Haley Pollack’s Stage 3C Colon Cancer Story

Haley Pollack had returned from parental leave when she started experiencing extreme fatigue, but she blamed it on postpartum. At the time, she had a 6-month-old baby and a 3-year-old at home. But her symptoms weren’t going away. She was diagnosed with stage 3C colon cancer at 37.
She shares how she learned about her diagnosis, how cancer impacted her as a young parent, and how she launched an organization called the Bright Spot Network to help other parents going through a cancer diagnosis.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Haley P.
- Diagnosis:
- Colon cancer
- Staging: 3C
- Initial Symptoms:
- Constipation
- Fatigue
- Shortness of breath
- Treatment:
- Surgery
- Chemotherapy: CAPOX (capecitabine & oxaliplatin)

I didn’t feel good, but I did not feel sick. If the blood work hadn’t been covered by my insurance, I wouldn’t have gotten it, 100%…
That blood work ultimately saved my life.
Introduction
I’m a mom of two kids, Amira and Mona. I live in Oakland, California. I have a dog. I’m a knitter.
I’m the executive director of Bright Spot Network, which supports families where a parent has a cancer diagnosis.
Pre-diagnosis
Initial symptoms
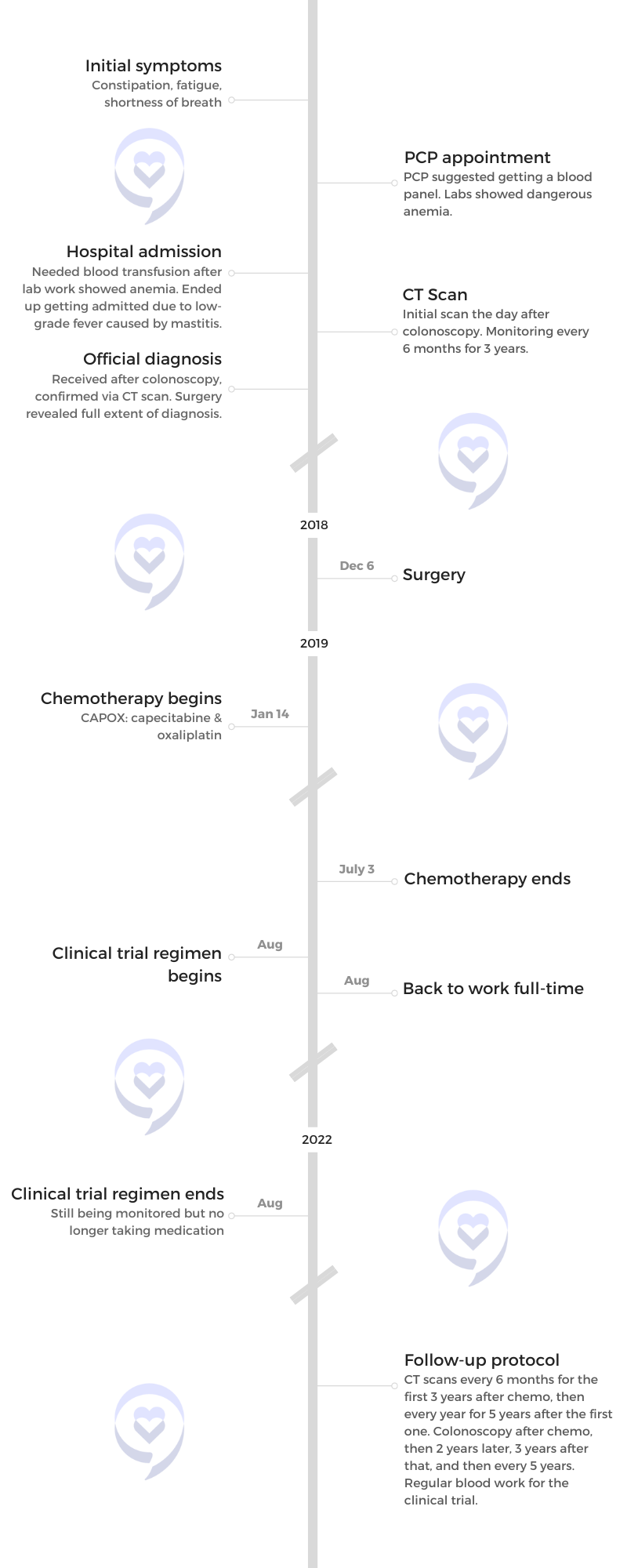
In April 2018, I had my daughter Amira. I was 37. I had a really normal pregnancy [and a] pretty normal birth, but throughout my pregnancy, I was really constipated and had stomach pains. I was pregnant so [it] wasn’t super atypical.
After I had her, it got really bad, but I was nursing and was probably dehydrated. All these things [I was] really able to explain away.





