Karen’s Stage 1 High-Grade Urothelial Cancer Story

Karen was diagnosed with stage 1 high-grade urothelial cancer after having kidney stones removed. Her story of strength and survival began years earlier.
An armed robbery left her a paraplegic at 19 years old. Since that tragic event, she has been in a wheelchair. Because of her paralysis, she needs to catheterize five times a day to empty her bladder, which eventually led to recurrent UTIs.
A cluster of kidney stones led her to the hospital. When the lithotripsy failed, the doctor put in a scope and saw the tumor.
She shares how she managed her mental health, learned to self-advocate and find a community for support.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Karen R.
- Diagnosis:
- Bladder cancer
- Initial Symptoms:
- Recurrent UTIs
- Treatment:
- BCG immunotherapy
You can’t stop tragic things from happening, but you can definitely use them for good.

I was shot in an armed robbery when I was 19… [I became] T10 complete paraplegic, lost eight units of blood, and was lucky to survive.
Introduction
I live in Baton Rouge, Louisiana.
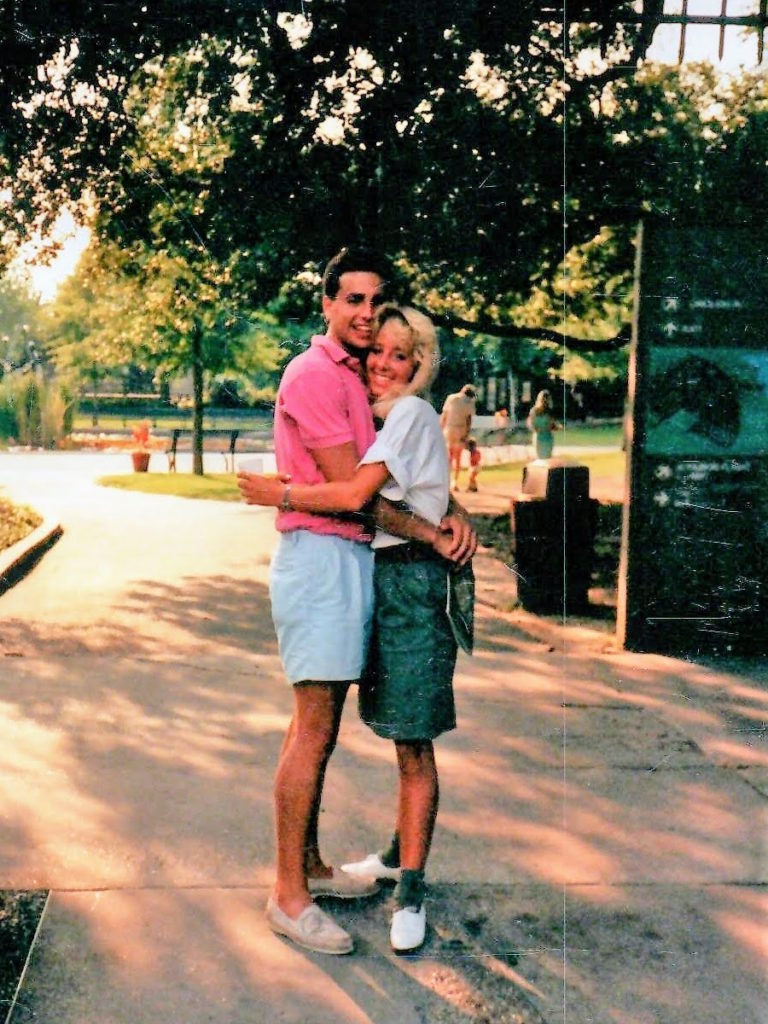
I was shot in an armed robbery when I was 19, [the] beginning of my sophomore year. I was a student at LSU. My boyfriend and I had gone out to this blues place after an LSU game [where] he played guitar that night.
We were going to get in our cars. My car had been broken into so we were looking at that [when] some kids with guns came up from behind us. Somebody put a gun [at me] and grabbed my shoulders. There was a kid with a gun on Mike’s side of the car [who] put a gun to his head.
I got shot in the back point blank as a result of a shuffle that happened. [I became] T10 complete paraplegic, lost eight units of blood, and was lucky to survive.
Crazy way to start college.
[I’ve been] a manual wheelchair user for 35 years as a result. I finished my undergrad in psychology, got a master’s in social work, [and] got married. Not to him — everybody asks me that. We dated for seven years and I called the wedding off after invitations were mailed out.



