Lindsay’s Stage 4 Metastatic Relapsed Colon Cancer Story
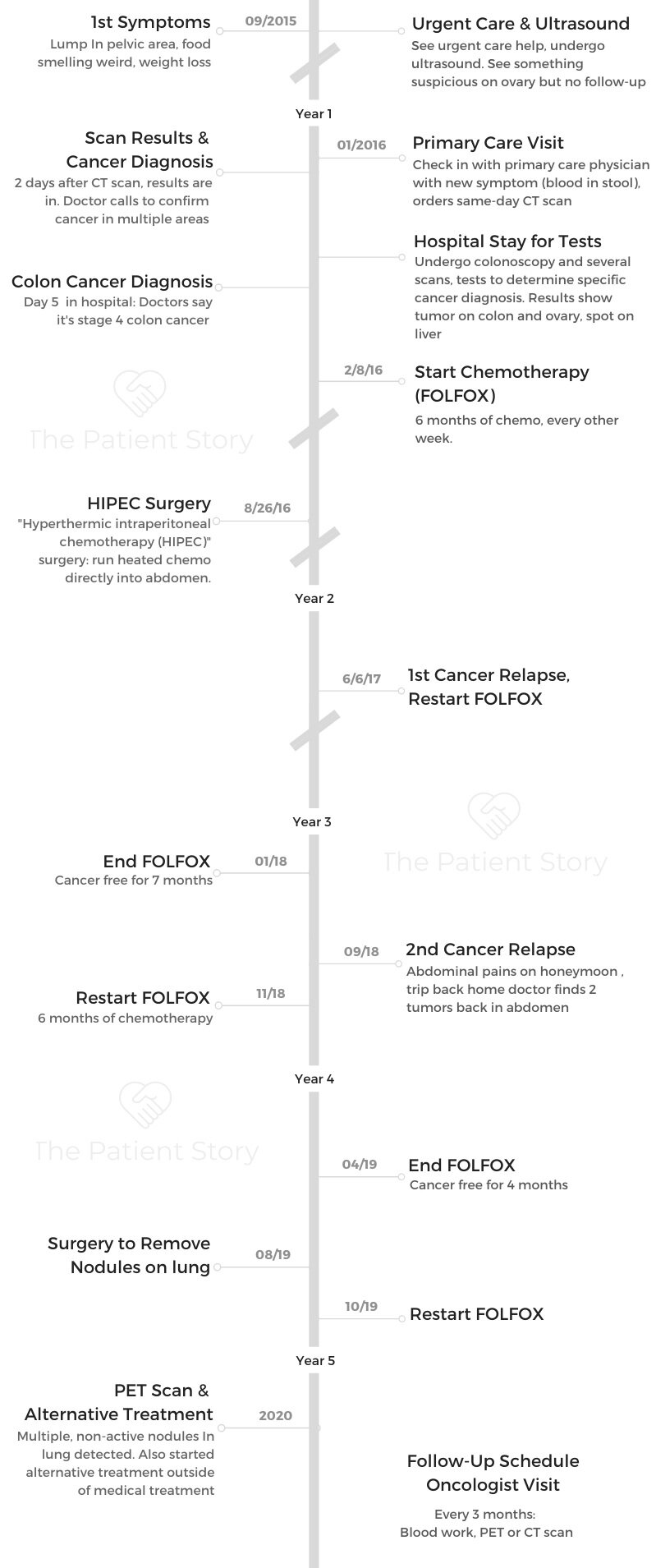
Lindsay shares her stage 4 (metastatic) colon cancer story, the relapse, and all the treatments she underwent: chemo, surgery, maintenance chemo, and a second surgery.
In her in-depth story below, Lindsay digs deep to highlight many issues that she had to navigate after the colon cancer diagnosis, including being her own patient self-advocate, managing through the stress of a relapse, trying alternative therapies, and trusting oneself through the process.

- Name: Lindsay D.
- Diagnosis:
- Colon cancer
- Relapse
- Staging: 4
- 1st Symptoms:
- Lump in pelvic area
- Food smelling weird
- Losing weight
- Treatment:
- Chemotherapy
- FOLFOX (infusion)
- Colectomy (surgical removal of colon)
- Maintenance chemotherapy
- Xeloda (oral pill)
- Chemotherapy
- Topics of interest:
- Self-advocacy
- Alternative therapies
- Living with cancer
- First Symptoms and Scans
- Diagnosis
- Describe the moment you got the diagnosis
- How did you break the news to your loved ones?
- Diagnostic tests in the hospital
- Getting through the waiting periods
- Describe when you heard the diagnosis
- Dealing with a caregiver with a different style in handling the diagnosis and treatment
- People will give you their unsolicited opinions
- How do you handle all the incoming messages from well-wishers and question-askers?
- Where had your cancer spread to?
- Treatment Decisions
- Chemotherapy (FOLFOX)
- Surgery (HIPEC)
- Transitioning from chemo to surgery plans
- Describe the type of surgery you underwent
- What happened at the appointment with the surgeon?
- Describe the colon surgery (colectomy)
- My body was just like, 'Nope, we're not going to do it.' It was a long wait.
- Dealing with a prolonged hospital stay
- Going to the bathroom after surgery
- Post-surgery scan
- Surgery results
- Follow-up schedule after surgery
- Relapse and Continued Treatment
- Alternative Therapies
- Mental & Emotional Impacts of Cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Surround yourself with those people, and be open to support and community and reaching out. It opens up a whole new world. It’s a crazy journey. It’s such a bittersweet thing because there’s so many bad things and scary things about this.
But then there’s so much that you can learn and that you can pay forward. In those moments, it makes you feel like there’s a little bit of a purpose for this.
Lindsay D.
First Symptoms and Scans
How old are you when you were diagnosed?
I was 32 years old. It was 3 weeks before my 33rd birthday.

What are the first symptoms?
In September, I started to feel a lump in my pelvis area. I had my son the year before, so I thought maybe it was just still me healing from having a C-section. I put it off.
I was like, “I’ll just watch it.” My husband’s a physical therapist, so I told him about it. We thought maybe it was scar tissue buildup, so he worked on it a little bit. After about a month or so, he’s like, “This isn’t going away. Maybe we should get it checked out.”
During that time, I’d started having other symptoms. Food started smelling really weird to me, and I started losing weight.
Then I started thinking, “Maybe I’m pregnant again.” I took a bunch of pregnancy tests. They all came back negative.
I usually range about 115 to 120 (pounds), and I had gotten down to like 95 pounds. I dropped a lot of weight really fast, and so I knew something serious was happening.
I’m like, “Okay, it’s not that.” Then with the weight loss and everything, just not feeling well. Then I started getting a lot of pain in that area. When I would stand up, it was almost like a burning sensation. I decided to go into an urgent care, and I told them what was going on.
What happened at urgent care?
They decided to do an ultrasound. They’re like, “Well, we can see something’s happening, but we don’t know what it is. We want to get you in for an MRI, so we’ll be in touch with you.”
