Shari’s Stage 4 MCL Non-Hodgkin’s Lymphoma Story
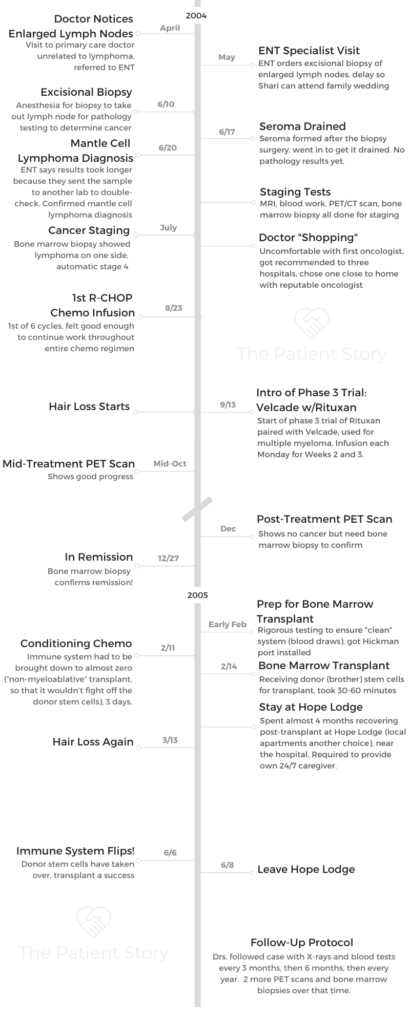
Shari shares how she was diagnosed with stage 4 mantle cell lymphoma. She went through chemo, a phase 3 clinical trial (Velcade) and an allogeneic bone marrow transplant to get into remission. Shari also highlights the importance of caring for mental health, what support helped the most and self-advocacy for patients.

- Name: Shari B.
- Diagnosis (DX):
- Mantle cell lymphoma
- 2-7% adult non-Hodgkin’s lymphoma cases
- Mantle cell lymphoma
- Age at DX: 50
- 1st Symptoms:
- Unrelated to lymphoma: doctor noticed enlarged lymph nodes at visit for laryngitis
- Treatment:
- Chemotherapy: 6 cycles of R-CHOP
- One infusion on Monday every 3 weeks
- Outpatient
- Phase 3 clinical trial: Velcade on intervening 2 Mondays
- Allogeneic bone marrow transplant:
- Donor: brother
- Chemotherapy: 6 cycles of R-CHOP
- Getting Diagnosed
- Video: Shari on Getting Diagnosed
- What were your 1st symptoms?
- How was your visit to the ENT (ear, nose, throat) specialist?
- Describe the excisional biopsy
- Did you wake up in any pain from the excisional biopsy?
- Getting the biopsy results and the diagnosis
- How did you process the cancer diagnosis?
- How did you break the news to your family and to work?
- Describe the visit with your primary care doctor
- Learning to delegate tasks to people who can handle it
- When the doctor diagnosed you, did he say, "mantle cell lymphoma"?
- Getting Staged
- Treatment Decisions
- Chemotherapy and Side Effects
- Video: Shari on Chemotherapy and Side Effects
- How was the port?
- Tip: how to help with the port injection
- Describe the chemo infusion schedule
- How were the chemo side effects overall?
- What helped with the queasiness?
- Introducing a Phase 3 trial drug into the regimen
- Any new side effects from Velcade and Rituxan?
- You believe your healthy state before the diagnosis helped
- Hair Loss
- In Remission
- Bone Marrow Transplant (BMT) or Stem Cell Transplant (SCT)
- What was the overall transplant plan?
- Why did they recommend the allogeneic bone marrow transplant instead of autologous (self-donated stem cells)?
- What was the bone marrow match process?
- How did you prep for the actual transplant?
- How was the prep for the conditioning chemo?
- You got the Hickman port
- Describe the 3-day conditioning chemo regimen pre-transplant
- An occupational therapist helped you with physical strength
- Dealing with weight fluctuations
- Describe the final steps before the transplant for your donor (brother)
- Collecting the bone marrow stem cells
- Describe the actual transplant process
- Post-Transplant Recovery
- How was recovery immediately after the bone marrow transplant?
- Describe the Hope Lodge
- What kind of support did you need during BMT recovery?
- Recovery would take months
- You lost your hair for the second time
- How long did you stay at the Hope Lodge?
- You had to go back into the hospital for a while
- It started getting better after a few weeks
- The possibility of a second transplant came up
- Undergoing regular bone marrow biopsies
- Describe the recovery back at home
- What was the follow-up protocol?
- Bonus benefit of the bone marrow transplant
- Reflections
- Video: Shari shares her post-cancer reflections
- When did you feel "back to normal" again?
- Dealing with worry over potential relapse
- How did you manage mental and emotional health through cancer treatment?
- What was the best kind of support you received?
- The importance of self-advocacy in cancer care
- What's your last message to others out there?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I’m just a positive person. A positive attitude doesn’t stop bad things from happening to you, but it stops you from obsessing over them before they happen.
Being a results- and goal-oriented person, I just needed to have that something to look forward to, something that was going to make me happy.Whatever it was. It could be going out to dinner. Who knows? But I just wouldn’t let it keep me down.
Shari B.
Getting Diagnosed
Video: Shari on Getting Diagnosed
What were your 1st symptoms?
