Mark’s Stage 4 Metastatic Prostate Cancer Story

One day, Mark woke up unable to walk. After countless tests and scans, Mark was diagnosed with stage 4 prostate cancer. Additionally, the cancer had spread to his lungs and bones.
Mark shares how a positive mindset helped him through his cancer journey, how cancer has led him to be more grateful, and how he advocated for the treatment plan that worked best for him.
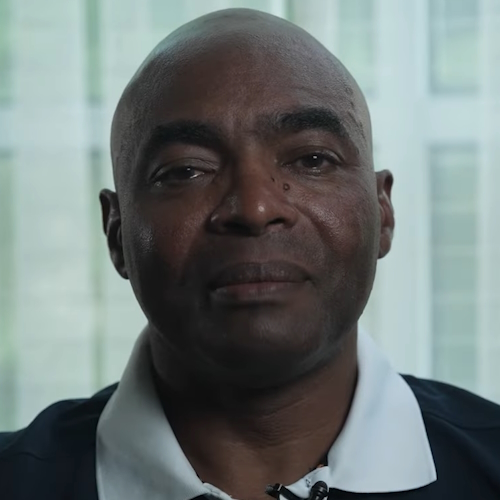
- Name: Mark K.
- Diagnosis (DX):
- Prostate
- Lung
- Bone
- Staging: 4
- 1st Symptoms:
- Inability to walk
- Tests for DX:
- MRIs
- CAT scans
- Biopsies
- Treatment:
- Chemotherapy
- 6 rounds
- Maintenance therapy
- Monthly injection for lungs
- Injection for bones every 3 months
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-Diagnosis
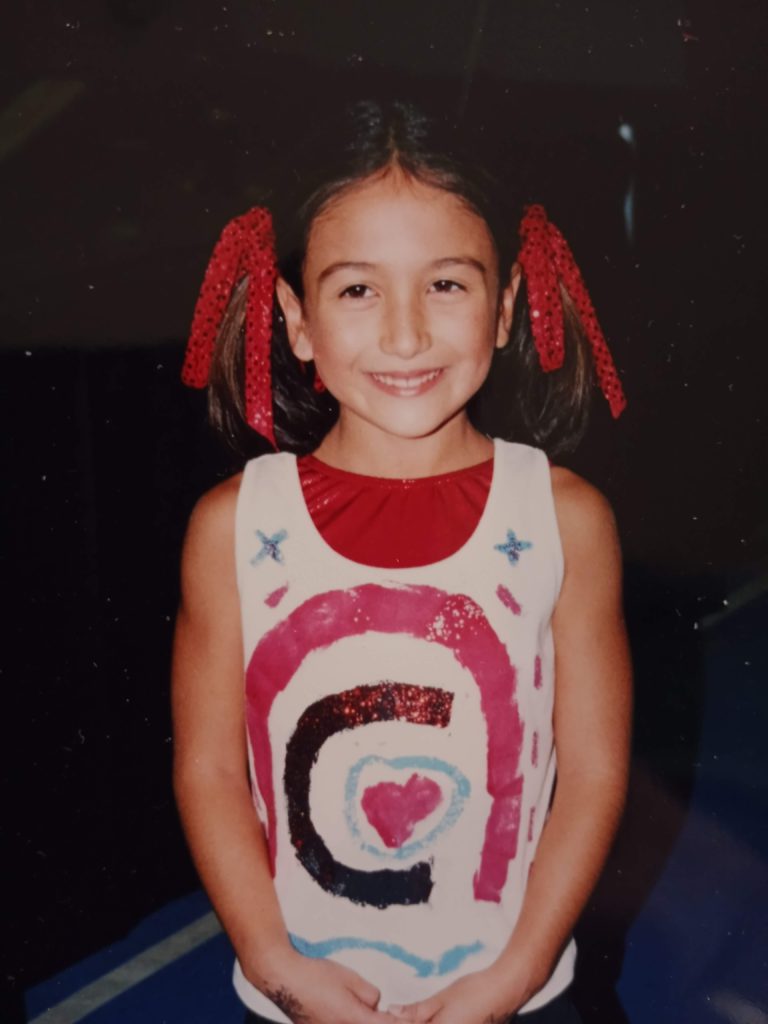
Introduction to Mark
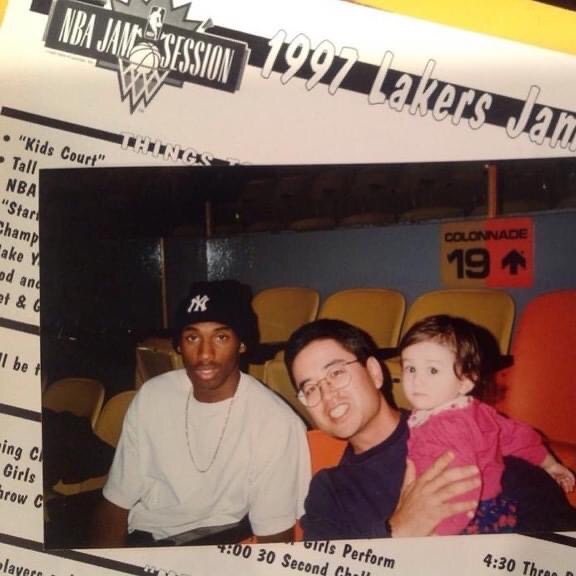
Prior to cancer, I was in great shape. I worked out at the gym 4 to 5 times a week, and I was really active. I was into sports, and I still used to play a little basketball. I used to be really into sport fishing and all that.
When cancer hit, it really affected me physically, not mentally. It actually made me much stronger mentally. Physically, I still deal with things, but I’ve gotten a lot better.
At my worst stage of cancer, I was barely able to walk across the room. It took me 10 to 15 minutes to walk across the room. It took me half an hour to take a shower. In 2021, I did not leave my room for 3 months.
I just was in my room because I physically couldn’t [leave]. I had a hard time. I’d go downstairs some, but not that much. It was an effort just to take every step. That’s what’s changed.
I’m just so thankful because we live in the hills. The very first time that I came down from my room after being in my room for 3 months, I opened up my front door, [and] it was just glorious. It was awesome.
When you haven’t seen the sun for 3 months, it’s indescribable, absolutely indescribable. That very first time I was able to open my door and go outside, it was just different. The sky was bluer. The trees’ leaves were greener. The birds were chirping loudly.
I just took everything in. You just notice and appreciate things so much more. That was my experience with that, and I still appreciate that to this day. I don’t take anything for granted.

