Nick’s Stage 3-4 Marginal Zone Lymphoma Story

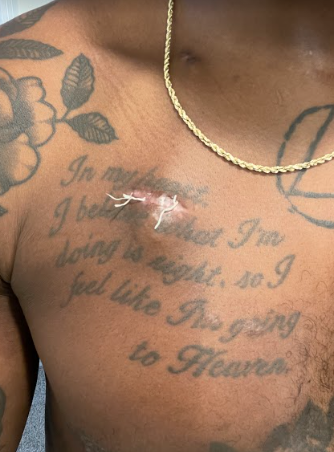
Nick has persevered through a series of health challenges. After 13 months of self-advocating, he received a diagnosis of IgG4-RD, a rare autoimmune disorder. Then 7 years later, it morphed into nodal marginal zone lymphoma.
Nick shares his story, which includes undergoing treatment twice, setting an example for his 3 young children, and turning pain into passion
Thank you for sharing your story, Nick!
- Name: Nick Mundy
- 1st Symptoms:
- Daily hives
- GI issues
- Weight loss
- Heart issues
- Night sweats
- Diagnosis:
- 2014: IgG4-RD
- 2021: Nodal marginal zone lymphoma
- Subtype of non-Hodgkin’s lymphoma
- Stage 3-4
- Treatment:
- Rituxan (rituximab) infusion
- High-dose steroids
- Introduction
- The IgG4-RD Diagnosis
- Receiving the diagnosis
- Being treated as lymphoma
- How did it feel receiving the diagnosis after 13 months?
- What was it like trying to get a diagnosis for 13 months?
- Did you feel like people didn't believe you?
- Advocating for yourself
- Frustration and hopelessness
- What did the Mayo Clinic oncologist say to you when you said, "What if I had listened?"
- IgG4-RD Treatment
- Marginal Zone Lymphoma Diagnosis
- Processing the Diagnosis
- Treatment and Side Effects
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Introduction
Tell me about yourself
I’m a family man. I am fanatical about personal growth and maximizing my humanly potential. I fortunately understand that my time here is limited, and it’s not guaranteed.
I’m somebody who tries to make the most out of every moment, every interaction, every day. I try to win the day. If I’m blessed with more time, eventually those days turn into weeks that I’ve won, and hopefully months. I try to positively create as much momentum as I possibly can.
Another thing is that I try to do it in a manner that inspires others to do the same. People want to know why you are moving the way you are, or why you carry yourself the way that you do. [It’s] so that I can open up and share a little bit of my story and my journey to hopefully positively impact that person and to leave them better than when I found them.
I’m absolutely fanatical about life and about my time here. I want to do something amazing with that time, and I want to impact as many lives as I possibly can.
I am a husband. My wife’s name is Shelby. We have been together since December of 2012. [We’ve been] married since February 22nd, 2016. That’s 6 years.
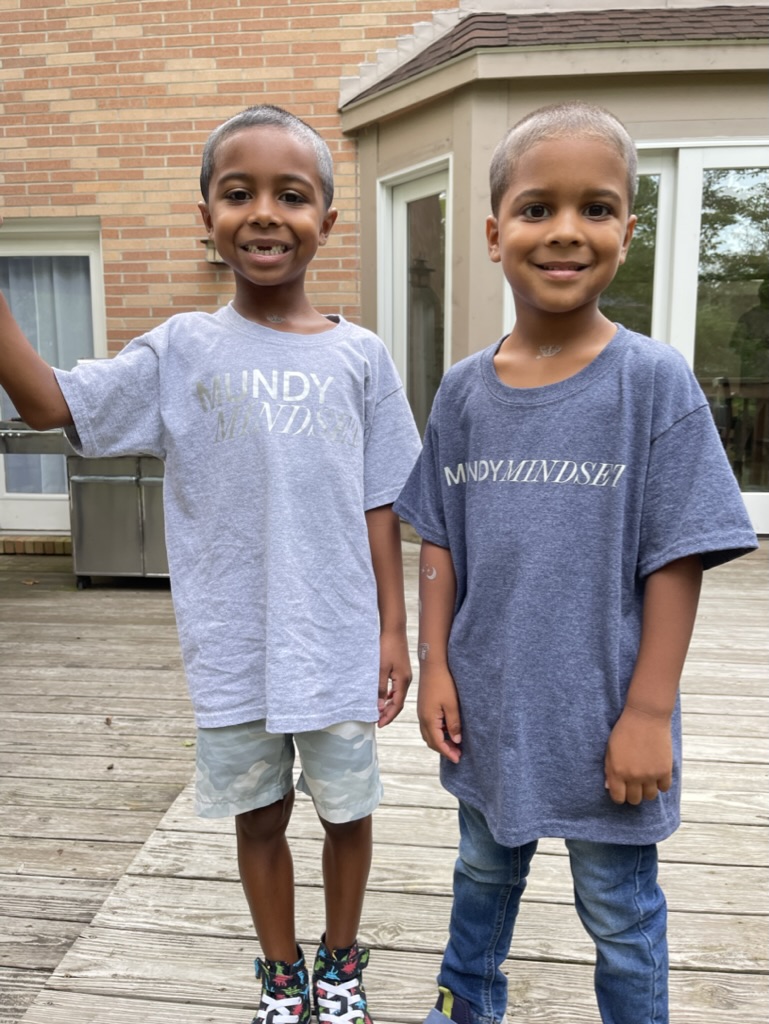
We’ve got 3 amazing boys. We have twins that are 5, and then we have a 7-year-old as well. She’s a boy mom; [I’m a] boy dad. It’s never a dull moment around here. They keep us on our toes. We always tell people we’re playing zone defense, so it’s very interesting around our family’s household.
Can you summarize why you went to the doctor years before you were diagnosed with cancer?
[Shelby and I] had only been together for 6 months, and then one night I had some symptoms that drove us to the hospital. [I] had to show some humility and ask my girlfriend at the time to take me to the hospital because I wasn’t feeling well.
‘I shouldn’t have to do this. I’m the victim here. I’m the patient.’ Yet that mentality doesn’t get you very far in this game.



Throughout a series of tests and CT scans, the doctors found that I had an enlarged prostate, but also an enlarged heart that they claimed was an athlete’s heart at that time, which can be common in young African American men. But this was something they were pretty serious about. They told me not to play any more basketball, to cease physical activity and to go see my doctor as soon as I made it back home to Cincinnati.
As soon as I got back into town after that weekend, my visits with the doctor began. They became more and more prevalent. Shelby accompanied me through a lot of those appointments for the next 13 months.






Knowing something’s not right but not getting answers
There was a lot of confusion, and I’d say a lot of anger as well. Some sadness. Over the course of 13 months, I lost about 49 pounds. I had 3 different biopsies and 2 different bone marrow biopsies. I had all types of ailments and infections or illnesses along the way that caused me pretty uncomfortable pains.
It was a long journey. To be told that “we don’t know” or “we’re not sure” or to get placed on the back burner was extremely difficult. I had to learn to advocate for myself and to advocate for my own health.



I had to call a lot of doctors back. I had to schedule a lot of tests. I had to call and inquire on a lot of different results and blood work and make sure that blood work and those results or scans were picked up by me and taken to another doctor.
When you’re going through it, you feel like, “I shouldn’t have to do this. I’m the victim here. I’m the patient.” Yet that mentality doesn’t get you very far in this game. Unfortunately, it can lead to death or even way worse, worsening of your symptoms or illness that you currently have.
Intuitively, I knew that I needed to advocate for myself, but without Shelby, my mom, my dad, and having some great support around me, I don’t know that I would have continued to seek the help that eventually got me to the Mayo Clinic.
»MORE: How to be a self-advocate as a patient






The importance of a support system
It’s crucial. I even tried to push away Shelby, my girlfriend at the time, because we were so young. I was 23 when I first got sick. She was only 22. You fast forward a year of sitting in doctor’s offices and having so many heartbreaks and ups and downs.
I just thought, “You got to go. You should leave. You don’t deserve this. We don’t deserve this. We’re kids. I don’t enjoy sitting in these doctor’s offices or appointments or waiting rooms, and I know that you don’t. I know that you can’t.” That was never even an option for her. She never even thought twice about it.
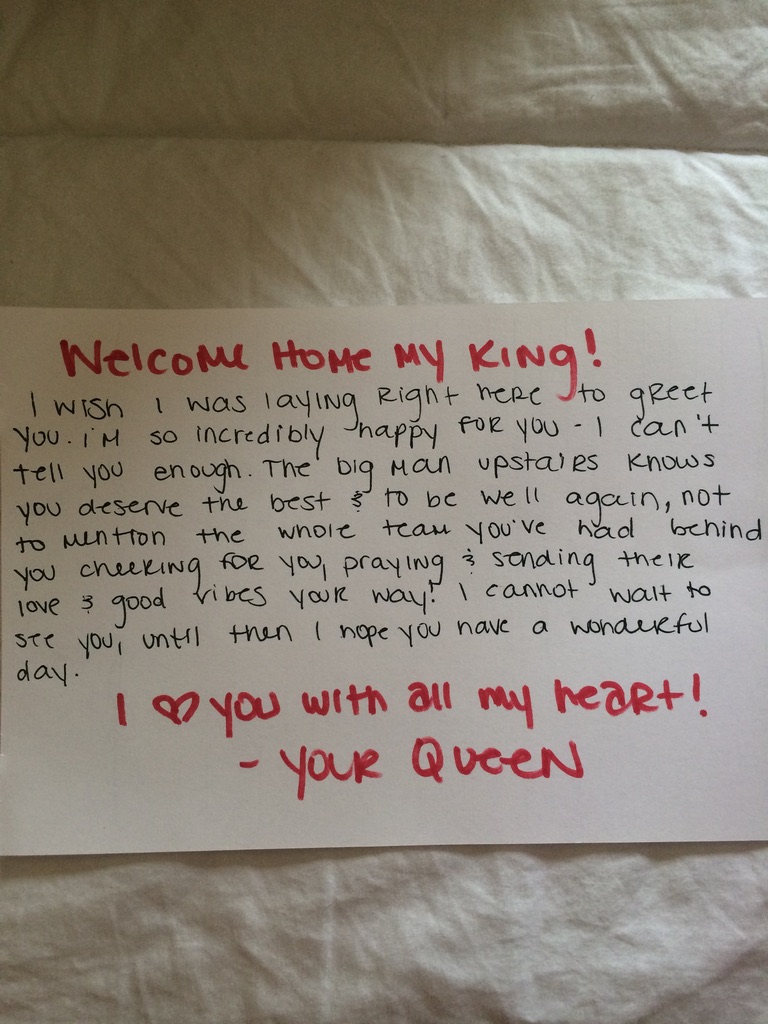