That’s the weirdest thing. I didn’t really have anything you’d call a symptom that I recognized. I had just done this incredible bike ride — that’s my thing, I’m a cyclist — with 160 miles in 9 hours.
I was having some problems with laryngitis. It had nothing to do with the lymphoma, but that’s what made me go to the doctor to make sure I wasn’t coming down with something. For my 50th birthday next month in May 2004, my husband and I were going to the South of France to do a bike tour.
I went to the doctor to make sure I wasn’t coming down with a virus. The physician’s assistant felt my neck and said all the lymph glands around my neck felt like a string of pearls.
He said that wasn’t normal and that I’d have to get it checked out.
I said I would after I got back from my vacation because otherwise I felt fine, and I didn’t have any other symptoms. I didn’t have any pain. I wasn’t tired. Just didn’t have any real symptoms. That was all it was, was the lymph glands that I didn’t even notice.
How was your visit to the ENT (ear, nose, throat) specialist?
In mid-May, I went to Dr. Mark McClinton, an ENT and fellow cyclist. He’s feeling around and then gets to another part of my neck and goes, “Whoa!”
I knew him. He was a bike club buddy. I’m like, ‘What do you mean, “Whoa?”‘ Doctors don’t say, ‘Whoa!’ They say, ‘Oh, this is interesting,’ or ‘Oh, this needs to be checked out.’
That was a little bit freaky. He said that they had to do a biopsy, and I said it’d have to be after Memorial Day Weekend because I was going to my niece’s wedding. I was wearing a strappy dress, and I didn’t want this bandage sticking out there.
Unbeknownst to me, my sister told me later that she could see this enlarged lump from across the room. I had no idea.
Describe the excisional biopsy
For the biopsy, I was put under an anesthetic, and he actually cut some lymph glands out. He had to really slice out a group of lymph nodes. That was in a hospital under propofol.
Did you wake up in any pain from the excisional biopsy?
I don’t remember any specific pain from that excisional biopsy. About a week later, I went in because it was swelling a lot, and that’s when he had to drain a seroma. It was nothing serious.
First, what the doctor did in his office was use LMX cream, a lidocaine-cream, and put it on there for about an hour until it numbed the skin because I was freaked out. Most people would probably say, “Oh, who cares?”
I’m needle-phobic, or I was. This did help me get over it.
Getting the biopsy results and the diagnosis
Every day I didn’t get results, I figured it couldn’t be that bad because if it was something bad, they would have told me by now.
He told me at that seroma appointment he hadn’t heard anything yet, and it was 3 days after when he contacted me to go back in because they got the results. That was a very surreal experience.
He inspected and took the stitches out, then said, “Okay, let’s get to your report.”
He picks it up and said, ‘Unfortunately, it’s not good news. You have lymphoma.’
How did you process the cancer diagnosis?
Even though part of me said, “It was probably just an infection. This is all a big deal for nothing,” there was a little part of me that was worried that it might be something. My father died from lymphoma. My father’s older brother died from multiple myeloma.
Interestingly, 3 months before my diagnosis, my father’s younger brother was diagnosed with lymphoma. My grandmother, my father’s mother, had Hodgkin’s disease when she was 80.
They did tell me there was no familial link with lymphoma.
When the doctor said you have lymphoma, my first thought was my dad, who died in 1995. I thought, “How am I going to tell my mother?”
Jeff, my husband, was with me. The doctor had handed me a box of tissues. I looked at my husband, who started crying, and handed him the box of tissues, and said, “Okay. What’s next? Give me a plan of action. What do I do next?”
That was it from that point on. I just needed to know what was next. The next thing to do was to get staged and then figure out where to go from there.
I wanted to have a reaction that I could be proud of. I didn’t want to burst into tears. I didn’t want to crumple on the floor in a fetal position.
I wanted to be somebody I could be proud of. It really wasn’t a conscious thought. I just thought, ‘This is how I am.’
I am a type A+, so I just needed to move forward. I needed to know what to do next.
»MORE: Processing a cancer diagnosis

How did you break the news to your family and to work?
My mom was living up in New Jersey at the time, and I’m in Florida. From there, he told me I needed to get staged and would have to figure out whether it’s an indolent form or aggressive form. We went out the door, and Jeff is still a little bit on the numb side. He’s not saying a whole lot.
I got in the car. The first thing I did was call work since we had gone to the appointment from work. My husband and I worked together at the time. I told work I wouldn’t be in because I had just been diagnosed with lymphoma.
I couldn’t say cancer. Cancer sounded worse for some reason. They were freaking out.
Next call was to my family practice doctor. I told them I had to go in because I’d just gotten this diagnosis and I needed them to talk to my oncologist.
Then I called my sister. My whole family knew I was getting this biopsy, that I was making light of it. I called my younger sister, Judi, and told her it was lymphoma. I told her I needed her to tell Rick, my older brother, and let him know. I told her she had to go over to my mom, not call her to tell her this news.
My sister’s kind of like me. She takes it over. She’s Miss Organized. She said, “Okay, we’ll do this.” I knew I could leave it in good hands with her.
My sister and brother knew my mom was having a luncheon, so she’d be home. Around the time after her luncheon, they both went up, and I could just imagine this: as soon as she opens the door and sees them, she’s going to know.
It’s like if you have a soldier who’s overseas and you open the door. If it’s the lieutenant and the chaplain, you know what they’re going to say.
