Stephanie’s Stage 4 MCL Non-Hodgkin’s Lymphoma Story

Stephanie was surprised when abnormal blood tests led to a diagnosis of stage 4 mantle cell lymphoma (MCL).
Stephanie’s journey includes a year and a half of watch and wait, a clinical trial and hyper-CVAD chemotherapy.
Through all this, she learned the importance of asking questions and celebrating the little things.
Thank you for sharing your story with us, Stephanie!
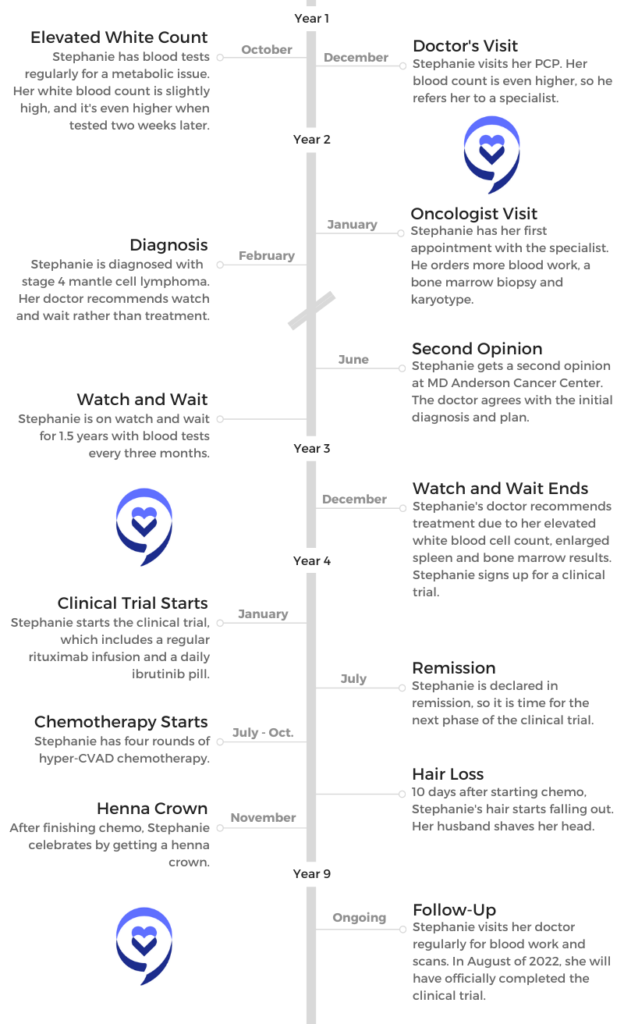
- Name: Stephanie R.
- 1st Symptoms:
- Elevated white blood cell count
- Diagnosis
- Non-Hodgkin’s lymphoma
- Subtype: Mantle cell lymphoma
- Stage: 4
- Treatment
- Watch and wait (1.5 years)
- Clinical trial
- Rituxan (rituximab)
- Ibrutinib
- Hyper-CVAD chemotherapy
- MCL Diagnosis and Watch & Wait
- Introduction
- Bone marrow biopsy
- The Diagnosis
- Watch and Wait
- Being on watch and wait instead of treatment
- Processing not being in treatment
- What questions do you recommend asking your doctor?
- Finding an MCL specialist
- The importance of advocating for yourself
- Choosing to stay with MD Anderson
- Being on watch and wait for 1.5 years
- Helpful tips for dealing with the wait
- Healthy distractions
- MCL Treatment and Clinical Trial
- More Mantle Cell Lymphoma Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
MCL Diagnosis and Watch & Wait
Introduction
Tell us about yourself
I’m a scientist by training. I’m a molecular biologist. I work in the biotechnology industry, in the patient advocacy space at the moment. I’ve done research for a number of years, and then I worked for a patient advocacy organization for about 10 years before joining the company I’m at right now. I’m married. I have a fur baby — no children, but a cat I love dearly. I live in Texas.
I’ve been in cancer research, so I’ve been in hospitals, I’ve been in cancer wards, and I’ve walked with cancer patients through their journey. But I was going in for me, and as I walked in and it was for me, it hit me in the face that they think I have cancer.
How did you discover you had cancer?
I have a metabolic issue that requires that I get blood work done periodically. At this point, it’s about twice a year. I was going in for a regular checkup, and they took blood. It came back with a high white blood count, which isn’t necessarily anything to worry about, but it was unusual.
They recommended I get it checked in a couple of weeks, so I did. It could have been an infection or something. I went back in a couple of weeks, and it was up a little higher still. Then they recommended that I get it tested again, and it was a little higher still.
By that point, I had followed up with my primary care physician, who let me know he was concerned about that and recommended that I see a specialist.
I was a little concerned because I had seen the white blood count go up, and the first one was a little bit high. The next one was just a little bit higher still. That third one was definitely high, and it was still going up, not coming back down.

