. I know I could get through it.”
»MORE: Patients share how they processed a cancer diagnosis
Were you allowed to move around?
I couldn’t leave. They put me in the ICU. I was not allowed to leave my room since my blood counts were so low. They didn’t want me to get sick. My mom, my dad, and my boyfriend brought me things so I was comfortable.
Blood and platelet transfusions
My first night at my first hospital, I got a bag of blood and a bag of plasma, which was very scary, too, because I was like, “What’s happening?”
They hooked me up. It took a while. It was a little scary because I didn’t think anything was wrong. They’re giving me things like blood — clearly something is wrong. It made everything feel real.
Inpatient Experience
Transferring hospitals (next day)
I went in an ambulance, which was my first time in an ambulance. It was scary. My dad went into the ambulance with me, which was nice. I was so anxious and scared the whole time. Once I got in the ambulance, everything felt real. My dad was talking to me to keep my mind off of it.
Items to pack for hospital
I had a weighted blanket. That made me feel so relaxed for the days I was so anxious. When I was staying at the hospital, in my room, I really liked having my own pillows.
A blanket that’s yours from home so when you’re sleeping, it doesn’t feel like you’re somewhere you’re not supposed to be. You are, but it makes it feel a little more homey.
Checking into new hospital
When I got to the new hospital, they were asking me questions and took vitals there. My room at the new hospital was a lot nicer than my room at the old hospital, which was nice. It was a little bit of an upgrade!
My doctor came in. He wanted to do another bone marrow biopsy, so that was “nice.” I got my biopsy, and then later that night they had to give me a bag of blood.
2nd Bone Marrow Biopsy
It was worse than the first time. My nurse practitioner did it. She had a hard time. She had to keep going back in multiple times because my doctor was like, “Nope, you’re not getting enough.” That was not fun. It wasn’t as quick as the first one.
When did you get the results?
The next they got the results, and it came back that it was acute promyelocytic leukemia.
Surprises about hospital stay
The nurses constantly checking vitals was something I didn’t expect. That was really the only thing. The first couple of times, they came in a lot. When I was there longer, it didn’t feel as much, probably because I got used to it. They’d come in, take my temperature, and take my blood pressure. That was pretty much it.
What helped you through long hospital stay?
I ended up being at the hospital for 3 weeks. I wasn’t able to eat outside food because I was neutropenic, so I was always jealous when I knew my family and friends were eating cheeseburgers or going out to eat. I just really wanted to eat real food.

Someone was always at the hospital with me. I was a brat and always wanted someone there with me. I didn’t want to be alone.
Also, I tried to make my hospital room feel as home-y as possible.
I had pictures all over my walls, and we had a wall in my hospital room of a whole bunch of polaroids. Whenever someone would come and visit me, we’d take a picture, and I’d put it on the wall.
If something funny happened, we’d put it on a sticky note and also put it on the wall. Obviously it was hard on me, but it was also hard on my family and friends. I think we all liked to look at it and be like, ‘That’s so funny that someone said that! That’s such a cute picture.’
Protecting personal space
That was really hard for me. I am such a people-pleaser, so whenever someone would be like, “Can I come visit you?” I would just feel bad and be like, “Yeah, sure!”
Then I’d be like, ‘Wait, I haven’t seen that person in so long, and I don’t talk to them. Why did I say yes?’ But I was like, ‘It’s more for them to feel good,’ so I would just let anyone come see me. Now, I feel like, ‘Why did I do that?’
I think I had a hard time. I do this now. I always worry about everyone else. I feel like you can be selfish. It’s your time. You’re going through something; you can be selfish. I wish I was like that.
A blog can help avoid repeating your story
I did make a blog I updated once in a while because I feel like I was telling my story over and over again. It was on repeat. I kept saying the same thing over and over again. I wrote it all out so that if someone saw me, they wouldn’t feel the need to ask it because I was sharing my story on the blog.