I told my husband that I was glad I was the one with lymphoma, not the one telling my mother I have lymphoma.
»MORE: Breaking the news of a diagnosis to loved ones
Describe the visit with your primary care doctor
We went over to my doctor’s, and I sat in this waiting room filled with people. I told them at the desk what I was there for. Two seconds later, he comes out and tells me to go in. People were giving me dirty looks.
He said something interesting to me. “If you’re going to have cancer, lymphoma’s probably the best one for you to get because it actually does have a pretty good cure rate.”
That made me feel better. He said whatever I did, I shouldn’t go home and look up “mantle cell lymphoma” on the computer. He knew I would want to do that. Of course, I did.
Learning to delegate tasks to people who can handle it
I am very fortunate in that I have very supporting family and very supportive friends. It’s amazing how people came out for me.
When the doctor diagnosed you, did he say, “mantle cell lymphoma”?
He said mantle cell lymphoma, and he said that the reason it took so long was that the lab was so distressed by this diagnosis that they took the sample of tissue and sent it out to another lab in California to have them test it. It was double-checked, and that’s why the biopsy results took so long.
Getting Staged
What was the plan for staging?
The next 2 months were a whirlwind. Later in June, I went to the Cleveland Clinic in Weston, FL, for staging. That included MRIs, bloodwork, PET scans and my first bone marrow biopsy.
Describe the bone marrow biopsy
My uncle had been diagnosed 3 months before me, and I had called him when I found out [about the cancer]. I said I needed to have this bone marrow biopsy done, and he said it was nothing. My uncle has a very high pain tolerance, and haircuts hurt me, so my pain tolerance, especially for needles, [was low].
The doctor was giving me what they call a bilateral, which means on both sides of my hips. It entailed me lying face down on a table that put my butt up in the air, and then they drilled down into the bone to suck out the bone marrow.
Jeff, my husband, told me it looked like raspberry jam. Now I can never eat raspberry jam ever again!

She gave me an Ativan to take an hour or so before to calm me down. I took 2 of them. You’re only supposed to take 1, and it still wasn’t doing anything. I was in a lot of pain, but that was me.
I even had Jeff in there with me. I told him to squeeze my toes, and he was squeezing my big toes, so now my big toes hurt and my hips hurt. I was not really good at this. I don’t know whether she had bad technique, but it was traumatizing.
Then you had to do the second one. She had put some Ativan under my tongue while I was there to get me to calm down. I really didn’t take until she was halfway through the second one.
Then all the Ativan I took started working at once, and I have no recollection of the rest of the day. I just remember it was really not a good experience.
Describe the MRI with contrast dye
The PET scans, the X-rays, they weren’t bad. The MRI that I had, they wanted to do one of my brain just to make sure it hadn’t gone anywhere else.
For the contrast dye, she did something wrong when she was putting the needle in, and it leached into my arm. It felt like a torch on the inside of my arm. I’m crying and blubbering like an idiot. She had to go get ice packs to put on there because it was very painful.
Needless to stay, I didn’t stay with that hospital.
It was a good thing the bone marrow was done bilaterally
The next time I saw the doctor was the follow-up, when they got the results back of this bilateral bone marrow biopsy. It might have been a week later.
It turned out to be a good thing she did a bilateral because it was so diffuse in my bone marrow. It was still early in stage 4 because the cancer was in the bone marrow. They found it on one side of my hip, and they didn’t see it in the other.
If they would have just taken that one side, it might not have been diagnosed in time [as stage 4], so that was good.
Treatment Decisions
What made you want to seek a different medical team?
When she started talking to me about my options, she was so laissez-faire about it. “You could do this, or you could do that.”
I needed a plan of action. That’s when Jeff and I went doctor shopping. I interviewed different hematologist-oncologists.
Always get a second opinion (if possible)
Something like this, regardless, you should get at least a second opinion to see what another doctor would say. She was so, “You can do this or that.” How am I supposed to make the decision? I just wouldn’t know.
Right there, I knew I needed to talk to at least one other doctor to see what they thought, if they said the same thing — that the cancer was indolent, I could wait and see, which is not my personality.
»MORE: How to be a self-advocate as a patient
What did you learn most after going “doctor shopping”?
One of my friends is a transplant surgeon in the Mayo Clinic in Jacksonville. He got me in to see the hematologist-oncologist there so I could get an evaluation. We went went there for that.
Another one of my friends who was suffering from a form of pancreatic cancer, diagnosed about 6 months before I was, was going to the Moffitt Cancer Center and said, “These people are great. You have to come here.” So we found a doctor there we could see.
He was actually conducting a trial for mantle cell lymphoma, so I thought maybe I could try to get into this Phase 2 trial.
Someone else gave me the name of another doctor in an oncology group right down the street from where I live. When I called there and they said, “What kind of cancer?” and learned it was lymphoma, they referred me to Dr. Greenberg, their lymphoma expert. Then I went to see him.
All 3 of these doctors said exactly the same thing, that I needed to have chemotherapy to put myself in remission, followed by a bone marrow transplant from, preferably, a sibling donor. That could change my immune system out, and I’d be ‘cured.’
They all said the same thing. The Mayo Clinic doctor wanted to do a much more aggressive chemotherapy regimen called hyper-CVAD, which required a hospital stay.