He said, “This doesn’t look like a normal infection. You might have some sort of viral infection that you’re just taking a long time to get rid of, or there’s a number of other things it could be. I just would feel better if you would see a specialist.”
He did not at any point say, “Cancer.” It wasn’t in my head that he was thinking cancer, but I was a little concerned. I thought something was going on.
Realizing it might be cancer
He said, “This is the office I’m going to refer you to. They’ll set you up with an appointment, and you’ll go in.” I looked, and it occurred to me that it was an oncology office, but it didn’t really sink in that it was an oncology office until I was walking into the oncology office.
I think my background got me because I’ve been in cancer research, so I’ve been in hospitals, I’ve been in cancer wards, and I’ve walked with cancer patients through their journey. But I was going in for me, and as I walked in and it was for me, it hit me in the face that they think I have cancer.
I was a little surprised that it hadn’t occurred to me until that moment that this is what was happening. I was thinking it was some sort of an infection. It’s a high white blood count. It’s really not that big of a deal.
I didn’t really know much about blood cancers, but I knew a little bit about CML and some of the more common ones, so I was starting to think maybe it was something like that.
I knew I was doing what I needed to do, so I just moved forward even though I was quite nervous that day. At the point that it hit me, it really kind of threw me off my game. I was not going in in a good headspace.

Waiting for an appointment
All this happened toward the end of 2014. The holidays got in the way. By the time they made the referral, we had to get through the holidays and the new year and get in. It was a good about 6 weeks between when he said, “You need to see a specialist,” and when I actually got in to see the specialist, which is probably why I was not all that worried about it.
They didn’t seem all that worried about needing to see me very quickly. Once I saw him for the initial consultation, there were follow-up appointments, and those took a while for the same reason. It began to wear on me, I would say.
Once it occurred to me that they thought I had cancer, I was in a hurry for them to figure out what it was, and they weren’t in such a hurry. We need to figure this out because I need to do something. Why are you not in more of a hurry?
Undergoing scans and tests
Up until the point I saw the specialist, it had just been blood tests. They were looking at my white blood count. He did more blood tests, but he did significantly more blood tests. I felt like perhaps they were draining me of all my blood.
But he also ordered a bone marrow biopsy and a CT scan, just to see what was going on. He didn’t order the CT scan on that first visit. That was a follow-up visit. There were quite a few tests.
Then it turns out they were drawing all the blood because not only were they doing blood tests, but they were doing what’s called the karyotype to look at my genetic markers, because that’s eventually how I was diagnosed. I had a translocation. Two of my chromosomes had flipped, and that’s how they determined I had MCL.
CT Scans
The CT scan is just a long day. I don’t find it particularly difficult, and every one I’ve ever had has been in sort of an open unit. You do have to be alone in a room. They give you either something to drink or sometimes an IV infusion or sometimes both, depending on what they’re using as markers. It’s a radioactive marker.
You’re alone in a room because you’re suddenly radioactive, and they give you some guidance about when you go home. It sheds pretty quickly, but you have to be careful for a little while around your family.
Then you have to wait for like an hour while it works its way through your body, and then they take you in for the scan. The scan itself takes like 20 minutes. Usually you lay on a bed. They move you through and sort of coach you through the whole thing.
I don’t find that part particularly difficult, but some people don’t love being in the machine. I don’t like the waiting part. That’s the part that gets me. The first one was a CT scan. I’ve had several PET scans since then.
Bone marrow biopsy
The bone marrow biopsy is not fun. Basically they are taking a giant needle and putting it into the middle of your hip bone to take some of the marrow out. The marrow is what’s in the middle part of your bone.
It’s painful. I’m not going to lie. They will give you things to help you through it. Keep moving afterwards, because if you get still, you get really stiff and sore. I learned that the hard way.
They will often tell you things like Claritin or an antihistamine will help with the pain. I’ve heard people say that it did. It didn’t for me, so just know that. Not everybody reacts the same. I found Tylenol or Advil to be sufficient, but talk to them about that because it can affect other things that you might be on.
The Diagnosis
How did they use the tests to figure out you had cancer?
The tracer that you drink for your CT scan, certain cells in your body will absorb it faster than other cells. Those are rapidly growing cells. If you have a cancer, it will absorb it, and it will show up on the scan more than your typical organs.
There are a few other things that can show up, but they know what those are. They can look at them as background noise. That will tell them if you have, in my case, cancer in any of your lymph nodes or maybe in your spleen or wherever it might show up.
I didn’t on that first scan. Nothing showed up on the CT scan. But it’s one of the things they did to try to identify exactly what was going on and how much it had spread or how much it was through my body.

