My Dad’s Cancer Journey: How He Inspired Me to Take Control of My Health

Nick has persevered through a series of health challenges. After an agonizing 13 months, he finally got a diagnosis: IgG4-RD, a rare autoimmune disorder. Seven years later, this pseudolymphoma morphed into a rare type of non-Hodgkin’s lymphoma that only represents up to 2% of non-Hodgkin’s lymphomas.
As Nick tries to set an example for his 3 young children, it was the example that his father set for him as he was growing up that taught him how to prioritize his health.
They share the importance of finding a medical team that is a good fit for you, someone you can trust, and why you should always advocate for yourself.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Don’t be afraid of the prognosis. Be afraid of not knowing and not doing anything about it. Medicine in today’s world can do a lot of things.
Harry
Introduction
Nick: First and foremost, I want to thank you guys because I wouldn’t be here today. You have supported me through so much.
I feel like because of the way that you raised me, the experiences, the patience, the forgiveness, all of those things [have] helped mold me into who I am today so I just want to say thank you. Thank you for being open to doing this because this is not something that we do typically as a family so it’s pulling us all out of our comfort zone.
Ultimately, it’s not about us. It’s about creating awareness and showing other people of color and just other people in general what this can look like and how important it is to have positive role models in your life. I don’t take that for granted so I just wanted to say thank you for that.

Gail: Oh, you’re more than welcome. We wouldn’t have done it any other way. We wouldn’t have had it any other way.
Nick: A big reason why this came up and why The Patient Story gave us this platform to do this [is] because I mentioned a big reason that I’m still here today is [that] I had you guys as positive role models in my life.
I always saw [you] go to the doctor [and] prioritize your own health so it was just something that was natural for me. As I’ve grown up [and] gotten to meet more people and [heard] what their experiences have been like, that is not the case for everybody and for a lot of people, unfortunately.
What a great opportunity for me to put a spotlight on this and just let people know how impactful and how imperative it is to your overall health, quality of your life, and longevity to prioritize yourself, to go get checked.
Going to the doctor was an inconvenience, but it wasn’t costly and it was for my own benefit.
Harry
What motivated you to prioritize your health?
Nick: What drove you to prioritize your health all of those years, [going] to the doctor and [getting] prostate exams in the middle of the workday?
Harry: That’s how I was raised. My parents didn’t have a lot of money so we used to go to the children’s hospital [in] my early years.
I was raised to go to the doctor and get a physical. Then being in the fire department, you always had to be physically sound.
When I went to Great America, [the] first thing they said was, “Hospitalization. We can get you.” I said, “Well, I got this.” And they said, “No, we’re going to give you ours as well.”
It’s been easy for me because I’ve always worked and always had insurance. Going to the doctor was an inconvenience, but it wasn’t costly and it was for my own benefit. And that’s why we raised you that way.
Just go to the doctor [and] get it checked out. [If] you start coughing, we’ll give you a little cough medicine. If that didn’t work, we’re going to the doctor.
It’s important that everybody gets a checkup. Don’t be afraid of the prognosis. Be afraid of not knowing and not doing anything about it. Medicine in today’s world can do a lot of things.

Good health and peace of mind are the two things that you need the most. Everything else is just like gravy.
Harry