The doctor at Moffitt said they didn’t want me in the trial because I was young, and it was early. The trial was really for people who didn’t have options left. He said I needed to do chemotherapy: CHOP with Rituxan, followed by a bone marrow transplant.
Then I go to Dr. Greenberg, and he says the same thing. He and I just, from the moment I walked in there, started talking and hit it off. He’s like a kindly uncle. He’s my age, but he felt like a kindly uncle.
Why travel to Tampa or up to Jacksonville when I have this great guy in my backyard? It turned out he had a curriculum vitae (CV) as long as your arm. He was very impressive.
Chemotherapy and Side Effects
Video: Shari on Chemotherapy and Side Effects
How was the port?
Dr. Greenberg said I needed to get a subcutaneous, double-lumen port in. In retrospect, it wasn’t a big deal. It was just the anticipation. You get a lot of anxiety because you don’t know what to expect.
They put you under — propofol is my friend — they make an incision, they put this thing in there, and they attach it to a central vein. Then they sew the skin back over it.
It was covered, which is protected from germs. That’s the biggest part about that is if you get an infection in your port, especially if you’re immune compromised.
That was protective, and then it didn’t take very long for that to heal up. That was nothing when it came down to it. But it was the anxiety that was worse than what actually happened.
When I went in to get my chemo, they came into this little room in hazmat gear and mix this stuff up in front of you. They usually put in an antiemetic so you don’t get sick.
They also give you stuff for allergies in case you have an allergic reaction, which makes you fall asleep. I usually fell asleep through quite a bit of my treatment.
Tip: how to help with the port injection
I would put that LMX cream on there and covered it with saran wrap an hour before I’d get the infusion, so when they did puncture my port, it felt like nothing. It just felt like somebody touching my skin. That was good.
Describe the chemo infusion schedule
They sat me down in this comfortable chair, and I lay back with a book, fell asleep, and 8 hours later, it was done. My treatments themselves were about 6 hours. I was going every third Monday for that.
How were the chemo side effects overall?
It wasn’t as bad as I had expected actually.
I’d heard all these horror stories about people throwing up and losing tons of weight, which was actually something like, “Yay, a weight loss program!”

But it actually didn’t affect me quite like that. Of course, it’s scary as shit. I was really nervous going in the first time. After the first Monday and within that next 3 weeks, I did feel a little nauseated. Nothing really bad.
I went to work the next day on Tuesday and the rest of the week. I was fine. By the end of the week, I was really tired and a little on the queasy side.
What helped with the queasiness?
Somebody told me to get some fresh ginger root, peel it, take an inch-long piece and steep it in hot water with a little bit of honey. It helped my queasiness. That was only for that first cycle.
»MORE: Cancer patients share their treatment side effects
Introducing a Phase 3 trial drug into the regimen
The next treatment, which was 3 weeks later, Dr. Greenberg came in and said there was a Phase 3 trial of adding Velcade to Rituxan, that monoclonal antibody.
Velcade has been very effective for multiple myeloma, and there are some similarities between multiple myeloma and mantle cell lymphoma, so they wanted to see if it would help.
On the intervening 2 Mondays, I went in for 4 hours. I’d get an infusion of Rituxan and Velcade. They had an infusion for the Rituxan and then injected the Velcade into the line, and that was it. That was usually just a 4-hour thing.
I’d go in the morning, then went home, had some lunch, then went to work. Overall, Monday I’d have R-CHOP, then the next 2 Mondays I’d have Rituxan with Velcade, and then the R-CHOP again all over again (for 6 cycles).
Any new side effects from Velcade and Rituxan?
No. I went to work everyday except for the all-day chemo. For R-CHOP, I was there for close to 8 hours each time. Then I’d go home and take a nap. That Benadryl just made me sleepy.
I really didn’t have any other effects. On the weekends, I went biking with my bike club. I didn’t know any different, so I just did what I felt like I could do.
You believe your healthy state before the diagnosis helped
I think what helped is the fact that I was extremely healthy and fit before this happened. I rode 160 miles! I think the fact I was relatively young — 50 might not seem young to some people, but to me it was — and healthy. I really think that helped.
Just as an aside, at the time I had my cancer diagnosis, there were 4 other people in my bike club all diagnosed with different types of cancer. One had breast cancer, one had thyroid cancer, another had colon cancer. Every one of them survived.
They all got through it. Everybody was generally young and healthy. I think that really helps, if you can stay healthy before you get it.
Hair Loss
Describe the hair loss
It really was the least of my worries. I really couldn’t care. I had great, beautiful, thick brown hair. I still don’t dye my hair. It never really changed. I loved my hair.
When I would start to wake up in the morning and there’d be this angora cat lying on my pillow, I’d be like, “Ugh, darn it.” I said, “Enough of this. I can’t stand this mess.”
How did you prepare for shaving your head?
There was a place not far from where I live that had a wig shop that catered to people going through chemo. They have a very private booth. Shave your head, and you pick out a wig.
I picked out 2 wigs, an everyday wig and a Sunday meeting wig. It was fun. The truth is, it really didn’t bother me. I didn’t really wear the wig unless I was at work or when I was going out.
Usually around the house I was bald, and I really didn’t care. The best side effect of this whole thing was I didn’t have to shave my legs for 2 years. It was awesome! I saved a lot on shampoos and razors.
