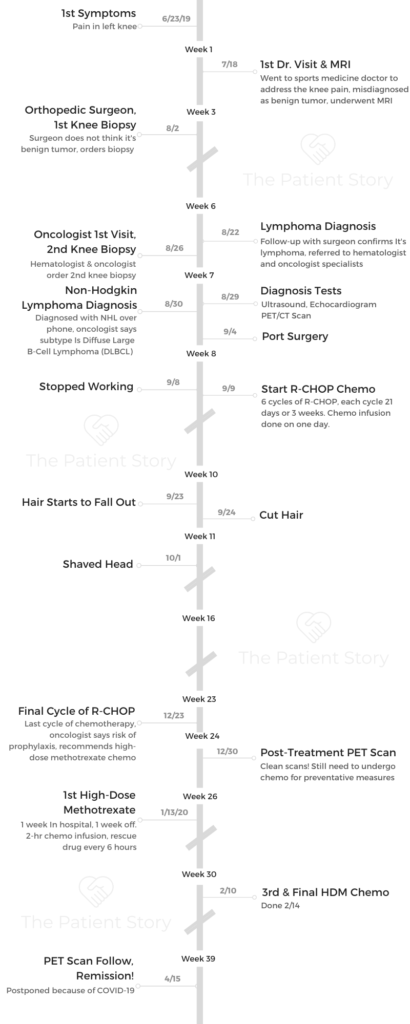
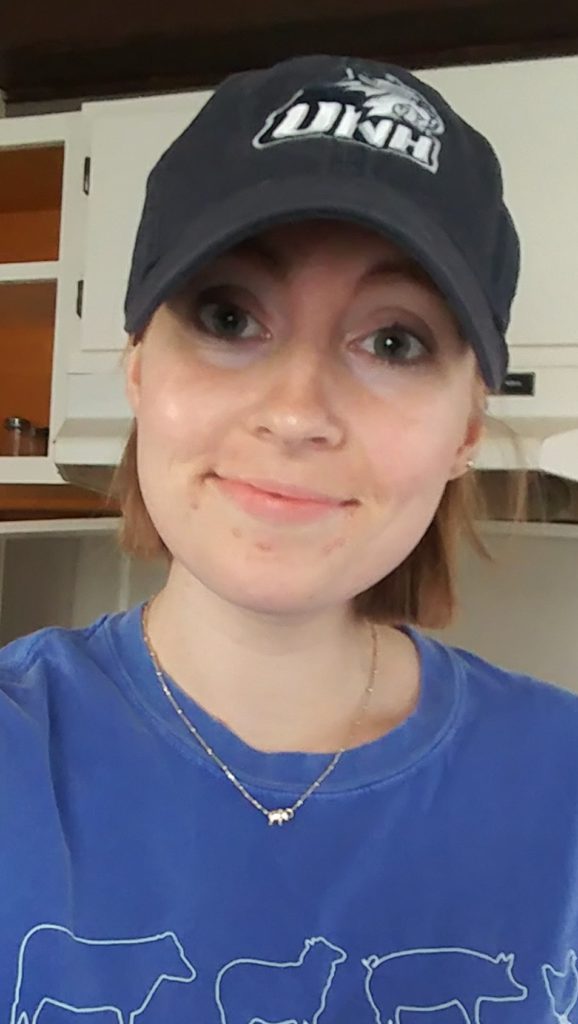
Emily’s Stage 4 DLBCL Non-Hodgkin’s Lymphoma
Emily was diagnosed with stage 4 diffuse large B-cell lymphoma (DLBCL), a subtype of non-Hodgkin’s lymphoma.
She describes undergoing chemo, being an AYA (adolescent young adult) cancer patient, how to ask for help and the support that made the most impact. Thanks for sharing your story, Emily!

- Name: Emily G.
- 1st Symptoms:
- Pain in left knee
- Diagnosis (DX):
- Non-Hodgkin’s lymphoma
- Diffuse large B-cell lymphoma (DLBCL)
- Staging: 4
- Path to DX:
- MRI
- Ultrasound, echocardiogram, PET/CT
- Knee biopsy
- Treatment:
- Chemotherapy
- R-CHOP
- Outpatient
- 6 cycles
- R-CHOP
- High-Dose Methotrexate
- Inpatient
- 3 cycles
- Chemotherapy
- Side Effects:
- Nausea
- Headaches
- Mouth sores
- Unable to sleep much
- “Chemo brain”
- Loss of appetite
- Neuropathy in fingers
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Chemotherapy is a full-time job, so you shouldn’t feel guilty for not doing anything because your body is working really hard to fight off cancer.