Getting diagnosed with prostate cancer
Nick: You and I haven’t really talked too much about this. I never forget that you had cancer, but our experiences were vastly different.
You went all those years and got these exams. Did anything ever come up? Any signs or symptoms along the way?
Harry: It really was a shock to me, to be honest. I go to the doctor annually. If I got sick, I go to the doctor. I worked for that and the insurance is there so I would go.
I went for a routine [check and the] urology doctor says, “Something ain’t right.” They did a biopsy and he said, “You have prostate cancer.” So I said, “Well, what do we do?” And he said, “Well, you can live with it or we can take it out.” And I said, “Take it out.”
People make such a big deal of things that aren’t necessary to have a happy life. Good health and peace of mind are the two things that you need the most. Everything else is just like gravy on potatoes is what it is.
Nick: I love that.
Harry: That’s the gravy of life. So I got a little less gravy, but I still got life. It wasn’t a hard decision. It wasn’t an easy one, but I did what I thought was the right thing to do.
Nick: It’s so powerful to have both of you [as] examples [and] also you as a strong black man, prioritizing your health, and not letting whatever stigma or what other people think. That is why you’re still here with us and I’m extremely grateful for that.
You had surgery. They removed the prostate and I’m sure that that was extremely challenging as well. Can you share a little bit about that experience?
I was raised that God [doesn’t] give you burdens you can’t carry. So I just carry it, not worry about it.
Harry
Harry: The hardest part is when you get the diagnosis. When I prayed about it and thought about it, it wasn’t that big of a deal. I’m still here. I’m still living. I still have fun. Still got my wonderful wife.
It didn’t change my life. It didn’t make it worse. It didn’t make it better. It’s just something that happened. I was raised that God [doesn’t] give you burdens you can’t carry. So I just carry it, not worry about it. Wake up every day, happy to be alive. Got my faculties about myself. It’s a great day.
Gail: Because he acted so quickly and was going to the doctor, it had not gotten to the prostate wall.
They did not have to do radiation so that was great. Now we go every three to six months, depending on what his urologist says, and just [have] the PSA checked. We’ve got that coming up.
I don’t go to [the] doctor every time I get a cough or a sneeze, but I do get regular checkups. If they find something, we do what we can about it.
Harry
Dealing with “scanxiety”
Nick: One of the things that cancer survivors often continue to combat is test anxiety or scan anxiety.
Nick: You got to go quarterly and for some people, that’s a lot. It has them relive all of these things that were pretty traumatic.
I have developed different things in my own routine to handle that. Do you ever have any scan or test anxiety? Do you ever worry?
Harry: No, no. They say you need to come [to] get checked, I go get checked. That’s all I can do.
I’m not a doctor. I don’t know medicine so I can’t judge. If he says I need to be checked, I do it. It’s that simple.
[For] a lot of people, it’s denial. They don’t want to be sick so they try to deny it, put it off, or push it back. I’m not that guy.
I don’t go to [the] doctor every time I get a cough or a sneeze, but I do get regular checkups. If they find something, we do what we can about it.
Nick: This is what I do as well in between appointments and before I go in. We talk about managing our expectations, objective thinking, neutral thinking, [and] just telling yourself the facts.
The facts are I feel good. I have everything I need to win the day. I’m loved, I’m provided for, I’m safe, and, right now, to my knowledge, I don’t have cancer. No one’s told me that so I’m going to move and operate as if I don’t have cancer. If that comes up again, then we’ll deal with it when that happens.
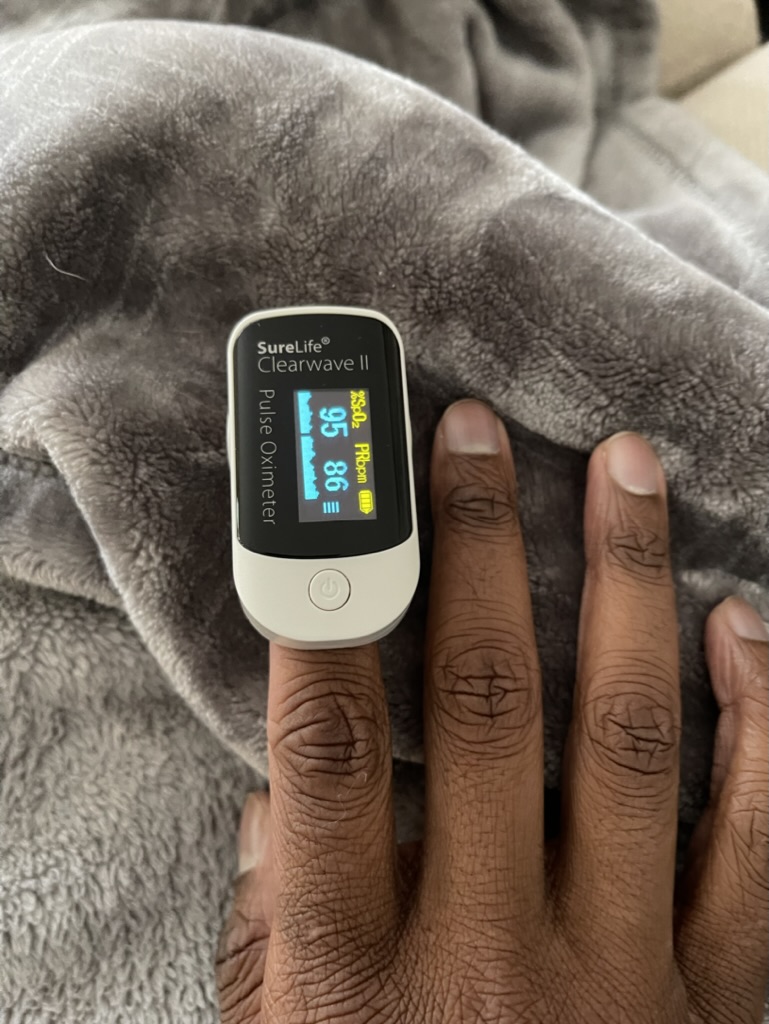
But often, that scan anxiety and test anxiety can just manifest. Honestly, I feel like sometimes that can lead you back into a resurgence of cancer because you’re living in a state of toxic stress and anxiety.
Gail: The negativity.
Nick: As I continue to learn more about this, when you’re in a state of toxic stress and worrying about things that you can’t necessarily control, your immune system’s down and you create an environment for disease to come back up.
A lot of the stuff that just fills me up and that has helped me get through the trials of my own life.
You are rooted in everything that I do — the way I move, the way that I think, my tattoos — all of it. I’m extremely grateful and I love that it comes from you guys.
When you do find somebody, you stick with them because then you develop that rapport, that trust.
Nick