A couple months went by, and I hadn’t heard from them. In January, I just went to my primary care doctor. By then, I started having blood in my stool.
I knew something was really serious and went in to talk to him. That’s when he was able to get me in for a CT scan that day that I went in.
Be your own advocate
What I’ve learned is you really have to be your own advocate. I didn’t have any family history of any type of cancer, so that wasn’t even on my radar.
Now, looking back, I feel like I even had symptoms maybe 2 years prior. Right after my son was born, I was having a lot of digestive issues.
I would go into my primary care, and they just said, “You’re constipated.” It made sense. You could feel it, and it made sense, too. The stuff they gave me helped.
But that was it. There was no, ‘Let’s try to test for something.’ You really have to fight for yourself.
When you feel like there’s something wrong, you almost have to just keep going in and telling them, ‘We need to do something more.’
That would be the advice. Looking back now, what I wish I would have done was be a little more proactive in the very early signs of saying, “Is there any way we can check to see if there’s something more here?”
»MORE: How to be a self-advocate as a patient
Describe the ultrasound
The ultrasound I got on the same day that I went in. I did get the results back that day. That’s when they said, “Well, we see something here.”
They could see something on actually my ovary, but they weren’t sure what it was. Of course, I started doing my own research, and I thought, “Maybe it’s fibroids or this or that.”
I was coming up with all kinds of scenarios. That’s why they said they wanted to do the MRI to just get a better detail to see what was happening.
I just ended up with my primary (care doctor), and after telling him my symptoms, he immediately scheduled me a colonoscopy and the CT scan. I was able to get in to the CT scan that day. I went ahead and did that. From there, that’s when they were able to tell me what was going on.
Describe the CT scan
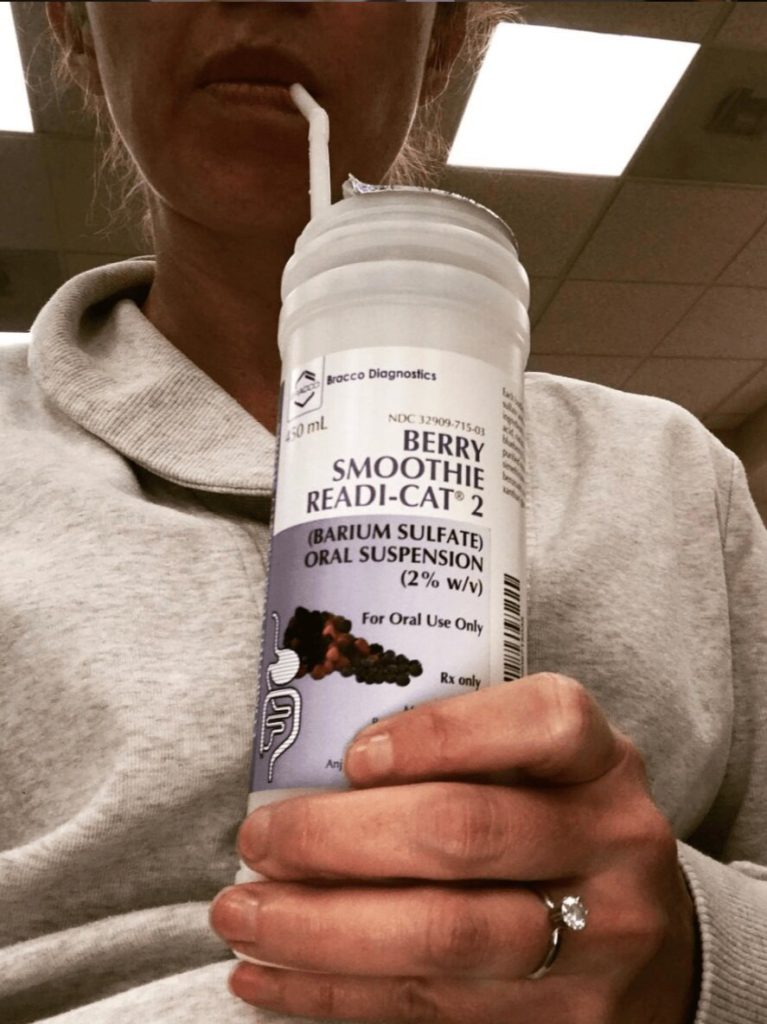
There’s a couple different scans you’ll hear about along this journey. One’s PET scan, and one’s a CT scan.
With the CT scan, they have you drink this chalky milkshake that has some sort of radioactive something in it so that when they scan the body, [what] shows up [are] the areas that there could be something going on in the body. You’ll drink that, wait about an hour, then they call you back, and they usually put an IV in.
The contrast dye feels like a warm sensation. Then they put you through something that’s like a CAT scanner and like a tube. I’ve learned to just kind of meditate during that time, because I know some people get claustrophobic.
That’s where I go mentally when I have to have these scans because it’s something that becomes a part of your whole journey, once you’re on this journey, is these types of scans.
How long does it take to get the ultrasound results?
It was 2 days. [It] depends throughout the journey where you’re at. If they need to know the results quickly, you could have them, like I said, within a couple days.
Now, it usually is about a week before I’ll hear something back about my results.
Diagnosis
Describe the moment you got the diagnosis
2 days after my scan, I was actually at work and with a client. My receptionist came over, and she’s like, “Lindsay, your doctor’s on the phone. Do you want to take this? Do you want me to just take a message?”
Because I was waiting on these results, I just told my client I need to take this call. I went to our break room area, and he was like, “Mrs. Snipes (maiden name), are you sitting down?”
I’m like, “Sure. Yeah.”
He’s like, ‘I’m sorry to tell you this, but you have cancer, and it’s in more than one location. I need you to get to a hospital as soon as you can, because we don’t know what it is. We just know it’s in more than one spot, and I need you to get to the hospital.’
He asked me what hospital I was going to go to, and he’s like, “That way I can have the doctors and staff ready for when you come in.”
I assume this is what it would be like when you hear people talk about how your whole life flashes in front of your eyes, because that’s what it felt like to me.
It’s almost like I saw the rest of my life in the future of what it could be or what I could end up missing. It’s just overwhelming to try to take that all in from a phone conversation.
It’s crazy because it’s one of those days where you remember everything single second. It’s like time freezes.
You’re like, ‘I have cancer. What do I do with that information? How do you unload that on anybody?’
I got off the phone with him. I was thinking, “I still have a client sitting in my chair whose hair is half cut. What do I do?” In that moment, I was like, “There’s nothing I can do about this right now, so I’m going to put that aside. I’m going to go finish my haircut.”
I did, and I’m sure he could tell something was wrong. Of course, I wasn’t going to tell him what was happening.
»MORE: Patients share how they processed a cancer diagnosis

How did you break the news to your loved ones?
My current business partner — we worked together at the salon at the time — I needed to tell her because we had some wedding trials coming up with brides.
That was the first time I said it out loud. I just went over to her, and I was like, ‘I can’t work this Saturday because I have cancer.’
She just started crying. That’s when I finally let go and started crying. We just went to the back room.