I met my husband in grad school. He was getting his engineering degree. I had a nine-month-old when I started grad school. Then I became a licensed clinical social worker [and] worked in hospitals for 20 years.
I now work for a company called Numotion. We’re the largest supplier of custom wheelchairs. I still sort of use my social work degree trying to help people with disabilities.
I do a podcast: Life Possible with a Disability. It’s mostly for people with mobility impairments.
I do a lot of social media. Part of my job is social media for people with mobility impairment disabilities. It’s LifePossibleKR on Instagram and Facebook. It’s not just education and super strictly professional. You get to see glimpses into my life.
I let a lot of my personal life bleed over into those channels — maybe more than I should — because I want people to see that life with a disability or with a cancer diagnosis can still be such a beautiful thing.
I think that’s what you do with [a] tragedy. It’s the best way to handle it. And my cancer diagnosis as well. You can’t stop tragic things from happening, but you can definitely use them for good.
I was having a lot of UTIs. But when you [do] intermittent catheterizing, you kind of do so that was not a big, major warning sign.
Pre-diagnosis
Initial urothelial cancer symptoms
Because of my paralysis, I have to do intermittent catheterization to empty my bladder. I have to use a catheter five times a day and that’s just something that I don’t even think much about. [It’s] pretty routine but can cause infections.
Unbeknownst to me at the time and to a lot of people now, there are plastic softeners in catheters that have DEHP (di(2-ethylhexyl) phthalate) in them and that is, of course, a known carcinogen. It’s a combination of a foreign object repeatedly going in and out of your bladder and then the infections. I’m working now and advocating to get DEHP and other carcinogens out of catheters because we need to be able to eliminate that.
It was February. I had a cluster of kidney stones that I ended up in the hospital. One was obstructing and I had to have it removed. Once I healed from that down the road, he said, “There [are] some other stones in there that we’re going to have to deal with.”
Fast forward six months later, he did lithotripsy, where they use sound waves to hammer those stones from the outside of your body, and it “failed” because he said I moved. I was like, “Well, your nurse sedated me, so…” And I was like, “There should probably be a money-back guarantee. I feel like this is your fault.”





The lithotripsy failed. He said, “We’re going to have to go in in a few months and put a scope. I’m going to have to go in with a tool, cut these stones, and pull them out. I don’t want what happened last time to happen again where it obstructs and you could go septic.”
I was having a lot of UTIs. But when you [do] intermittent catheterizing, you kind of do so that was not a big, major warning sign. I didn’t have blood or anything yet.
He went in with that camera to remove the kidney stone and when he did, he saw the tumor. It was a high-grade urothelial cancer that he caught early. Stage 1.
I was lucky that it was not yet in the muscle and I don’t think they normally catch them on stage 1 because you can’t tell. You have to go into the bladder and look. Urine prevents from lighting up a tumor so unless you’re in there looking, you’re not going to see it.
I know how to roll with the punches when it comes to bad news, but I was in a fog.
Urothelial Cancer Diagnosis
After removing the kidney stone, he told my mom and [me] that he thought it probably was [bladder cancer].
When I went to the office, the nurse was coming to get the patient before me, but I could tell [by] the way she looked at me very empathetically. I was like, “Okay, I have cancer.” I felt like I knew before the words came out of his mouth.
But when he said high grade, I was like, “Got it. If I had to have it, [a] low grade would have been better.” I just had all kinds of probably stupid thoughts.
I didn’t cry. I have been through a lot. My husband died in 2016 and I raised teenagers by myself. I’ve always worked. My daughter had cancer as a kid. My mom went through cancer treatment. I know how to roll with the punches when it comes to bad news, but I was in a fog.