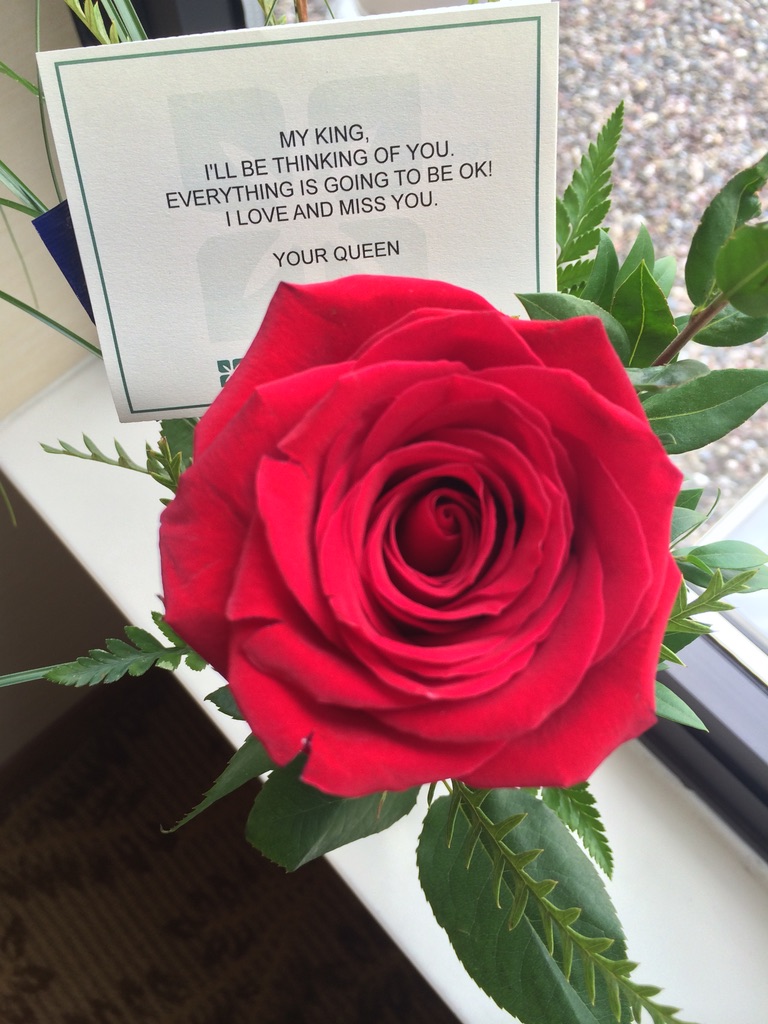
When she told my aunt, she was like, “That’s my man,” and she stuck beside me. My aunt even asked her at one point, “Why are you still with him as he’s going through all this?” And she was like, “Because he’s my man.” She really stuck beside me throughout all of it.
The IgG4-RD Diagnosis
Receiving the diagnosis
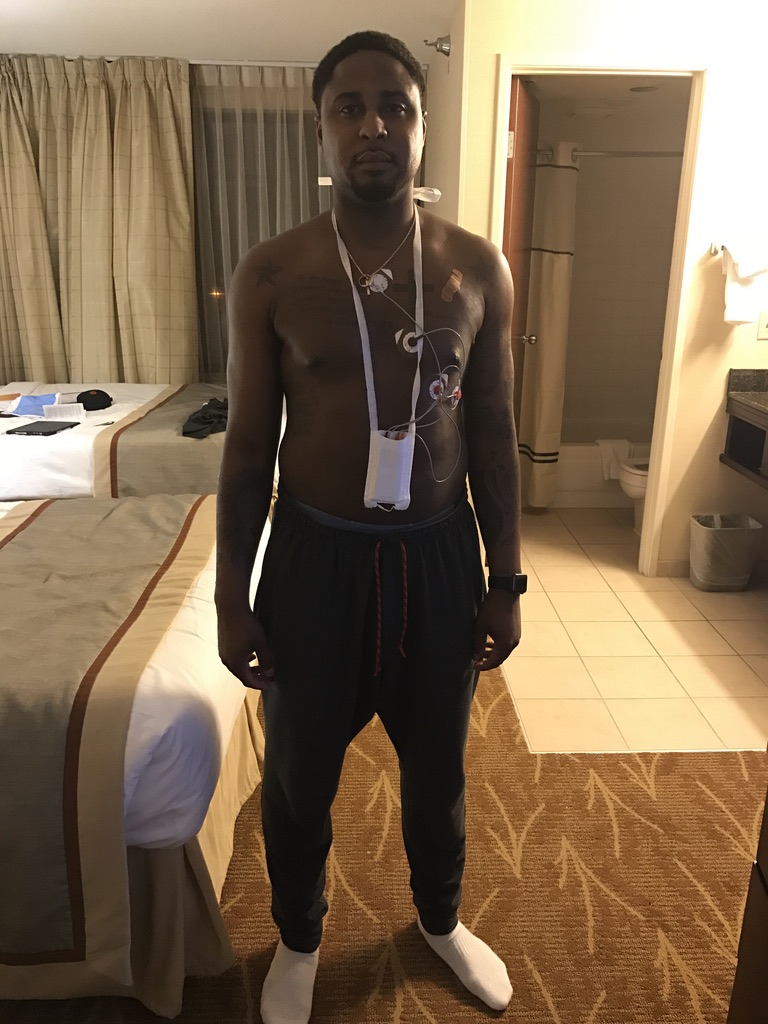
The local hospital said it might be lymphoma, and Nick went to the Mayo Clinic. There, he underwent a bone marrow biopsy and full body plasma transfusions.
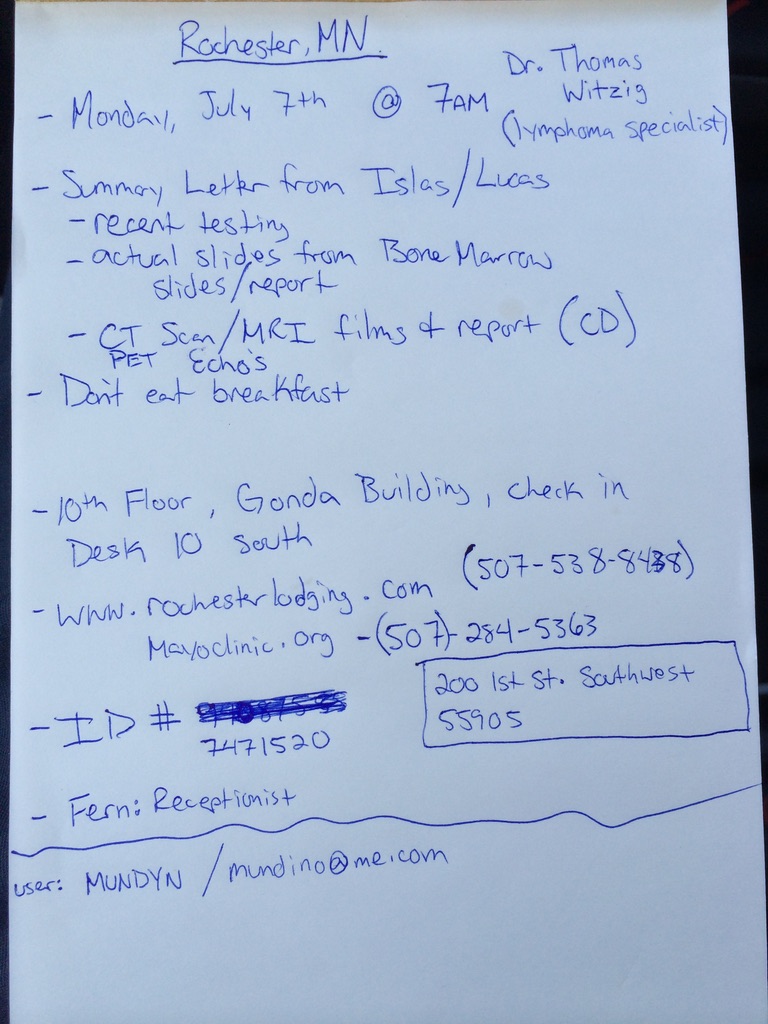
I got to the Mayo Clinic, and I’m very fortunate that I got in. Throughout my journey, I understand that a lot of people will try to get in with whatever illness that they may have, and not everybody is accepted.
I feel very fortunate to have been accepted into the clinic, especially when I was. We were pretty much at a dead end and didn’t have any answers. Nobody wanted to treat me for a partial diagnosis of an unnamed type of lymphoma.


When I got there and had all of the tests and all of the procedures done that you just mentioned, it took about 2 weeks. Then I finally got a diagnosis of IgG4-RD. Then they called it a pseudolymphoma.
They started diagnosing this disease at around 1998, I believe my oncologist told me. So very, very rare and new. I believe he only had one other patient other than me at the time that he had ever seen this in. I was the youngest patient he had ever had, especially with it in their heart, and then also manifesting in the lymphatic system as well. It really threw them for a loop.
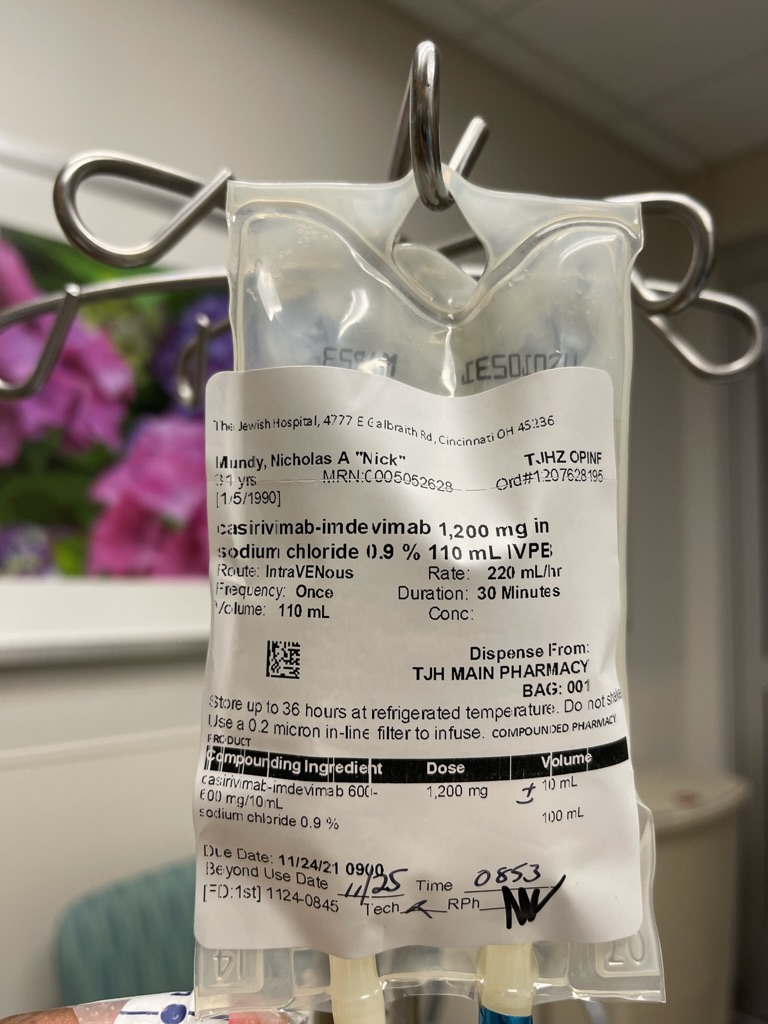
Being treated as lymphoma
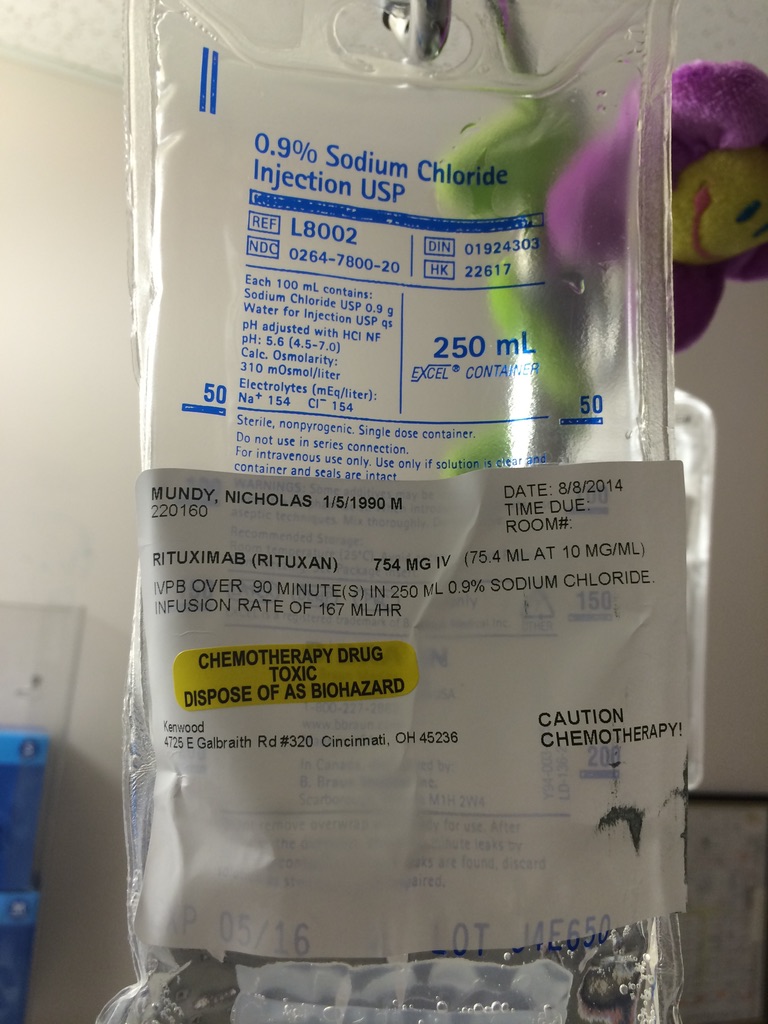
It wasn’t technically a lymphoma, but they treated it as a lymphoma. They put me on a Rituxan (rituximab) procedure and then also high doses of steroids to treat it in the same way that they would a low-grade lymphoma. The lymph nodes in my neck were massive and almost like golf balls on both sides.
When I returned to Cincinnati, Ohio, I began going to chemotherapy (at the age of 24 in August 2014) every week for a month to get this medicine.