Then I was trying to call my husband, who was my boyfriend at the time, to tell him. Then I finally got through to him.
Again, it was another one of those moments where you’re just like, “I need you to meet me at the hospital because I have cancer.”
I have no way to explain this, because I’m like, “This can’t be right.” In that moment, you’re just like, “They messed up on something. Something’s wrong. It can’t be this.”
From there, I had one of my coworkers drive me to the hospital. I was there for 5 days after testing and scanning to try to figure out what type of cancer I had.
Diagnostic tests in the hospital
When I went in and they finally went over the CT scan with me, I had a tumor on my colon, another tumor on my left ovary, and then I had a spot on my liver.
Colon cancer doesn’t typically spread to the ovary. They were not sure if I had colon cancer that had spread to the ovary or if I had ovarian cancer that had spread to the colon.
The first night I was there, I had to drink this solution [like what] they give you when you get a colonoscopy. It looks like a gallon jug of water, but it’s a weird taste. It’s like a salt water. I had to drink that whole thing to clean out my system to prepare for the next day, [when] I had a colonoscopy.
Because the tumor on my colon was pressing against my ureter, which is the little tube that’s kind of between your kidney and your bladder, they had to put a stent in there. I went straight from a colonoscopy to that procedure.
Then the days kind of start to blur because literally they would come in whenever they needed to get me in for a scan. One night they came in and wheeled me out in the middle of the night to take me to get a scan.
Then they have to send off the biopsy, and so I spent a lot of time just waiting to find out what was going on. Day 5 is when they finally came in and went over everything and my diagnosis.
Getting through the waiting periods
The waiting is definitely hard, at least for me. I need to know what’s happening so we can make a plan. Not having a plan, I get anxiety. So just keep yourself busy.
I ended up having to spend a couple of those days making phone calls to my family, because my family lived in Florida and I now live in California. [I had] to call my mom, my sister, and my brother to give them the news.
To be honest, it’s a little hard the first few days because you have to keep having that conversation over and over again as you start to tell people what’s happening to you.
Then you’re going to have your ups and downs. You’re going to feel like, “I got this. I’m going to do this.” Then you have those moments of like, “This is so unfair. Why did this happen to me?”
You’re scared, but you’re trying not to be scared. It’s a lot of feelings and emotions. Luckily, I had a lot of support while I was in there. I had friends come by and bring me stuff, crossword puzzles, just things to do, or just come and sit and talk with me. We would try to talk about other things.
Then, and even now, it’s mindset, and it’s trying to keep yourself in a positive, optimistic place.
»MORE: Dealing with scanxiety and waiting for results

Describe when you heard the diagnosis
Day 4, they came in and said, “We still don’t know if it’s colon or ovarian, but we can say that you’re at stage 4 because it has metastasized outside of the original location.”
I knew no matter what it was going to be, I was at a pretty serious stage.
Day 5, they came in, and they said that it was colon cancer. I’ve been very thankful to my oncologist because she made me feel like there was hope in all of this. She said, “Colon cancer, there’s actually more treatment out there,” at that time.
I’m not sure what it is now as far as colon versus ovarian, but she had told me at the time that I had a lot more treatment options with the colon cancer.
Even though the diagnosis does come with this tag of being not curable, there were a lot of new medicines and new treatments coming out, so stay positive and optimistic that we would be able to work through this and prolong my life as much as possible.
I truly believe that I will see a day that I’ll get past this. I’ve read so many stories. Even though you get those words, there is hope, and there are people out there that do beat this stuff.
My husband is in the medical field, so of course he goes to the worst-case scenario. He wanted to know my prognosis.
I actually said to him and the nurse, “If you guys would like to step out in the hallway and talk about that, you can. That’s fine if he wants to know. I don’t want to know. I don’t want that in my head. I don’t want another human being giving me an expiration date.”
I did not have them tell me [prognosis], and she ended up saying the statistics don’t match up right now with with me or a lot of people that I’ve met along this journey because we’re younger, and a lot of the testing that they’ve done has been on older men that were getting colon cancer.
Even though there are statistics out there, that doesn’t necessarily mean that we fall into them. Other than the cancer, I’m healthy.
»MORE: Read different experiences of a cancer diagnosis and treatment
Dealing with a caregiver with a different style in handling the diagnosis and treatment
In the beginning, it’s really hard. You have to learn to kind of shut people out. I hate to say that, but I tell this to people who reach out to me that have a friend or a family member that’s going through this. I say, “You need to go at their pace, because right now, they are being bombarded with a lot of information and a lot of choices.”
People will give you their unsolicited opinions
Before this, I knew nothing about cancer other than breast cancer, October you wear pink, and you lose your hair from chemo. That’s pretty much all I knew about cancer.
To have to be on the other side of that, have your doctors telling you one thing, then you have family members telling you things, and then you have friends that have now all of a sudden become doctors, and they’re giving you their opinion — it can be very overwhelming.
You are not a bad person by just saying thank you and leaving it at that. You don’t owe anybody any explanation. You really just have to learn to trust yourself and trust your judgment, because you’re the one feeling it.
That’s how I’ve gone about this entire journey. I’ve had people disagree with the things that I wanted to do and the things that I’ve chosen to do. That’s okay, because I get it.
They’re scared because they can’t feel it. They can only be the observer, so they have no idea where I’m feeling it. If it feels right to me, then that’s the choice that I make.
During that time, after my diagnosis, I went into the bathroom by myself because I was like, ‘I just need a moment by myself.’ I kind of gave myself a pep talk.
I looked myself in the eye in the mirror, and I said, ‘Lindsay, you have cancer. This is what it is. Dying is not an option. Either you’re going to figure out a way to live with it, or you’re going to beat it.’
That’s kind of been the mantra I’ve held onto through the whole thing, really just keeping my mindset and trusting my judgment.

How do you handle all the incoming messages from well-wishers and question-askers?
In the beginning, it was just more or less like saying, “Thank you for your opinion,” and leaving it at that.
You do have to learn to be okay with not answering your phone. It’s okay if you don’t respond to somebody because, again, you’re dealing with a lot, so that’s what I had to do. I almost had to just shut it off.
It’s like, “Look, I’m not trying to be mean or anything. I just it’s overwhelming right now, and I need to work through what I need to work through. Then I will let everybody know.”
Delegate somebody to answer your text messages for you. I’ve had my husband take my phone, and I’m like, ‘You handle everybody because I need to handle me, and you can answer all the questions.’ That’s okay, too.
Just trying to find little ways to learn to let people help as well. That was another big one that I had to learn, because I am very stubborn and like to do everything myself.
It was really hard to have my friends bring me food or offer to pick up my kids for me or whatever, because I felt like it was taking that away from me, but you’ve got to learn your limits. That takes some time.
Where had your cancer spread to?
That’s when I had my CT scan. I had the tumor in my colon, and then I had a tumor on my left ovary and a spot on my lung. Those were the only areas.