Where do you live?
I live in Southern California, in the San Fernando Valley. [I was] born in Southern California, in Santa Monica, grew up in West Los Angeles, and moved to the Valley, which is 45 minutes away. I’ve been here all my life.
I have 2 daughters and they mean everything to me. My daughters are just so awesome. They were the driving force in my will to live.


1st symptoms
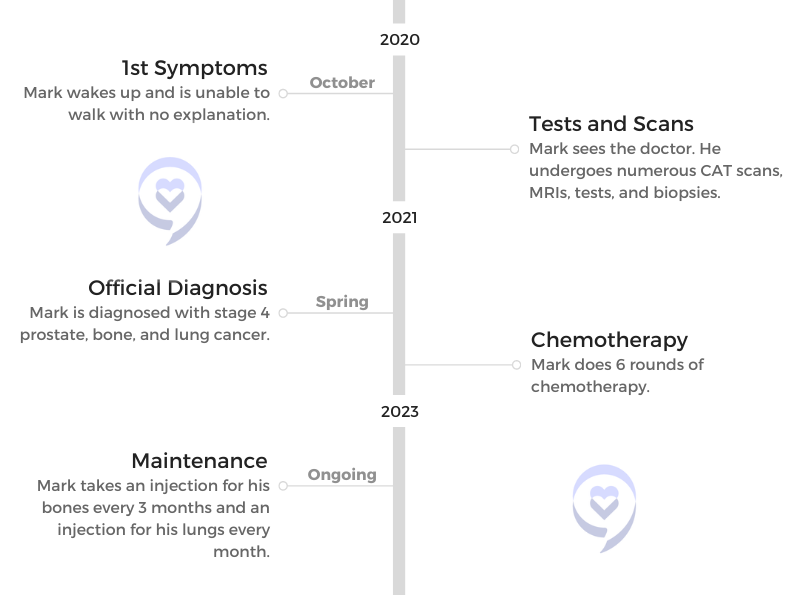
It started one day out of the blue in October of 2020. It just happened. Literally happened overnight. I woke up one morning, and I wasn’t able to walk.
My wife took me to the doctor. He kind of patched me up to the point where at least I could move around a little bit. That’s when I started doing a deep dive into my health and everything like that.
I knew something was wrong because they don’t put you through test after test after test after invasive test after inhumane, awful stuff without a reason. That’s when I knew something was really wrong because it just moved from one test to the other test. Initially 2 or 3 times a week, I was going through some type of procedure or something.
That’s when I started doing my deep dive into everything. I was thinking to myself, “Man, when is this going to end?” Because it was almost never-ending. There were tests, MRIs, CAT scans, biopsies. You name it, and I went through it. That’s what happened there.
Was not being able to walk a consistent symptom?
Yeah, it did last. It slowed me a lot. From October 2020, not being able to walk one day, and then as time went on, in the winter and the spring of 2021, that’s when I was in my room [and] having a difficult time. I started 6 rounds of chemo shortly after that. That didn’t help with things either.
The Cancer Diagnosis
How long did it take to get a diagnosis?
It was a long time. It was probably 3 or 4 months. I don’t know the exact time amount, but it was a long time because it was just a gauntlet of test after test after test.