How did it feel receiving the diagnosis after 13 months?
It was extremely relieving. When I came out of my heart surgery, I was surrounded by doctors of different nationalities. I want to say there were 8 to 10 people in the room. Everyone kept apologizing and saying, “I’m sorry.”
They let me know right away, “You were the interesting case. You may never want to be the interesting case, but we’re here for you. We’re all going to be looking at your case moving forward.”
Fast forward a couple of weeks. To even have a diagnosis was a relief. It didn’t feel great to tell me that it was almost like the chances of hitting the lottery or that “you should go buy some scratch offs.”
At the end of the day, I was just fortunate. I was grateful to have an answer so that I could at least begin taking some action. Every doctor’s appointment that I left prior to that, I left with question marks of the unknown. Honestly, with the way that I was headed and the way that my body was deteriorating, I had really come to grips with the thought that I wasn’t going to make it much longer.



What was it like trying to get a diagnosis for 13 months?
Being asked by so many others that care about you, and then for you to have to articulate, “I don’t know.” Then people that care about you want to know, “Why don’t you know? What don’t they know?” It was extremely frustrating, but mainly the feelings of hopelessness and despair started to set in.
At first, you’ve still got some energy, and I’d say you’re still pretty hopeful. You continue to have doors shut, and people tell you, “Hey, we don’t know.” You’re talking about your life. Then you’re also on the other side, physically deteriorating away. Every time you go to the doctor, you weigh less or you’ve got something else coming up.
Maybe subconsciously, that’s why I had asked Shelby to maybe leave as well. I didn’t feel great about what the future held if I were to stay on the same trajectory that I was when I was going through all of these doctor’s visits for 13 months.


Quite sad and very scary, to be honest. Scary because as a young man — I think most young people in general — I felt invincible, almost indestructible. I had never really thought about my own mortality. I had never really thought I’d have to face that at such a young age. No one really prepares you for that, and so I dealt with it in the best way that I possibly could.
There were definitely some unhealthy ways of numbing — trying to compartmentalize, utilizing some of the medication that I was given, or drinking excessively to try to push those feelings down so that I wouldn’t have to deal with them. It was just extremely scary. I wasn’t sure how to talk about it, and I wasn’t sure who to talk to. [There was] a lot of hopelessness.

Did you feel like people didn’t believe you?
Yeah, absolutely. There was one specific doctor that I went to. It was an infectious disease doctor. I actually will never forget this. I was actually thinking about it this morning, wondering if this would come up.
I drove a work vehicle way out of my territory, where I was supposed to be for the day, to downtown University of Cincinnati’s campus. My mom and my dad met me there actually, because at this point, I had lost a lot of weight. I had a lot of different symptoms and had been to many different doctor’s appointments that had no answers, so we had been referred to an infectious disease doctor.
At this infectious disease doctor, I want to say he took almost 30 vials of blood to test for all types of different [things]. It was the most that I’ve ever had taken just for testing. But at this point, we were all just like, “Anything that you can tell us, please let us know.”
We were very hopeful going into it that maybe this infectious disease doctor would be able to tell us what was going on with me and why I was having all of these symptoms: the night sweats, the weight loss, the fatigue. [I] gave him the blood and gave him the symptoms. I never heard anything back.

Advocating for yourself
The advocating for myself came into play. I called in twice. After calling in twice — and I’m saying over the course of a couple of weeks, calling in multiple different times — I was finally able to get a return. His partner’s physician’s assistant reached back out to me and told me that the doctor had thought that I had breathed in some sort of bacterial compound from the ground.
They were doing a new driveway and putting in some new parking in the neighborhood that I lived in at the time. We told him there was some excavation going on. His response to all of this stuff that they had taken from me was, “Oh, well, he’s breathed in more than likely some sort of spores or bacterial infection that he’s gotten from the excavation that’s happening around the house. If you continue to keep him on Benadryl and some over-the-counter medicine and some antibiotics, he should be good to go.”



Frustration and hopelessness
That was really frustrating to me because I had never had anybody take so much from me. There was a lot of time that went in between there. Then also no call, no follow-up.
A lot of that hopefulness, and this is where that hopelessness kind of started to come in. This was my last-ditch effort after seeing oncologists and all types of different doctors before and not having anything.
This to me almost said, “Oh, this doctor doesn’t actually think I’m going through some of the things that I’m going through.” It almost felt like it was just, “Pick something out of a hat and tell them this is what it is.”


I was pretty frustrated. I remember asking my oncologist at the Mayo Clinic months later, “What if I would have listened to that person? What if I would have listened and stopped there and gave up, because that’s what I chose to listen to?” It just didn’t sit well with me.
As we’ve mentioned many times before, you have to continue to press on. If you don’t feel a certain way or if you know that there’s something else going on with you, you’ve got to continue to search for answers.
That’s where your support system can come into play majorly. You may be out of energy and you may be exhausted, and that’s where you’ve got to be able to lean on your support system to help you to make sense of everything that’s going on in your world right then.


What did the Mayo Clinic oncologist say to you when you said, “What if I had listened?”
That was my biggest question. What would I have done if I would have listened to this doctor? Then also, what do people do that don’t have health insurance? It cost me a lot to get there, and I had great insurance with the company that I had worked for.
The answer, I believe, is that you wouldn’t be here. You would have more than likely died. People that inherited this autoimmune disease in the past that have gotten this more likely than not have not had the means of going through all of the different doctors, oncology specialists, hematology specialists, PET scans and the CT scans to actually identify what it is that they’re dealing with.
[I] felt very fortunate, but also very sad because I can’t be the only one. I know that the odds look like that on paper here today, but I know there’s got to be other cases out there. We just don’t know.


IgG4-RD Treatment
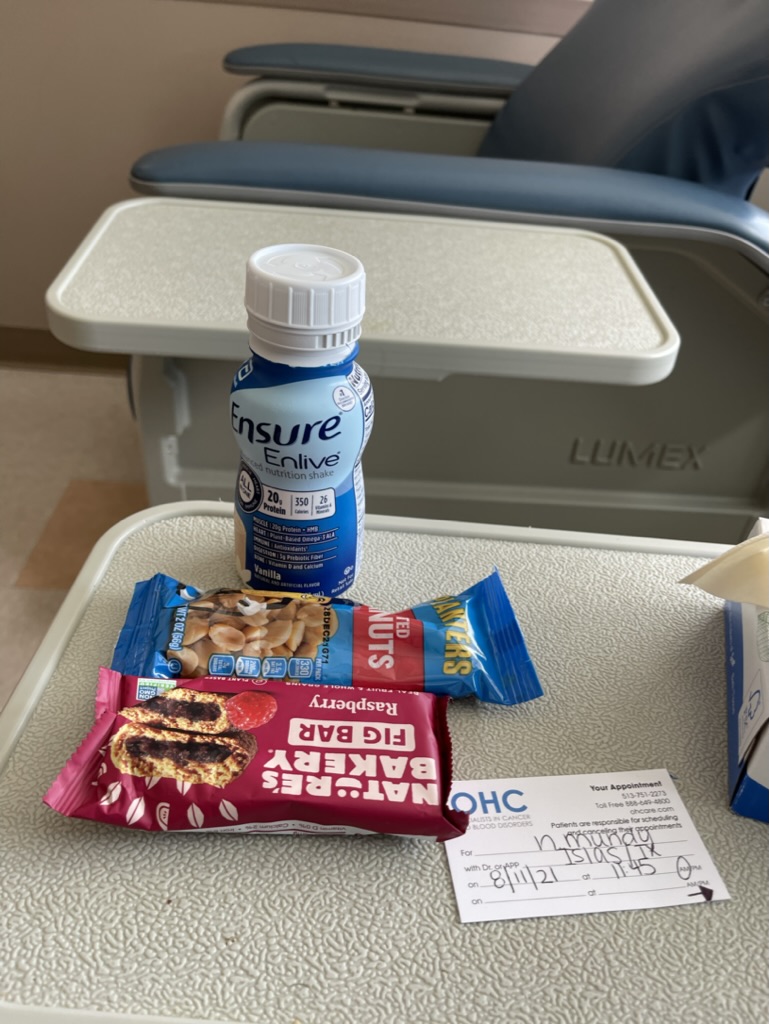
How long did you go through treatment?
Rituximab and steroids every 2 months, then eventually every 9 months.
From August of 2014, all the way until my last treatment [around] December 2019.
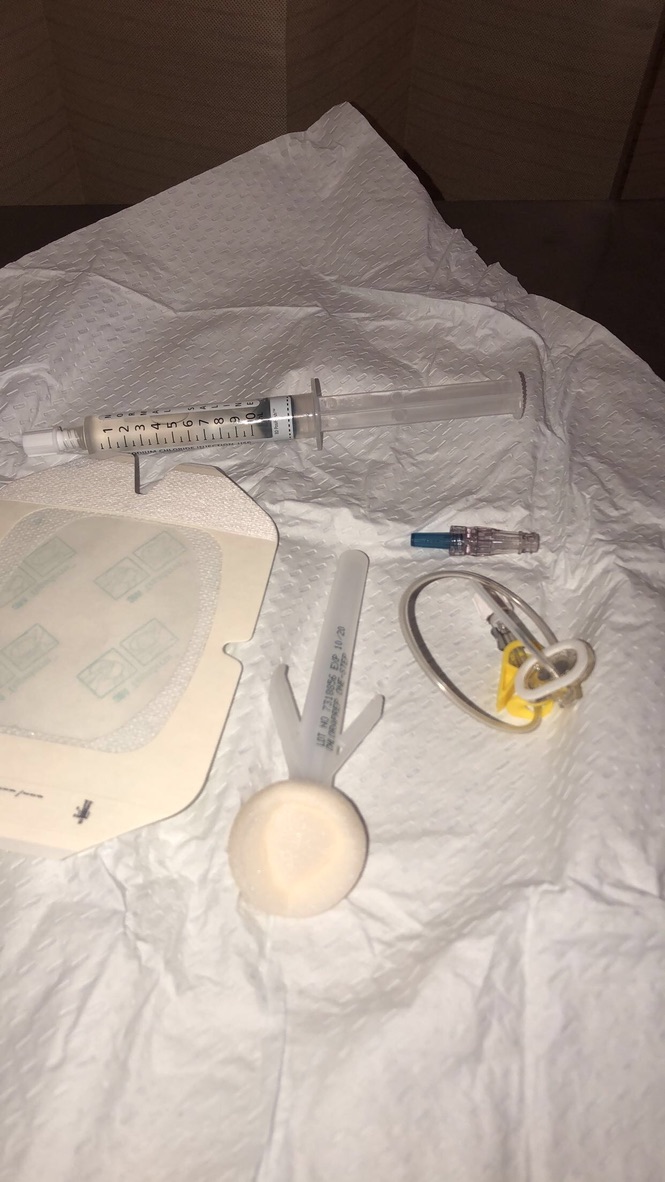
I got a port put in originally in August of 2014 from my autoimmune disease and for going to chemotherapy. Then we got to a point where I was only going twice a year, so my oncologist at the Mayo Clinic was more than on board with me getting my port removed.
To me, that was more of a mental victory because it didn’t cause me any physical pain or issues. But it was that reminder of having this thing that I had to go get flushed regularly. I wasn’t not even coming in here that often anymore. I was like, “Maybe we could get it out, and I could get a little mental victory for once.”
They were like, “Absolutely.” [I] got the port taken out. I went to chemotherapy and worked throughout my whole career, pretty much from August 2014, all the way up until December 2019.
»MORE: Patients talk about working during cancer treatment