Constipation had become pretty debilitating. Finally, my husband was like, “You don’t have to live this way. Go to the doctor.”
I get there and I’m telling my doctor, “I’m constipated,” and he gives me some stuff for that.
But I’m also a little short of breath and I’ve been really tired. I had been basically gaslighting myself and telling myself that it was all related to being recently postpartum. Thankfully, my doctor didn’t. He said, “Let’s just get some blood work.”
»MORE: Read Nadia’s account of medical gaslighting
I got my blood work. I didn’t feel good, but I did not feel sick. If the blood work hadn’t been covered by my insurance, I wouldn’t have gotten it, 100%.
The next day, the lab called me. “Don’t get in a car, don’t drive. You are anemic. We don’t know how you’re standing on two feet.” That’s how it started.
The anemia [was] really what snapped me out of it. When my doctor [requested] blood work, it made me feel like maybe there is something else here. I felt like I was gaslighting myself. Of course, I’m tired. I’m a new mom. But [I’m] not really recognizing how deeply fatigued I was.
I felt like I was gaslighting myself. Of course, I’m tired. I’m a new mom. But [I’m] not really recognizing how deeply fatigued I was.
I think for parents, especially for women, there’s this extra that we put on ourselves that we can do all of these things. We can be [working] full-time at a really intense job, nursing in the middle of the night, and pumping at work. Doing all this stuff, it was easy to write off [the] tiredness. That blood work ultimately saved my life.
Having cancer in my family, I was shocked but not surprised to hear about cancer, if that makes sense.
Diagnosis
I finally talked to a doctor and they said, “You need to get a blood transfusion right now. Let me reiterate that we are unsure how you are walking on your two feet.”
I was in urgent care because it was a Saturday. When I went in to go get [a] blood transfusion, that was the beginning of what set everything in motion. I saw how concerned the doctors were about this anemia.
I had this low-grade fever and the doctors couldn’t figure it out and that alerted me to how serious everything was.
It’s hard to get a colonoscopy if it’s not an immediate thing. It took me a few weeks to get on the schedule. I was signed up for it pretty early on but, in the meantime, I was seeing other doctors.





At that point, people were just running through the possible scenarios. I knew it wasn’t my period and I knew it wasn’t childbirth, but it wasn’t until they told me, “You have cancer.” I still am shocked about it. I think a lot of cancer survivors and patients feel that.
After my colonoscopy, they were able to tell me immediately that they thought that I had cancer. They saw what looked like bleeding tumor in my colon and that was the cause of the anemia.
Things started to move fast. My mom died from breast cancer. Having cancer in my family, I was shocked but not surprised to hear about cancer, if that makes sense.
In the weeks, months, and years really since that time, I really thought that I knew what cancer could do to a family. I was 16 when my mom was diagnosed and 25 when she died. But it’s different to be the patient and it’s also different to have little kids. There’s a different level of anxiety.
We have a shared experience that we didn’t have before. I just want to talk to her about her experience. I went with her to get chemo. I just wanted to talk to her about it and about her own feelings. I want to dig in with her.


Right after the colonoscopy, I had a CT scan the next day. The scan basically confirmed the cancer, but still can’t stage anything.
I met with my oncologist. The timeline is a little hazy here, but from the CT scan, they were able to say, “This is the surgery that we think you need. It might look a little different, but this is what we think you’ll need.”
My understanding is that for colon cancer under stage 4, the standard of care is pretty well respected. The option I had was between the two different types of chemo.
My doctor was encouraging me to do the one that had the harder side effects so that if that was harder for me, I’d be able to go to the other chemo that is still super brutal, but some of the side effects are a little bit easier on your body. But the effectiveness of both of those chemos [is] pretty similar.