What was going through your mind during this?
What was going through my mind was, “I just want to get some answers.” There was no doubt in my mind that there was something really wrong, but I just didn’t know what. That was just where we were at. It was just, “Let’s do this; let’s do that.”
Receiving the diagnosis
My oncologist called my wife and I into her office to give us the diagnosis. My wife took it one way, and I took it another way. My oncologist said, “Your cancer is so bad that I can’t cure you,” and she said, “I suggest that you get your affairs in order.”
My wife is like, “We’ve got to do this. We got to do that. We’ve got to get these papers done.”
I said, “Okay, I’ll do it.” Basically, I was kind of relieved that the oncologist told me that because I finally knew.
She also told me, “Yes, you have stage 4 prostate, bone, and lung cancer.”
I said, “Okay.” By that time, I had been preparing my mind for a while because of all these tests. Basically, in my mind, I knew something was really wrong. I didn’t know what. By the time she gave me the diagnosis, mentally I was ready for it.
From day one, I was just bound and determined. As far as I was concerned, dying was not an option. Period.
Mark K.
When she told me that, it basically set off a starting gun in my mind. I respect my oncologist, but I wasn’t about to buy into what she was telling me. I didn’t know how I was going to do it, but there was no doubt in my mind that somehow, some way, I was going to figure out how to win.
Telling loved ones about the diagnosis
I just told them. It was important for me to let people know and share it with people. [My family] were the first people I told. My older daughter, Lisa, the one who [stayed with me], said, “Okay, I’m going to come out and help you.”
Then my other daughter, Connie, lives in Texas with her husband, Matt. She came out as much as she could.


When you’re living it, our vision is outwards, so we see out. We don’t see ourselves. Even though I looked in the mirror, I didn’t realize the extent of what people saw me as. Lisa later told me that after seeing me that she was just really, really scared when she saw me.
From day one, I was just bound and determined. As far as I was concerned, dying was not an option. Period.
Looking back, did you have any symptoms before not being able to walk?
I had [the cancer] for a while, but I think what happened was when you’re working hard like I do — I’d go to the gym, and I’d go there for an hour and a half. I didn’t go there to socialize. I went there to work out. I pushed myself every single time I went to the gym, and I made the most of it.
When your body is that in tune for — I did that for decades, worked out that hard. Then when COVID hit, I wasn’t able to do that. I’m 64 now. I started to feel my age, and I started to feel things that I’d never felt before because I’d always worked out really hard.
I knew that it was going to be some kind of problem because, yeah, when you’re working out that religiously and that hard, I knew that things are going to start showing up. I just kind of felt that.
Relationship with oncologist
[My oncologist] and I started off with a very contentious relationship. You have an appointment with your oncologist, and it lasts 15 minutes. I’d always bring a notebook in and a pen to write things down. She would say, “We’re going to do this, or we’re going to do that.”
If it involved medication or anything like that, I would write it down. I would go research it, and I’d tell her that. I said, “Well, what do you want to do?” I’d want the names of everything. For instance, I wanted the exact name of the type of chemotherapy that she wanted to administer.
I got the name of it, researched it, and found out all about it. It’s a type of chemotherapy that’s been around for a while. It basically was as safe as a chemotherapy can be. Some of the chemotherapy, in their description is, “Hey, this can kill you.” I wasn’t going to have any part of anything like that.
One day I ran into my oncologist, and she was just so mad at me. Steam was coming out of her ears, and she says, “Why don’t you just do what I tell you to do?”
I was just real calm and real quiet. I just said, “Because I want to know exactly what you want to do and what it’s going to do.” Since that time, I’ve been on time or early to every single appointment. I’ve made every single hospital visit, every single test.
Over time, she realized how serious I was about living.