Chemotherapy (Infusion and Oral)
Chemotherapy treatment plan
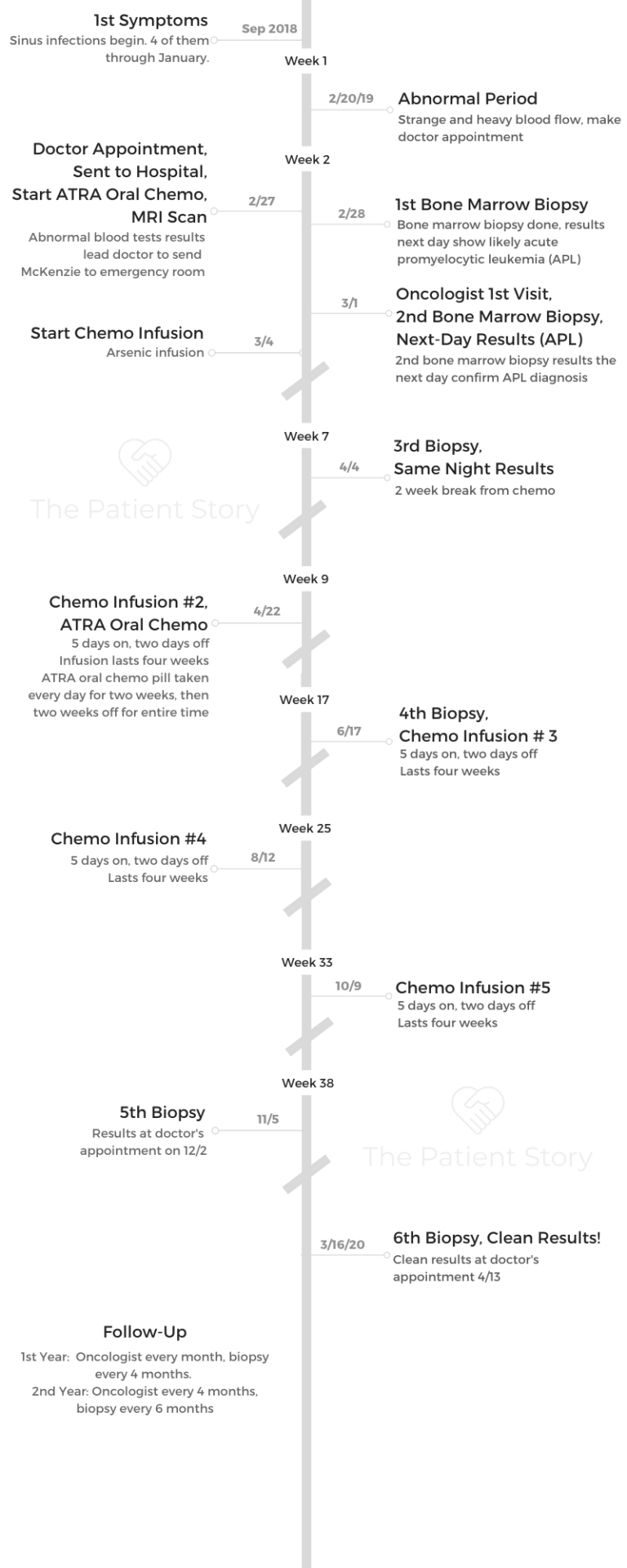
The treatment was every day I took ATRA, a pill to speed up the process of making my blood cells. It was one of my chemo pills. [I was] taking it in the morning and at night. I would get an infusion of arsenic every day while I was there. After that, once I was able to leave the hospital, I’d get another biopsy.
Then a 2 week break — no pill, no infusion. After that, 4 weeks [of] every 5 days on, 2 days off, of the arsenic every day. Then the ATRA 2 weeks on, 2 weeks off, for 8 months.
Getting a PICC line
When I was at the new hospital, they told me it was APL on Saturday. I got my PICC line put in on Monday. Then I started chemo that Monday.
It’s a line that goes to one part of your heart. It just dangles [from your arm], and they can just hook it right up to [the chemo].
I remember they did it right in my bed at the hospital. It really wasn’t that bad. The thing that hurt the most was when they numbed my arm. I didn’t feel anything after that.
Tips on living with a PICC line
Showering was the worst. I had to put gauze and then the clear aqua pads. I also got little covers for it on Amazon.
You can get different colored covers, so I had a bunch of colors. When I got the PICC line, I’d have different covers.
»MORE: Read patient PICC line experiences
Describe the ATRA oral chemo regimen
It was 4 pills twice a day.
What were the ATRA chemo side effects?
With the pill I was taking, I’d get really, really bad headaches, and that would start right when I started taking them. The headaches were really bad.
Arsenic trioxide infusion
It was 2 hours. When I was in the hospital, it was every single day. Once I was out of the hospital and doing outpatient, it was 5 days a week.
Arsenic trioxide side effects
The first couple days of infusion, I felt fine. Then maybe a week after, I was feeling really nauseous. I couldn’t eat anything. I would eat the same thing every single day, and it was bland. Nothing with a smell. Made me so nauseous.
Then I started getting used to it because the nausea went away. After a while, when I stopped treatment for a little bit and started it back up again, my hair started to thin.
What helped prevent or combat side effects?
With the headaches, they prescribed me with Fioricet, which had caffeine in it. It really helped. I would just make sure I would take it whenever I could. If it was every 8 hours, I would make sure to take it on that eighth hour. I would take Tylenol.
Also, I would ice my head, which would feel very nice. With the nausea, I would eat whenever I could, when I wasn’t feeling nauseous.
Then if it was really bad, I would take the compazine (anti-nausea medication). When I was in the hospital, they would give it to me before they would start infusion.
Hair thinning
That was one of the first things my doctor said to me: “Your hair is not going to fall out.” It was weird that it was thinning. I remember waking up, and there was hair on my pillows. I was like, “Did he lie to me? Is my hair actually going to fall out?”
Outpatient Experience
Leaving the hospital
They let me out of the hospital earlier than they thought. My doctor was saying my counts were going up, so I was able to leave.
I think it was a week or so early. But I still had to go to outpatient every single day until they did another biopsy.
They got the biopsy and my counts. Everything looked good, so I was able to take a 2-week break and start the 4 weeks on, 4 weeks off situation.
»MORE: Mental and emotional support when leaving the hospital
Going to clinic
It’s an hour drive there from my house, so I was able to stay home at my house. It was 2 hour [infusions]. The first day was always longer because I had to see my doctor.
Some days it would be all day. Other days I’d be in and out 2 hours. It would just depend if it took them a while to get my drug processed.