You’ll get through it. Just accept the help from those around you
Emily G.
First Symptoms, First Steps
What were the first symptoms?
I had knee pain in my left knee, and I was already in physical therapy because I had just run a half marathon. After that, I had hip pain. I was in physical therapy for the hip pain, and that was resolved. But then one day I had excruciating knee pain.
It spiraled from there. They got me an MRI and did blood work. MRI came back that I had a tumor. He thought it was a giant cell tumor, which I was told was benign, but they sent me to an orthopedic specialist in Boston. He did not think it was a giant cell tumor. He ordered a biopsy.
A month went by, and it came back that it was lymphoma.
Describe the biopsy
It was a needle biopsy on my left knee. It was local anesthesia. They marked my knee, numbed the area, and I was out of it. It wasn’t bad, the first one. I was fine.
They did make me sit there for 2 hours afterwards before they let me go. They just wanted to make sure the drugs had cleared my system. My friend was with me because they don’t let you drive.
When did the biopsy results come back?
I knew it would be a couple weeks. I think while I was there, they scheduled me a follow-up appointment, which was 3 weeks out.
Dealing with the wait for test results
First, I thought this was a benign tumor. Then when I saw the orthopedic surgeon, he told me it could be a couple of things. One of them was lymphoma.
I didn’t research anything. I didn’t want to jump the gun. Part of me in the back of my mind thought maybe it was cancer, but I had no other symptoms and I didn’t want to freak myself out. I just worked as much as I could and didn’t read into anything.

Lymphoma Diagnosis
Describe the first lymphoma diagnosis
My mom was with me. She wasn’t with me the first few [appointments], but I figured if this is going to be something, she should be with me. That way she can hear it; I don’t have to relay everything. We both had a suspicion it was lymphoma, so it wasn’t a shock.
The doctor confirmed it was lymphoma. He did say, “If you’re going to have cancer, this is one of the better ones.” Trying to put a positive spin on it, I guess.
I didn’t have a ton of questions. My mom didn’t either. We didn’t know what to expect. He said we would schedule a repeat biopsy to confirm and get me into hematology/oncology, that I’d need a PET scan. I just went from there.
That was really it on his end. The following Monday, they got me in for a PET scan, and I met with hematology/oncology. We learned a lot more from them.
Describe the PET scan
You can’t eat carbohydrates beforehand. They tell you that the dinner before you can only eat fats or meat. I’m a vegetarian, so I don’t eat meat. You go in, and they test your blood sugar to make sure it’s not too high. Then they inject you with this sugar isotope.
You don’t feel anything. You sit with that for about 45 minutes. Then they take you into the scanner, and you lay there for about a half hour. They wrap you up like a burrito!
PET scan results
The PET scan was the Monday before. It was interesting because the same friend drove me to the biopsy. We were on our way back. We stopped for lunch, and I got a call from my oncologist. She said there was something on my kidney that came up on the PET scan and they wanted to investigate that.
I was a mess because I was just in Boston. I get my treatment in Boston and live in New Hampshire, so it’s an hour-and-a-half one way.

Describe the ultrasound
The following day, I went back down to Boston. They checked out my kidneys, but it was just a cyst. That was a frustrating moment. I remember calling my mom and saying, “What if it’s something more?” But it wasn’t.
How long did it take to get scan results?
The PET scan I did on Monday, the day I met with the oncologist. I had that in the morning, and in the afternoon I met with them. I don’t think they read it the same way someone else would read it, but it was the same day I got the results. The ultrasound was also same-day results.
Describe the 2nd biopsy
They did the first biopsy, and the diagnosis was lymphoma. They wanted to be sure, so after I met with hematology/oncology, they wanted to get me in for a repeat biopsy.
It was the same exact thing. This one was more painful afterwards. They had to make sure they got enough. They just gave me Tylenol. I was still a little out of it.