In fact, she wanted me to get on this medication. I said, “I don’t really want to do that.” She looked at me, thinking, “Here we go again.” I told her, “I’ll tell you what. I’ll make you a deal. If things go south, and the necessity arises that I need to take it, then I’ll take it. But I don’t want to take anything just to take something.”
She goes, “Okay, that’s fair. That’s fair.” She looked at all my test results recently, and she said, “Everything is either better or at least the same.” That’s really great. She said, “Okay, I’m good with that.” I said, “Fine, I am, too.”


Treatment Plan
Starting treatment
When I started my journey, once I got my diagnosis, I treated my cancer probably 50% conventional and 50% alternative/natural. Again, I stress that this is what I did because this is what I wanted.
For me, the chemotherapy played an important part in the fact that I needed to stop the rapid growth because it was in so many areas. It was in my prostate, it was in my bones, it was in my lungs, and probably in other places, too.
Because the cancer was spreading so rapidly, I decided to go. I didn’t want to, but I decided to do the 6 rounds of chemotherapy. It took a lot for me to do that because I’m really familiar with the effects of chemotherapy and things like that.
It’s non-discriminate. It goes after not only the cancer cells, but it goes after the good cells, too.



The first round that I took, I got so sick. I was sick for 4 days, and it was like being on a high that just wouldn’t go away. You couldn’t sleep it off. You’d wake up, and you’d feel just as bad or worse.
»MORE: Cancer patients share their treatment side effects
I called up the guy at the lab, and I said, “Man, if I get that sick again on round 2, there’s just no way I’m going to keep doing this. It’s just miserable.”
They said, “Just be patient. I think it will start kicking in on your second round.” That’s exactly what happened. From rounds 2 through 6, I was fine. Parts of my hair did fall out, but as far as the effects of feeling the chemotherapy, I was fine. That was good.