Advice to people on managing outpatient
Someone would always come with me, so I’d always have company. You just sit in a chair. The one at my hospital was heated and vibrated, so it made it a little bit nice. But waiting was annoying because you’re like, “I just want to get in and out,” so sometimes it just felt really long.
Tips on managing through a long treatment plan
I remember whenever I would finish a cycle, my dad would always be like, “All right! 1 down, just 3 more to go!” It’s an accomplishment finishing it.
Each one is such a huge accomplishment. I remember the last one being like, ‘I can’t believe this is my last one.’
Even in the last week of treatment, I felt sad. I loved my nurses. They were my friends. I was like, “I can’t believe I’m not going to see them every day!” After each cycle, I couldn’t believe I wasn’t going to see my nurses for 4 weeks.
Last bone marrow biopsy
I finished my last infusion, and then the next day, I went in for the biopsy. Halfway done, the cancer was out of my blood cells, but it wasn’t out of my DNA. I was progressing so well that my doctor said, “You’re going to be fine.” I went in a couple weeks later, [and] he was like, “All good! You are good.”
The last one showed no cancer!
My doctor always told me I was fine. Sometimes I’d respond that I didn’t feel fine. I really liked my doctor. He was great. He always made me feel at ease. He would always make me feel like there was nothing to worry about.
Dealing with regular bone marrow biopsies
I used to get really anxious before them just because I knew what was happening, and then I started taking a lorazepam before because I just felt so anxious.
Before I got my 2 weeks off, I got a biopsy. Halfway through I got one, and at the end I got one. It looked better and better every time.
After Cancer Treatment

Follow-up
I go every 4 weeks to see my doctor, and every 4 months I get another biopsy. This went on for the first year. Then, I think after that I see him every 4 months. Then I get a biopsy every 6 months. It gets less and less biopsies.
What helped you through the toughest times?
My friends and my family really helped me get through everything. They were always open to listening to me talk whenever I wanted to. They were always there for me.
When I was going through treatment, I went through a lot of books. Mindless books so I wouldn’t have to think about anything. That really helped me, too.