Understanding medical mistrust
Nick: I don’t want to assume or generalize, but as I think about medical mistrust and the fear of going to the doctor, from my understanding [and] knowledge of history, black people haven’t always been treated the best in the medical community. We were the subject of test experiments for years and that just doesn’t go away. What can be done? Where is that mistrust rooted?
Harry: I recall the segregationist when I was growing up. But my father always wanted us to have the best, so he fed us and took us to the doctor to make sure we were healthy.
You just have to put your trust in the doctor that you have. When I came back from the military, my mother’s doctor [became] my primary care physician. After a while, he told me, “I got a new guy coming on. You guys could grow up together,” and he’s still my doctor to this day.
We had a great relationship. I tell him, “Just tell me like it is. Tell me what it is and what you recommend.” I put my faith in him.
Nick: That’s the only doctor I know you’ve ever seen.
Harry: Yeah. He’s good. My mother always made sure we got a physical every year. If we got a cold or cough, my dad would try to treat us with his remedies. My mom said, “I’m taking him to the doctor.” That’s how I was raised so I don’t have a problem with doctors.
Gail: I think, too, that you do have to just trust.
I’ve said many times: every doctor is not a fit for everybody, but you shop until you find somebody who is a fit for you and then you put your trust in that particular doctor. If you don’t trust them, then move on and find somebody else.
For the most part, doctors are in that field for the right reasons. You have to trust that they’re going to do the best [for] you. I don’t care if you’re red, white, black, green, or yellow. You have to put your faith in the doctors and in God. God will take care.
Every doctor is not a fit for everybody, but you shop until you find somebody who is a fit for you and then you put your trust in that particular doctor.
Gail
Nick: That’s great. I love that because that is the same thing that you taught me about advocating for myself as well. If you don’t feel comfortable with a certain doctor or you don’t like the way the visit went, that doesn’t mean that you have to stay with that doctor.
[It’s] the same thing with therapists. Just because I didn’t have the best experience with this therapist in this city [at] this time on this date doesn’t mean all therapists are bad. It doesn’t mean all therapists don’t get me. It doesn’t mean that therapy doesn’t work.
It just means that I need to continue to advocate for myself and continue to look. Then when you do find somebody, you stick with them because then you develop that rapport, that trust.


From autoimmune disease to non-Hodgkin’s lymphoma
Nick: I think that was in July 2013 when I first got sick and went to the hospital. They told me my heart was enlarged, my prostate was enlarged, and I needed to go to the cardiologist right away [and] cease physical activity and sports. Everything right after that kind of picked up.
It wasn’t immediate but that triggered a domino effect of going to the doctor almost every month. I was getting sick with different things.
Autoimmune diseases impact everyone differently in different ways and can sometimes be tricky to diagnose. But one of the things that I think you guys will both remember — and I know you could definitely have empathy for — was that discouragement of going to so many different appointments, getting surgery to remove lymph nodes, bone marrow biopsies, and then not having conclusive results, not having a diagnosis. It would have been easy to kind of cash it in.
I told Shelby at one point, “You shouldn’t be going through this. Nobody deserves to go through this. I don’t want you sitting in doctor’s appointments. We’re kids.”
But nobody gave up. Even when I had lost my steam sometimes, my support system — you guys and Shelby — always motivated me to continue to go. [You even] drove me if I didn’t want to go.
Nobody had given me anything to make me believe that they were going to be able to cure me or help me figure this out.
Nick
That was a learning experience in itself. Having the procedures done [at the Mayo Clinic], the full body plasma transfusion, another bone marrow biopsy, and then them sitting us down like, “Hey, we’re going to do surgery on your heart,” and then talking to us about the statistics and risks and having to sign papers.
Nobody had given me anything to make me believe that they were going to be able to cure me or help me figure this out. I remember almost bargaining with God and just like, “If you get me out of this, if I can at least make it through this heart surgery, I will change how I’m living. I will try to get better.”
I was fatigued. I was drained. I didn’t have the mental capacity. I didn’t have the physical energy to be able to ask good questions. I didn’t even know what to ask. I didn’t know what this looked like, what you’re supposed to do, or how you’re supposed to go about this.
You don’t get a handbook that says, “Here’s how you should go about this. These are the question you should ask,” so having someone like you who is anal about that kind of stuff was a game changer. I’m sitting there, embarrassed, I’m like, “Ask one more question, please. Can we just go?” But that is what you do need. [Having] you doing that is huge.
Gail: They treated you with chemo.
Nick: But I wasn’t a cancer patient, so I didn’t fit into a support group. I had you guys, but I didn’t have the resources of being in a cancer support group, even though I was being treated and talked to as a cancer patient, and being told I had lymphoma, which was difficult.
Then now [I] have a type of non-Hodgkin’s lymphoma that only represents up to 2% of non-Hodgkin’s lymphomas. I’ve been [an] interesting case before. I’m already a case study at the Mayo Clinic. I already understood that I was like hitting the lottery. Now I happen to be his only patient that had the IgG4 mutate into a full-blown lymphoma, also [a] rare type of lymphoma.
But I trusted him and I trusted Dr. Islas. Even though I got the understanding of stage 3-4, I never thought was going to die. I knew because I had done so much work investing in myself: getting sober, going to therapy, and working on myself emotionally, mentally, spiritually, [and] physically. It was almost like I personally believe my higher power got me ready to go to war to be able to face this.