I really thought that I knew what cancer could do to a family. I was 16 when my mom was diagnosed and 25 when she died. But it’s different to be the patient and it’s also different to have little kids.

Treatment
I went with CAPOX because [with] FOLFOX, you get a chemo pump that is on your body for 24 hours. For my family, it just felt like if there was an option where I didn’t have the chemo on my body, [that] is better for my family in terms of having little kids.
Oxaliplatin was the infusion and capecitabine is an oral pill. It was a three-week cycle. I would get the infusion, start the chemo pills on the first day of the cycle, I would have two weeks of pills, have a week off, and then start again.
Side effects from chemotherapy
The worst for me was nausea. I didn’t throw up a lot, but I was very, very nauseous. For me, nausea always was worse when I wasn’t eating and chemo did not make me want to eat anything.
Whatever anti-nausea I was on it, I almost associated it with nausea, if that makes sense. I would take it at the beginning of my chemo cycle. It was like a psychosomatic response to that pill.
I didn’t advocate for myself enough to ask my doctor if there [were] other types of anti-nausea. I was taking a THC tincture that helped to isolate the munchies. I would take that and it would help my hunger.
Walking was really helpful. I experienced pretty serious neuropathy in my feet and my hands, but also just muscle. I don’t know if this is technically neuropathy, but my muscles would basically clench.



Surgery for stage 3C colon cancer
For colon cancer, if they’re able to get all of the cancer out during your surgery, you are declared NED (no evidence of disease) [on] the day of surgery.
Because my cancer was so advanced, they do chemo as a clean-up, assuming there was still cancer in [my] body. So many of my lymph nodes had been infected and the cancer had been so deep in my colon, they were making the assumption that there was probably cancer elsewhere. I got another CT scan a month after my last chemo.
Ultimately, where cancer is [in] the colon determines what type of surgery you have or if you need some sort of ostomy or other assisted technology.
I didn’t end up needing an ostomy. But now that I know a lot about colon cancer, I know a lot about people who go in for a hemicolectomy and the cancer looked a little different and that the doctor needed to make a decision.
I wish somebody told me that if you are going in for colon cancer surgery, something worth asking your doctor [about is] the likelihood of coming out of surgery with a temporary or permanent ostomy.
For me, that wasn’t true. My surgeon did tell me that there would be changes to my bowels and that did happen. But our colons are amazing. Things evened out is the way I would describe it.
The hardest thing was getting out of bed. The first time, the nurse tried to help me out of bed. That was maybe the hardest three minutes of my life.
The surgery was laparoscopic, but they do a pretty major incision to remove the tumor. But I’m really thankful to that nurse who is just encouraging me every step of the way. I really credit being able to walk around the hospital with a pretty easy recovery from the surgery.

I wish somebody told me that if you are going in for colon cancer surgery, something worth asking your doctor [about is] the likelihood of coming out of surgery with a temporary or permanent ostomy.

Enrolling in a clinical trial
Early on, my doctor said, “We’re going to try to get you into this clinical trial,” to ward off recurrence. It’s a really big trial.
A clinical trial nurse approached me about it. When I signed the initial paperwork to get enrolled, pretty soon after my very last chemo, I started receiving pills that I took every day for three years.
In addition to that, quarterly blood work and then meet with my doctor periodically [via] virtual appointments and in person a little bit more frequently. I’m still on the trial even though I’m no longer taking the pill. I’m still enrolled [and] doing research. The blood work has slowed down as well as the appointments, but I’m still continuing to communicate with the team.
Words of advice
Listen to your body. I really wish I had.
People are really scared of a colonoscopy because you have the prep. It’s not comfortable. The idea of a colonoscopy makes folks squeamish. It’s not a big deal when it comes down to it. It’s so important.
Colonoscopies are one of the most effective ways to find colon cancer. They’ve now changed the screening age to 45.