Treatment
I started doing my research right away. Being a social worker, I found [the] Bladder Cancer Advocacy Network. They have a podcast called Bladder Cancer Matters. I learned a ton from them and decided to start [treatment].
I love my doctor here, but MD Anderson had blue light cystoscopy and some other avenues if the BCG failed. For this type of cancer, BCG is immunotherapy. It’s actually the tuberculosis vaccine and it’s the most effective treatment.
There’s a shortage [and] I was afraid that I might not be able to get it in Baton Rouge so I started going to MD Anderson for the beginning part of treatment.
There’s still a shortage, but I haven’t had any trouble getting it. [At] MD Anderson, they were actually splitting doses though because the data was showing that a smaller amount was almost exactly the same efficacy. You had to wait for two other patients to split a dose.
It was very difficult driving back and forth to MD Anderson. And honestly, my doctor and I weren’t really seeing eye to eye.
Advocating for yourself is doing tons of research on your own.
The importance of advocating for yourself
Advocacy as a social worker has always been important to me. I knew the importance of advocating for myself, even when you’re at a cancer center of excellence.
My doctor is world-renowned and he’s got fellow student doctors following him around. But when it came down [to] getting the BCG treatment, [a] five-hour drive when you’re getting any kind of chemotherapy or immunotherapy is excruciating.
I decided to take a friend or family member with me [on] every trip and we’d spend one night, like a silver lining of having a cancer diagnosis. But with the trip being so hard on me, it really needed to be worth my time.
I got a cytology report back about six to nine months into treatment where it said that the cancer was back. It was a high-grade urothelial cancer with squamous cell changes and that’s not good news. I found that out on my chart. No one called me.
I couldn’t get my doctor on the phone. I would leave messages and he would have his PA (physician assistant) call back every time, even though I specifically request to speak to him.
He was going to put off another biopsy for four months because of some scheduling problem of his. I was like, “Highly unacceptable. Absolutely not waiting, sorry,” so I get the appointment moved up.





I wanted to speak with him. I’m like, “If this is true and we biopsy today or tomorrow and find out that it is a squamous cell change, what are the next steps?” He basically said, “You’ll need to have your bladder removed.”
Advocating for yourself is doing tons of research on your own. I was like, “From what I’ve read, that’s not the next step. There could be other next steps.”
I’m young. I was 53 at the time. I was like, “I’m not ready to have organs ripped out.” I didn’t drive all the way here for that.
He said, “There are two other patients of mine that didn’t have their bladder removed when I recommended it. I gave them a certain chemo and they’re both dead.” And I was like, “From chemo?” And he’s like, “Yeah.”
Then at some point, I was like, “What does bladder removal look like?” He’s like, “You’ll have to cath.” Heads up: I’ve been cathing for 35 years and if you didn’t read my chart… He didn’t want to come in to talk to me at all. But since he didn’t look at my chart, I was already kind of done with him.
The biopsy was scheduled. We had the biopsy. It was a false positive, so yay me. But I never went back to MD Anderson after that.
It was made very clear to me through the Bladder Cancer Advocacy Network that a good doctor is never offended by a second or third opinion.
How did you find another doctor?
I went back to my doctor [in Baton Rouge]. He trained at the Mayo Clinic and he leads the urology department here. Now, they didn’t have the blue light cystoscopy, but as I went on, I was like, “You know what? That may not be the most important thing here. At this point, [what’s important] are treatment options, somebody [who] cares about me, and actually [knows] me.”
He knows me and his nurse knows me. If I asked to speak to Dr. McCall or [if] there’s a bad lab result, Dr. McCall’s calling me. And he knows I cath. He has friends at Tulane or at LSU Medical School that are MD Anderson- and Mayo Clinic-trained, and that’s what you have to look at, too.
You may not have to go to the cancer center of excellence. There are physicians trained from those facilities that have all the same protocols and maybe more. Maybe they’re willing to do more.


