Diagnosis and Treatment for Bladder Cancer

How is Bladder Cancer Diagnosed?
One or a combination of several of the following tests may be used to diagnose bladder cancer:
- Cystoscopy – Your doctor inserts a small tube known as a cystoscope through your urethra to examine your urethra and bladder for signs of cancer.
- Biopsy (TURBT) – Collecting a cell sample to analyze for cancer. This is sometimes done during a cystoscopy by passing a unique tool called a resectoscope through the cystoscope.
- Urine Cytology – A urine sample is analyzed under a microscope to check for cancer cells.
- Urine Tumor Marker Test – Urine samples are taken to analyze for certain substances (markers) commonly linked to bladder cancer cells.
- Computerized Tomography (CT) Urogram – A contrast die is injected into a vein in your body that eventually flows through the kidneys, ureters, and bladder. X-ray images are taken during the test to provide a detailed view of your urinary tract and assess potential cancer areas.
- Retrograde Pyelogram – similar to a CT urogram, but done in reverse to get a better look at your upper urinary tract. A doctor will thread a catheter through your urethra to inject contrast dye into your ureters. While the dye flows to the kidney, x-ray images are taken.
Cystoscopy, in combination with a biopsy, is typically used as the definitive test for bladder cancer. However, different tests may be used depending on your symptoms and personal situation.

[during the cystoscopy] they’re basically slipping a tiny tube with a camera through your urethra to head on into the bladder and have a look-see around. That’s being shown on a screen.
– Margo W. | Read More
Diagnosing the Extent of Bladder Cancer
If it appears that the bladder cancer has spread, your doctor may recommend additional tests to see if it has spread to other parts of your body. This helps when determining the grade of bladder cancer. Some of the tests to diagnose the extent of bladder cancer include:
- Additional CT scans
- MRI
- PET scans
- Bone scans
- Chest x-ray