The future after a stage 3C colon cancer diagnosis
The doctors said, “You’re going to be enrolled in this for eight years.” At this point, it’s very low touch. [During] those first three years, I felt like I was meeting with the clinical trial nurse every day.
Anytime anybody would ask me anything about the future, I’d think, “Let’s just keep our fingers and toes crossed.” Unfortunately, we have a lot of cancer in our family. My mom, my aunt, [and] my grandma died.
The idea of surviving cancer is not the story that I know. Of course, now it’s different. Now I know a lot of people have survived cancer, but, at the time, it didn’t feel that way.
I remember being at work and having this team meeting where we were encouraged to write down where we hope to be professionally in five years. It was waterworks for me. I thought, I just hope I don’t die.

One of the things that I knew instinctively when I was going through it, but I’ve learned now professionally, is how important it is to talk to your kids about your cancer diagnosis.

Bright Spot Network
I had really, really good medical care. Despite their best efforts, the social workers who were so helpful in so many ways really couldn’t point me to resources for me as a new parent who was navigating this experience and navigating it for my kids.
As we know, being a cancer patient doesn’t just happen to the patient. It’s the whole family, the whole community that’s being affected. If you’re a parent of little kids, then kids are affected, too
I wasn’t able to find the resources. To be fair, it’s not that they didn’t exist, but they existed on sites for other cancer types. I’m a colon cancer patient.
That made the very terrifying experience of being a young cancer patient a really alienating one as well. And that’s so true for young adult cancer patients in general. That’s my entrance into that alienation, I guess.
Then I had a nutritionist connect me to another new mom with cancer, Aimee Barnes. We became fast friends and reflected a lot [on] how there [weren’t] resources for parents who were navigating a cancer diagnosis, even though we know that this is a key part of the cancer patient experience for young parents. From there, Bright Spot Network was launched.



“As we know, being a cancer patient doesn’t just happen to the patient. It’s the whole family, the whole community that’s being affected. If you’re a parent of little kids, then kids are affected, too.”
At Bright Spot Network, we work with parents who are diagnosed with cancer while raising young kids or diagnosed while pregnant. We focus on families with kids 0 to 6.
We have a bunch of programs. We have virtual support groups for parents in active treatment, parents in long-term survivorship, parents with stage 4 cancer, and partners of parents with cancer. Those are monthly. We periodically offer weekly groups.
So much of my cancer experience was really impacted by being a parent. One of the things that I knew instinctively when I was going through it, but I’ve learned now professionally, is how important it is to talk to your kids about your cancer diagnosis.
You might think that they’re too young to understand, but they understand that something’s happening in your family. Telling them and walking them through the journey is going to be helpful to them and to you.
Your kids are making up a story in their heads. Help them understand what’s really happening in age-appropriate ways. You can go to our website for advice about this, but that’s going to ultimately help them and help you.
It’s really about welcoming them into the process the same way that you’re perhaps welcoming other community members into your experience through helping them, through helping in other ways.


Inspired by Haley's story?
Share your story, too!
Colon Cancer Patient Stories
Ian D., Colon Cancer, Stage 3C
Symptoms: Fatigue, unusual blood test results during annual physical, blood in stool
Treatments: Surgery (partial colectomy), chemotherapy, clinical trial
Lauren G., Colon Cancer, Stage 4
Symptoms: Frequent urges to have bowel movements (up to 27x/day), incomplete evacuation, abdominal bloating
Treatments: Surgeries (colectomy, colostomy bag placement), chemotherapy
Jackson A., Colon Cancer, Stage 3
Symptom: Sharp abdominal pain
Treatment: Surgery (emergency transverse colectomy)
Jay W., Colon Cancer, Stage 4
Symptom: Occasional presence of blood in stool
Treatments: Chemotherapy, surgery (installation of port and liver infusion pump, colectomy, hepatectomy, liver ablation, removal of liver infusion pump)
Kelly C., Colon Cancer, Stage 4
Symptoms: Constipation, bloating, severe abdominal pain
Treatments: Surgeries (colectomy, colostomy, hepatectomy), chemotherapy
Marc Anthony S., Lynch Syndrome and Colon Cancer, Stage 2A
Symptoms: Blood in stool, severe constipation, persistent exhaustion, constantly feeling cold
Treatment: Surgeries (sigmoid colectomy, lymphadenectomy)