In the meantime, I was changing everything about my diet. I was working that, along with what I was doing with the chemotherapy. A very good friend of mine is a nutritionist. Up until this particular time, I was a vegan, and I thought, “Man, I have the greatest diet and all this kind of stuff.”
He said to me, “I’m going to give you a diet. I would suggest you follow it, because if you do, then I think you’ll be around in a year. But if you don’t, I don’t know what’s going to happen to you.”
That was a major, major thing for me to radically change everything about my diet. Here I am thinking, “I’m a vegan, and I’m healthy,” and all this kind of stuff, but why? If it’s that healthy for me, why do I have so much cancer?
I pondered that for the longest time, but when your back’s against the wall — and my back was. I had to make some changes, and radical changes. I said, “Okay, give me the diet, and I’ll follow it.” To this day, I still follow it.
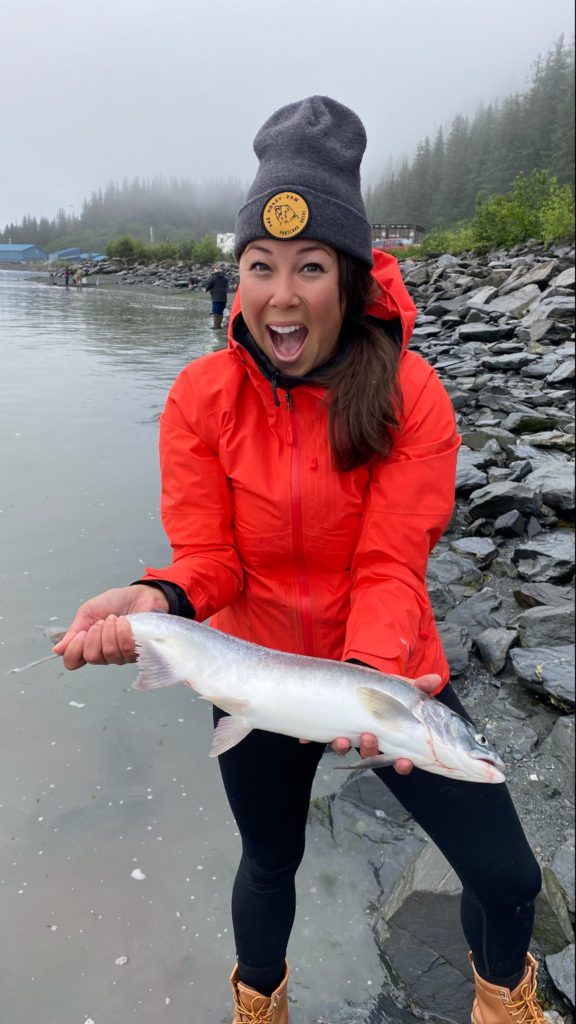
I added wild salmon. I added organic chicken, organic turkey, and organic beef. Then I changed some of the other things as well. I do a lot with my diet. It’s very, very complex, but in my opinion, that is what has saved my life, and that’s why I’m around today.
The ironic thing about it was my body craved it. I started eating it, and it tasted so good. It was really delicious. Again, I was down to 123 pounds. My daughter comes in. She stayed with me for 2.5 months and was cooking meals for me, and she was cooking up to 5 full meals a day.
She said that she would put a plate of food down, and I would eat it so fast she thought I was going to bite her hand.
I look back, and I would not have been able to put on the weight if I’d have stayed with my vegan diet. It just isn’t that way. By adding the protein and listening to him and doing other things — I’ve done a lot of other things — that’s what has made the difference for me.
What happened after your 6 rounds of chemo?
I did the 6 rounds of chemo. Concurrently with that, I started implementing my diet. I take a number of supplements. I was doing that every single day. Everything played an important role in all of this.
What I’ve done is I’ve treated my whole being. Not only the physical, but also the mental as well. I was working with a hypnotherapist from Cyprus. She helped me a lot and taught me a lot of things that I had no idea about, [like] working with the subconscious mind.
She told me that she looked forward to working with me because I already had the basis of the mindset necessary to accept everything that she was going to teach me. It’s worked out really, really well.
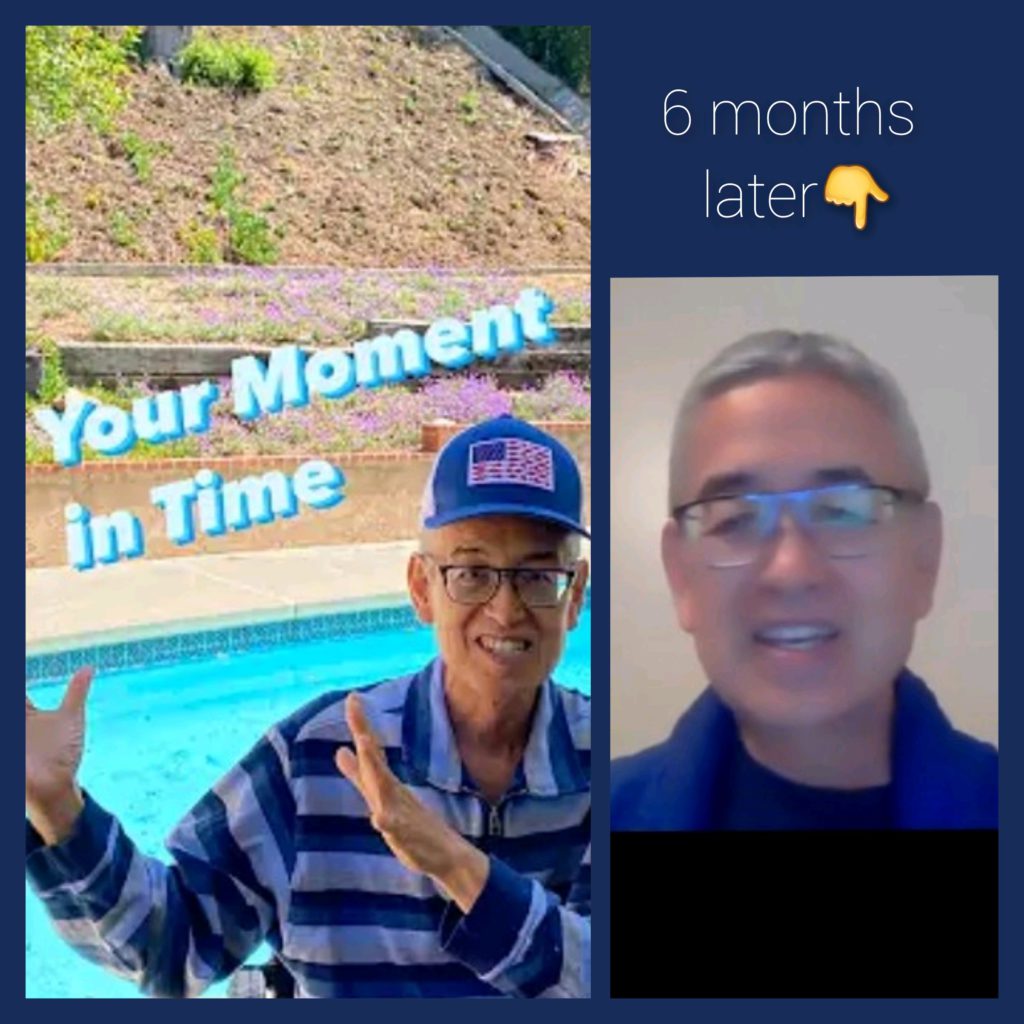
How are you doing now?
It’s going really well. When I started my cancer journey, my PSA for my prostate, which is the marker for prostate cancer, was almost 1,000. My oncologist said she had never seen anything remotely that high.
What I basically did was I targeted the 3 main areas of my cancer: my prostate, my bone, and my lungs. As far as my prostate goes now, my PSA is down to 0.6 from almost 1,000.
Then my lung cancer, I saw an actual scan of my lungs. There’s supposed to be 2 white entities, and these 2 white entities had black blobs floating through all of it. That’s the way I started my lung cancer journey.
I’ve taken some things that have really, really helped in my lung cancer. My lungs are doing much better. I don’t know exactly where they’re at, but compared to when we started, they’re like light years better.
The same thing with my bones. I still have some cancer in my bones, but the metastasis has stopped, and things have gotten much better. I haven’t used any prescription meds for pain at all through this whole journey. I do CBD and other things as well.
Are you on any maintenance therapy?
I do take an injection for bones once every 3 months, and then another monthly injection for my lungs as well. That’s about it. I do it with my diet and my supplements and my mental exercises and things like that.