Treatment Decisions
Deciding where to go for medical treatment
I’m with an insurance group called Kaiser. That’s what we have here in California. It’s a big group. The nice thing about them is they’re all under this umbrella. When my primary care doctor called the hospital that I went to, they already had the colon cancer team ready to go and the team I would have if it ended up being ovarian cancer.

I was already working with both of those teams in the beginning, and then once we figured out that it was colon cancer, I was already working with my oncologist.
Getting a second opinion
My oncologist, I’ve been working with her since day 1. I went and got a second opinion at a pretty big group out here. I won’t say who they are just because I didn’t have a great encounter with the doctor. Not that he was bad or anything, but it was just very interesting.
She made me feel like there was hope, and this guy was very much by the book and like, “These are your only options. If you don’t have this, you’re basically screwed.” That was another thing of trusting my gut and trusting my judgment.
I had this one doctor that is like the top guy at the place that he works. I didn’t go with him because my oncologist that I’ve been working with has really worked along with my values and who I am. It’s really made this journey to me a lot easier.
Getting medical advice and second opinions
Everybody’s different, so everybody wants a different thing. My husband’s cousin was diagnosed with the same type of cancer as me. She was my go-to person for everything. While I was in the hospital, I was calling her, like, “What should I expect next?”
It was nice to have her to reach out to, but she was very much all medical. She was like, “Trust your doctors to do everything. Trust everything they recommend.”
I listened to my doctors. Obviously, they’re really well trained in what they do, and they’re amazing at what they do, but they are another person giving their best opinion.
I’ve done a lot of research on my own, and this goes to being a self-advocate for yourself, because there’s so much information out there. I’ve unpacked a lot of it in the last 4 years, and I’ve learned so much.
I needed a balance of something natural with the medical, and that’s worked really well for me. Again, one of those things is knowing who you are and what makes you feel like you’re in the right hands or on the right path.
Colon cancer treatment plan
It’s pretty straightforward with colon cancer. Usually, their first line of defense is chemo, depending on the situation. Obviously, I didn’t have a full blockage in my colon, so there was no need to rush on having surgery.
She actually said she’s like most surgeons — if it’s not an emergency situation, they want you to do about 6 months of chemo before you can talk about doing surgery.
She said our first line of defense is chemotherapy. The chemo I was on is called FOLFOX. It’s a cocktail. Oxaliplatin is one of the drugs, and the other one is fluorouracil (5FU).
That was another interesting thing that I learned about dealing with cancer. I always just thought chemotherapy was chemotherapy, but now I explain to people it’s almost like your Starbucks order or your your signature drink that you order at the bar.
It’s not always the same thing. The type of chemo that I’m on may be different than the type of chemo someone with ovarian, breast cancer, or just different types of cancers would have. For me, it was FOLFOX.

Keeping a sense of humor
One of the first things I found out was that I wasn’t going to lose all my hair, and so through all of this, I joke a lot.
It just helps me to just kind of laugh about the situation and try to keep a good mindset about it. But I was like, ‘What, I got cancer, and I don’t even get to lose my hair?’
I had lost so much weight. I had a wedding that I had to do. I was probably a couple weeks after my first treatment, and we ended up having to stop. I had to buy clothes. I didn’t fit any of my clothes because I lost so much weight, and my friend was like, “Is it bad for me to say that I’m jealous of your cancer?” I was like, “No, you can totally say that!”
Having a humor about it, because it’s scary. You’re going into the unknown. You’re about to be on this drug that you see people [on], and they’ve lost their hair. This is from being on a medication, so it is scary.
Chemotherapy (FOLFOX)
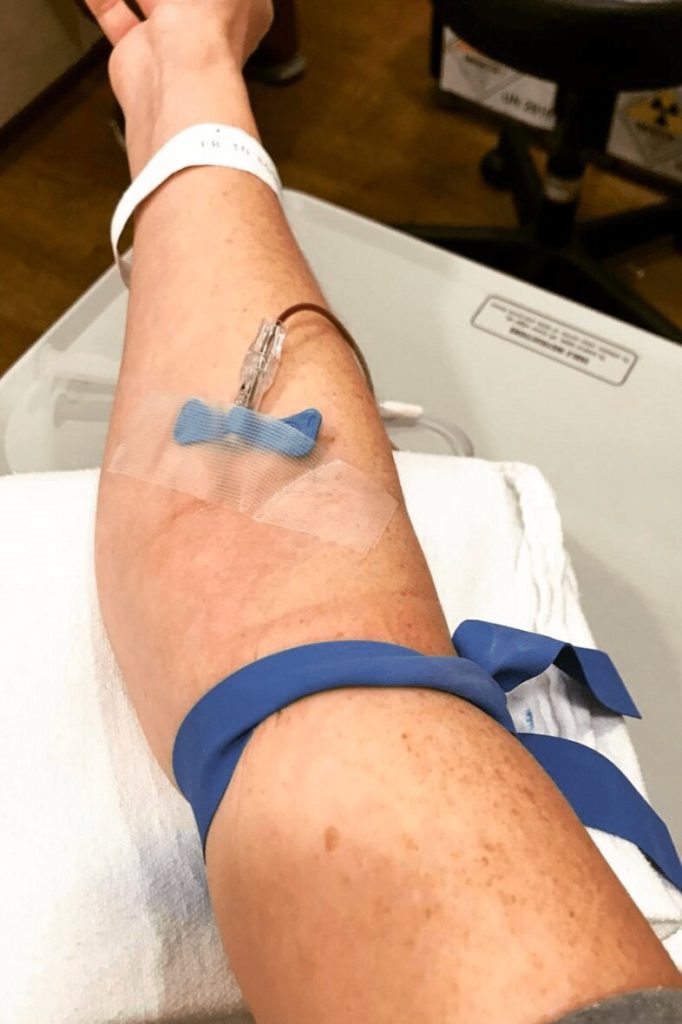
Did you get a port or PICC line?
There’s a lot of different ways that they can give chemo. One way is through a PICC line, which is this tubing they run into your arm. It goes directly into your heart.
I knew I was going to be on chemotherapy probably for a long period of time. I went ahead and had a port put into my chest, so it’s under my skin. I don’t have to have it changed, but they do tap into that. Just the whole chemotherapy experience my first time was really interesting.
»MORE: Read patient PICC line experiences

What is FOLFOX like?
I’ve talked to other people who have stage 4 colon cancer, and maybe it was a little bit more aggressive than mine was. Theirs was a little different, but for me, my treatment was every other week I would go in.
I would go in on a Monday, and I would be at the clinic for 2 hours getting the Oxaliplatin, which was one type of drug. Then I had to take home what I called my chemo kit.
It was a little pouch of the 5FU, and I had that on a slow drip for 48 hours.
I had to wear this pack. I was attached to my port, and I had to carry around this pack for 2 days, continuously getting chemotherapy.
Technically, you’re on it for 3 days, and then you get a week off.
What are the FOLFOX chemotherapy side effects?
Summary: thinning hair, aversion and pain with cold (touch), nausea, fatigue
You don’t lose all of your hair, but it does thin out quite a bit.