The bone marrow biopsy was the same thing. They were looking at my bone marrow to see if it was infected with any sort of cancer cells. My bone marrow was showing some lymphoma cells in it.
That’s how I was originally staged with stage 4 non-Hodgkin’s mantle cell lymphoma. At first they thought it could be CML, which is chronic myelogenous leukemia, or a couple of other more common things just because of the way it presented with me.
I was still in denial. Maybe I was still thinking, ‘It’s probably nothing there. They’re just being careful.’
Translocation
In the blood test that they ran, they did a karyotype, and they looked at my chromosomes. Everybody has 23 pairs of chromosomes. You probably know X and Y. That determines your sex. You have 22 other pairs as well.
With mantle cell lymphoma, 2 of them trade places, and it’s a specific 2. They were looking at that, and with chronic myelogenous leukemia, a different 2 trade places. I ended up being diagnosed with mantle cell lymphoma.
That’s called a translocation when they move, and I had the one that’s typical for mantle cell lymphoma. Other than that, all I had was the high white blood count, and then it did show up in my bone marrow.
»MORE: Genetic Testing for Cancer
Receiving the diagnosis
It was the first time when I went back for the results from all these tests. I was still in denial. Maybe I was still thinking, “There’s probably nothing there. They’re just being careful.” Then when he sat me down, he showed me. I ask a lot of questions, so he showed me all the results and explained everything to me really well.
All I could think about is, ‘I am not telling my mom on her birthday, and I can’t do this at the baby shower. So I guess I have to tell them on Wednesday.’
I would advise you to take somebody with you to any of these appointments, and I’ll get to that in a minute. Your brain will stop working, and you need somebody there that can ask questions. When he was like, “These results tell me that you have mantle cell lymphoma,” my brain clicked off.
The only other thing I could tell you that he told me was, “Do not go online and look this up.” So of course, what’s the first thing I did? It was to go online and look it up. He told me I had mantle cell lymphoma. My brain clicked off. I remember thinking, “I don’t want to die.”
He explained to me what some treatment options and things were. I couldn’t tell you what he said. I had to go back for a follow-up to sort of decide what course we were going to take. That’s the point at which I started paying attention to what the options were.
»MORE: Reacting to a Cancer Diagnosis
How did you break the news to your loved ones?
I’m married. The first thing I thought is, “Oh, dear God, I have to tell my husband.” Then the next part of that was, “And I’m going to have to explain it to him, because he doesn’t know cancer like I know cancer.” We have a very healthy, good relationship, and he’s very strong and supportive.
It took me a minute to be like, “Oh, I have to say this out loud, and I have to tell him.” When he got home from work that night, he knew I had a doctor’s appointment. He asked how it went, and I told him. He just sort of listened to me download how I was feeling about all of it.
Then he was like, “When are you going to tell your family?” Meaning my mom and my brothers and my sisters-in-law. This was in February, and it was the week of my mom’s birthday and the baby shower we were having for my sister. All I could think about is, “I am not telling my mom on her birthday, and I can’t do this at the baby shower. So I guess I have to tell them on Wednesday.”
»MORE: How To Tell Your Family and Friends

Watch and Wait
Being on watch and wait instead of treatment
He did recommend watch and wait. We talked about it more at that second appointment, when I actually could hear what he was telling me. I honestly hadn’t ever paid attention to watch and wait. It was something that was recommended for certain cancers, but in the world I worked in, it wasn’t really an option.
I asked a lot of questions. I was like, “What? Why are we not going to do something? You just told me I have stage 4 lymphoma. I feel like we should do something.” He did a great job of explaining to me that, yes, it was stage 4. I worked in breast cancer at the time.
He literally sat down and looked me in the face and was like, “This is not breast cancer. You have to trust me. Ask your questions. This isn’t the same thing. Just because you have stage 4 doesn’t mean you’re actively dying in the next short period of time. At the moment, it looks like you have a not-aggressive form that’s not spreading very rapidly. It will be better if we can watch and wait for a while, because once we start treatment, we’re down a path that we have to continue until you go to remission. We can’t just keep switching treatments forever.”
Processing not being in treatment
I understood that, but I didn’t like it all that much. We know that there’s something big wrong with me, and we’re not doing anything about it. I have to figure out how to just walk around knowing that I have cancer growing inside of me. But I understood why he made the recommendation.
I asked enough questions to get comfortable with that. He was saying the first choice would probably be chemotherapy. I was like, “I don’t really want to go through chemotherapy if I don’t need to go through chemotherapy. You can tolerate this.”
He was also really good and would check in with me and be like, “Some people just can’t cope with this, so if you really can’t cope with this, let me know and we’ll figure out a different path.” Just the fact that he would check on me and ask made me able to do it a little bit longer.
What questions do you recommend asking your doctor?
I think people worry about different things. I wanted to know what were the other choices? What does treatment look like? How long are people on watch and wait? How will we know if it’s progressing? I needed to do something. Those were the things that were bothering me, and so that’s what I asked about.
I did get a second opinion just to make sure that was the right approach, but they did also recommend watching and waiting between the 2 oncologists. They both had patients that were on watch and wait for significant amounts of time. I asked about that.
That also really helped me because I realized I didn’t know how long I would be on watch and wait, but it could be like 5 or 10 years. That was significant because, again, the other choice at the time was chemotherapy. If I could postpone that for 5 or 10 years, why wouldn’t I?
Finding an MCL specialist
He was local to me and at a good cancer clinic. It was certainly in a community setting, not an academic research institution. I live not close, but a reasonable distance from an excellent academic medical center, MD Anderson.
It’s super important for you to advocate for yourself. You know yourself.
I drove down to MD Anderson and got a second opinion there, and I picked MD Anderson because they have a lymphoma clinic. They have a couple of specialists there that literally focus on lymphoma.
The importance of advocating for yourself
It’s super important for you to advocate for yourself. You know yourself. You know if you feel comfortable with the decision or if you have any questions that are sort of lingering with you.
I would say you should always get a second opinion. Some doctors may give you a vibe, or you may feel like you’re getting a vibe that they don’t want you to. But by and large, they appreciate your involvement and your engagement.
Most oncologists at least will welcome a second opinion because they know that your life is in their hands, too. If somebody else sees something different, then they can collaborate and figure out what’s the best approach. If it’s the same recommendation, then that’s confirmation.
I’ve heard a few stories of patients that felt uncomfortable about getting a second opinion. I’ve never known a doctor to be like, “I hate it when a patient gets a second opinion.”
You’re making big decisions. I worked in the field, but this was not my area of expertise, and I was making decisions I didn’t have a lot of information about. More information is better, and if you can get a little bit more information, it just gives you a little bit more confidence about what decisions you’re making.
»MORE: Cancer Patient Advocate

Choosing to stay with MD Anderson
I did end up being treated at MD Anderson when I was eventually treated. I was very open with my local oncologist about it, and MD Anderson was very good at working with him. It’s not like I live in Houston. It’s a few hours away. They worked together. When I would get tests done at one place, they would send them to the other. I don’t know that it would always work like that.
In general, most academic medical centers (if you’re traveling to get there) are very willing to work with you locally and make it easier on you because the travel is not easy. I just felt more comfortable being treated at an institution that saw a good number of patients with what I had and had some experience.
It was blood tests every 3 months and CT scans every 6. I did both at my local center, and then MD Anderson recommended that I come back in a year just to get checked there again. I did a year of follow-up with my local oncologist, and then I went back to Houston and got that second CT scan done there.