Reflections
Importance of self-advocacy
It goes back to societal norms. We’re all taught that you always listen to your doctor. Then the second part of that is when people hear the word “cancer,” what do they automatically think? You’re going to die. Majority of people think that way.
Those are things that we’re taught from a young age as a society. I talk to people all over the world, and all over the world, the perception is the same. Absolutely the same.

I tremendously respect doctors, my oncologist, and everything like that. I give them respect. They do know what they’re doing with what they have in front of them.
To me, 15 minutes, which is the treatment time that most patients receive, is not enough time to get to know that person. One of the main things when a person gets a diagnosis is does that oncologist really know the makeup of that person? Does that oncologist know how that person is going to react?
My oncologist has come to know me over time, but at first, it was just basically telling me, “Shut up and get in line.” I wasn’t having that. I respect what she has said, but I wasn’t buying it as me. That’s not me.
I didn’t know, when I started, what was going to happen, but I put in my mind that if there was any way possible on this earth, I was going to live. I look at the obituaries. I glance through them every day, and I said, “There’s no way my name is going to be there. No way.”
The message that I share with as many people as I can is you need to be you in this journey. If you feel that you have the fight to do this — and it is a battle. There’s no doubt about it. The biggest battle that you’re going to have as a cancer patient is [mentally]. That’s the biggest battle.
For me, I wouldn’t wish cancer on anyone, but cancer has changed my life for the better. It’s just opened my eyes to so many things. I appreciate things that I just took for granted. I took for granted so many things.