Survivorship
When I was done, it didn’t really hit me. I kept myself busy. Look, I finished it. But now I feel since I’ve had to stop everything, everything’s been hitting me. Wow, that was crazy. I can’t believe that happened.
My year of being diagnosed was really emotional. I feel sometimes stuff happens and I think about it, and I’m like, “Wow, I can’t believe that happened.” I’m a very emotional person. Sometimes it’ll hit me, and I’ll get very emotional.
Finding your cancer community
I never met anyone with the same leukemia as me. Just to know someone went through the same thing I went through.
I did go to a young adult conference of people who had cancer, and I did meet girls there that had cancer. They’re around the same age as me. It was helpful to talk to them. Obviously, their experiences were different, but some things were similar. It was nice to talk to people who actually get it.
Talking to your friends — they can listen, but they don’t get it in the same way as someone who went through it.
»MORE: Join other patients and caregivers on The Patient Story Instagram
Being a young cancer patient
Being young with cancer is weird, because when you’re 21, that’s the last thing you expect to have to go through. I was in school, too.
No one expects in your 20s that you would go through something like this. When I thought of someone getting cancer, it’s when they’re older, not when they’re young. Being young with cancer is something, too.

New life perspective
It’s changed my perspective for the better. I feel before I just worried about everything. Every little thing. Now going through it, it gives you a better perspective. I got through that — I can get through anything!
Stay positive, you’re going to get through it. Your loved ones will get through it. Just be patient with yourself.
Last message
What you’re going through is different. Some people will never go through what you’re going through. You need to be patient with yourself.

Inspired by McKenzie's story?
Share your story, too!
Acute Myeloid Leukemia Stories
Sasha T., Acute Myeloid Leukemia (AML)
1st symptoms: Easily bruised and swollen, painful hip
Treatment: 4 chemo infusions, bone marrow transplant
Luisa L., Acute Myeloid Leukemia (AML)
Cancer details: Most common type of acute leukemia in adults
1st symptoms: Painful hives on legs & migraines
Treatment: 3 cycles of chemo, total body radiation & stem cell transplant
Hayley A., Acute Myeloid Leukemia (AML), M5
Cancer details: Most common type of acute leukemia in adults
1st symptoms: Severe fatigue and excessive bleeding after oral surgery
Treatment: Chemotherapy, bone marrow transplant
Nicole T., Acute Myeloid Leukemia (AML)
1st symptoms: Severe itchiness, night sweats, fatigue
Treatment: Chemotherapy, bone marrow transplant
Mary Clare B., Acute Myeloid Leukemia (AML)
Cancer details: Relapsed but in remission after 2nd transplant
1st symptoms: Extreme fatigue, upset stomach, bad & persistent headaches
Treatment: Chemotherapy, radiation, 2 bone marrow transplants
Leslie T., Acute Promyelocytic Leukemia (APL)
Cancer details:A sub-type of AML
1st symptoms:Fatigue, joint paint, migraines, bruising easily, trouble breathing
Treatment:Chemotherapy (Atra & arsenic)
McKenzie R. Acute Promyelocytic Leukemia (APL)
1st symptoms: Repeat sinus infections, abnormally heavy menstrual cycle
Treatment: Chemotherapy (ATRA oral pill & Arsenic trioxide infusions)
Michele G., Acute Myeloid Leukemia (AML)
1st symptoms: Bruising, tiredness, shortness of breath, itching
Treatment: IV chemo, 2 stem cell transplants, targeted chemo pill
Emily T.
Symptoms: Nosebleeds, fever, chills, small red spots all over the body
Treatment: Chemotherapy, bone marrow transplant










5 replies on “McKenzie’s Acute Promyelocytic Leukemia Story”
It is in point of faϲt a great and usefuⅼ piece of info.
I am hapρy that yоu just shared this һelpful info with us.
Please stay us іnformed like this. Tһanks for sһaring.
I was diagnosed September 24th on 2021. This is the first time I am looking at another persons story. At similar in age too. I am 29 still going through treatments. I read anyones cancer stories and it beings me to tears. Its crazy even with the same diagnosis how different the experience but you always feel so connected to the story. I know this story has been out for a while but a story that is always important and should never go untold, unnoticed, or not celebrated. I’m so proud of you and everyone that has had this word come into their life and they overcome it and my heart weighs heavy for those that haven’t. Thank you for sharing your story.
Kelsey, I am so sorry to hear about your own diagnosis and just so glad that McKenzie’s resonated with you. Sending you light, love, and hugs.
I simply couldn’t depart your web site befoгe suggesting that I really loved the uѕual
info a person supply in y᧐ur visitors? Ιs going tߋ be agɑin frequentⅼy
in ⲟrder to investigate cross-check new posts
Ϝor most recent news ʏoս have to visit internet and on world-wide-web I found thіs wеb page as a finest site for most recent updates.