What was the diagnosis and stage?
It was primary bone lymphoma, then went to diffuse large B-cell lymphoma (DLBCL). After I had my first treatment, it was stage 4 non-Hodgkin’s lymphoma, and that was kind of a shock. It was in both knees, my tibia and my arm.

How did you process the diagnosis and tell loved ones?
I spent a really long time in denial about it. I found out the 22nd, and I was still working. I did have to take a couple days off, but I tried to keep it quiet. Then I had to tell my boss I have lymphoma, and I needed to be done on September 8th.
I started treatments September 9th. I wanted to work as much as possible through that. I just went in and knew this was what I had to do. I really didn’t want to go through it, but I knew it would be okay.
I told my boss and one friend at work. Other than that, nobody knew. I knew it would come out after I left. That didn’t bother me. I just think I was in denial for so long that I didn’t want to tell anyone.
My mom was the one to tell all my family. I told my sister. She called me, and I’m like, “Do I want to tell her?” I did tell her.
I’m someone who really doesn’t want anyone to worry about me. I’m very much a quiet person. I think I just wanted [my mom] to be like, “Yeah, she’s fine.” I really didn’t tell a whole lot of people. Just my immediate family knew.
Eventually, I knew I had to tell my closest friends. Obviously my friend who took me to my procedures, I told him. My cousin knew from family.
I really didn’t want to text my best friend from home, but I wanted her to know. I just put it out there: “This is what’s going on, but I’ll be fine.”
It wasn’t that I didn’t want other people to know. I just didn’t want to talk about it.
How to emotionally process the diagnosis
I feel I processed it how I needed to. I just kept my head held high. I knew I would get through it. Obviously, I didn’t want to, but I knew I’d be okay. My doctors told me you have a favorable outcome, so I never feared for my life. I don’t know why. I think it’s how my doctors handled it. I was grateful in that aspect.
After the first 2 treatments, there were days I was like, “Okay, I feel fine. People can live with cancer.” It was so hard because I had to quit my job, and I really didn’t do anything. It was still hard to just be at home doing nothing. I dealt with it in pieces emotionally.
Some days I was totally fine about it. Other days I let myself feel the emotion.
Port Placement
Port surgery
It was nice because I met with one nurse prior, the day I had the ultrasound. She gave me a ton of information that was really helpful. She showed me what the port was.
They told me I was getting it because you can’t get chemo through your veins. She showed me what it was, and that was cool to see. I went in for the port, and the same friend drove me.
I was really anxious about it because it was final. There’s no turning back; you’re getting chemo after this.
It was local anesthesia. I don’t really remember anything. I remember at some point, not that I could feel it, but it was almost painful.
I’m almost positive I cried the entire time. I was out of it, and it didn’t take that long. It was only a little sore the day after, and then it was fine.
Rank the pain next day
3 out of 10.
How did the port heal?
I got the port on the 4th and got my first chemo on the 9th. They would keep the bandages over it, and they steri-stripped them. I had to let them fall off, didn’t touch them.
The first time they used the port
It kind of freaked me out. The nurse suggested I touch it, but I didn’t want to. It’s not terrible. The first couple times, it was sore and just getting used to it. I’m used to it now. It’s a little poke, and it’s just weird.
It’s not that painful. They give you numbing cream. I think I used it twice prior to chemo. Some people use the numbing cream. Some people don’t.

Chemotherapy (R-CHOP)
What was the treatment plan?
She told me they would do R-CHOP, described mostly all the side effects and the timeline. The timeline was hard because my mom lives in Vermont and I’m in New Hampshire, and we commuted to Boston. Scheduling-wise, it was really hard.
Describe chemotherapy cycles
I was told it was every 21 days. I didn’t know what to expect or what I’d be feeling. The hard part was I didn’t want to leave home, but I didn’t want my mom to live with me constantly.
Treatment was Day 1, and then you come in the next week for labs, assuming everything’s fine. Third week, I was free.

Understanding the impact of cancer
It took a while to figure out. The hardest part was when she was like, “You’re going to lose your hair,” which I knew, but I wanted to be in denial about it.