Being on watch and wait for 1.5 years
When we talked about it originally, I asked a lot of questions and got comfortable with the decision, because I understood that we were trying to delay chemotherapy, but it was a hard year and a half.
This is not actually a normal symptom of MCL. I just happened to have this symptom: my white blood count continued to go up every single time. It went up a little bit sometimes, and it went up a lot sometimes.
Every time I was like, “Is this the day that they’re going to tell me I need treatment? Is this the day that they’re going to tell me?” I would wake up, and if I had a sore throat or I felt like maybe something was kind of swollen, I would be very worried. I would call and ask if we needed to have that checked out.
While I was comfortable with the decision, it was not a peaceful time at all. I was maybe a little hypervigilant compared to most, because I literally was worried about everything. They probably got tired of me calling and asking them if they need to check this out or what was going on.
Helpful tips for dealing with the wait
I would fall back on, “I’ve gotten the opinion of 2 doctors. They have experience with this. Other people have gone through this.”
I wasn’t really part of a support group or anything at the time. In hindsight, I probably maybe should have found a group to talk to, but I didn’t have one.
I would just sort of rely on all those reasons I had made that decision: that they were monitoring me, that they were seeing the same things I was seeing, and they still thought it was okay. I would talk myself down basically.
Healthy distractions
I did pick up my exercise routine a little bit, and I changed up my diet. “I’m going to give myself the best chance I can to prolong this as long as I can,” I thought. I went on an anti-inflammatory diet and was actually in pretty good shape. I have no idea if it did anything for the MCL or not, but it was good for me. It made me feel like I was doing what I could.
»MORE: Eating Healthy During Cancer Treatment
MCL Treatment and Clinical Trial
Treatment Options
How did you know it was time to start treatment?
While I was on watch and wait, I was being seen by my local oncologist, and they were doing regular blood tests and then periodic CT scans. I had had the 2 CT scans locally and then realized it was time that I needed to go back to MD Anderson to check in with them.
I made an appointment with them, and my most recent blood test from my local oncologist was quite high. My white blood count was 125. I was a little worried about that. I really felt like even though it absolutely was time for me to go back to MD Anderson, I was sort of prompted to go because I wanted to just get the second opinion again.

This time they did the same workup. They drew the blood again. They did another CT scan, and they did another bone marrow biopsy. Not only was my white blood count quite high, but my spleen was significantly enlarged and showed up on the CT scan, which hadn’t showed up locally. My bone marrow was significantly more affected.
We had the conversation about treatment because they were most worried about my spleen. I’ll admit it. Having now seen the picture, it was quite enlarged. I didn’t really notice anything. I just felt a little full when I would eat, unusually full. That’s because it slowly got larger, and I didn’t really notice until they saw it on the scan.
How did you react to the idea of starting treatment?
As I had mentioned previously, every time I sneezed, I basically was like, “Is this it? Is this when I need to go for treatment?” My first reaction was, “This is what it’s like. Now it’s time. We’re here.” I had also told you that when I was first diagnosed, the option had been watch and wait or chemo.
My immediate thought was, “Now it’s time. Oh, crap. I need chemo.” I was quite scared about that. I knew we needed to treat the cancer, but I also know what chemo can do to you. I was not very happy about it. Plus, then what about my job and all this other stuff I have to do?