»MORE: Dealing with hair loss during cancer treatment
Was there any emotional impact on you?
It really didn’t bother me. The last thing I wanted anybody to do was to shave their heads in solidarity. Why would you do that?
If that makes somebody feel good, great for them. I think it’s awesome. But I just didn’t want anybody to do that because I didn’t feel that bad about it.
In Remission
Did you have scanxiety during your treatment scans?
I just wanted to find out. I like information because knowledge is power, so it was, “Let’s see what happens.”
The PET scans were great. Halfway through, there was no new growth. The PET scan is really interesting in that you fast, then they give you an injection of basically sugar water. Wherever there’s growth, where the cancer is, it’s going to shine like a beacon.
There was nothing remarkable. The only growth that they actually saw was where the biopsy was done. There was healing going on, so there was new growth, but from the healing.
I just wanted to know. Once I knew, I could move forward regardless of what the answer was.
»MORE: Dealing with scanxiety and waiting for results
One complication during treatment
Only one setback occurred. On Election Day (November 2, 2004), I came down with an unexplained fever and spent 3 days in the hospital.
It never got worse, and it cleared up without any of the doctors knowing what happened. I completed the rest of chemo, which included shots of Leukine after each treatment to bring up my white count, without further issues.

How did you know you were in complete remission?
This aggressive approach paid off. After my last treatment, on December 27, 2004, a bone marrow biopsy showed that I was in complete remission. Yay, me!
How did you process the news of remission?
I celebrated, but we’d already started making the plans to go to Moffitt Cancer Center [for the transplant]. Halfway through, Dr. Greenberg and I talked about this. He wanted me to go to the Fred Hutchinson Center, which is out in Seattle, and it was supposed to be the Mecca for bone marrow transplantation.
I said I contacted Moffitt Cancer Center, and they put me in with this Dr. Anasetti. Dr. Greenberg goes, “Dr. Claudio Anasetti?!” I said yes. He said he studied under him at Fred Hutchinson, didn’t know he moved to Moffitt and to go with him.
That made me feel really good. Dr. Greenberg said Dr. Anasetti is a rockstar (he’s retired now). He was another guy who adored that man. He was just wonderful.
We’d already had that plan started. When I had the bone marrow biopsy that showed I was in remission, all the results were sent to Dr. Anasetti. The ball started rolling for that.
Bone Marrow Transplant (BMT) or Stem Cell Transplant (SCT)
What was the overall transplant plan?
They told me mantle cell lymphoma has a 90% relapse rate with just chemotherapy, but it’s a 5% relapse rate with a bone marrow transplant.
Why did they recommend the allogeneic bone marrow transplant instead of autologous (self-donated stem cells)?
You can do autologous. Right after my diagnosis, a guy I worked with, his girlfriend’s sister was diagnosed with mantle cell lymphoma at age 50.
She didn’t have a matching donor, so she did get the autologous transplant. They radiated her whole body, killed everything off, and then she got that and was doing fine more than 5 years later.
I was told the first choice is an allogeneic bone marrow transplant with a sibling donor.
What was the bone marrow match process?
First thing is they had these HLA blood tests. Human leukocyte antigen. It was actually better to go with my older brother. Even if my sister matched, every child that you have — my sister had 3 kids — changes the HLA slightly.
Even if we were kind of close, her 3 children would have moved us further apart, so it would have been a more difficult transition.
My sister didn’t match anyway, and my brother did. Stars shone upon me there again.
He was perfectly willing. I have heard of people whose family member did not want to do it, which boggles my mind. I can’t imagine that.
My sister-in-law said my brother would crawl across broken glass on his bare chest for me, for his little sister, which produced no small amount of bawling from yours truly.
How did you prep for the actual transplant?
The nurses — saints, every one of them — took 14 vials of blood, which they checked for any type of disease, parasite, virus and bacteria known to man. They check for every single thing that you could possibly have in your body.
Any virus, parasite, bacteria, anything. You had to be completely free of any of that, so I had to go through that.
How was the prep for the conditioning chemo?
On a Monday, I went into the hospital. They did all these blood tests in a room in the transplant wing. Then they started infusing me.
You got the Hickman port
I was outfitted with what’s called a Hickman port, an external port inserted directly into my central vein. I called it my teat.
It sticks out of your skin, which is great because you don’t ever have to be poked anymore.
They just put everything through the lumens. Mine was a 3-lumen Hickman port.
Describe the 3-day conditioning chemo regimen pre-transplant
They gave a 3-day course of “conditioning” chemo to get my system ready for transplantation.
My immune system had to be brought down to almost zero. It’s what’s called a “non-myeloablative” transplant, so that it wouldn’t fight off the donor stem cells. This was really awful.
This was the beginning to middle of February. To give you an idea, on the Sunday before I started this process, I rode 40 miles with my bike club at 18 to 20 miles per hour, having recovered from the CHOP chemo between the end of December and beginning of February.
By that night, I thought, “Okay, get that number of the truck that hit me.” I just remember being halfway there.
I had to have these infusions for 12 hours. They had to give me a lot of water. They called it “bladder Teflon.” It’s some kind of chemical that kept this really caustic chemo from destroying the bladder. It was pretty nasty.
An occupational therapist helped you with physical strength
Two days after the first round of conditioning chemo, an occupational therapist came to my hospital room to help me bend my arms and straighten my legs a few times.