The biggest side effect is sensitivity to cold, and you don’t realize how awful that is until you realize how much almost everything you eat [or] drink is cold at some point. Either you’re pulling it out of the refrigerator or the freezer.
Even room temperature water can sometimes be too cold. It stings and makes your finger sting and makes your feet sting if you’re touching the floor. I had to keep socks on when I slept because I had hardwood floors. If the floor was cold, it would sting my feet. Touching anything would sting my fingers. Eating anything.
It’s almost like you have an allergy or an allergic reaction to cold. I remember one day getting into the car with my husband, and it was a really hot day. I put the air vents on me, and that cold air [started] hitting me in my face.
All of a sudden, I started to feel like I couldn’t breathe. I thought something was wrong with me, like maybe I was getting too much chemo. I made my husband take me back to the clinic, and I told them something’s wrong. Something’s happening.
They gave me Benadryl, and then she said it was because I had put the cold air directly on my face. That’s the biggest side effect. Obviously, there’s nausea, which is very, very common and in most chemos.
Fatigue. I had to really learn my limits with that. Your body is just aching. It’s like almost you could feel it in your bones. It’s like your skin is sensitive, so it’s not fun.
Obviously, not everyone experiences all of these side effects, but those are probably the most prominent ones that I experienced.
Describe the chemo and side effect cycles
I’d have one what I called my good week, which was my week off of chemo, and then my bad week, so every other week.
Usually for side effects, the coldness would start right away. That was one that was immediate. I really didn’t start to feel sick or nauseous until the third day when I would take my pump back, and they would disconnect me from the pump.
Pretty much all the chemo was in my system. That is when I would start to experience more not feeling so well and just being really tired.
Then the pain in my body would [start] Wednesday, so that would last until about Sunday. Monday, I kind of started to feel a little better. Then usually by the end of the week, when it was time for me to go get blood work and start all over again, I would start to feel better.
The first year, I did the 6 months of chemo because then I did end up having surgery. I did 6 months of chemo, and that was every other week. As it builds up, obviously, the side effects get a little bit more intense, and they take a little bit longer to come out of on the other end.
What helps prevent chemo side effects?
During all of this time, I was working with a nutritionist and taking a lot of supplements. He was really helping me minimize my side effects.
I know vomiting is pretty usual to happen when you’re on chemo. I’ve never gotten sick, like actually thrown up, being on chemotherapy in the past 4 years that I’ve been on it.
I got little tips from my husband’s cousin. Different little candies that you can suck on, that kind of help. I started to just leave my [water filter] out.
Then just buying a lot of gloves and scarves and socks. I stocked up on all of those because the issue with the cold sensitivity is if you let it get too bad, you can end up getting neuropathy and actually have some permanent neuropathy from the chemotherapy.
Just little tricks you start to learn. Switching up your schedule. My husband would take the kids to school those weeks so that way I could sleep.
Learning to just rest. Rest is probably the biggest thing that I feel like may be difficult for a lot of people, because we’re always so busy and go, go, go.
That’s just the way our country works. We just go all the time, so learning to just be still and rest when your body is telling you to rest probably was the biggest challenge for me to try to work to help me heal.
How many times do you undergo a scan?
Their goal was to shrink everything down as much as they could . Then we could go and take it to a surgeon and see what they said [and] if they felt confident or comfortable doing surgery. During that time, we did scan everything.
We typically do scans about every 3 months. We did 3 months of the chemotherapy, and then I had my first PET scan. We would check up on it just to make sure.
How often is blood work done?
I have to get blood work done before every chemo treatment. There is a thing in your blood testing called CA levels, and basically it just reads the amount of cancer that’s in the blood.
This reading can differ in different people. Some people’s readings are really low, but they still have a lot going on, or vice versa. They really can’t go off of that.
But my CA level always followed pretty well with what was happening in my body. As those started to come down, we could tell it was working. Throughout this journey, that’s been very helpful for me. I’ve been very fortunate that is always a good reading, because it can get really hard when you’re waiting 3 months to get scanned.
You’re like, “I’m going through basically hell with chemotherapy, and I don’t even know if this is working.”
It can be very frustrating, but being able to follow that helps. Then having the scan and seeing that the chemo was actually working. You take all of those little, small accomplishments.
Surgery (HIPEC)
Transitioning from chemo to surgery plans
The chemo was working really well and everything was shrinking down, so they referred me to a surgeon.
I went to speak with him. He looked at my scan, and he’s like, ‘I think you may qualify for this specialized surgery. It’s intense, but it’s probably your best hope for getting ahead of this.’
I was like, ‘Well, if I’m a candidate, I’m open to it.” I’m open to trying anything. I’m okay with being aggressive.
They sent my scan to a doctor in San Diego and had him review it. It came back that I did qualify for the surgery. There’s a lot of restrictions with this surgery. You can’t have any kind of anything going on with the lungs.
He did mention because of the tumor pressing up against my ureter, my left kidney, I was having some issues with that. He’s like, “If there’s any issues with your kidneys, they may decide that this is a no-go.” It was a very fine line of getting into that. The requirements are very specific as far as how you can qualify for this surgery.
Describe the type of surgery you underwent
It’s a very major surgery. It’s called hyperthermic intraperitoneal chemotherapy (HIPEC). Basically, the idea of this surgery is that they go in and debulk, which is removing any tumors or anything that they see.
Then after that, they take these 2 prongs they put in the abdomen, and then they close you up and run heated chemotherapy directly into the abdomen for 90 minutes to hopefully get rid of any cancer cells that they can’t see.
That’s the thing. Just because they get rid of the big stuff doesn’t necessarily mean you’re always in the clear. Cancers [and] tumors have to be a certain size before they start picking up on a scan.
They brought me in, and I went down to San Diego to see Dr. Lowe. He’s one of the top guys that does this type of surgery, which is about 3 hours away from where I live. We went down and met with him.
He and his team were, again, very amazing. I’ve been very fortunate that the people that I have decided to work with have that same idea of hope, with the goal of really trying to get you better.
What happened at the appointment with the surgeon?
I had my meeting with him, and we went over everything that was going to happen during the surgery. They were going to go in, and they were going to remove a section of my colon. I wasn’t going to need the colostomy bag, which I was really happy about.
He was removing my left ovary, and he actually gave me the option because I was so young at the time. He said typically he told his patients to take both ovaries because there would be a high chance of it spreading to the other ovary now that it’s been on one.
But he told me because I was so young, if I wanted, in case I planned on having more children, they could leave one ovary. I already had 2 kids, so I opted for just having my ovaries removed because I wanted to be safe.
We went over all of that, and then they were going to have to reconstruct my ureter because it had been touching the area of my tumor. That required a second surgeon to come in at some point during this surgery to do that part of it.
Describe the colon surgery (colectomy)
When I went in, it ended up being a 7.5-hour surgery. It’s probably one of the most intense things I’ve ever been through in my life.
Probably the hardest part was I ended up being there about a month after the surgery because — and this is kind of TMI — I wasn’t allowed to leave the hospital until I pooped, because they had done surgery on my colon.