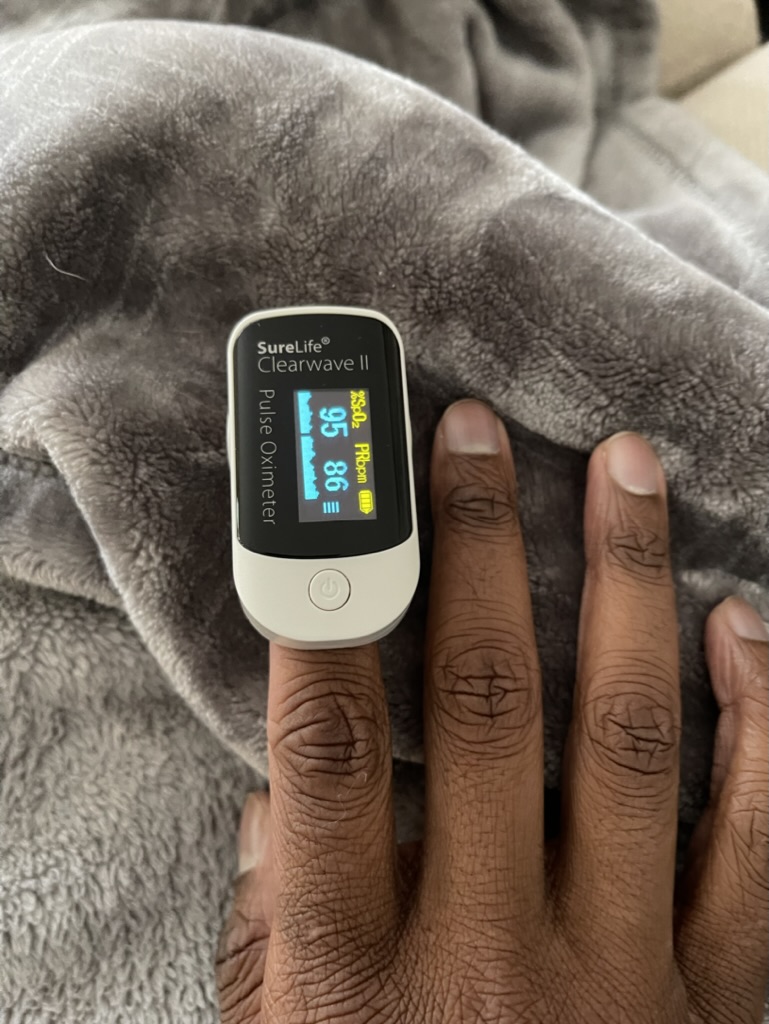
Your treatment stopped during the COVID pandemic. How did you feel during that time?
There was a lot of confusion around, “How am I going to get to the clinic? Is it safe to get to the [Mayo] Clinic?” Flights weren’t very prevalent at the time. I was supposed to get chemotherapy at a 9-month mark and wasn’t able to work that out between insurance and logistics and everything.
I actually ended up going about a year without chemotherapy. No tests, no scans during that time. During that time, I felt pretty good. I felt relatively healthy. During that time, I took more ownership than I ever had in the past.



In the past, I really just was kind of just following all of my doctor’s orders and doing the bare minimum, if I’m being honest, and doing what they told me to do. If they told me to be at chemo on this time, this date, that’s what I did. I showed up that time, that date.
Then outside of that, I didn’t do anything in my own power to put more distance between myself and my autoimmune disease, or to put more distance between myself and heart disease. I had what I call a wake-up call. [I believe] the universe was kind of preparing me for the journey that I had ahead.

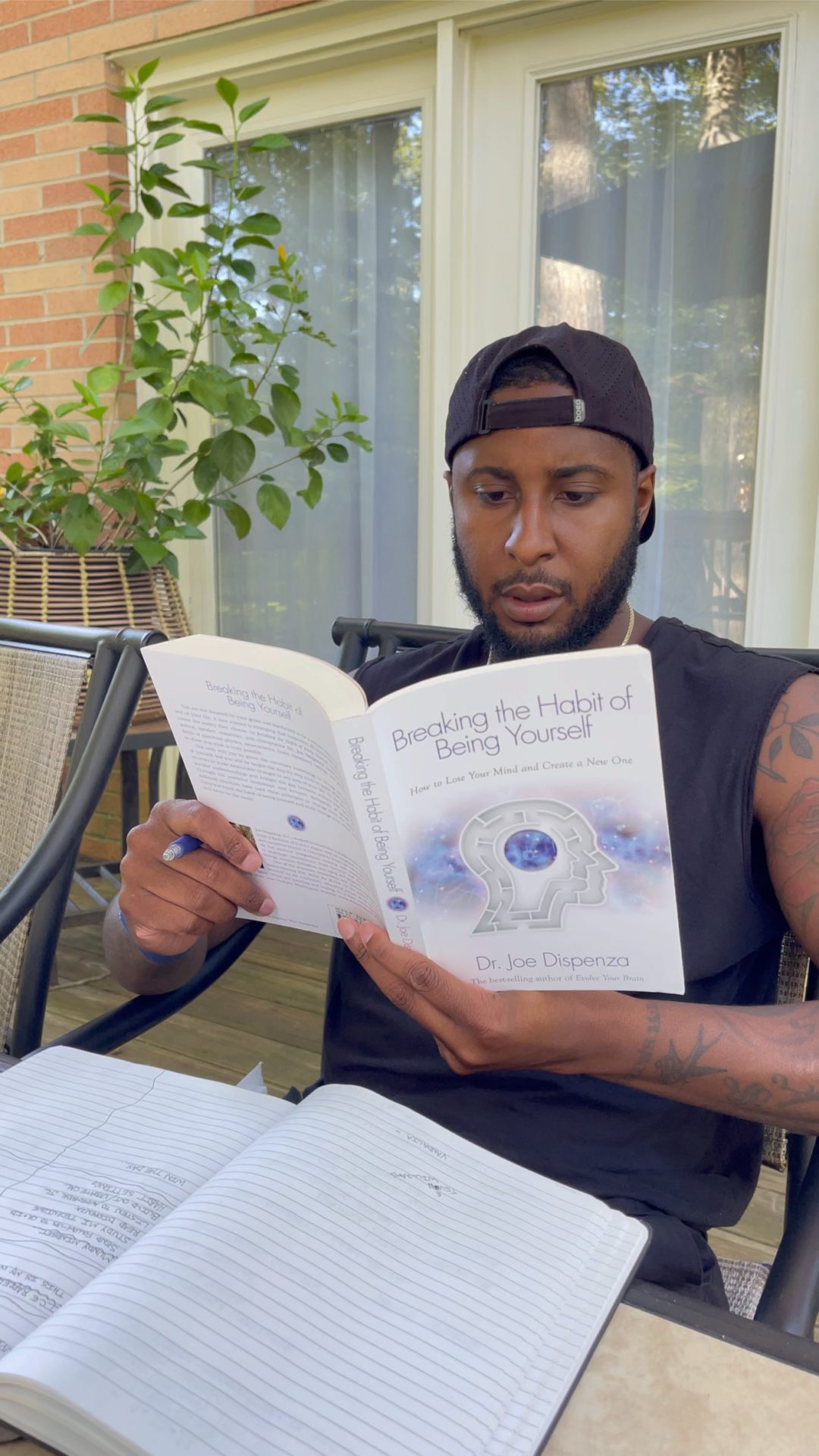
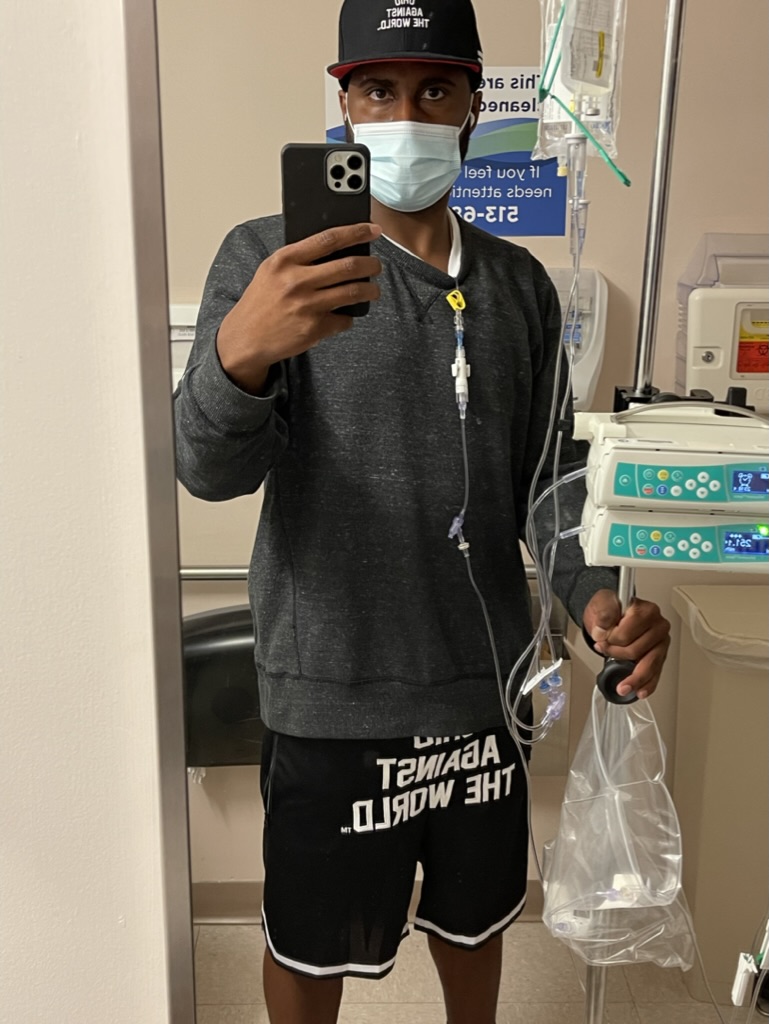
Symptoms returning
In August of 2020, I started working out more. I started to really prioritize my holistic health, focusing on physically improving, mentally improving, emotionally improving and spiritually improving. During this time, I was feeling good.
I lost some excess weight that I had put on from years of taking steroids and eating whatever I wanted. That probably stemmed from all of those years of being really skinny and losing a lot. I just started eating whatever I wanted, and then I really ballooned for a while. This was the first time where I was like, “I’m taking control, and I feel good.”

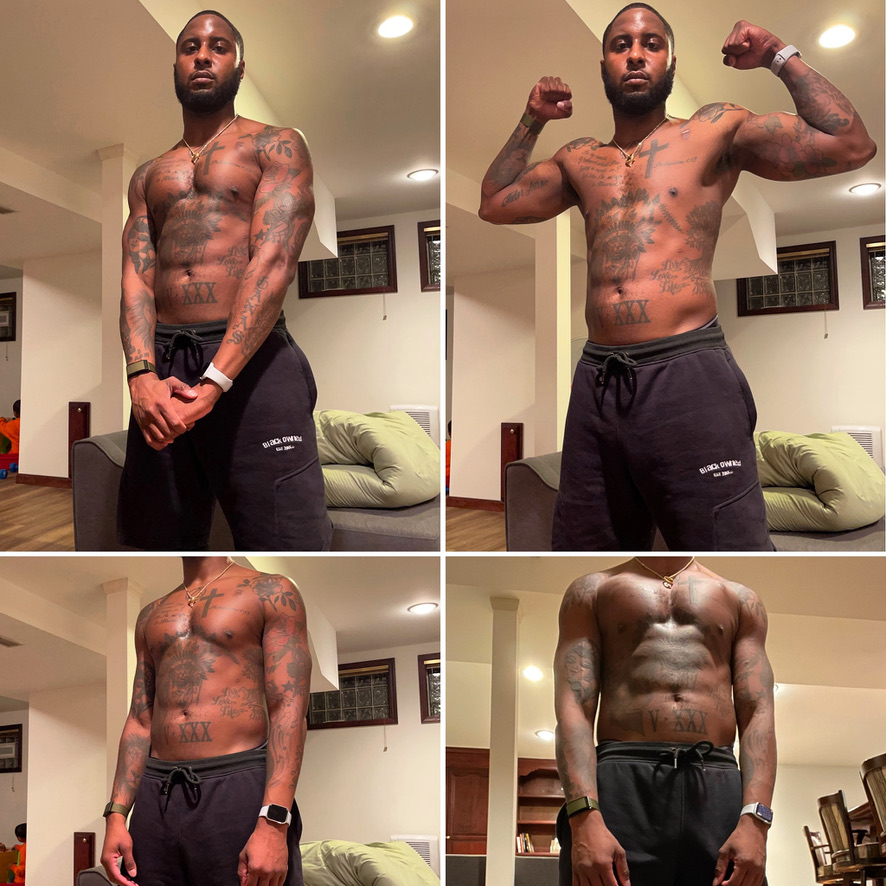

It was probably around October 2020, and I started having night sweats again. Maybe I wanted to look past it or wanted to overlook it and didn’t want to really say, “Oh, man, maybe I got something going on again,” because I felt so good in all of the other areas. I looked good in the mirror for the first time in so long.
I was like, “Man, it can’t be that big of a deal. This might just be something else.” I kind of just swept it under the rug and then went and got a PET scan in December of 2020. That’s when there was another thing that took a left.
Marginal Zone Lymphoma Diagnosis
What was it like when you got your PET scan?
I went into my PET scan. Actually, it wasn’t in the hospital. They had a trailer that they were using, a mobile PET scan office that was right outside the hospital. The technician had a partner with her. She was super sweet, and she was asking me some questions. She was walking me outside into the trailer to get all set up.
You have to make sure you sit still and quiet for a while. But prior to that, they wanted to know what my story was. Why was I here? “You’re too young to be here.” If I had a dollar for every time someone told me I was too young to be here or to be going through this, I’d be rich.
I explained. I had told them about my history as a young man, and they were like, “Oh, wow, you look so good. You’re a fighter. Everything is going to be good. We just know it.”
I was like, “Absolutely.” I hadn’t been in better shape. I was ecstatic. I was like, “Let’s do this scan.”