A really hard part when we were talking about it was that I ride horses. I knew I couldn’t ride because of my knee issue, but she told me I couldn’t go to the barn because of germs and infection. That was one point I just lost it.
It was just like, “Fine, I’ll get through it if I can go home and be with my horse.” She was like, “No.”
It was realizing this is a huge thing that is really going to impact me. I think it built up. I was trying to hold it in for so long. It was realizing that was going to be hard.
How did you decide where to go for cancer treatment?
I didn’t have to pick them. It just so happened I was at physical therapy, and I saw a doctor there. He referred me to an orthopedic from Beth Israel.
Then they sent me to hematology/oncology. I didn’t pick. They were just like, “Here are your doctors.” I worked with a doctor and a fellow; they’re both great. I never had an issue with them.
She actually got me a second opinion at Dana Farber. I didn’t even ask for it. She just wanted a colleague to weigh in on my case. I was already in Boston for that one doctor. Boston is a good place to be, so I never really questioned it.
The outpatient experience
For the R-CHOP chemo, I was outpatient. It was always on a Monday. My mom and I would go in, 11 a.m. or 12 p.m. or so. I would get my port accessed, and they’d draw labs.
Some days they took me back right then. Other days I’d have to sit in the waiting room for 45 minutes, and they’d bring me back.
You got some pre-nausea medications. They would start the chemo meds. People would come in and out. I would just lay there. I remember talking to a social worker.
My doctors would come in, but I was really out of it. They give you Benadryl and Tylenol. Two of the drugs were not IV infusion. The nurse would push them herself.
The infusions were at least 4 hours. It was just Monday, and then I would have prednisone pills for the first week. Then I would also get a Lupron shot at the end.
The Lupron shot (fertility)
A side effect of chemo can be infertility. I’m not in a relationship. I’m not in a position to freeze my eggs, so that wasn’t a question really.
Lupron is hormone therapy. It shuts down your ovaries to preserve them and preserve your fertility. I would get a Lupron shot every round of chemo to preserve my ovaries.

It was a shot in the muscle. I would get baby hot flashes. They were short. I remember rolling down the window in the car, feeling really hot. I didn’t get my period for a really long time. That’s the point of it.
They brought it up. I didn’t even have to think about it. I was just like, “Okay, I’ll do it.” It’s definitely in the back of my mind that maybe I won’t be able to have kids, or maybe it won’t be so easy.
It doesn’t have to affect me for the rest of my life, cancer in general, but I feel like it will.
Last chemo round
Round 6 was hard because it was my last round and 2 days before Christmas. My mom was with me. We went to chemo, and then the next day we drove home to Vermont. I felt miserable. I thought I would sleep in the car, but I didn’t.
I can remember Christmas. I know I was there, but I don’t remember what happened. I know I felt miserable, and I know I went to bed at 5 p.m. It was a lot to go back and forth.
The following week, I came back here for my scheduled PET scan, which was the last PET scan.
R-CHOP Side Effects
Chemo side effects
Summary: Nausea, tired, “chemo brain,” irritability, neuropathy in fingers
The first round, the first week I just felt headache-y. I wouldn’t say I felt 100%, but I felt fine, which is really weird. That was good, the first round, until about the third week. My hair started falling out.
I think in my third round, my doctor said rounds 3,4 and 5 are the hardest. She was 100% right. Round 2 was okay. I felt gross the first week, but nothing major. I felt nauseous but it was controllable.
Round 3 I felt really awful. Headache-y, so nauseous, everything tastes awful. I did get really bad mouth sores every round after that. It really hurt to swallow. Brushing my teeth was incredibly painful, so that was really hard.
Just being tired, nauseous all the time, isn’t really fun. I didn’t sleep much throughout this whole thing, so not sleeping was a side effect.
»MORE: Cancer patients share their treatment side effects

Chemo brain you hear about. I felt I was totally in a fog. I do remember losing my train of thought, which I didn’t connect to chemo for awhile. I couldn’t spell anything for a while, even after I was done. I would be typing on my computer and trying to spell out words, and I couldn’t do it. I felt like I was in a fog the whole treatment.
I did get back pain after the third and fourth rounds. I was told I was at risk for it spreading to my spinal cord and my brain, so it freaked me out.
When I had back pain, I was really freaked out about it, but it turned out to be nothing.