My body was just like, ‘Nope, we’re not going to do it.’ It was a long wait.
The plan was for me to only be there 14 days afterwards. After the surgery, the timeline is kind of hard, because now I realized probably the first 3 days, I was really out of it.
I don’t remember much about those days other than what my husband’s told me. After that, I did experience some bloating in my stomach, and luckily it was just fluid. They were able to drain that.
Typically, you’re out within 14 days after the surgery, but I ended up almost exactly a month after before my body was like, “Okay, we’re ready.”
Dealing with a prolonged hospital stay
It was probably more mentally challenging than it was physically, just because I’m very stubborn. I’m wanting to get up and start moving around.
Mentally, it was taking a toll because I was 3 hours away from my family, so it wasn’t like they could come visit me every single day. I spent a lot of time by myself. That was really hard.
All in all, the surgery went really well. They got all of the cancer out that they could see. When I got that scan back and he said everything is clear, it was one of the most exciting days of my life.
Going to the bathroom after surgery
I had a catheter, and at the time, they had a tube. I had the GI tube in my stomach. That was basically my way of going to the bathroom, so I wasn’t actually using the toilet at all. I was hooked up to a ton of tubes.
They have an incision, there’s a tube that actually goes into there, and then there’s a bag. It fills up, and then a nurse comes in and gets rid of everything. As they see that amount in the bag going down, they start to try to see if they can get you to go on your own. We tried a couple times, and it didn’t work, so it’s just a waiting game.
That was very frustrating. It was very defeating most days and draining. By the time I finally went to the bathroom, I literally cried because I was like, ‘I get to go home. This means I get to go home finally.’
It’s a very emotional battle that happens, because every day your goal is, ‘I’ve got to go to the bathroom today.’ But you’re in a situation where you can’t force it to happen. Your body is going to do it when it’s ready.
Post-surgery scan
The days are blurry right after, but I’m assuming it was probably a couple days after the surgery that I had the scan and then probably a couple more days. Probably a week after the surgery is when I got the news.

Surgery results
It was the surgeon and their team that gave me the news while I was still in the hospital. I found out while I was in the hospital when they scanned me after the surgery.
The surgeon himself came in to give me the news, and he was such an amazing person. He came by to visit me every single day.
He had even planned a trip with his family, and before he left that day on the trip, he came by to see me to check on me and to let me know he was going to be out of town and his team was going to come in.
It was him and a whole team. They all came in, and they gave me that news. It was just one of those moments to celebrate, like, “Okay, we can do this.”
It was almost a moment of re-energizing me, giving me that same motivation I had when I was first diagnosed. When you’re first diagnosed, you’re like, “I’m ready; I’m ready; I’m ready.”
Then you go through highs and lows with the treatment because you feel so crappy, and then there’s a lot of other stress on the outside of dealing with cancer, especially when you have a family.
You feel like you become a burden. There’s a lot of stuff attached to that. But that news re-energized me and gave me hope again.
Follow-up schedule after surgery
Then I had to reconnect with my oncologist. I took all the information, and they sent all that over to her. I’m trying to remember at that time if we’d talked about it, because sometimes they’ll do maintenance chemo when your scans are clear, but I always opted to take a break.
I would say I needed to give my body some love, give it a break from this treatment, and let my immune system build back up. But I believe after the surgery, it was more like, “Okay, we’re good.”
In 3 months, we’re going to scan you again. For the first year, it’s going to be about every 3 months. We’re going to do a PET scan, just to check and make sure everything stays that way.
Basically, I was free to be normal for a while. It felt so good. My hair grew back all nice and cool and thick. Just to feel good every day to wake up and and feel good — you take that for granted when you’re healthy.
Relapse and Continued Treatment
Colon cancer relapse
During this journey, you start to really learn your body. You start to really have a good intuition with your body. (A year later) in June, I had started having pain in my lower abdomen again, and I was getting worried.
Then we did the scan. It came back the 2 tumors on my lower abdomen had come back, and it was the most defeating news that you can get, especially the first time. I actually had them take my port out because I thought I was doing so good. To get that news was crushing. You go through the motions, you feel so good, [and] your port is out of you.
There’s no words to describe it. I think I even took a picture, because then it was like, ‘Now I have to set up an appointment to go get a port put back in my chest.’
It was like starting all over again. I just felt like everything I had just done over the past year — going through that surgery and everything — and it was like, ‘Okay, here we go again.’
Second treatment plan
I had done so well on the FOLFOX, so we decided to go back to that. I felt good about that because this time I knew what to expect. I knew how to prepare for it because I had gone through it before.
It was just to get it back to the plan. Then I did another 6 months of chemotherapy.
On and off chemotherapy
It’s crazy, because over the last the year after the surgery, it was basically this on-and-off situation. I did 6 months of treatment. I would do really well on the treatment. We shrunk down the tumors to where clearly they didn’t go away but small enough that they were not being picked up on a scan anymore.
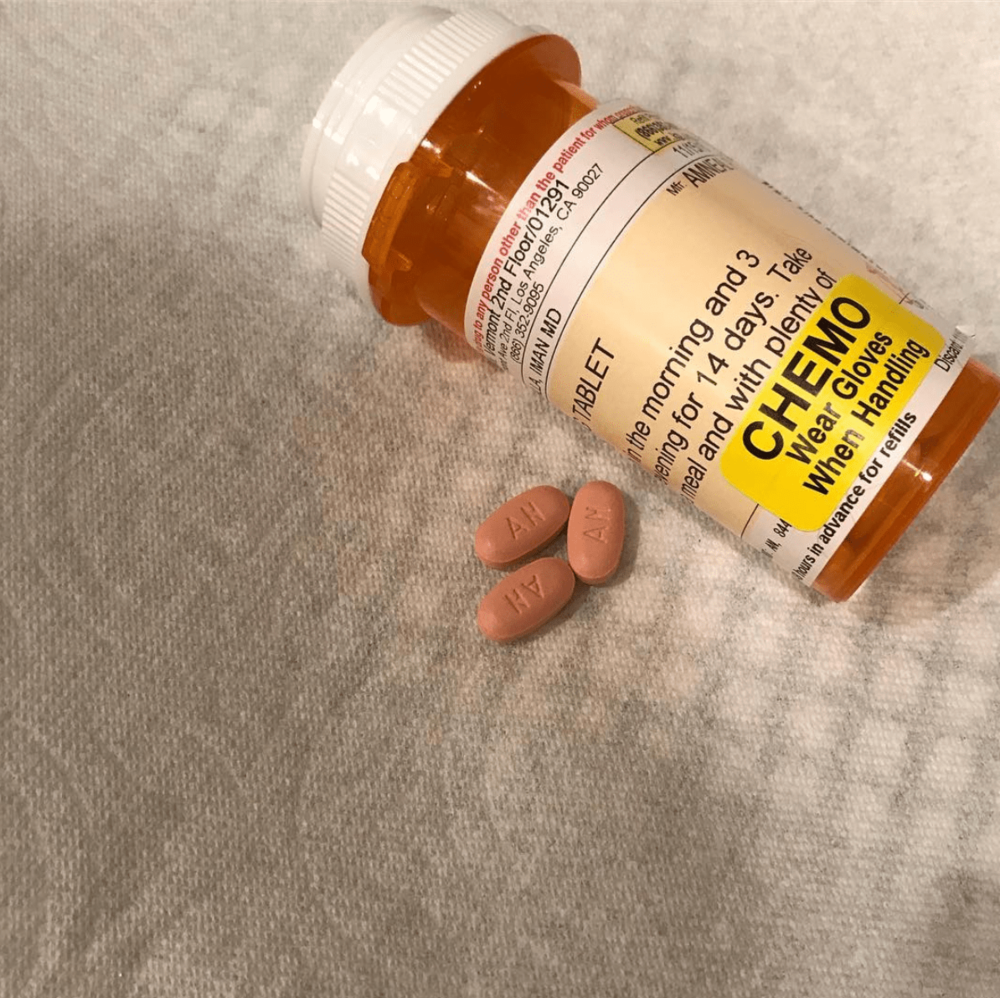
During that time, I would go off for treatment, and she had offered to do a maintenance chemo. There’s a chemo pill called Xeloda, and you take it orally.