What treatment did you undergo?
I’ve been going through BCG. I’m still going through BCG. I was diagnosed in October 2021. Made a year clear. We had that one scare, but it was a false positive.
I’m [at] the point where every six months, I get scoped and then I get another round of treatment. It’s a three-year thing with no gaps, but I got COVID. You can’t go when you have COVID. I didn’t have bad COVID and I was like, “Can I just hurry up and get treatment?” But you can’t.
I’ve got another scope coming up and another round of treatment, but I feel like it’s mostly in the rearview mirror. A few years but every six months, so it’s not nearly as disruptive.
The first round was six weeks in a row. I went to Houston every week for six weeks. Then you wait three months and you got treatment once a week for three weeks.
I work full time and I’ve got a lot of responsibility. I have three kids in their 20s. I’ve been a single mom for a long time, too, so every six months is like cake compared to what we’ve been through.
I go down the street and I get a full dose. They’re not splitting the dose here, which is nice.
You see how many people really love you that you don’t slow down normally to appreciate.
What challenges did you go through during urothelial cancer treatment?
I try not to put my whole life on hold during treatment and tried to incorporate as many fun things as my body could handle.
One of the best things was when I put it on Facebook, friends I hadn’t seen in 10-15 years reached out in the kindest ways. “I’m not working right now. Do you want a ride? Do you want me to ride with you or drive?”
I’m not one to take a bunch of help. I’m pretty stubbornly independent. But I was like, “Yeah, you know what? You want to go? Because I don’t know if I’m going to feel terrible on that ride home and I need to get back to work.”





I had met my now fiancé in June before the October diagnosis and we were in a long-distance relationship. He lives in Arlington, Tennessee, and I’m in Baton Rouge. We incorporated MD Anderson into our dating life. It’s not the most [ideal], but I didn’t want to not see him or not see my friends.
Now, I can look back and say you see how many people really love you that you don’t slow down normally to appreciate.
It’s a financial burden, especially if you’re trying to travel out of state for treatment.
I reached out to the MD Anderson social worker. They have all the resources. I found out there were programs that helped with hotel and/or mileage. But it does get expensive, especially if you’re missing some work.
My work [was] amazing. If I travel during the week for treatment, I could work at night [or] on the weekends. They were great.
Go straight to your type of cancer and find the advocacy network that’s most popular because they are armed with a ton of information.
Words of advice
When I got shot at 19, I realized that doctors are not omnipotent. Most of them start off with great intentions, but they don’t know everything. I learned that really fast being thrown into the medical world at such a young age.
Yes, there are many brilliant physicians out there and I admire them for persisting through medical school and all that. But every doctor doesn’t know everything.
In grad school, I learned about statistics, how to read a study, and to look for biases in the studies. If the study is done by a radiation oncology department, they may have a bias toward radiation. You have to look at the study and who did it. You have to find as much information as you can.
My daughter had cancer growing up and it was rare. Again, I had to fight a lot of fights. It was based [on] me being armed with as much knowledge as I could find.
Go straight to your type of cancer and find the advocacy network that’s most popular because they are armed with a ton of information. That’s how I found out about the BCG shortage and the standard of care for a high-grade urothelial noninvasive cancer. I would go straight to one of those advocacy networks.