Exploring a clinical trial as a treatment option
This was at MD Anderson with my oncologist there. He’s a research specialist, and he explained what the treatment choices were. He also explained that there was a clinical trial. He had started it as a smaller trial, and he had just gotten approval to expand it to double the number of patients. It was originally 50 patients, and he got approval to double it to 100.
Of course, I was interested because I have a research background, and that’s what I do. The beauty of this clinical trial was testing a combination of 2 targeted therapies, or drugs that we call biologic drugs.
It’s not chemotherapy or chemicals that kill basically anything that’s growing. It’s kind of like carpet bombing your body, but it kills the cancer. Biologics are more targeted. They find something specific about the cancer cell and attack that. They can occasionally have some side effects, but it’s not the mass toxicity that you get from chemotherapy.
This was a combination of 2 of them that I asked a million questions about. The data looked like it was a good combination that would be effective. After you responded to those drugs — assuming you responded to those drugs — then they would follow with just a couple rounds of chemotherapy, because they have to offer you the standard of treatment.
Something that a lot of people don’t necessarily understand about cancer clinical trials is that you have to get at least whatever the standard of treatment is, and you usually get more. It’s more screening, it’s more follow-up, and it’s an additional drug. There’s no placebo.
»MORE: Clinical Trials in Cancer
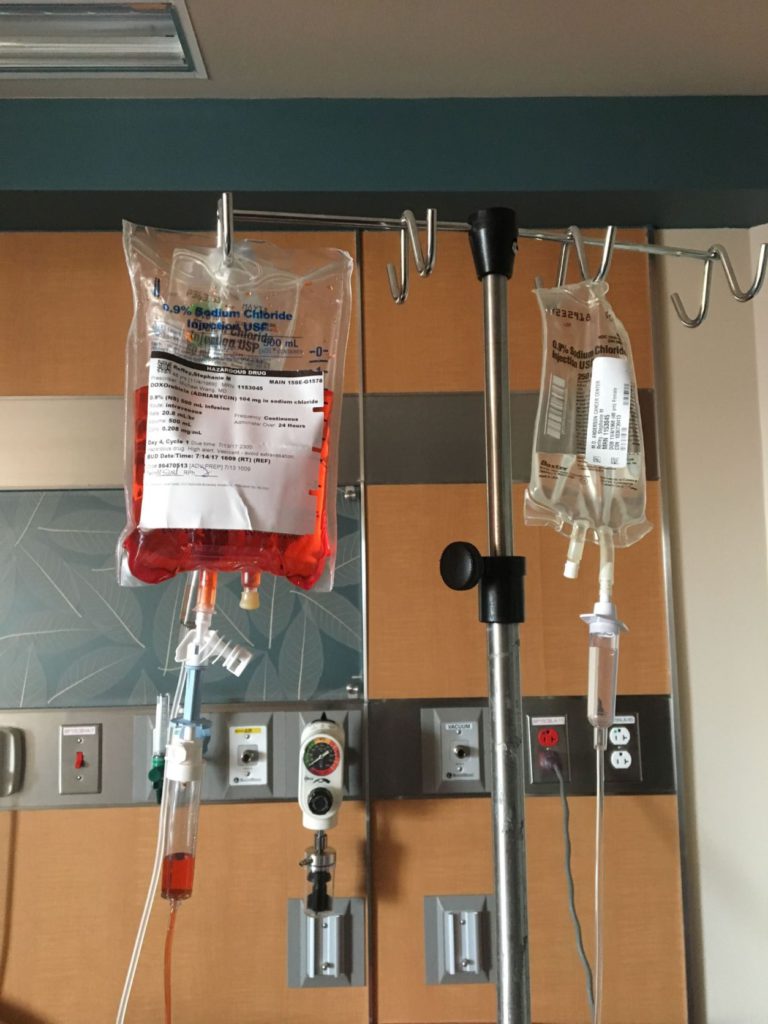
Hyper-CVAD chemotherapy
There are 8 drugs in the chemotherapy, yet it’s an A/B cycle. Cycle 1, you get the A drugs, which there’s 4 of. Then cycle B, you get the other 4 drugs. Then you go back to A, and then you go back to B.
Hyper-CVAD will take the disease down, but it won’t knock it out. It was unheard of to get to full remission with hyper-CVAD.
It’s an infusion. It’s a 4- to 6-day infusion, depending on which cycle it is. Then you have 3 weeks off, and then you go back for the next cycle. It’s the more aggressive of the chemotherapy treatments for MCL, but because I was younger and pretty healthy otherwise, that was what they were recommending for me.
If I had been an older patient, they probably would have picked a different regimen because hyper-CVAD’s tough. It’s the same regimen they give you if they’re doing a bone marrow transplant.
»MORE: Chemotherapy
Factors to consider and questions to ask
First of all, when you’re considering a clinical trial, keep in mind that yes, it is experimental, but in the cancer world, they believe it’s better than the current standard of treatment.
I would ask why they think that? What are the data? You may not care about that. I did, so I asked a lot of questions about, “How’d they come up with this combination, and why do they think this is better, and what are the outcomes with just the hyper-CVAD?”
For a lot of other people, they just want to know why they’re recommending this clinical trial. “How many other people are in the clinical trial? Are there people like me in the clinical trial?”
I was a young woman with what is most commonly an old man disease. He was quite excited to possibly have a woman in the trial, and then he asked me to help recruit other women into the trial after I had joined.
I really wanted to know why they thought this would be better than what the current treatment was. What he told me at the time was hyper-CVAD will take the disease down, but it won’t knock it out. It was unheard of to get to full remission with hyper-CVAD.

Enough people in that first 50 reached complete remission. They really thought that they could at least get you to complete remission. They didn’t know how sustainable it would be, and he was very honest with me about that.
For me, that was it. If you can’t get me there with this, but you might be able to get me there with that, I’m going to try it because that’s better. You also need to be comfortable with the fact that it’s research.
Resources
The Leukemia & Lymphoma Society has a great resource for learning about clinical trials and even has prepackaged questions you can print off and ask your doctor. The Lymphoma Research Foundation also does. Theirs is a little more specific for lymphoma because that’s what they focus on. These are great resources.
Don’t hesitate to ask questions. Everybody has questions about clinical trials. I asked so many questions that he actually took me into his office and pulled up a presentation he had just done at a scientific meeting and basically gave it to me to answer my question.

Treatment options after hyper-CVAD
He did explain that he would start with the hyper-CVAD chemotherapy. It would knock it down. We would go back to the watch and wait pattern. He was like, “I don’t know. It could come back quickly. It could come back slowly like it did before. You can have another 2 or 3 years between now and needing your next round of treatment.”
He’s like, “We could try hyper-CVAD the next time, but odds are if it grew back after we gave that to you the first time, it’s not going to work so well. We usually go to a second kind of chemotherapy the second time, and then that knocks it down. Then you go back to watching and waiting.”
At that point, it’s a game of, “Can the chemotherapy regimens keep you going long enough to have a full life?” But you’re also building up all the different treatments and toxicities, so that’s not pleasant.
Stem cell transplant was an option. He was like, “At some point after the chemotherapy, we’ll talk about the stem cell transplant.” They could harvest my own stem cells and put them back in, or it could be from somebody else. We would talk about that then.
Really, those were the choices. It was sort of this life of going through chemo, watching and waiting, going through the next treatment, watching and waiting, hoping something was sustainable or at least sustainable enough that I could make it to my 80s.
Clinical Trial
Choosing the clinical trial
Realizing it was experimental, you could not say for sure what was going to happen in my case, but there was enough data from these previous people who had participated in a trial to suggest that they could at least get me to complete remission.