Typically, someone that has been diagnosed at my stage and with this cancer, even when you’re not doing the major chemo, if things are going good, they do what they call maintenance chemo.
You just consistently stay on chemotherapy. For me, again, I’m someone who needs a balance, and I was like, “I’m gonna take a break.”
As much as chemotherapy helps, it’s killing everything. It kills the cancer cells, but it’s also doing damage to everything else in your body. I just felt like I needed to take a full break from that, but I always did really well.
I got 7 months out of the second time before the same thing [happened]. Tumors came back, and then I’d go back on the chemo. And again.
Continuing with FOLFOX
That’s another thing. I feel like having the balance of the nutrition and the supplements and doing all that stuff outside conjoined with the chemotherapy really helped me handle this chemo really well.
My oncologist actually just recently told me, “You’re so lucky that you’ve been able to stay on this.” In the beginning, when I started FOLFOX, I was told I’d get about 6 months to a year out of this treatment.
Typically, the cancer starts to figure out ways around that treatment, and then you have to switch to another type of chemotherapy. Over the last 4 years, I’ve still been able to stay on FOLFOX, and it’s continued to work.
Trying maintenance chemotherapy (Xeloda, oral pill)
There was one point where I did try the Xeloda. It’s just a pill. I would have just been taking that alone, just the pill.
I believe you do a week of it, and then you get a week off. I opted not to take that to give myself a break. When I was good, I wouldn’t take any sort of treatment.
But then this last time that it had come back, I decided maybe we could try. There is a treatment where you can do the Xeloda pills with the oxaliplatin. Instead of bringing home a pump, I would just come home, take a pill, and replace the pump.
That really wiped me out. I had never experienced chemo like that, where I couldn’t get out of bed. I was just like, “I can’t do this. I have 2 kids. I need to be able to function.” We ended up switching back to the FOLFOX.
Chemo contains the cancer but doesn’t cure it
I would have a scan about 3 months in that would have us decide:
Are we still moving on with this treatment?
Where are we at?
How much has the tumor shrunk down?
I always had a pretty good reaction. Then usually by the 6 months, we were able to shrink those 2 tumors down to the point where they weren’t visible or showing up on a scan.
This last time we had talked about potentially if it came back, those same tumors, we’d look into maybe doing surgery. The good thing is I’ve been able to contain this pretty much for the most part to just those 2 tumors.
Scans show possible new cancerous activity
This last scan last year, actually, I had something show up on my right lung. It had been there since right after my surgery, but there was no activity in it. We were just watching it because there’s nothing you can really do about it if it’s not active.
In a PET scan, they inject you with a radioactive — for lack of better words — sugar water. These things attach to inflammation in the body basically, and it lights up if it’s active. That’s how they can tell the activity level in a cancerous tumor.
After one of my scans, it showed up that this thing in my lung had started showing some activity. It was still relatively low, but it was doing something that it hadn’t done before. We decided that we would biopsy it, and it came back that there was cancer, so I had a second surgery.
Describe the second surgery
It was very minimally invasive. They were able to do it — not laparoscopic, when they go in through the chest. It’s called something else, but basically, it was just a few incisions in my side. They went in and removed the nodule, and all was good.
Thinking of changing treatments
Then my latest scan at the beginning of the year, I had all these nodules show up on my lungs. They were not active, and they’re still not active. Because there’s stuff going on in my lungs, they won’t do any type of surgery. They just don’t want to take any chances since there’s multiple nodules there, even though they’re not active.
I don’t know if they’re afraid that it could become active. They just say with the lung situation, it gets very tricky what they’ll do as far as surgeries.
We were at a point where we were starting to wonder if maybe the FOLFOX wasn’t working anymore, because my CA levels usually are a good determination of how the treatment’s working.
I had been on treatment. There were some mess ups with my scheduling, so I wasn’t being very consistent with the chemo. Just miscommunication happened, but my levels kept going up every time I would go in for blood work. Not much, but still they were going up versus going down.

We were actually debating on starting the next line of chemotherapy, which is called FOLFIRI. I believe they just get rid of the 5FU, and it’s a different drug with the oxaliplatin or vice versa. We didn’t really get into too many details, because we hadn’t decided if we were going to go that route yet or not.
During all of that time is kind of when all of this (corona)virus stuff started happening, and then I was connected with someone that had this natural treatment.
That’s what I’ve been looking for the past 4 years: trying to find a natural way to treat this. Chemotherapy can be exhausting after a while, and in my situation, my oncologist told me chemo isn’t going to cure me. It’s containing everything, but it won’t fix the problem.
I’ve been trying to find the root cause or ways that I can change some of this without going through all of this medication and feeling the way that I felt being on it.
Alternative Therapies
Trying alternative therapies
I recently decided that I am trying this natural treatment out, especially during this time that we’re going through right now with the whole coronavirus and stuff. It makes people like me more susceptible to a much more severe reaction to the coronavirus.
I was really nervous about having to go into the clinic because it is at a hospital and being around people that can potentially be sick. Also, being on chemotherapy suppresses your immune system. That scared me, and I was connected with someone that offered a natural treatment.
It’s something for a long time I’ve been wanting to try, and I thought this would be the best time to try it because it allows me to stay home and stay safe.
I’ve talked to my oncologist about it, and I was like, “I’m gonna give it 3 months. He’s saying in 3 months I should see a difference if it’s going to work.” For me, the worst-case scenario is I go back to chemotherapy treatments.
The natural treatment
It’s working with cannabis, but you don’t smoke it or ingest it. Basically, this guy has created a suppository. He has this machine that he pulls out the molecules of the THC and breaks it down to the size that it can attach to cancer cells.
Apparently, we have this cannabinoid system in our body, and that’s why there’s so many studies out there saying that cannabis can really help with cancer. He’s done a lot of research, and he sent me all of his work.