Keep good notes and ask good questions. It’s your health. Advocate for yourself.
Nick

Words of advice
Nick: Keep good notes and ask good questions. It’s your health. Advocate for yourself.
Gail: Be diligent. With [the] insurance system, you had to keep going back and forth with them. I think that’s why some people give up and don’t want to fight. You have to be diligent about it. You have to keep in touch with the insurance companies.
At one point, when they told you that insurance wasn’t going to pay for the Rituxan, you could have easily just said, “Okay, well,” but you didn’t. You fought with it and your doctors because you trusted in the doctors.
You stayed on it. You stayed on it and your doctor stayed on it so that you were able to get help.
You can’t give up. I tell the little guys all the time, “We’re Mundys. We don’t give up.”
Harry: We don’t quit.
Nick: Yeah, Mundys don’t quit. But you’re absolutely right.
If I’m being completely honest, another reason why I went a full year without it was [that] I was defeated. I was so pissed off. I felt like a victim. It’s like, “How do I, the patient who is going through hell, have to sit and be the middleman between the insurance company and the big hospital when the hospital made a mistake [in] billing for an injection?”
They coded it as an injection because that’s the standard of care that most people were getting. I was only approved to get it intravenously so when they billed me for an injection, which was not what I received, I got stuck with a $20,000 bill. The insurance people are like, “Well, you got to pay this,” and I’m like, “I’m not paying this.”
I had done that for years before because it had happened multiple times. At that point, in the middle of COVID and all, I was being naive, too. I’m like, “I’m good. I don’t want to deal with this.” But once again, my doctor stayed [with] me.
That is why I have been able to accomplish what I’ve been able to accomplish. That’s why I’m where I am today. I know that you guys are definitely proud.
I hope that you guys are here and I hope I’m here long enough to continue to see the fruits of your labor and all of the stuff that you have continued to just invest in me and see other people benefit. It’s extremely profound when you think about it. I’m just extremely grateful for it.
Harry: You’re a good man. I love you. You really are. I’m very proud. You’ve been through a lot and you kept your head up. Never heard you complain. I’m thrilled to be sitting here with you today. I don’t want to get emotional so I’m going to stop.
Gail: We love you and [are] very proud of you. We just want to see Mundy Mindset continue on with the next generation.
Nick: We got three great ambassadors in the making.

That is why I have been able to accomplish what I’ve been able to accomplish. That’s why I’m where I am today.
Nick
Marginal Zone Lymphoma Patient Stories
The Importance of Positive Role Models
The example that Nick's father set for him as he was growing up taught him how to prioritize and advocate for his health.
Nick M., Nodal Marginal Zone Lymphoma
1st Symptoms: Daily hives, GI issues, weight loss, heart issues, night sweats
Treatment: Rituxan (rituximab) and high-dose steroids
Kimberly O., Marginal Zone Lymphoma
1st Symptoms: None at first, routine blood work showed suspicious results, bad nosebleed
Treatment: Chemotherapy (bendamustine & rituximab)
Rachel P., Marginal Zone Lymphoma, Gastric MALT
1st Symptoms: Fatigue, bloating, stomach pain
Treatment: Chemotherapy, targeted therapy, surgery