The therapist helped me from literally sitting in a chair, straighten one leg, put it down, straighten the other leg, put it down, take my arm and go like this, then put it down, the other arm goes like this, put it down.
Then I needed to rest. That was effort. I even said to the occupational therapist that I had done a 40-mile bike ride just 3 days before.
Dealing with weight fluctuations
You see how round my face was? That was a lot of prednisone (steroids) in there, so I had moon face. I went from about 170 pounds when I got to the hospital, and the chemo never helped me lose weight. I never lost my appetite.
But with all the water and the prednisone, all the stuff they infused in me, my head actually looked like a basketball. My brother almost fell over when he saw me.
I went up to about 184 pounds for about a week. It was very uncomfortable. Finally, all the fluids started draining out of me, and I’d get back down a little bit.
Describe the final steps before the transplant for your donor (brother)
My brother had to make sure he was completely free of any disease as well before the donation.
We made arrangements for my transplant journey to start in early to mid-February. My brother flew down from New Jersey to begin his conditioning, receiving 5 days of shots to increase the level of bone marrow stem cells in his bloodstream.
It was the Neupogen shot, which was very interesting. I was supposed to get Neupogen, too. It’s supposed to raise your white blood cell count. When you get R-CHOP, it can deplete your white count.
Turned out I was allergic to the Neupogen and went into anaphylaxis. Jeff had to rush me to the hospital after the second time I got a shot of that. They gave me Leukine for that.
My brother was not allergic to it, so he got the Neupogen shots. What it does is increase the number of stem cells in the bloodstream. He was in a lot of achy pain. He never uttered one word of complaint to me. Never said a word.
Collecting the bone marrow stem cells
They gave him enough of this to really increase the bone marrow stem cell production. Then he went through 7 hours of an apheresis blood donation.
They basically put a needle in each arm, and over the course of 7 hours, they took the blood out, centrifuged out what they needed in terms of the stem cells, and put the rest of it back in.
It kept going through his system, and they’d siphon off these bone marrow stem cells. When they had enough, they put it in a bag, and that’s what they would use to transfuse me.
Describe the actual transplant process
On February 14, 2005, I received my sainted brother’s bone marrow stem cells.
It was basically like a blood transfusion. They attached the bag of good stuff to my Hickman port and infused it into me. I didn’t feel a thing.
My mom, my brother, my sister-in-law and my aunt were all there to support me. The nurses come in to infuse me. It basically looks like a blood transfusion. It’s a blood bag they hang on a hook and then connected it to my Hickman port underneath my shirt.
We’re sitting there watching this red stuff going down the line, then it gets underneath the shirt, and me being the silly person that I am, I just started going, “Pbltttt!”
My brother cracked up. He knew I was joking. My mother and the nurse were gasping. I couldn’t keep a straight face, and I started laughing! My mother threatened to kill me. That’s my mom and me. She has a sense of humor.
Overall, it took them maybe half an hour. It felt like nothing. I had no sensation whatsoever from this infusion.
Post-Transplant Recovery
How was recovery immediately after the bone marrow transplant?
I didn’t go home. I was at the hospital for about 10 days before they moved me into the Hope Lodge.
Things were starting to happen about 3 days after the transplant. I wasn’t feeling well, feeling rundown, odd, a little worried about hurting myself.
They gave me a little foam toothbrush to brush my teeth with because you have to keep your mouth clean, but you couldn’t damage any tissue. It was very strange.
I tried to be human every day — take a shower, wash my hair — but it was tiring.
I needed a chair in the shower to sit down. It was a pretty debilitating 10 days. I felt better once I got to the Hope Lodge. I had a lot of ups and downs. It was quite the roller coaster for a few months.
They kept me there for a week to 10 days. It’s shorter now since over the course of these years, they’ve modified the plan. They know what works and doesn’t work.
Describe the Hope Lodge
We opted to stay at the Hope Lodge, which is right on the grounds of Moffitt Cancer Center. It’s a free facility that is maintained by the American Cancer Society, which I’ve donated a lot of money to because it was wonderful. I would love everybody to have that opportunity.
Some people did go to local apartments that were set aside for that. I felt more comfortable in this more pristine environment. It’s a separate floor with a very specific air filtration system. They have a special kitchen facility.
I wanted to be there, and it was also very close to the hospital where all my tests were taken in case I needed to go.
What kind of support did you need during BMT recovery?
I was required to provide my own 24/7 caregiver staff. I was so fortunate to have a wonderful support system.
My mother, 77 years old and not in the best of health herself, suffering from COPD, put her life on hold to stay with me for 2 to 3 weeks at a time.
Then my husband, Jeff, would take a week off work to take care of me. Then my sister, Judi, would fly down from New Jersey for a week’s stay, and repeat. The third time Judi, my sister, was supposed to come, she was sick with strep throat and unable to be there. A bike club buddy, Heather, offered to take her place.
It was so amazing to have these people around me. More tears of gratitude.
Recovery would take months
The next 4 months were a series of ups and downs. Many, many downs.
My brother and I used to fight a lot when we were kids, like brothers and sisters often do. Sometimes, I won. This time, though, we were fighting on a cellular level. He needed to win in order for his immune system to replace mine.
The daily, then weekly, blood tests showed things going well. I had MUGA scans and breathing tests. I probably gave 3 gallons of blood overall.