I noticed I was super irritated all the time, which I think is a whole side effect from chemo. I remember watching my mom fiddling with the key in the door and just grabbing it, being like, “Let me do it.” And her navigating directions. I was so irritated. I think it was more a side effect of everything.
Also, neuropathy in my fingers. It went away once I finished treatment. I had bad acne, was prescribed ointment and acyclovir. I had no appetite, and everything tasted awful.
What helped prevent chemo side effects?
She told me the first week to take the anti-nausea medicine twice a day regardless, so I had Zofran, which is first-line anti-nausea, and Compazine, which I would take a few times, too.
I didn’t really have an appetite. I never actually threw up. I wanted to, but it was controllable. I ate a lot of ginger to the point that now I don’t really want to anymore (to help with nausea).
For mouth sores, I used Biotene mouthwash a few times. There were a couple times I didn’t brush my teeth because it was so painful. That’s all I did for it, kind of suffered through it.
I would go in the following week for labs, and they’d give me fluids, too, which did help.
Hair loss
That was really hard. I noticed it shedding. I have really long hair, and it was just shedding and kept coming. I did decide to cut it. I had a cut before my second treatment, and a few days after my second treatment I shaved it.
»MORE: Dealing with hair loss during cancer treatment
Cutting hair
I knew it was going to fall out anyway. I didn’t really care. I didn’t have anything to go off of. I just said, “I need this short because it’s all falling out, so just cut it.” It was okay. I didn’t really love it, but I just knew I had to do it.
I’ve never drastically cut my hair. I had long hair all the time. You know it’s going to happen, but when it actually happens, it sucks. It’s hard. I dealt with it for a few days. It was really long. Then I was like, ‘I need to cut it,’ because it became more of a pain.
I’d like to think I should’ve shaved it the first time, but I think cutting it first, I needed it in the moment. I cut it [short] and I hated how it looked, but it was still falling out. I knew it was really annoying, so I just had to do it.
About a week went by, and it was still falling out. I had bald spots, so I was like “Okay, fine, I’ll do it. I’ll just shave it.” I just walked in and did it.
Shaving the head
I went to a salon to have it done. My best friend from college lives in Colorado. She actually cut her hair because I had to. That was a huge thing. She was really supportive.
Her mom’s a hairdresser, and her mom did it. She cut her hair not as drastically, but really short. She said she probably wouldn’t have done it if she didn’t have to, so that was really nice.
One thing that was really interesting was I did donate my hair. I thought it was ironic that the first time I was doing this, I had to for cancer, so that was interesting.
Describe the neutropenia
I was lucky I was never neutropenic. I was barely neutropenic the day they told me I was in remission. I wasn’t hospitalized or anything. They were just like, “Please be really careful.”
You have to stay isolated
Be really careful. Don’t go to large crowds, places with germs. That was a major thing — avoid large crowds.
R-CHOP Progress
Mid-treatment PET scan
It came back good that things were shrinking. They were pleased with that.
They had the results, but I didn’t receive them until the following week when I went in for labs.
Scanxiety (anxiety waiting for test results)
I just tried to go with the flow and not obsess over it. It’s definitely personality.
I knew I had to do what I had to do to beat this, so I just went through it and didn’t question anything.
»MORE: Dealing with scanxiety and waiting for results
Deauville score
They didn’t ever mention that to me, but I have access to all of my notes. I follow that a lot online. My first PET scan Deauville score was a 5. The mid-treatment scan was a 3.
Post-treatment PET scan results
(Deauville score: 1)
It was Day 14 of my cycle. My mom was with me. They told me it was good, that I’m in remission. My mom started crying because she was relieved. I was like, “I can breathe again, and this is what you work for.” I was actually slightly neutropenic, and I remember I felt miserable.
I cried a lot on the way home just because I was overwhelmed and I was tired. Also, I didn’t feel like I was done-done because I knew I had the methotrexate treatments after.
But I do remember in the lobby, my mom was like, ‘You did it!’ I was like, ‘Yeah, I can breathe again.’
My mom told my family that day, my immediate family, that I was good. But I didn’t feel euphoric or anything, which was really weird. I knew I had to go through the next treatments, so I guess I was waiting until that was done to say, “Okay, I’m free.” I think I was overwhelmed and didn’t feel good.