I felt like this is somebody that has done a lot of studying on this. It’s not just some random person that’s doing this thing.
The reason he got into this was his friend was diagnosed with lymphoma, and she didn’t want to do any sort of chemo treatments and go down that road.
Because he had been in this industry for a long time, she asked him if he could find something. He felt the research has fallen upon all these studies, so he started doing it. I just felt really good about it.
I believe very much in what you put out into the universe, you get back, and I have been asking for this. I’ve been asking for the signs to show me to this path, and everything just kind of fell into place at the right time for me to try this. I feel really good about it. It’s still very early.
»MORE: CBD, Cancer & Treatment Side Effects
How did your oncologist respond to you trying alternative therapy?
I did tell my oncologist about it. Next month, I’m going to have blood work with her. Then in 3 months, we’re going to do a scan to see what it’s doing.
This is another one of those moments where my oncologist makes me really happy because she’s listening to me and made me feel like she’s listening. She knows through this journey, I’ve been doing a lot of natural stuff, and for her to not put me down or tell me I’m wrong meant a lot to me.
I told her I take full responsibility for whatever happens in this situation. She’s supporting me, and that makes me feel really good.
Mental & Emotional Impacts of Cancer
How to manage mental and emotional stress
It’s really interesting. In the beginning, and I told a few of my friends this, I was like, “In a way, this diagnosis was a bit of a blessing.” I know that sounds really weird to say because it’s also been a very crappy thing to go through, but it really opened my eyes to living.
I think when you’re healthy, we go through this life, and we take it for granted. We don’t take advantage of everything, and we don’t think about death.
Nobody wants to think about that, obviously. But when you’re put in this situation, you almost have no other choice but to face it and to face knowing that potentially you can die from this.
Once you can be honest with yourself about that, you kind of let go of this fear. When you don’t have this fear of dying, then what is there to be afraid of?

Now, I always look at life. We all have a beginning, and we all have an end. It’s what are we going to do in between that? I just absorb anything. I can read anything. I can learn. This is where the whole being an advocate for yourself comes into play.
Because I’ve learned so much about myself. I’ve learned so much about my body through this journey. When I speak about my journey, I do like to talk to those that are going through it to let them know you’re not alone.
I understand how you’re feeling. I understand those lows. I know what it feels like to question, “Am I just being a burden? Would it be easier if I just died?”
You’ve got to be able to pull yourself out of those moments, know that there is a purpose here, you are supposed to be here, and use what you’re learning about yourself to spread that to others.
My biggest message: I like to talk to people that are healthy to remind them do things now while you’re healthy to prevent getting to where I am. I feel like we forget about that when we’re healthy, and we forget to take advantage of life.
For those that are going through this, educate yourself and read about stuff. I do a lot of meditation. I’ve tried acupuncture. You name it, I’ve probably tried it, because why not? Why not?
Trust your journey. Everybody’s journey is different.
Trusting yourself
We can all give advice and say all of these things, but you have to make the decision that’s best for you. Try not to let people force you into something that maybe you don’t believe in or that you don’t feel comfortable doing. Don’t be afraid to ask questions because in the beginning, it’s overwhelming.
You’re like, “I don’t even know what half of this stuff means,” for a long time. Even still, now I walk that fine line of being a little naive about it, but it helps me stay in a better mindset. That’s what works for me.
The biggest thing is if you’ve been diagnosed, just take the time to listen to yourself, to learn about your body, and to understand how it feels. I know immediately when something’s wrong in my body now.
For those of you that are caregivers or you just have a friend or somebody, go at that person’s pace. Also go at their personality. For me, I like to joke about my cancer. Some people, I can tell, are like, “I don’t know if I’m supposed to laugh at that.” But you can. For me, that helps.
Surround yourself with those people, and be open to support and community and reaching out. It opens up a whole new world. It’s a crazy journey, and it’s such a bittersweet thing. There’s so many bad things and scary things about this, but then there’s so much that you can learn and that you can pay forward.
In those moments, it makes you feel like there’s a little bit of a purpose for this. At least that’s how I feel.

Dealing with cancer during coronavirus
The first couple weeks of this, I was really angry because I’d get on Facebook, and there was this back and forth of some people didn’t believe it was happening. Some people think it’s crazy because we all have to stay home. “You’re healthy, and I’m not going to get it.”
I actually made a video that explains where we’re coming from as being high risk, because I don’t technically look like somebody that would be at high risk. Like most people, when I tell them I have cancer, they can’t believe it.
For me, I put it out there to my friends and those that were questioning this. I said, “I don’t get the luxury of taking this as a joke. I can’t not take this seriously because it can affect me so much more than anybody else.”
We’ve had to take so many precautions — because my husband does work in the medical field — of him having to strip down in the garage before he comes in the house and going straight to take a shower before he touches anybody.
We have to sanitize everything. I’ve literally been in my house for 3 weeks now.
We’ll go for a car ride just so I can get out and see. For those that are healthy, people are asking you to stay home not necessarily because of you, but because of how you can affect those around you and those that maybe you care about.
While you can joke about it or you can think, ‘I’m not going to get this,’ we don’t get the luxury of thinking that. We have to take the flu, pneumonia, any kind of sickness — we have to take it so much more seriously because [of] the difference between you and us. You may not have any symptoms at all or very mild symptoms, where this could mean my life, and it means my kids lose a mother and my husband loses a wife.
It just gets really frustrating when you see people that think it’s a joke, because it’s not. We don’t get the luxury of questioning it.
Last message to other people dealing with cancer
I think in the beginning, it’s good to find some groups that you can be a part of. I’m a part of some groups on Facebook. I’ll be honest, for a while, I didn’t want to do any research about cancer. I didn’t want to join any groups. I didn’t want to do any kind of support thing, because to me, that made it real. It made me feel like I was giving in to this disease.
That’s so not what it is. You need that support, you need people to talk to, and you need people that understand what you’re going through. It sucks to say I was fortunate because you don’t want anyone else to be in this situation, but I was fortunate to have my husband’s cousin that I can reach out to.
She was able to shine lights on things when they would come up that were unknown to me. On this journey, especially in the beginning, everything you go through it, you feel like you’re in this dark tunnel. You have no idea where it’s going or what the outcome is going to be.
To be able to reach out to people and have them go, ‘Yeah, I went through that.’ That’s what I finally did when I had the lung thing. I just put it out there, and I said, ‘Has anyone had this? What’s the success?’ Because, for me, it was always a moment of getting really scared if anything happened in my lungs.
When that happened, I was like, “Oh no, is this it.” I got so much reassurance once I put that out there, and I had so many responses from the people that are doing what you guys are doing, The Patient Story.
It’s shining the light on those dark areas, so be open to reaching out to people. You’re not burdening anyone who has been through this by asking questions.
Once we’ve gone through this, you get that feeling of, ‘I want to help. I want to help as many people as I can.’
If I could give any advice, it’s to find your support group, because your support group really is what helps you get through those hard days.

Inspired by Lindsay's story?
Share your story, too!
Colon Cancer Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)