We had the abnormal CT, the extra scope that was abnormal, and then the surgical procedure to biopsy this growth that he saw to see more of what was going on.
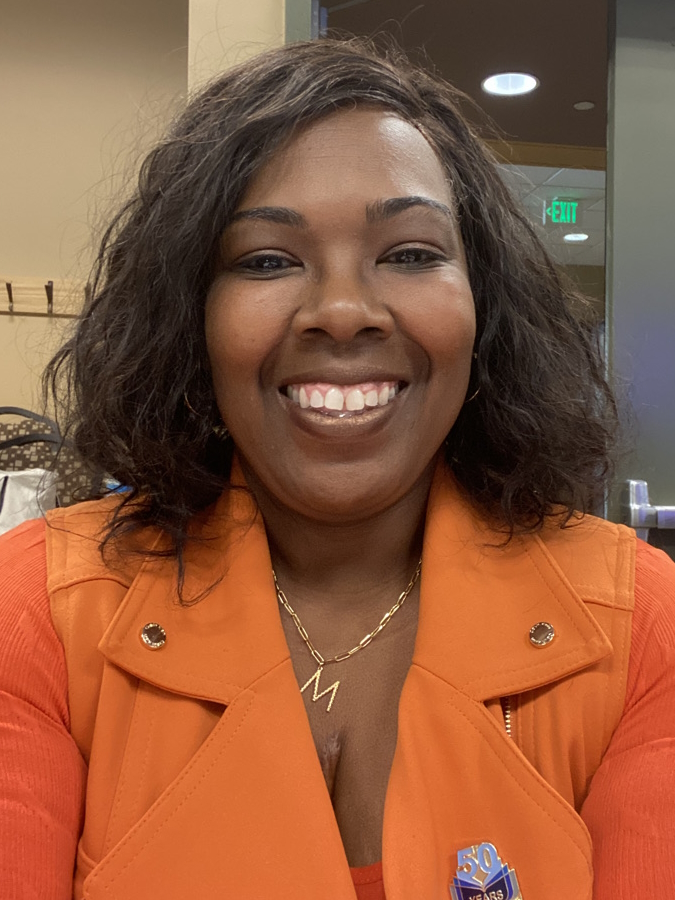
Ebony G | Read More
Grading Bladder Cancer
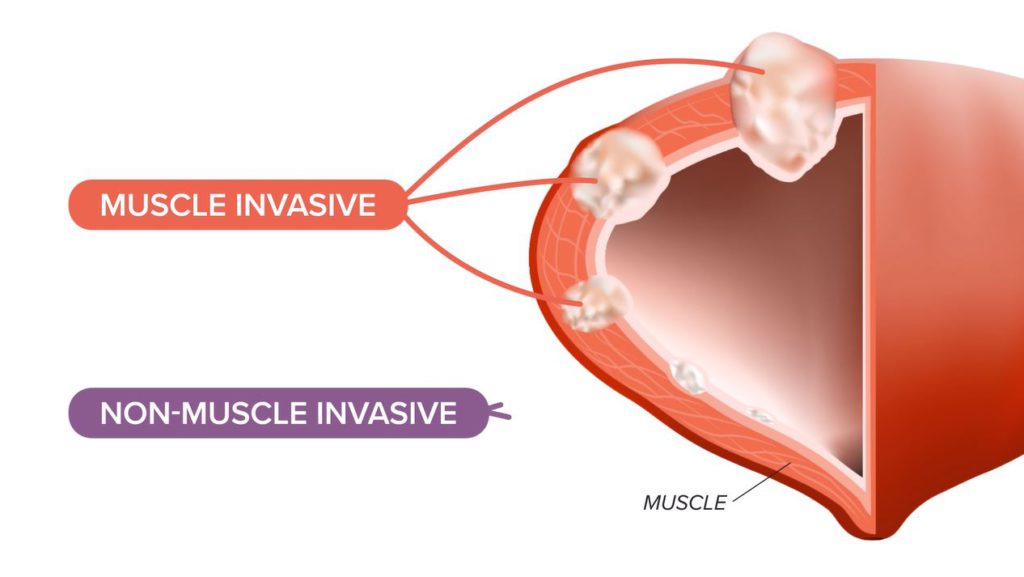
When bladder cancer is diagnosed, it is also given a grade. Grading is done on a scale of 0 – IV, with IV being the most severe. Grading for bladder cancer is based on the TNM scale, which essentially assesses how far the tumor has grown through the bladder wall if it has spread to the lymph nodes, and if it is metastatic.
Your doctor may perform additional diagnostic tests to grade the bladder cancer. While all bladder cancer is important to treat and monitor, the higher the grade, the more urgency there is for action.
Visit our bladder cancer overview page to learn more about staging.
Treatment for Bladder Cancer
There is no one set treatment plan for bladder cancer. Treatment options and recommendations will vary based on several different factors, including:
- The stage of the cancer
- Your age
- Expected impact of the treatment
- Other health conditions you may have
When working through the treatment options with your care team, it’s essential to ask questions and understand each treatment’s benefits and potential side effects.
Bladder Cancer Surgery
Transurethral Resection of Bladder Tumor (TURBT)
As you may have noticed, transurethral resection is one of the procedures used to diagnose bladder cancer. However, it can also be used to treat early-stage bladder cancer.
A TURBT uses a resectoscope to go into your bladder through your urethra to remove abnormal tissue or tumors.
Occasionally, a surgeon will need to perform fulguration after removing a tumor. This involves using a high-energy laser to burn any potentially remaining cancer cells.
A TURBT is considered a surgery, but the side effects are generally mild, and most people can go home from the hospital the same day as the surgery.
Cystectomy
When bladder cancer is invasive (it’s spread into or through the bladder muscle wall), you may need to have a cystectomy to remove either part or all of the bladder.
- Partial cystectomy – if the cancer has only spread to one part of the cancer, then your doctor may be able to only remove part of the bladder. Lymph nodes near the tumor may also need to be removed. This helps a patient avoid reconstructive surgery.
- Radical cystectomy – If the cancer has spread to several parts of the bladder, your doctor may have to remove the entire bladder. In men, the prostate and seminal testicles are also removed. While in women, the ovaries, fallopian tubes, uterus, cervix, and part of the vagina are also removed.
If you have to have your entire bladder removed, you will require reconstructive surgery to allow your body to store and pass urine. The different types of reconstructive surgery include:
- Incontinent diversion – a portion of the intestine is used to create a passage from your ureter (tubes that carry urine from the kidney) to the skin on your abdomen via a small opening known as a stoma. Urine then flows continuously into a bag stuck on your stomach that is periodically emptied.
- Continent diversion – works similarly to an incontinent diversion, only there is a valve that prevents the continuous flow of urine. However, the urine must be removed via a catheter several times daily.
- Neobladder – the surgeon creates a “new” bladder by using a piece of intestine to connect your ureter back to the urethra. This allows you to urinate normally; however, you have to urinate on a schedule as you won’t get the feeling that you need to “go.”