We wouldn’t know how long that would last, so it might end up being a very similar cycle. When you’re starting from nothing, it feels at least like you have further to go until that next treatment than if you’re starting halfway there, for lack of better terminology.
Rituximab and ibrutinib process and side effects
The rituximab is an infusion, so I had to go in. They have to ramp you up to it. They checked me into the hospital. They started me on basically an IV slow drip of Rituxan. I had a pretty classic but pretty aggressive reaction to it at first.
It can trigger something called the rigors in you, which affects basically your whole body. It’s like you have a really bad fever and the chills that you get with a really bad fever. You’re just balled up and shaking. They clocked that right away, buried me in warm blankets and gave me something to counteract that. My husband tells me it was only like a minute or so that I was going through the rigors. It felt like half an hour to me.
Then they slowed the drip down. That first one, to get the whole dose in, took actually 2 days for me. That’s pretty unusual. They had to slow it down quite a bit. Beyond that, they then would speed it up. Eventually, it got to the point where the infusion would be like 4 hours.
I would just go in at first every 2 weeks, and then it was once a month for the Rituxan infusion. For that first month, I was only on the Rituxan. Then they added the ibrutinib. The ibrutinib was a pill, and it was just a pill that I took every day. One pill once a day.
»MORE: Targeted Therapy
Working during treatment
I could go about my life other than having to go for this infusion once a month that, like I said, did only take 4 hours most of the time. I was able to work through the whole thing. I had enough leave time that I could take days off to go get the infusion, and my company was really good about it. I would hope they would be; they’re a cancer organization.
I sort of proactively talked to HR about what it would look like if I needed to take leave, because I didn’t know how I was going to feel at all or how much I was going to need to be in and out of the hospital with this treatment. Early on, we walked through what work would look like.
I just declared this day the celebration day, and then the next day I worried about chemotherapy.
She gave me the paperwork and told me at whatever point I wanted to go that route, just to fill the paperwork out and give her a call, and she’d help me get it filed and stuff. Super supportive there. I’m probably jumping ahead, but I ended up doing intermittent family leave for the chemo portion of my treatment because I was in the hospital for a week at a time.
»MORE: Working During Cancer Treatment
Remission
Every month when I would go for my infusion, they would do blood work. At first they just did the blood work to see how I was responding. They would look at my white blood count. They would look at a few other things to see how I was responding to the test.
Then 3 months in, they did another bone marrow biopsy to check if my bone marrow was responding to these biologic drugs. My white blood count was significantly down and my spleen was down back to normal size, but my bone marrow was still showing some mantle cell lymphoma. I kept going on the biologic.
Then at 6 months, they tested again, and I had had a complete response. My white blood count was below normal now, and my bone marrow was completely clean. Nothing showed up on the scan — my spleen, no lymph nodes, no anything. I had had a complete response. They declared me in remission.
Now it was time for phase 2 of the trial, which was the chemotherapy. Because I had reached complete remission, I only needed 4 months or 2 full rounds of the chemotherapy. It could have been that or 8 or 16, depending on what your response had been to the first part. I got lucky. I only needed the short version.
I was ecstatic. I had a party when they declared me in remission, literally. I just declared this day the celebration day, and then the next day I worried about chemotherapy.
Chemotherapy
Undergoing hyper-CVAD
I knew what I was doing when I signed up for the trial, but I had maybe underestimated the significance of knowing that I didn’t have cancer in my body but still going to go through chemotherapy.
I am glad I only had 4 rounds. It was tough. It got progressively worse. The first month with the A cycle, I handled it pretty well. I had sort of my contingency plan in place, because I wasn’t sure when I got out of the hospital if I was going to feel like going to work or if I was not. I was able to work. I went back to work the very next day and mostly was fine.

The B round, I suffered more in general. It left me feeling pretty sick. Most people, it’s the other way around, but I got nailed with the B round. I still worked the whole time unless I was in the hospital. Frankly, I could have worked when I was in the hospital getting an infusion. My company didn’t want me to, so I took that time off.
For A round, I would go in 5 days pretty steadily. It’s 5 days. They sequence the drugs. They start you on 1, and then they add in the next. You’re hooked to an IV the whole 5 days.