Find a mentor. Find physicians [with] that specialty.
Ask a bunch of questions. I wanted to know the most effective course of treatment according to the data. I also wanted to know if this fails, then what’s next? What other options exist? And that obviously served me well down the road.
Who are the best physicians in the country? Can I get there? Can I afford to? Where could I stay to get a second opinion?
It was made very clear to me through the Bladder Cancer Advocacy Network that a good doctor is never offended by a second or third opinion.
When your tribe reaches out to help you, they want to help.
Trying to not take it on all yourself
For some people, that’s really hard. I happen to be one of them — wheelchair or no wheelchair.
When my mom moved in with me recently, she’s like, “Can I help you?” I usually say no. I’m like, “I got it.” But now, I started saying yes.
“What can I do?” I’m like, “You want to bring me a pizza?” When your tribe reaches out to help you, they want to help. Saying no is almost a disservice to your friend.


Resources to help with the financial burden of cancer
Social workers are the plethora of information. If they don’t have it, they will find it. I just reached out. That’s how I found everything that was available and where.
There are programs out there but no one’s going to present you with the welcome packet that says, “Here are all the things we have to offer.” It takes a little digging.
Whatever your particular diagnosis is, a lot of them have nonprofit organizations that have resources. If it’s a financial burden, you need to reach out to the facility and to your advocacy network.



Talk to people in the waiting room. They may have done it for years and really know the ropes.
Taking care of your mental health
Being a social worker, I would say [you] might require some counseling. You shouldn’t be afraid to reach out for that as well. See what benefits you have through work or other mentioned things.
Having a mentor through the Bladder Cancer Advocacy Network was really helpful because you get to hear other people’s stories. Honestly, I learned a lot in the waiting room from other people waiting for treatment.
Talk to people in the waiting room. They may have done it for years and really know the ropes. That was how I learned I could get the BCG in Baton Rouge probably, not from anyone else. My doctor mentioned it early on, but I was thinking the best thing for me was a cancer center of excellence.
Bad things are going to happen and all you can do is really make the best of it.


Staying positive
So much of being diagnosed and hearing that you have cancer is such a mental strain. Your brain goes to the worst places. Stay really positive throughout the whole thing. Sounds very cliché, I know.
A lot of how a diagnosis of any sort impacts you, you get to frame it however you choose. It takes a minute because you can die. That’s the first thing you think of. “I could die.”
There’s a lot of data to show the connection between a positive mental attitude and a good outcome. It’s not the cure-all, but it sure doesn’t hurt.
I am just bound and determined not to let life get me down. But, obviously, my fiancé, my children, my mom, and my friends, knowing that you’re really loved and appreciated.
A sense of humor. That was really important. That helps.
I’m not saying it’s easy. When I got shot, I said, “This is not fair. I’m a good girl.” I was a rule follower, scared to death of my parents, and just a good kid. My father said that fair was for games like Monopoly and that he never told me life was going to be fair. I was like, “Okay, well, that sucks.”
But it does put it in perspective, right? Bad things are going to happen and all you can do is really make the best of it.

Inspired by Karen's story?
Share your story, too!
More Bladder Cancer Stories
Vickie D.
Symptoms: Intermittent pain in the gut and burning sesnsation
Treatment: Chemotherapy (dd-MVAC) and cystectomy (bladder removal surgery)
Margo W.
1st Symptoms: Blood in urine
Treatment: Chemotherapy (methotrexate, vinblastine, doxorubicin and cisplatin) and radical cystectomy
LaSonya D.
Symptom: Blood in urine
Treatment: BCG immunotherapy, cystectomy (bladder removal surgery)
Ebony G.
1st Symptoms: Blood in urine, weight gain
Treatment: MVAC chemotherapy, bladder removal surgery, neobladder
Diagnosis and Treatment for Bladder Cancer
Learn about the diagnosis and treatment process from bladder cancer survivors and medical experts. Discover diagnosis and treatment options./p>
Bladder Cancer Series
Bladder cancer patients Ebony & LaSonya talk about their cancer journey, including their first symptoms, how they processed their diagnosis, treatment options, and how they found support. Dr. Samuel Washington, a urologic surgeon, also gives an overview of bladder cancer and its treatments.