After the scan
When I left the scan, that energy wasn’t in the room. I wasn’t sure if it was because it was raining, but it was raining when I went in. I just kind of had this feeling. I wondered what they saw. Because I’d been through so many of these things and getting cardiac MRIs or echocardiograms, I wanted to ask some questions. They were like, “I can’t really tell you.”
I don’t try to pry too much out of my technicians anymore. I could just tell that things were different. They wished me the best, but the lady’s face changed completely. It was more like my caring mother or caring motherly friend at this point.



But once again, [I was] in denial, just like the same with the night sweats. I was like, “Huh, I’m feeling good. I feel like I’m winning, so I’m going to sweep it under the rug again and keep it moving.” Plus, I had really done a lot to ground myself in remaining objective [with] neutral thinking.
In the past, I had done so much living in the future and worrying about, “What am I going to do if this happens, or what am I going to do if they say this or if my oncologist says I have this? Well, what am I going to think about that?”
That caused so much anxiety. At that point in my life, I wasn’t doing that anymore. I was like, “Hey, the facts are: I feel good, I just took a PET scan, and that’s all I know.” That’s where I left it.
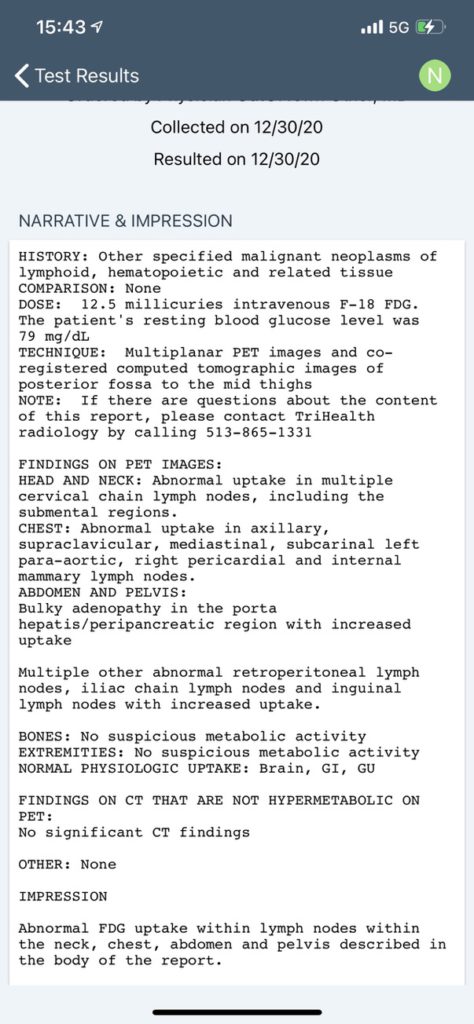
Receiving the PET scan results
Because everything is so smart nowadays on the phone, nobody called. I got the results in the palm of my hand on my summary report. [It] said findings: abnormal, abnormal. abnormal, abnormal. The denial at this point was like, “Okay. Something’s definitely off, but I’m not sure what it is.”
I didn’t want to go Google all of these big words on here, give myself my death certificate, and punch my stamp here today before I even heard from a professional. I tried to ground myself. I tried to pick up the phone and call to see if I could get an appointment to review the results with my local oncologist.
Then I also called my oncologist at the Mayo Clinic, because the oncologist at the Mayo Clinic was ultimately the one who had asked me during my last treatment way back at the Mayo to get a PET scan the next time I got to the doctor. [I] sent the information over and was hoping for a professional opinion, but I knew that it wasn’t good with the word “abnormal” capitalized multiple times throughout this report.
What happened when your oncologist at the Mayo Clinic called?
I was at work. I was training a couple of new hires, and I had a telehealth appointment with my Mayo Clinic oncologist.
He said, “Nick, it looks like you’ve got some type of cancer, and it’s spreading throughout pretty much a good portion of your body. I need you to get up here immediately so that we can do a biopsy and figure out what’s going on. We need to figure out if this is your IgG4 resurging, or we need to figure out what is happening here. How soon can you get to the Mayo Clinic in Rochester, Minnesota?”
At that moment, that’s when I knew things were real. Leading up to that call, I knew that it was only a matter of time before we had to get back into the fight mode. I had already kind of readied myself a little bit.
I had even told the people at work, “Hey, I have a feeling I’m not going to be here in a few weeks. I’m going to have some tests. I’m going to have some things that are going to come up.”
I’ve been through this before, and I wanted to prep. I was in a leadership position at this time with direct reports, and I wanted to make sure everyone else was taken care of. I didn’t want them to see me sweating. This time now, I had 3 kids and a lot more to lose.
Leaning on support
I was rocked, but also I knew I had a great support system. My mom started going to the Mayo Clinic with me for my original visit and was really my road partner for the majority of my trips, up until I was at that point where I was going only once or twice a year and was doing pretty well.
I called her and said, “It looks like we have to get out the Mayo Clinic clothes again. Get the hoodie and stuff, some of the souvenirs we bought thinking we weren’t going back. I think we need to go back.”



What was the impact of the word “cancer”?
I was just in disbelief. I had heard “lymphoma” so many times before, but [with] the pseudolymphoma, I almost felt like I didn’t really fit in a box anywhere. I didn’t fit in the cancer survivor group exactly, because I didn’t have a cancer diagnosis. There was nobody else in my little interesting case group over here. I was a little bit scared once again.
Also, I just remained grounded in the fact that I wasn’t sure exactly what I was dealing with just yet. I wanted to wait and to really understand what kind of cancer and what the protocol looks like. I knew that my oncologist was going to be extremely thorough, as he always is, to give me that information.
I was scared, and I just wasn’t sure what that fight was going to look like just yet. Honestly, I kind of assumed that it would be similar to whatever I had gone through in the past. [I was] just thinking, “If I’ve gone through it once before, I could probably get through it again.”



Did your autoimmune disease turn into lymphoma?
Yes. As I mentioned before, my oncologist started diagnosing the IgG4 autoimmune disease in 1998 and had only had 2 patients really, including me. He had told me about several conventions that he had gone to. I think he found one other person that was being treated in Japan for something similar.
The way he explained it to me was, “You already have a remarkable case, but you are the first person that I have ever treated that had IgG4 where your autoimmune disease mutated into a full-blown lymphoma.” Those were his words.
My autoimmune disease had mutated into a full-blown cancer, into a lymphoma. They staged me 3 through 4, meaning it was on both sides, throughout my entire diaphragm, had made its way into part of my liver, and then was starting to make its way into my bone marrow.



Processing the Diagnosis
What did hearing that feel like?
My doctor is very open, very honest and straightforward. He explained to me once again the odds of the autoimmune disease, but then he also explained the rarity of the type of cancer that I had, which ended up [being] nodal marginal zone. He said that accounted for almost only 2% of the types of non-Hodgkin’s lymphoma that they see. Nodal marginal zone is pretty rare.
He did say that if caught early and especially if somebody is healthy — relatively, with everything else going on — that he did feel optimistic that we could treat it and get it to go away.
But he was very honest and upfront, letting me know that for being as young as I was (I was 31 at that time) and having had the history that I had had over the course of the last 8 years since I was 23, with lymphatic diseases and issues, that there’s a good chance that it may come back again at some point. This could be something that I deal with for a while.
Just very open, very honest, straightforward. Oncologists and doctors don’t win any prizes for making you get the warm and fuzzies and feel good about everything, but it was what I needed to know. [It was] what I needed to hear. Once again, you would think that I just took him at his word and everything, but I even saw another oncologist back home. [It was] just to make sure that the treatment plan and everything else that my oncologist at the Mayo Clinic had rolled out was what she thought as well.
»MORE: Patients share how they processed a cancer diagnosis
Getting a second opinion
Dr. Cynthia Chu, my neighbor, is a 3-time survivor of cancer, and she’s had non-Hodgkin’s lymphoma before. This doctor here locally treated her for it, and they just absolutely raved about her. Honestly, if they hadn’t spoken so highly of her, I probably would have never gone to see her.
I went and saw her as well. She was extremely direct with me and let me know the staging right off the bat, whereas I had to ask my other oncologist what stage. I think that probably goes into us working together for so long, and maybe they didn’t want to scare me. I’m not sure. She was very direct with me and told me exactly what I was dealing with.
She also let me know that the standard of care that I was getting was the top of the line for the time my cancer was diagnosed and how they were treating lymphomas. She said, “It is the standard of care; it is the best care. I would treat you if you needed me to, but where you’re getting your treatment is the best place that you could possibly go.”
That reassured me. “Okay. The facts are the facts, and now we’ve got to get to work.”



What emotionally, psychologically and spiritually propelled you forward?
Setting an example for your children
What propelled me forward was knowing that I have 3 boys. I’m sure that the statistics have changed, but I believe the last time I heard [it was] that 1 in 3 people is going to live with or fight cancer at some point in their life.
It’s very easy for me to look at my 3 boys, just do that math pretty quickly, and understand that the facts say that one of them may inherit cancer or go through this at some point in their life.
They’re looking at my ancestry and my medical history. Cancer runs in my family. For me, that was not an opportunity to stop, but more of an opportunity to lean in. I’m big on leadership, leading from the front, leading by example, and hopefully providing an example for my boys to see what we do when life happens.
When things get hard, what do we do? When we face challenges, what do we do? They’re going to ultimately learn that through the examples that they see and the people that they surround themselves with.
That was something that I took to heart very seriously. I had an opportunity to not only better myself, but to provide an amazing example of what it looks like to fight, what it looks like to prioritize yourself, and to not be defined by your circumstances. [Instead] rise above a tough situation and then make the most out of the hand that you’re dealt. That was a big motivating factor for me.
»MORE: Parents describe how they handled cancer with their kids