Taking walks
You can move around. I knew the guards at the hospital, and I’d go down to the coffee shop to get a coffee and see what was going on. I could walk. My husband made me walk. He was like, “You’re not going to lie in this bed and just waste away. You’re going to get up and walk.” We mapped out a route with the crosswalks and things that was 2 miles. I walked at least 2 miles every day with my pole, who I named Fred. He was my dance partner. I was okay.
The B round, like I said, I got sicker with that one. That’s when I learned about anti-nausea drugs and all the things that they’ll give you to help with side effects. I weathered through that pretty well, too. I kind of felt like I had the flu with the B round, but I still would get up and walk and do everything I could.
»MORE: Managing Chemo Nausea
Clearing the drug from your kidneys
Then the second A round was a little bit worse. The B round was a little less predictable. It was actually 4 days of an infusion, but you had to clear 1 of the drugs out of your kidneys before they would let you go home, because it could damage your kidneys. That can take anywhere from 24 to 72 hours. It could be 5 days. It could be 6 days. It could be 7 days.
I was pretty lucky. It cleared out of my system pretty well. The first time I was in, it was 5 days, and they let me go home. I had trouble clearing it the second time, so I think it was 7 days before I could go home the second time.
Treating side effects
Zofran was my best friend. I discovered coconut oil for mouth sores. They’ll tell you baking soda, which kind of works. But if you swish coconut oil around your mouth, it takes them right away. It’s amazing.
At that point, they give you drugs. They give you the drugs, and then they give you the drugs to counter the side effects of the drugs, and then they give you the drugs to help you sleep. Just embrace it, because you need to manage what’s going on in your body, for sure.
»MORE: Cancer Treatment Side Effects
Hair loss
The hair loss was a side effect of 2 of the drugs in the A regimen. I got through my first A regimen, and then 10 days after I went home, my hair started falling out. What they didn’t tell me was it would hurt. The hair pulling on my follicles, I guess. It hurt. I actually wanted it to go away because it was not a comfortable thing.
When you’re going through this journey, you have to celebrate even some small things. You just still need to find that joy and some way to bring it out.

My husband actually shaved my head for me. I didn’t go to a hairdresser. I just had my husband shave my head. He couldn’t do it the first time. We had to try again the second night. I wasn’t bothered at all. It bothered him a lot. But we got through it. He did a great job.
Turns out I have a really good head. I did not opt for a wig. I was bald or used head wraps the whole time.
»MORE: Hair Loss and Regrowth
Henna crown
Then my “you got through chemotherapy” gift to myself was that I got a henna crown after my last round. It was something I wanted to do. I had seen them. I thought they were beautiful, and it was a celebration for me. I happened to finish chemo at the end of October, and my birthday’s in early November, so that was my celebratory gift to myself.
I have a couple of friends who did henna pretty regularly. They’re of Middle Eastern descent. I called to see if they knew anybody that would do a crown for me. They knew somebody that would do the crown for me, and they came with me. We just had this very special, meaningful night.
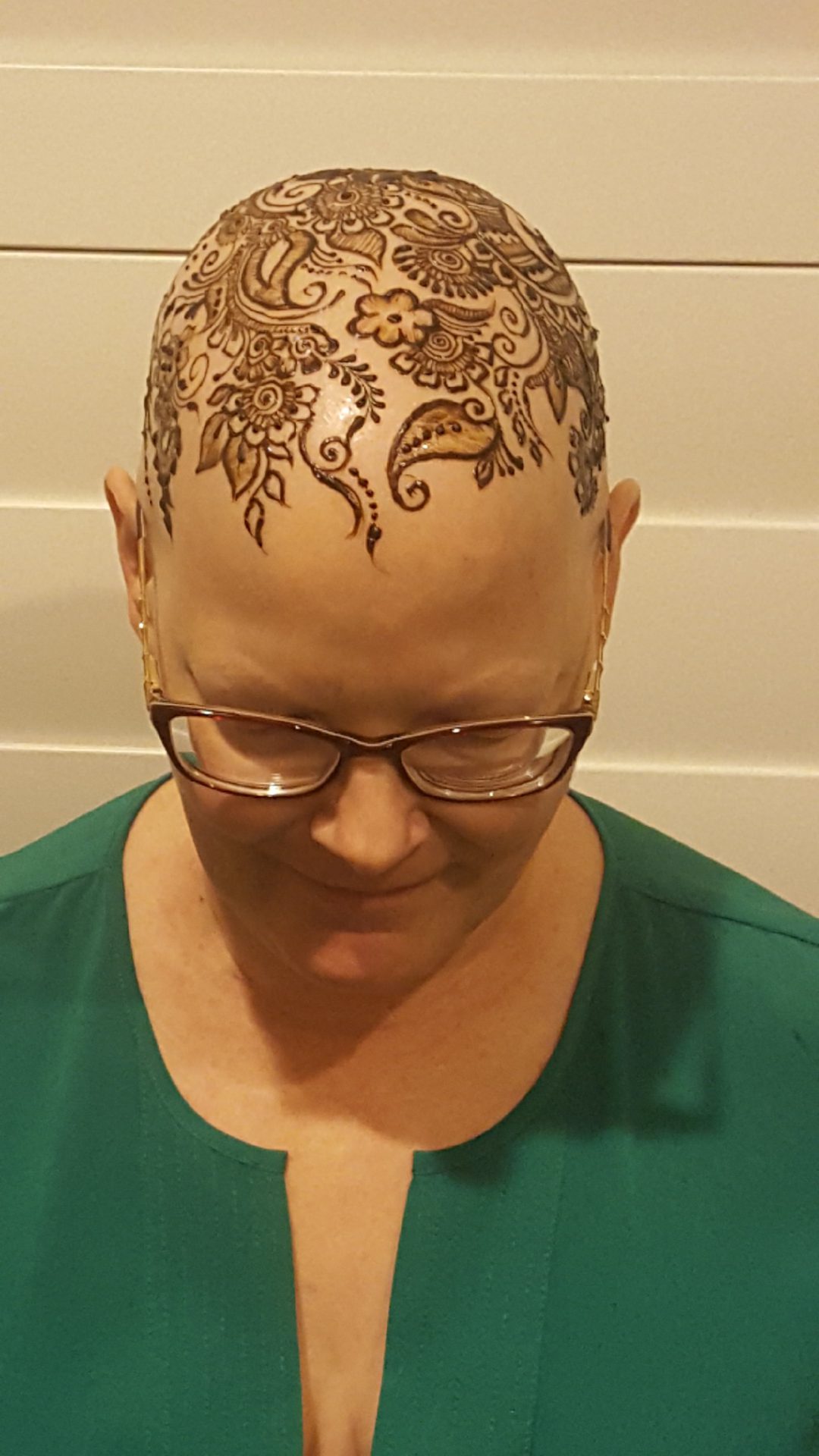