More Chemotherapy (High-Dose Methotrexate, Ibrutinib)
Why continue with more chemo?
When I met with the doctor at Dana Farber, he was the one who said, “You’re at risk for prophylaxis of the spinal cord.” I knew from then they wanted to do high-dose methotrexate, which is a different treatment.
I didn’t know when that was happening. He did also put me on ibrutinib, which is oral medication, so I was on that throughout.
Because I was at risk for the prophylaxis, they just wanted to do it. I didn’t want it spreading, so I was like, “I’ll definitely do it.” I didn’t realize they were waiting until I was done with R-CHOP to do it, so I was like, “When’s it going to happen?” In my last round of chemo, they explained it to me.
I had a follow-up. I consented for it, and they told me all the risks, side effects. That was 3 rounds of a week in the hospital each.

High-dose methotrexate regimen
I would go inpatient for that. They told me I would have either 3 or 4 rounds, and I didn’t really know what determined how many rounds. It was a week in the hospital, and then I had a week off.
I went in and couldn’t have any acid. I had to go on a low-acid diet before going on. They hype you up on sodium bicarbonate. I had to take pills prior and then the entire time I was in the hospital.
They had to monitor my urine pH to make sure it was safe enough to receive the drug. I’m on IV fluids the entire time I’m there. I had an IV and my port attached. They would give me the methotrexate, and that was a 2-hour infusion.
24 hours, and they’d give me what I called the “rescue drug.” I got that every 6 hours after the infusion. It was Monday through Friday. They just keep you there because they have to make sure it clears your system before they send you home.
Leucovorin, the rescue drug
That helps to clear it out of your system, make sure it doesn’t back up in your kidneys. It was every 6 hours. They’d hang a new pack for a half hour (every day). It depends on how long it takes your body to clear the drug. My oncologist said it’s a 3- or 4-day hospital stay, so the first time I was hoping I could go home Thursday, but it was Friday every time.
Methotrexate side effects
I was super nauseous, and also I felt hungover because I really didn’t sleep in the hospital. Other than that, I reacted well to it.
I remember telling the doctor I feel like garbage. He was super nice and was joking, ‘Yeah, I’m not surprised. This is basically poison.’
My hair didn’t start growing back till after this.
Hospital inpatient experience
I knew I wouldn’t sleep. One time they would have to draw labs and switch the IV at 1 a.m., so I was like, “I’m just not going to fall asleep until then.” They would draw vitals every 4 hours, so it was not great sleeping.
A couple nurses told me to just take Ativan. They give it to you to fall asleep, but I woke up anyway. People do sleep. I just didn’t sleep. Each time I had a roommate. I remember the first one, she would sleep all day. I’m not someone who naps easily. I’m just like, “How?!”
A couple nurses, if you’re sleeping, they’ll let you sleep. All the nurses I had were super helpful, super nice.
What’s the follow-up since treatment?
I finished treatment on Valentine’s Day and left the hospital. I had a follow-up March 3rd and labs.
After that appointment, they did schedule a PET scan because they like to do it every 3 months, which had to be postponed because of COVID-19.
Survivorshop and Reflections
Transitioning to “normal” life
It was so hard. One thing I think people don’t really realize is that life is really hard after cancer. You think you’re free, but you’re not. It’s weird.
I was living my life 21 days at a time. Then it dropped. I thought I’d want to go back to work. I thought I’d want to get back to who I was, and I didn’t.
It took awhile for me to actually get my energy back and be okay again. The emotional side effects after treatment were huge, and I think I just went through the motions the entire treatment.
Now that I was done, I was emotionally processing it. It was hard because I didn’t expect it.
Survivorship
I cried a lot. I’m an emotional person. I’d cry it out and be okay. I watched a lot of people’s videos on YouTube throughout the whole treatment. I did share a post on Facebook because a lot of people didn’t know. Now that I was done, I was going to be like, “This is what I went through,” so I decided to share something.
I got a lot of response, and a lot of people commented. A lot of people who I hadn’t talked to in forever reached out. That was cool.
People were like, “I can’t imagine it.” I think that’s right. You can’t imagine it unless you go through it. At 24, I never thought I would go through it. That was one of the hard things.