Not my time yet
Then also, I just didn’t believe that it was my time. I felt that I had so much positive momentum going. Like I said, I had this wake-up call before I had gotten sick. I just asked myself, “What am I doing to raise my own personal stock price in this world? What am I doing? How much have I invested in my own self?” And I hadn’t invested much.
That was when I went on my spiritual, emotional, mental and physical journey. Like I said, when I got the diagnosis, my physical [condition] was almost removed immediately through the hospitalizations, the weakness and the starting of the chemotherapy. I knew that there was something bigger at play here, because these were things that I wasn’t even thinking about necessarily a year ago.
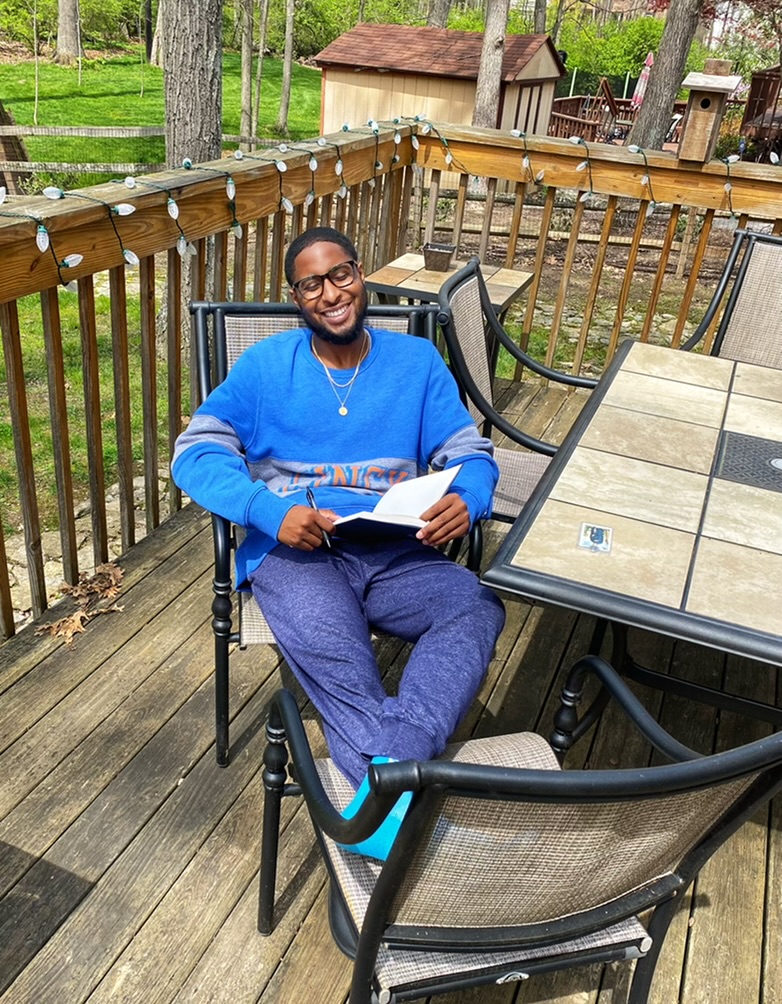
Now, as a result of having this foundation of a holistic wellness picture, I was able to say, “Physically, I may not be able to do as much as I was able to do 2 months ago. I may not be able to run as much or do as many pushups or any of those things. But I do have a great foundation for the emotional intelligence things that I can work on. I can still work on my emotional intelligence. I can still work on that. I can still read. I can still consume as much knowledge as I possibly can, then apply that knowledge to make my life as meaningful and fulfilling as I possibly can. Then spiritually, I’ve got a great opportunity here.”
Using it as an opportunity
That’s how I looked at it. It was to really see, “Are you really about the things that you say that you’re about?” [It was a chance] for me to lean in and to really do the work and roll up my sleeves, just like I had gotten down and done physically. I was like, “Okay, well, now this is an opportunity for me to really work on these other tools and make those just as strong as my physica [tools].”
That was the motivating factor for me. I had this feeling that my time wasn’t up, but almost more like I was kind of being tested on how much I can endure. Also, what am I going to do when life hits?

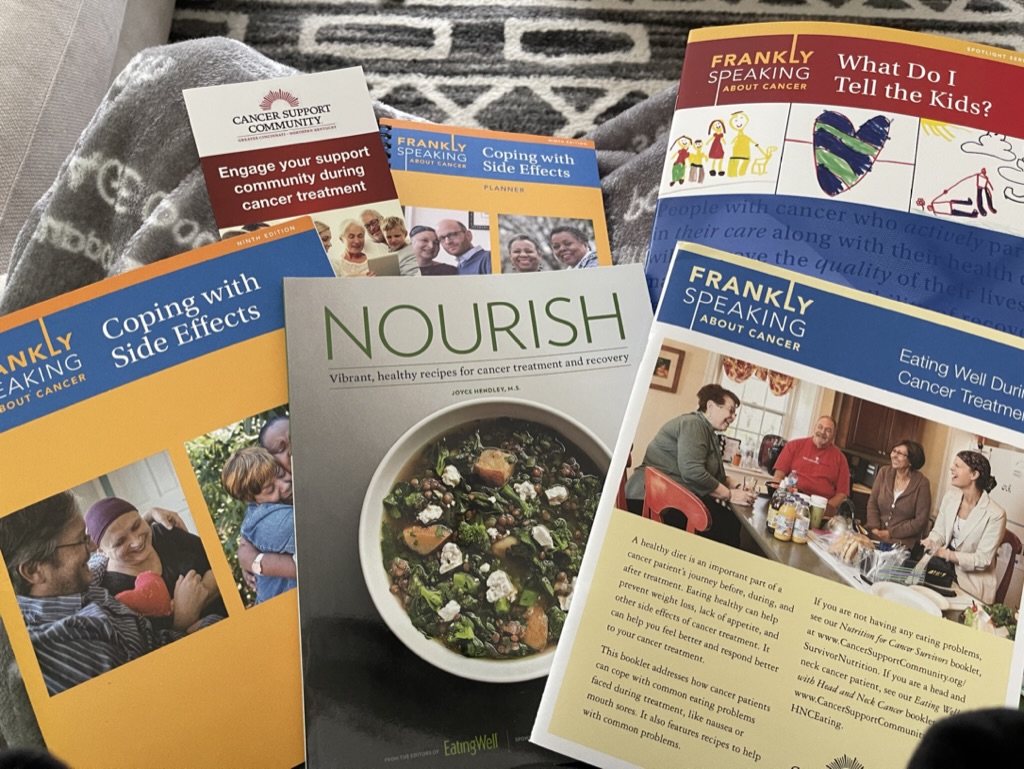
Treatment and Side Effects
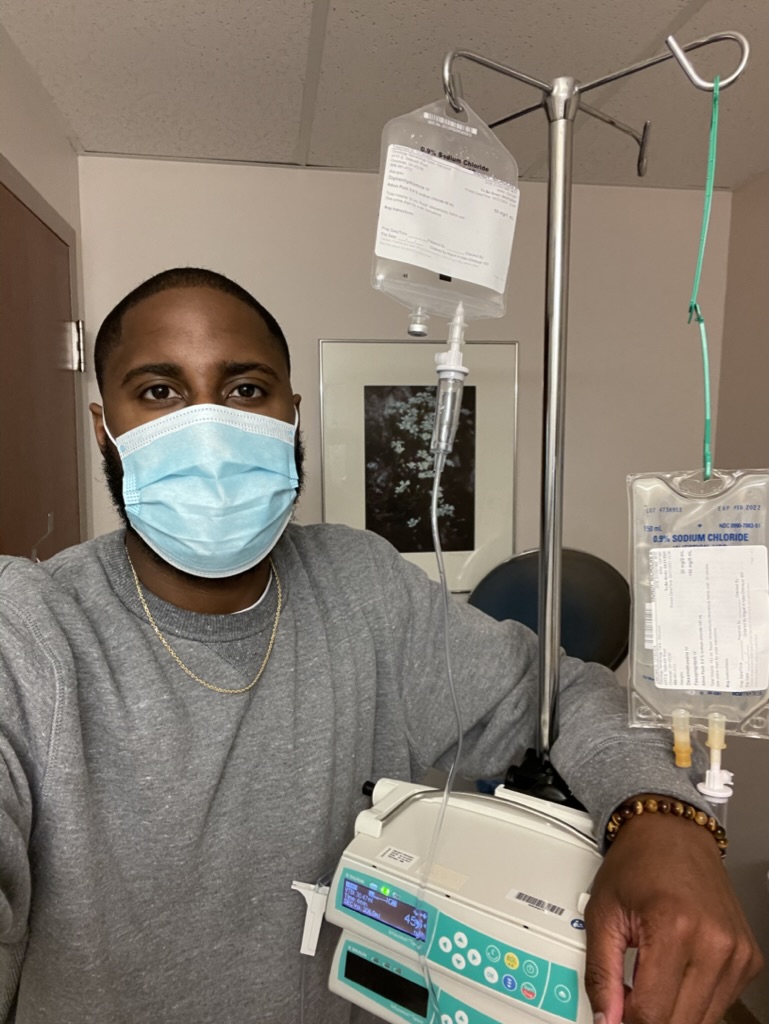
What was your treatment regimen?
Regimen of bendamustine, Rituxan and high-dose steroids
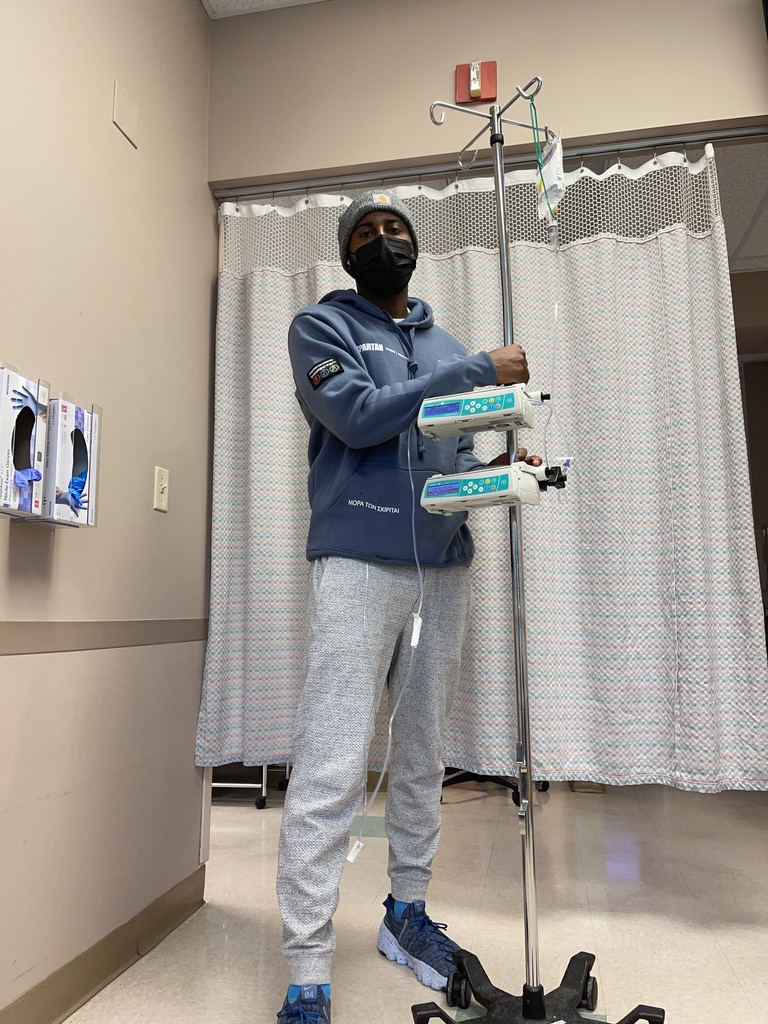
That was every 28 days. I went 2 days back to back. Let’s say I went on Wednesday, and then I went on Thursday. I received the intravenous drugs that you just mentioned there. In between, especially at the beginning, there were days where I needed to get additional fluids and come back into the hospital.
Neutropenia
Often with that treatment, because the bendamustine caused neutropenia and the white blood cell drop, one of the things that I battled often was neutropenia. I had febrile neutropenia a few times, so I spiked a fever. Because I had no white blood cells, I got several different, pretty nasty infections along the way that ended me up in the hospital.
[They were] things that healthy people typically just don’t deal with [because] our bodies are naturally strong enough to fight them off. I wasn’t able to. That landed me in the hospital, and so that was extremely difficult to go through and to juggle all of those things.
The chemotherapy really did a number on me. At the beginning, I was so sick. One of my lymph nodes on the right side was so large that I had to physically move it down so that I could swallow or just swallow water, swallow food and just eat anything.