You lost your hair for the second time
My hair had started growing back even while I was still getting the CHOP treatments, but the conditioning chemo caused a reversal of that within days. I had my head shaved again. I didn’t care.
How long did you stay at the Hope Lodge?
They told me it was going to be a minimum of 100 days. Me being me, I’m thinking, “I’ll be out in 90!”
I was so very wrong.
You had to go back into the hospital for a while
By the end of February, I was feeling a little better. Then into March, I took a really bad turn.
I’m throwing up; I can’t keep down water. My mom said to go back to the hospital, which is another reason it was so good to be right there. She called up the nurses, saying I was throwing up and couldn’t keep my meds down.
I had 30 medications a day, something like that. I had one of those pill boxes that have 3 things, and then I had an extra one. It was amazing how many pills I was taking, but I couldn’t keep anything down.
Back into the hospital I went. It was my mom’s turn again when I had this downturn back in the hospital for 3 days. I don’t remember much of anything, except lying there saying, “If I died, I guess it really wouldn’t be that big of a deal.” That was the lowest I’d been. That doesn’t last long for me. Then I went, “Okay, that’s really stupid.”
I started thinking about all the things that I wanted. I couldn’t leave my dogs. I had 4 dogs at home, so I thought I had to get home to them.
It started getting better after a few weeks
By the end of March, I started feeling better. Into April, I felt really good. I felt good enough to have Jeff, when he was coming that next time, bring our bicycles because I had to ride.
We did a little ride around the University of South Florida campus across the street. A couple days later, he took me to a park. Just being outside in the sunshine and the fresh air rejuvenated me.
The possibility of a second transplant came up
Then in the beginning of May, things took a bad turn again. The doctor said my new system wasn’t “flipping.” Some of the numbers weren’t good.
On May 5, 2005 (worst birthday ever for my 51st), I had another bone marrow biopsy. It was my eighth bone marrow biopsy.
It appeared that my immune system wasn’t “flipping.” That means Rich’s stem cells weren’t taking over.
Of all the times to best my brother!
Dr. Anasetti suggested I ask my brother if he would be willing to donate more stem cells if needed. My brother, Rich, did not hesitate for a nanosecond. He was ready whenever it was needed (more tears).
We monitored my condition daily over the next few weeks. My doctor was right on top of everything, adjusting medications I was taking.
All of a sudden, he asked me if I was ready to go home. My immune system had flipped literally overnight!
The day before, I was ready to call my brother to come in. Dr. Anasetti said it had just changed. They did a blood test, and all these numbers showed my system had flipped. My brother’s cells had taken over.
Undergoing regular bone marrow biopsies
They did another bone marrow biopsy to make sure the cancer wasn’t coming back and that everything was still clear. That’s what they had to do.
Describe the recovery back at home
My mom was with me then, and the next week she drove me home to her house. I would be immunocompromised for several months and needed a very pristine environment.
With 4 dogs at home and a husband who’s not exactly the Felix Unger type, it took a while for Jeff to ready our house with extra cleaning and disinfecting.
I recuperated slowly between mid-June and late July. My first task, the day after I got home, was to get on my bike. It took me 5 minutes to pump the tires, but I got out and rode 6 miles. The next day I rode 7 miles. Two days later, I rode 10 miles.
That alone was therapeutic. I also needed to get my mind working again. By the end of July, I was working from home, but Dr. Anasetti and Dr. Greenberg would not clear me to be around large groups of people until my immune system was healthy enough.
I was finally able to go back to work in person in October. It was exhilarating!
What was the follow-up protocol?
I had just one PET scan and one MUGA scan toward the end of my stay at the hospital. I then had one more PET scan after.
Drs. Anasetti and Greenberg followed my case with X-rays and blood tests every 3 months, then 6 months, then every year. I had 2 more PET scans and bone marrow biopsies over that time.
By the end of 5 years, Dr. Anasetti said I was the best result he had ever seen in a transplant patient to date. I did not need to come back unless it was a social call.
Bonus benefit of the bone marrow transplant
Interestingly, the stem cell transplant not only cured my cancer, but it cured me of allergies and asthma as well.
I’m now healthier than I was before the lymphoma. At 66, I’m still riding 30 to 50 miles 3 days a week and exercising for at least an hour almost daily. I don’t see me stopping any time soon.
Reflections
Video: Shari shares her post-cancer reflections
When did you feel “back to normal” again?
We were doing bicycle touring again on these 10-day tours. I really enjoyed life again. My doctors could see it.
But my biggest goal was to ride with my bike club before the end of the year. I rode a little bit further and a little bit faster every time I got on my bike.
Finally, on December 31, 2005, I rode 40 miles with the 18- to 20-miles-per-hour group. I was back. I had kicked mantle cell lymphoma’s ass.
Dealing with worry over potential relapse
I just wanted to get back to who I was. I will say there were times for the first few years when I’d worry about the cancer coming back. It’s always sort of back there.
By the end of the third or fourth year, I stopped thinking about it. I knew I’d beat it. I just wanted to be back to what I was before. I didn’t want to be better, more enlightened or preach to anyone. I just wanted to be me again.
How did you manage mental and emotional health through cancer treatment?
I’m just a positive person. A positive attitude doesn’t stop bad things from happening to you, but it stops you from obsessing over them before they happen.