It took about an hour for the woman to do my head. I didn’t really have any specific guidance for her. I just wanted something beautiful. I showed her a couple of pictures of things I liked, and she free-handed the whole thing. Then my friends got their hands done, and we have a couple of pictures of us together afterwards.
Then my husband picked all of us up, and we got some food at a local Middle Eastern place. I walked in, and immediately they knew. They just were like, “What a beautiful crown.” I just started crying because they were celebrating with me.
Celebrating the small things
For me, it was bringing some beauty out of some tragedy. You don’t have a completely bald head all that often in life, so I might as well make the best of it. That’s my favorite thing. It really was very healing for me to do that.
People think it’s odd, but it’s one of my favorite pictures of me. There’s one I’m kind of looking down, and you can just see the head. There’s a big flower right on the crown of my head. That’s sort of the crown part of the crown, if that makes sense. For me, it just is really a sign of life. Life came out of everything I had just gone through.
I believe in celebrating things. I told you I had a party after I finished round 1, and I believe in celebrating things. When you’re going through this journey, you have to celebrate even some small things. You just still need to find that joy and some way to bring it out.
Follow-Up and Lessons Learned
Follow-up after treatment and chemotherapy
Once I completed the chemotherapy, I had to go back a month later. I went back in November just so they could check how I was recovering from the chemotherapy and how everything was going. They did another set of blood tests to make sure I was still in remission and it wasn’t boomeranging — or whatever it’s called when you stop treatment, and then it comes back. I wasn’t.

Then after that, every 3 months I would go back for blood tests and a PET-CT scan. I haven’t had to do another bone marrow biopsy since the one was clear, and I’m very grateful for that. Then I did every 3 months for a couple of years, and then they pushed it to every 6 months.
This fall I will be 5 years out, so I haven’t been since last August. I’ll go back this August, and then I will officially have completed the trial. I will still go back for tests to follow-up for another 5 years, but the trial itself will be completed, and my data will count.
What does it feel like looking back?
That was a hard year. I don’t want to in any way say that wasn’t a hard year, but I learned so much about myself. I’m very grateful for that year. It sounds a little weird to say that, but I learned about myself.
This is your life. You know what you want to do. You know what you need to do.
I learned about other people. People came and showed up in ways I never would have expected — to help and support and help me get through that, to help my husband help me get through that.
I am very grateful to be on this side of it. I’m 5 years out, and I haven’t had any signs of any kind of recurrence. I feel like I made a really good decision about joining that trial.
Dealing with scanxiety
Scanxiety is very real. I think knowing that it’s real and acknowledging that helps, but it’s still real. I’m cranky for a couple of days before a scan. I don’t necessarily always recognize it, but I’m just definitely on edge, because I’ve already gotten that bad news once. In the back of your head is, “What if it happens again?”
The way I cope with that is just, “You made it through once. If you have to do it again, you will get through it again. You can do this. It’s okay.” It doesn’t make it less hard to cope with. The days after counterbalance it because you know you’re clean. You know there’s no more sign of cancer in you. You can relax as much as you were anxious for the days before. It all balances out.
»MORE: Coping With Scanxiety
Advocacy
I hope what you heard me say is just don’t be afraid to ask questions. Don’t be afraid to advocate for yourself. This is your life. You know what you want to do. You know what you need to do. You know how you make decisions. You make sure you get what you need to do that. That’s what I believe.

Inspired by Stephanie's story?
Share your story, too!
More Mantle Cell Lymphoma Stories
Tim H., Mantle Cell Lymphoma (MCL), Stage 3/2
1st Symptoms: Lump on left-side of neck that grew bigger over a couple years, new lump on right side
Treatment: 6 cycles Nordic chemo protocol, alternating cycles of R-CHOP and rituximab + high-dose cytarabine, autologous stem cell transplant
Sheryl B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: (Over 15 years) Skin irritation from temperature changes, rising WBC levels, unexplained fatigue, retinal hemorrhage, hardened abdomen (from enlarged spleen)
Treatment: 6 cycles Hyper-CVAD chemotherapy
Shari B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: None, lymphoma discovered at unrelated doctor appointment
Treatment: 6 cycles R-CHOP, 5 cycles Phase 3 trial of Velcade + Rituxan (normally for multiple myeloma), allogeneic bone marrow transplant (BMT)
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Fatigue, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Hives, inflamed arms
Treatment: Calabrutinib, Lenalidomide, Rituxan
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Elevated white blood cell count
Treatment: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: No symptoms
Treatment: R-CHOP chemotherapy, rituximab







One reply on “Stephanie’s Stage 4 MCL Non-Hodgkin’s Lymphoma Story”
Stephanie’s story is so detailed and easy to follow. She explains the treatment, the fears, the need for some control over what’s happening when you get involved in something that can mean life or death.
I congratulate her on her remission and her dedication to research. I have shared many of her highs and lows and am so thankful for the place she’s in right now. Why? Because I’m her mother!!