GI issues
I was really looking forward to starting chemotherapy because I was like, “I know that once I get the steroids (the prednisone), those things will shrink, and I’ll get better.” But man, I had so many stomach issues. My stomach was in so much pain after starting the chemotherapy.
Unfortunately, right before I started chemotherapy, I got E coli. My stomach was in really bad shape going into chemo as it was, and then to put all those tough, tough drugs on your stomach on top of it was really, really tough. For a month, I suffered pretty badly with a lot of stomach issues, just as a side effect.
I wasn’t able to eat very much. I had no appetite. I often had a very watery mouth, just like that precursor to getting sick. Dry heaving every once in a while, especially when dealing with the neutropenia. I would vomit. The diarrhea, the pretty unpleasant things that come with the nature of going through chemotherapy.
»MORE: Cancer patients share their treatment side effects



What helped with your side effects?
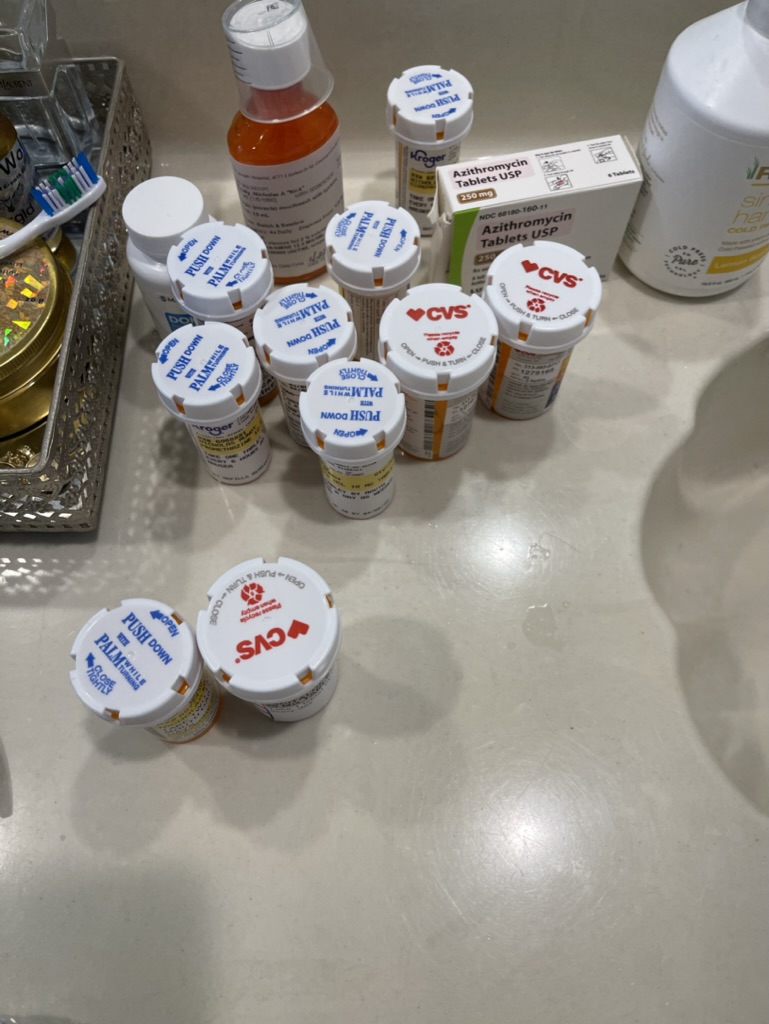
The thing that helped the most with the GI that they prescribed me was omeprazole, a 20 milligram tablet once a day. Ironically, they had prescribed me this during one of my hospital stays. There were so many medications that I was given.
I had lost or forgotten that was one I could take that would help me. I was already taking so much. No one told me or reminded me. I found it one day and remembered, “Oh my gosh, they told me that if I had stomach issues, that I could take this as well.”
I started taking that regularly every morning, and a lot of those underlying stomach issues and major discomforts that I was having went away. That was almost like a party in itself. I had found this medication, and I was like, “Yes!”
I couldn’t believe that I had forgotten it, but then I also offered myself a little bit of grace. I have this drawer full of medication, and sometimes you forget which ones that you’re supposed to be taking or which ones are elective.

Maintenance chemo
The neutropenia and the white blood cell deficiency was a big portion of my story. [For the] original chemotherapy schedule, they scheduled me for 9 months.I was going through that every 28 days, 2 days on.
I finished that at the end of August. I finished that, and then September, [I] took a month off and got scanned. Everyone at this point was like, “Hey, let’s high five. You have no more cancer.” I didn’t have any cancer on the scans, which was amazing.
But something — I think probably all the years that I had gone through this before — told me, “Hey, it’s not over really just yet. Just because your scan doesn’t show cancer doesn’t mean you’re done going to the doctor.” I was still going to have to get my port flushed. I was still going to get blood work, and I was still going to have the scans and the tests that were going to come for years after.



In October of 2021, [it was] 2 days after starting work. At that point, I didn’t have any chemo on the calendar, and work was like, “Do you have any chemo?”
I was like, “No, I’m done. I’m doing well and feel like I’m ready to come back.” Then 2 days into work, I went back for a checkup. The local oncologist was like, “Hey, by the way, standard [care] says that we put you on a minimum of 2 years of maintenance, every 8 weeks of Rituxan and steroids.”
[That’s] what I’ve been going through since August of 2014, and so I went and got maintenance chemotherapy through January.
Stopping maintenance therapy
Every time that I went to the doctor to get my maintenance and to get my blood work, I was still battling white blood cell deficiency and neutropenia.
Every time I went, I was continuing to get Zarxio. They’re shots to boost my immune system, basically, to make it safe for me to be out in the world during the pandemic. Also, I wanted to travel, and it seemed like every time I was getting ready to leave town, to go do something, or to go participate in a race, I would get some blood results that would say that I was neutropenic.
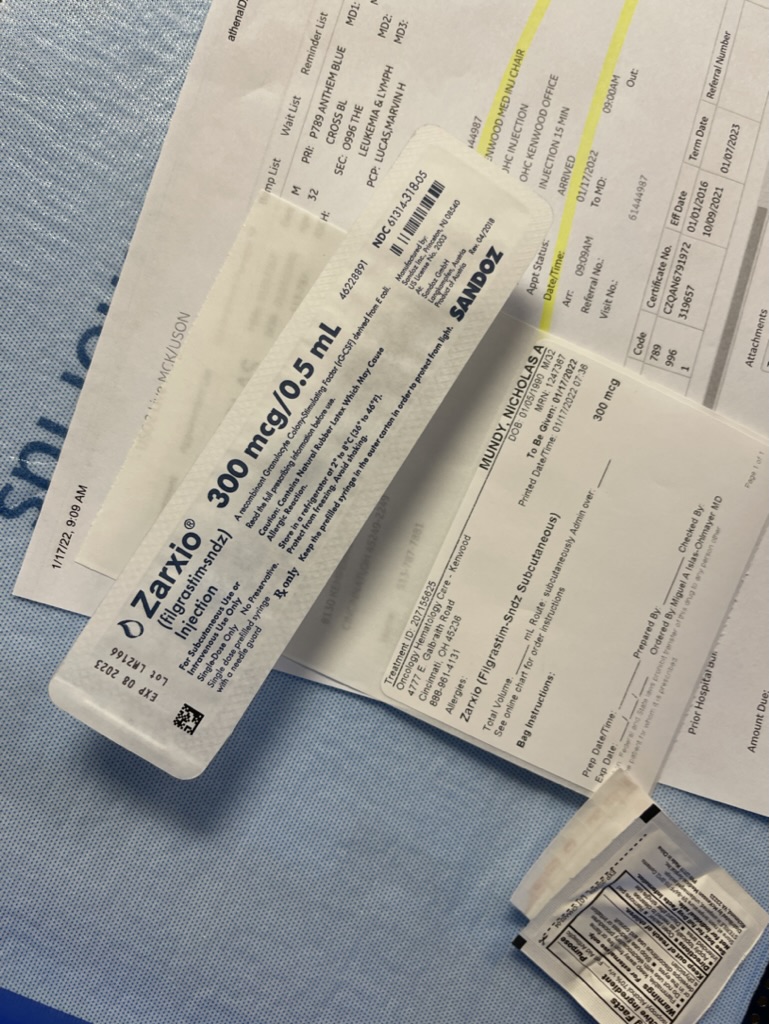
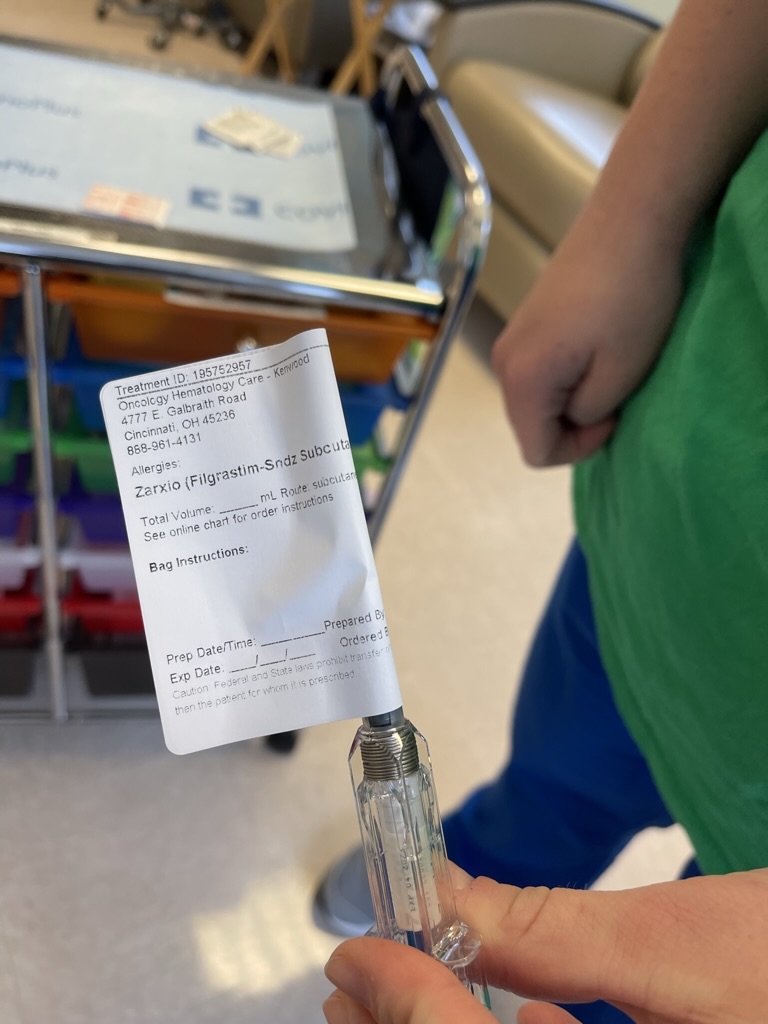
As a result of that, I had a third bone marrow biopsy done at the beginning of March, because my oncologist was worried — “Maybe you have leukemia or another type of lymphoma that’s coming up, because it doesn’t make sense that you’re still deficient here.”
The third bone marrow biopsy was inconclusive. No cancer, none of that, which was great news. They said, “We’re going to hold off on the maintenance at this point, because it’s clear that your body’s gone through it. We’re only keeping you sick at this point.” After a couple of times of getting COVID and some other things throughout this winter, they said, “Let’s stop.”
Reflections
How are you feeling now?
As of now, I’ve been off of maintenance since February, and there are still no signs of cancer. Honestly, for the first time — in my young adult life at all — since I was 22 years old, I feel healthy. I feel good; I feel fit. I have energy. I’m not having night sweats. I’m really celebrating life every day, every chance that I get.
I celebrate life when I’m not feeling well, but I’m really reminding myself of those days where you don’t feel good and how you really sulk in those days. They’re really long. I try to elongate these days of feeling good as well, because it’s been a long time since I’ve felt like this.