Being a results- and goal-oriented person, I just needed to have that something to look forward to, something that was going to make me happy, whatever it was. It could be going out to dinner. Who knows? But I just wouldn’t let it keep me down.
It surprised me, too, because my sister told me I wouldn’t believe how much they’d cried. I was surprised, like, “You didn’t have cancer. I didn’t cry!”
I only cried once when I got the diagnosis. I got home and looked it up on the computer, just like my doctor told me not to. It wasn’t good. But then I sat back and thought that wasn’t me. I’m not the person they’re talking about in the studies. I’m me. I was not going to let that happen.
It’s just the way I am. I just don’t let bad things stick in my head. Because my basic nature is to be upbeat and happy and positive, I could go, “Oh, this really sucks! It’s going to ruin things.” Then it’d be like, “Okay, now let’s just move on.”
I can totally get how other people have different experiences. It’s frightening. The fact that my father died from lymphoma should have made me more concerned, but it just made me more determined not to die because I just couldn’t do that to my mother.
I could not let her lose another person to this.
My uncle, who was also diagnosed with lymphoma, lived to be 80. He survived 10 years. He just kept going and going. He also was very positive, didn’t let anything stop him, enjoyed his kids and grandkids. That was the environment I lived in.

What was the best kind of support you received?
It’s kind of a joint thing. It was Jeff. Of course, my husband was wonderful. He took care of things that had to be taken care of. I had less worry that way.
Another aspect of healing was the outpouring of love and support from my friends and family. It was my friends and my bike club, who are like my family. We still keep in touch, even though they’re in South Florida and I’m in Central Florida.
Several people came to visit me. I got cards and letters from people all over the world after a recumbent biking buddy posted a story about me on his blog.
My work family was wonderful. One day a giant box arrived for me. In it were these little gifts and cards from dozens of coworkers. I burst into tears and cried all day with joy.
The power of love is really remarkable.
I swear sometimes I think that cured me. It was amazing. It was just the whole of it. It’s how people come out of the woodwork — you didn’t even know noticed you — were there for you and giving you encouragement. I think that really helps a lot.
My mom was the most amazing person. She was 77. She had a wonderful life in her retirement community where she lived in Coconut Creek. She was on oxygen for COPD, so she wasn’t really well.
She really put her life on hold for me. It was really invaluable. She lived to be 87 years old. She did all right, even with all the struggles she had. She was pretty cool.
Support is really important. My heart goes out to people who may not have that support. Maybe they’re an only child, or they’re estranged for whatever reason.
If you get in this situation and you are estranged from your family, bury it and reach out. Give them a chance to say, “Okay, yeah, it doesn’t matter who was wrong or right. We’re family.”
If you have close friends, they can be family, too. I had that as well.
The importance of self-advocacy in cancer care
I think people don’t want to insult the doctor by going somewhere else. If it’s a good doctor, they will tell you to talk to somebody else and other people. It’s not about them; it’s about you, the patient.
If a doctor is like, “If you don’t like my methods…” then that’s definitely a doctor I would not want. Their ego is more important than their patients’ health, in my opinion.
Don’t be afraid to say, “I’m going to talk to somebody else.” You just never know if somebody is going to have a different idea and have a reason why. I think that form of self-advocacy is really crucial.
It also makes you feel like you have some power, some control. It’s an out-of-control situation to be diagnosed with cancer, so having something you can control, see another doctor, that gave me a feeling that I can do something.
This is something I have the power to do. I hate the word “empowered.” I feel it’s overused, but it makes me feel like I have something that I can do for myself.
»MORE: How to be a self-advocate as a patient

What’s your last message to others out there?
It was out in beautiful horse country. Weather was gorgeous. We rode past farm after farm of animals. Get outside. Listen to nature. Take a hike in the woods. A walk on the beach.
Even if you go by yourself, just listen to the sounds of the world around you. The ocean, the birds, crickets. I can’t speak to anybody else. I’m a bit of a nature girl, but just that is a meditative experience for me. I don’t meditate. That’s as close as I get, being out in nature.
It’s rejuvenating for me, and I can’t see it not being that way for other people. If you’ve not tried that, try it. Find a little walk in the woods, and it just makes you feel better.

Inspired by Shari's story?
Share your story, too!
Mantle Cell Lymphoma (MCL) Stories
Tim H., Mantle Cell Lymphoma (MCL), Stage 3/2
1st Symptoms: Lump on left-side of neck that grew bigger over a couple years, new lump on right side
Treatment: 6 cycles Nordic chemo protocol, alternating cycles of R-CHOP and rituximab + high-dose cytarabine, autologous stem cell transplant
Sheryl B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: (Over 15 years) Skin irritation from temperature changes, rising WBC levels, unexplained fatigue, retinal hemorrhage, hardened abdomen (from enlarged spleen)
Treatment: 6 cycles Hyper-CVAD chemotherapy
Shari B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: None, lymphoma discovered at unrelated doctor appointment
Treatment: 6 cycles R-CHOP, 5 cycles Phase 3 trial of Velcade + Rituxan (normally for multiple myeloma), allogeneic bone marrow transplant (BMT)
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Fatigue, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Hives, inflamed arms
Treatment: Calabrutinib, Lenalidomide, Rituxan
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Elevated white blood cell count
Treatment: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: No symptoms
Treatment: R-CHOP chemotherapy, rituximab