What type of diversion am I going to have? Did I want to have a bag? No, I’m 52 years old. Why would I want a bag if I don’t have to?
LaSonya D. | Read More
Unfortunately, there are several side effects associated with all types of cystectomies, including:
- Infections
- Blockages
- Urine leak
- Incontinence
- Absorption issues
Depending on whether it was a partial or radical cystectomy, both men and women can be impacted sexually by the surgery. Men may lose the ability to produce sperm or get an erection, while women may lose the ability to orgasm, and sex may become uncomfortable.
Chemotherapy
Chemotherapy is a form of drug therapy used to kill cancer cells or prevent them from dividing. As a treatment for bladder cancer, chemo is typically given in one of two ways:
- Systemic chemotherapy – the chemo drug is injected into a vein to enter the bloodstream and reach cancer cells throughout the body.
- Intravesical chemotherapy – A tube is inserted through the urethra to flush the bladder with chemo drugs.
Chemotherapy can be given before surgery to shrink a tumor pre-operation, after surgery to prevent the chances of cancer returning, in combination with radiation therapy, or as the main form of treatment for bladder cancer.

The one that I wanted was the dd-MVAC (dense-dose methotrexate, vinblastine, adriamycin, and cisplatin). You go in one day and they give you two of the drugs. Then you go in the second day and they give you the rest of them. That’s for two months, two times a week, every other week for two months.
Vickie D | Read More
Immunotherapy
Immunotherapy is a treatment used to help a patient’s immune system fight cancer. Before starting immunotherapy, your doctor may recommend running biomarker tests to identify the most effective drug.
- Systemic immunotherapy – immunotherapy drugs commonly used to treat bladder cancer via injections into the vein include avelumab, novolumab, and perbrolizumab.
- Intravesical immunotherapy – the main immunotherapy drug used to treat bladder cancer via a catheter insertion is BCG (bacillus Calmette-Guérin).

For this type of cancer (urothelial bladder cancer), BCG is immunotherapy. It’s actually the tuberculosis vaccine and it’s the most effective treatment.
Karen R | Read More
Targeted Therapy
Targeted therapy blocks cancer-causing actions by proteins, enzymes, and other molecules. Some commonly used targeted therapy drugs for the treatment of bladder cancer include enfortumab vedotin, erafitnib, ramucirumab, and cacituzumab govitecan-hziy.
Clinical Trials
The possibilities for bladder cancer treatment are ever-growing. If there isn’t a viable treatment option for you, there may be a clinical trial that you can enroll in. To find active bladder cancer clinical trials visit the NIH’s Nation Cancer Institute’s supported clinical trial search.
Treating Bladder Cancer by Stage
While there are several options for treating bladder cancer, different approaches may be taken at different stages of the cancer.
- Stage 0 – TURBT with fulguration followed by intravesical chemotherapy
- Stage I – TURBT with fulguration is used to determine the extent of the cancer. If it’s low grade (slow growing), a second TURBT is typically given by intravesical BCG or intravesical chemo. A radical cystectomy may be recommended if it’s high-grade (fast-growing).
- Stage II – surgical removal of the infected area of the bladder and potentially the lymph nodes is recommended at this point. This may be followed with radiation treatment or rug therapy if there’s a risk of cancer returning.
- Stage III – Chemotherapy to shrink the tumor, followed by a radical cystectomy, is typically recommended. Following surgery, the patient is closely monitored and potentially given drug therapy to ensure the cancer doesn’t return.
- Stage IV – Chemotherapy is the main treatment for stage IV bladder cancer. Surgery at this point won’t likely remove all of the cancer, so treatment is aimed at slowing the growth of the cancer. Your doctor may recommend you for a clinical trial.
While these are the standard treatments for each stage of bladder cancer, your treatment plan may vary based on your situation and how the cancer progresses.