What helps you when you’re not feeling great?
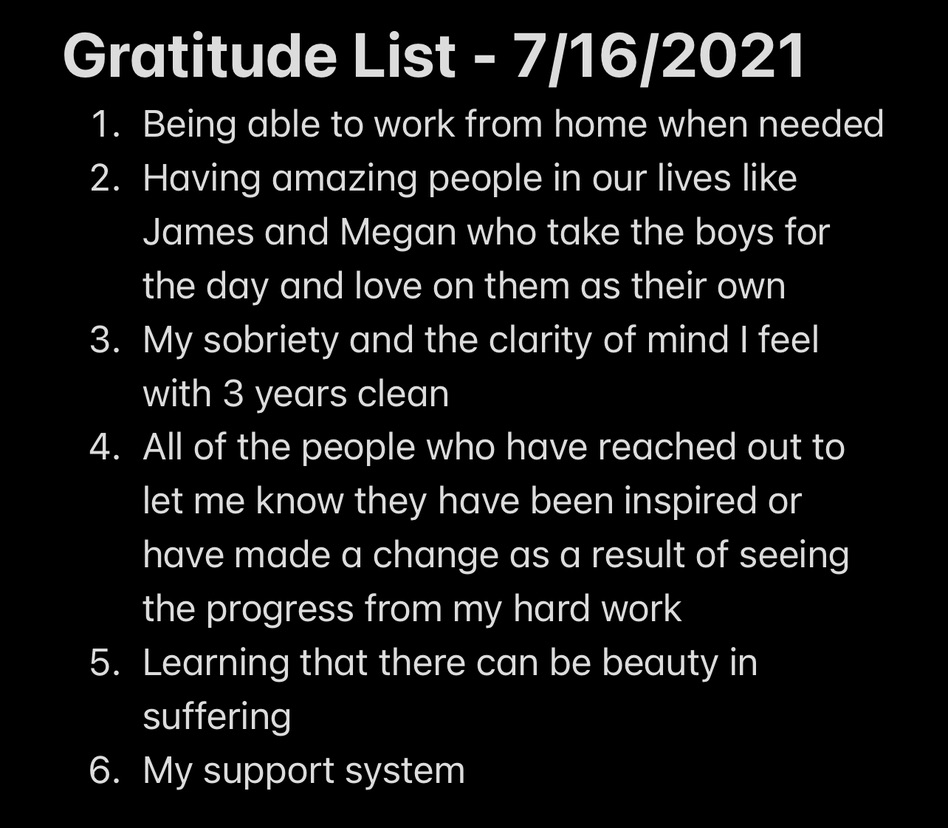
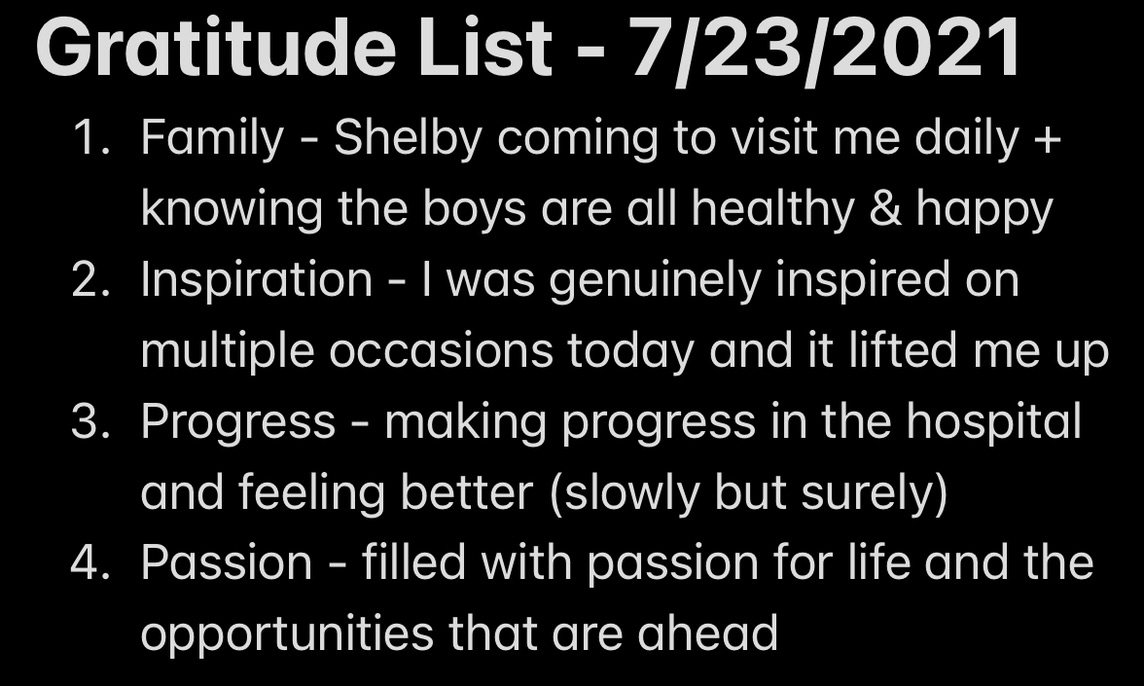
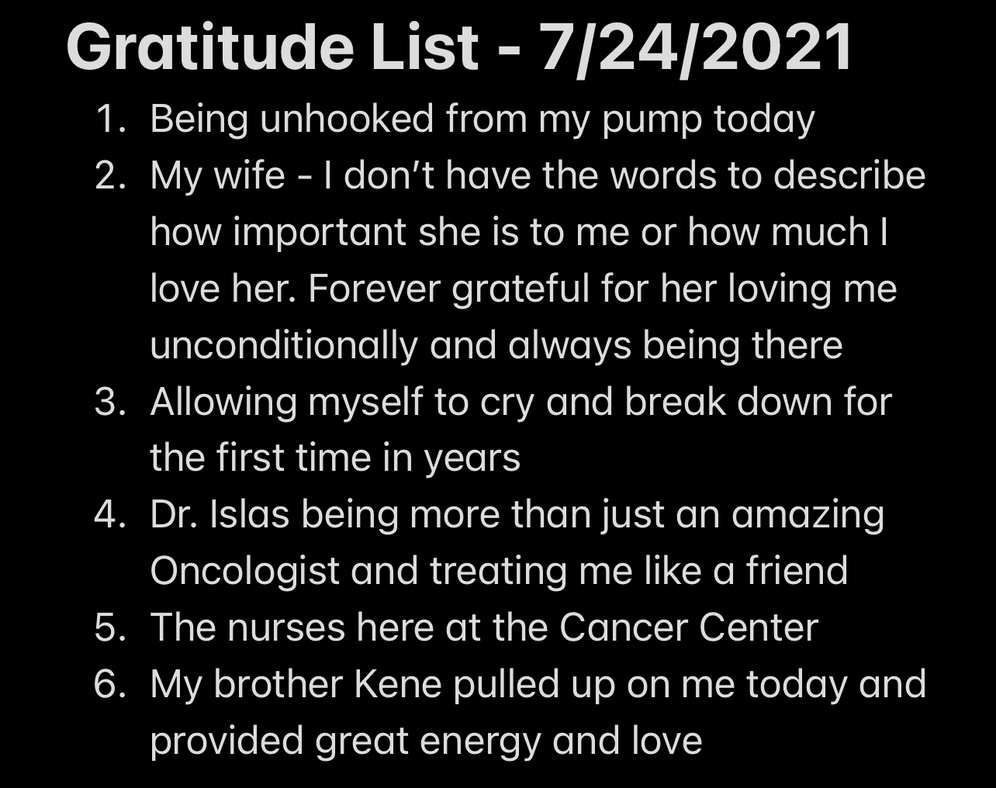
Gratitude list
One of the first things that I do is I try to sit down and do a gratitude list. I ask myself — and I ask it typically out loud — who or what am I most grateful for in this moment right now? Who or what am I most grateful for and most appreciative of in my life today?
That causes me to take a deep breath and to stop, rather than react to whatever emotions or feelings that I’m feeling right now, which are fleeting. They continue to change throughout the day, but often we react to those things. Then we become subject to whatever repercussions that we’ve caused during that.
It gives me an opportunity to slow down and to really shift back to neutral. Let me state the facts. The facts are I am extremely grateful to be above ground today. I’m extremely grateful to be able to brush my teeth, to put on my own clothes, to put on my shoes and to wash my body.
Things that if you’ve gone through this journey — to be able to even use the bathroom on your own and have some privacy, or to wipe your butt without having someone help you is major. Until you’ve gone through that, you take those things for granted often. I start back at the base level and start thinking about those things.
I’m grateful that my kids are healthy and that I have both of my parents. When I start going through that, I start realizing, “Wow, yeah, life could be better for my current situation, but it also could be a lot worse. I’m very fortunate to have the things that I do have today.” Whenever I’m really feeling it or in the thick of it, I go to a gratitude list.
Lean on support
Then point two is I pick up the phone and call somebody, or I lean on somebody that I can trust. I find that when I don’t say how I’m feeling, I typically compartmentalize or numb or bury those things. All that does to me is it keeps me sick over time. Then I have more emotional wounds to deal with later.
I’m trying not to add anything on, so I’m trying to use some of the tools and resources that I’ve learned along the way, [as well as] those real-time tools that I keep in that invisible bag of tricks at my feet. I try to utilize those, but gratitude is something that helps me get out of myself almost immediately.
How have you turned your pain into purpose?
I hear Eric Thomas speak about this a lot. He’s a profound motivational speaker that I look up to. [He] talks about recycling your pain. I didn’t realize that’s what I was doing as I was going through this, but I have used all of this pain. I have recycled this pain, and I’ve used it to find my higher purpose.
I follow that purpose with an extreme amount of passion. Like I told you at the beginning of this, I’m fanatical about personal growth. I’m fanatical about maximizing human potential. Then also, as you’ve heard me talk about some of the real-time tools that I use and remaining objective and neutral, I’m really big on mindset.



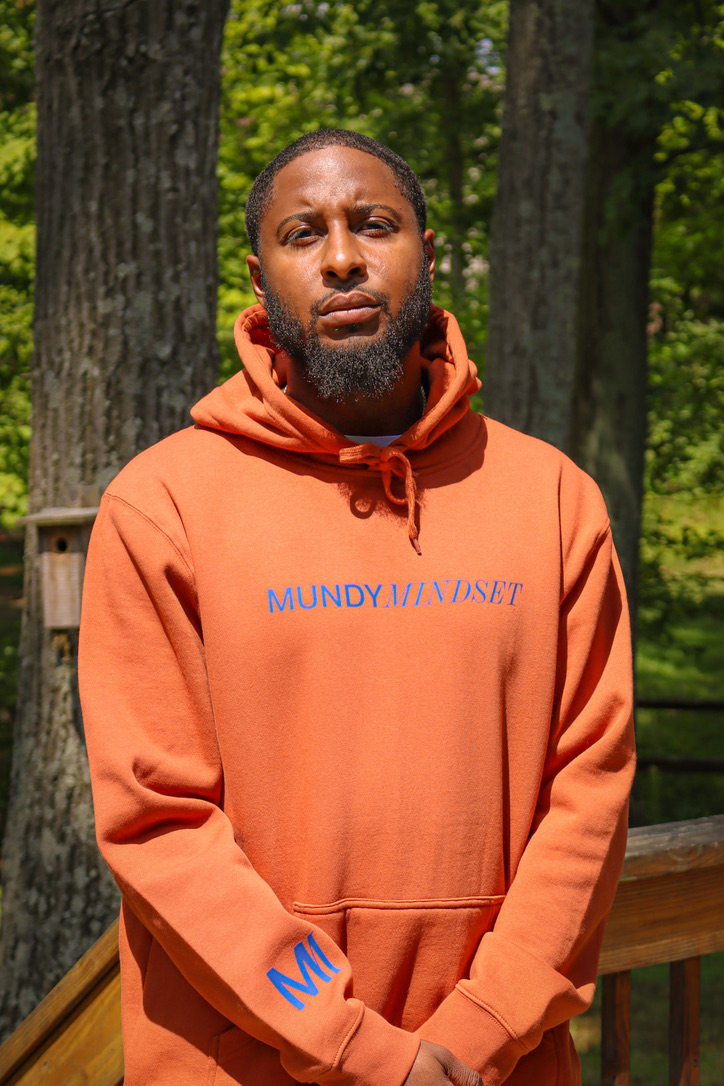

Mundy Mindset LLC
As a result of going through all of these different things that I’ve experienced over the last 9 years, I started a mindset and wellness coaching company called Mundy Mindset LLC. It’s a mindset and wellness coaching company. I teach people to utilize their resources that they have right in front of them and that they have within them, and to utilize their mind to propel them to ultimately create their reality.
Our minds are extremely strong, and as you’ve probably seen, your body will often follow what your mind is telling it. If your mind is telling you that you’re sick, if you have a defeatist mentality or attitude, if you’re focused solely on the negative, or if you have pre-diagnosed yourself with a death sentence, the body typically can follow. That can be extremely scary. That could cause worse issues that could cause you to die prior to your cancer diagnosis itself, just by sheer quitting or the quitting of your spirit.
I like to help people and teach them to take advantage of their time. Life is not fair. We have a limited amount of time. I teach people to live to their fullest, to utilize habit setting to achieve the goals that they want to accomplish in this life, and to really make sure that they’re leaving a legacy that they’re proud of.
They’re doing it in a way that inspires others around them to do the same. I’m fanatical about that. It’s my passion. I just want, like I said, to create a place where I leave many people positively impacted and leave people better than when I found them.
»MORE: Follow Nick on social media to learn more about Mundy Mindset LLC

Inspired by Nick's story?
Share your story, too!
More Marginal Zone Lymphoma Stories
The Importance of Positive Role Models
The example that Nick's father set for him as he was growing up taught him how to prioritize and advocate for his health.
Nick M., Nodal Marginal Zone Lymphoma
1st Symptoms: Daily hives, GI issues, weight loss, heart issues, night sweats
Treatment: Rituxan (rituximab) and high-dose steroids
Kimberly O., Marginal Zone Lymphoma
1st Symptoms: None at first, routine blood work showed suspicious results, bad nosebleed
Treatment: Chemotherapy (bendamustine & rituximab)
Rachel P., Marginal Zone Lymphoma, Gastric MALT
1st Symptoms: Fatigue, bloating, stomach pain
Treatment: Chemotherapy, targeted therapy, surgery



One reply on “Nick’s Stage 3-4 Marginal Zone Lymphoma Story”
Your story and strength is very moving and I am so glad I read your story and that you are feeling better!!! Your story has modified me to take my health more serious and to get moving and to prepare for my two knee replacements.