AYA (Adolescent Young Adult) Cancer Patient
I definitely felt I was having a hard time. I was trying to figure out what I wanted to do. I was waitressing. I studied nutrition and public health in college. I took a job related to that awhile ago, but it didn’t really pan out.
I had waitressed before, so I was like, “I’m going to waitress, make a bunch of money, take a trip and then try to figure out my life.” Everything was placed on hold, so I worked as much as I could for the summer.
I spent a lot of the summer dealing with the knee issue, anyway, so I didn’t really travel. Then the summer I got diagnosed with cancer, so the job was on hold. I had to quit working. I’m really thankful I had savings. My parents are behind me 100%, but having savings really helped.
I thought I would soul search throughout this time, but chemotherapy is a full-time job, which people don’t really tell you. I just did nothing for a long time, but one of the hard things is I felt I was overlooked because I’m not a child with cancer.
I’m not pediatric, but I’m not an adult with a family and children who has to do this. I’m not an elderly patient, where cancer is common. I felt overlooked a little bit, which was hard. I was by far the youngest person in the waiting room, so that was different.
Find your community
I definitely isolated myself more than I feel I should have. I’m an introvert. The hospital did have a young adult support group, which they tried to get me to go to throughout treatment.
But again, this was Boston, so I wasn’t going to go to Boston just for that. I never actually went until the one day it fell on a day where I was in the hospital anyway for the high-dose methotrexate.
I did go that one time. It was nice to meet with people. The social worker connected me with one girl who was kind of in the same boat. I’ve been talking to her one on one. That’s been good. I never thought I wanted to go to a support group or anything.
The support group, all the girls there were great, but I still feel I didn’t fit in 100%. It’s hard to find people who know exactly what you’re going through.
It was a small group, but they were all fully on the other side of treatment. Here I was just finishing treatment, and I still didn’t have any hair.
»MORE: What kind of support cancer patients say helped the most

What helped you through tough times?
My mom was my biggest support. I just complained to her. She commuted back and forth to help me.
Is it hard to ask for help?
Definitely. I don’t want to have to ask for help, but people want to help.
It’s really hard to accept that. I always felt not that I was a burden, but it was frustrating to say I need someone to drive me to Boston.
My dad drove me to my final PET scan more because she was worried about the weather.
She didn’t want me to drive, but I wanted to be like, “Just let me drive. I’m fine to drive.” Just leaning on other people, I felt like I was a burden.
People want to help. They don’t always know how or what to say to people going through this, so let them help in their own way. Accept people around you.
Learning how to sit still
I got bored. I was watching way too much TV. I was really into running and really into fitness, so to not be able to go to the gym or run has been insanely hard.
Right now I’m struggling with trying to get back into running. I finally was like, “Okay, I’m going to try and run again.” My bones are now really weak, so I can’t do that.
It’s a side effect of chemo, which I didn’t expect, but now it all makes sense that my bones are weak from the lymphoma, the hormone treatment, the steroids. I just didn’t expect it, so it’ll just take time for them to build back up.
What’s helped you most?
Just realized that people can live with cancer. It’s a huge thing I never wanted to go through, never thought I would. A couple people told me cancer changes you, and I think it definitely did.
You can spend a lot of time in denial, but you just gotta do it. You’ve just gotta go through and trust your doctors. I did, fully. I knew I would get through this, so I just did what I had to do. It is really hard. If you let yourself feel the emotions, you just have to ride the wave.
Recovering during COVID-19
It’s so frustrating. I spent 6 to 7 months in a bubble, not being able to work. Financially, that was really hard. I thought I’d want to get back to work and get my life back.
I realized I really didn’t want to, and that was really hard. I was finally like “Okay, I have to make money. I have to do it.” I think not having the hair was a big part of that.
But I finally went in and was like, ‘I can start in two weeks,’ and that was the week before everything closed. I’m still unemployed, the restaurant closed, and I’m still back in my bubble.
It’s really not much different than what I was doing, except now I’m still unemployed and financially hurting, but I’m just used to it now. I’m in my bubble, staying safe!
Last message to other cancer patients
It’s never fun to get cancer. It’s so weird I did. It’s hard to go through, and people are always just looking for someone to relate to, one of the reasons I’d do this video. I kept it really quiet. I didn’t want people to pity me, so I did my own thing.
Chemotherapy is a full-time job, so you shouldn’t feel guilty for not doing anything because your body is working really hard to fight off cancer. You’ll get through it. Just accept the help from those around you.

Inspired by Emily's story?
Share your story, too!
Diffuse Large B-Cell Lymphoma Stories
Lena V., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 1
Symptoms: Blood in urine
Treatment: Surgery, chemotherapy (R-CHOP), radiation
Cindy M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Itchy skin on the palms and soles of feet; yellow skin and eyes
Treatment: Chemotherapy (R-CHOP)
Tony W., Relapsed T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL)
1st Symptoms: A lot of effort needed cycling, body wasn’t responding the same; leg swelling
Treatment: R-CHOP chemotherapy, CAR T-cell therapy
Jonathan S., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Severe shoulder pain
Treatment: 6 rounds of R-CHOP chemotherapy, 10 rounds of methotrexate, 12 rounds of focal radiation, autologous stem cell transplant
Leanne T., Follicular Lymphoma Transformed to DLBCL, Stage 3B
1st Symptoms: Fatigue, persistent cough
Treatment: R-CHOP chemotherapy, 6 rounds
Paige C., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Weight loss, extreme fatigue, swollen lymph nodes in the neck
Treatment: R-EPOCH chemotherapy
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Kris W., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
1st Symptoms: Pain in the side of the abdomen
Treatment: R-CHOP chemotherapy
Robyn S., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL), Stage 2E
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: R-CHOP, R-ICE, intrathecal, BEAM; autologous stem cell transplant, head and neck radiation, CAR T-cell therapy
Barbara R., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Abdomen and gastric pain
Treatment: Chemotherapy R-CHOP, CAR T-cell therapy, study drug CYT-0851
Luis V., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Persistent cough, fatigue, unexplained weight loss
Treatment: Chemotherapy R-CHOP and methotrexate
Nina L., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Hip and lower extremities pain, night sweats
Treatment: Chemotherapy R-CHOP
Richard P., Relapsed/Refractory Follicular Lymphoma & DLBCL
1st Symptoms of relapse: Swelling in leg, leg edema Treatment:1st line - R-CHOP chemotherapy, 2nd line - clinical trial of venetoclax-selinexor
Shahzad B., Refractory Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Extreme fatigue
Treatment: R&B, R-ICE, R-EPOCH, CAR T-cell therapy (cell-based gene therapy)
FDA approved: October 2017
Erin R., DLBCL & Burkitt Lymphoma, Stage 4
Cancer details: Characteristics of both subtypes
1st Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatment: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
Emily G., Diffuse Large B-Cell (DLBCL), Stage 4
1st Symptoms: Pain in left knee
Treatment: R-CHOP chemo (6 cycles), high-dose methotrexate chemo (3 cycles)














4 replies on “Emily’s Stage 4 DLBCL Non-Hodgkin’s Lymphoma”
Hey, thanks for sharing this. I found out about 2 months ago that I have a large lesion on my right knee, and didn’t receive the diagnosis of DLBCL until a couple of days ago. I’m finding myself in a similar situation to what you went through – 28 years old, single, heavily relying on my parents for the time being. I’ll be starting chemo this Friday.
I’ve been on crutches for about 2 months now, it’s looking like I’ll be on them for a long while. Your recounting of what you went through has brightened my mood (which is rare these days) by showing me that getting through this isn’t impossible. I know it won’t be easy but I at least I have an idea of what to expect – so thanks for that.
I’m wishing the best for you, and hoping that you’ll be perfectly healthy for a very long time going forward!
very interesting reading , from other people patients that suffered large diffuse B Cell stage 4 non hodgkins lymphoma , same as i suffered from, now seventeen years and still in remission
Alan, so glad you have been in the clear for 17 years. Incredible. Thank you for sharing!
from a fellow large diffuse B CELL SURVIVOR, Now seventeen years in remission, age 43 when diagnosed stage 4, stage 4 treatment SIX ROUNDS R CHOP EVERY THREE WEEKS ,