I used to walk out my front door, and it was like I didn’t even think about anything. Now, I open my front door, I look outside, and I really, really love and appreciate the simple things.
I reflect back and I realized that when you’re in your room for 3 months and you’re isolated like that, to have the ability to walk outside is such an incredible blessing and such a great thing.
My pet peeve is these doctors and oncologists give these diagnoses: “You have 6 months to live. You have a year to live.” People buy into that number, and it drives me out of my mind. I meet so many people, and I hear stories of relatives and friends who were given diagnoses, and they died almost to the day, so many to the day of the diagnosis.
The mindset is so, so crucial and so, so important, because you do have the ability to plow through and make it.
»MORE: How to be a self-advocate as a patient
The mental battle against cancer
I want people to live. I want people to beat cancer. But the only way that you can beat cancer is if you don’t let it beat it up here [in your head]. Once you accept something less than living, then you’ve lost. Have that mentality with it, because there’s no doubt about it. This cancer is a battle.
It’s a battle from all different directions. There are so many different things that a person needs to deal with. The two main things that you have to take care of is your mind and your body. It’s so critical to realize that.
[For] so many people, there’s nothing wrong with [thinking], “Why did this happen to me? Why am I going through this?” But you cannot dwell on it. You have to dwell on how to make it better. How do I overcome this instead of feeling sorry for myself?
Did I feel sorry for myself? Yeah, probably about an hour. The conclusion I came to was, “I’ve gotten cancer for a reason, and the reason is because I could handle it.” I knew I could handle it. God doesn’t put anything in front of you that you can’t handle. After that hour, I knew that somehow, some way, I was going to be able to break through.



I started my YouTube channel when I was really in bad shape. I’ve been able to put up a video every single week. I started my channel because I wanted to help one person, and the one person that I helped the most was me.
These are the days that I wanted to be around for.
Mark K.
Last message for patients and caregivers
If you get diagnosed, whatever you’re afflicted with — whether it’s heart disease, cancer, or autoimmune disease — the journeys are different. But in a lot of ways, they’re the same because in order to get better, the mind is so critical, and [so is] actually really believing that you can get better. If you don’t believe that you can get better, nobody else is going to believe that.
It’s your life. When you go to the doctor and they tell you, “You have 6 months to live,” they are concerned about you, I’m sure. But who’s going to care more about your life, you or your doctor? It’s you. That right there should tell you that it’s on you to do everything that you can to find the answers so that you can keep living your life and making a great life.



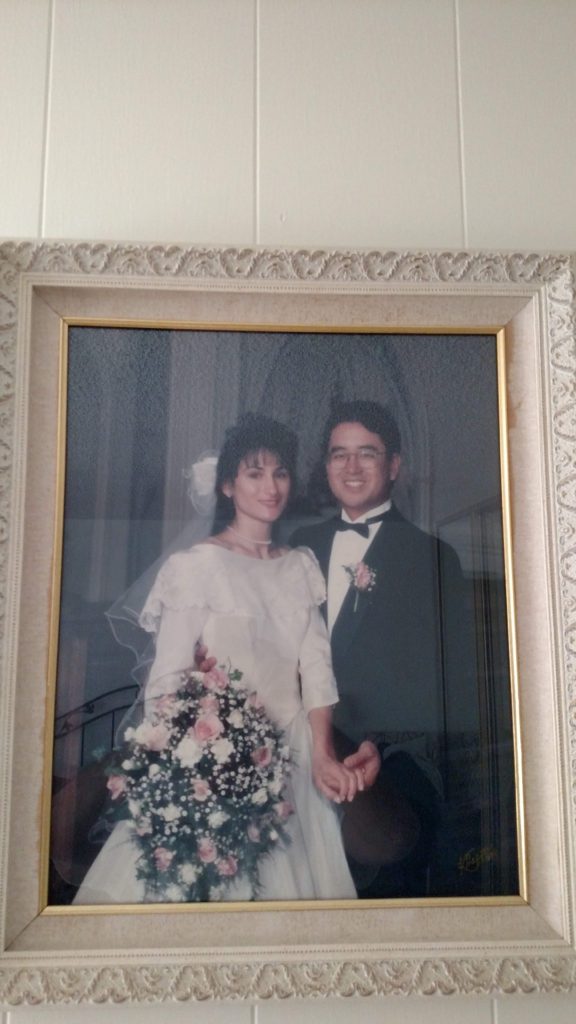
I’m just so, so happy every single day. I’m so fortunate to meet so many incredible people. At this point, there’s no doubt in my mind I’m going to be around for a while. [My daughter’s wedding] was back in October. I was just looking out and reflecting. It was up at her mother-in-law’s ranch up in Santa Maria. It was really, really great, but the thing that was so awesome was the fact that I just reflected, “These are the days that I wanted to be around for.”

Inspired by Mark's story?
Share your story, too!
More Prostate Cancer Stories
Paul G., Prostate Cancer
Symptoms: None; elevated PSA levels
Treatment: Prostatectomy (surgery), radiation, hormone therapy
Mark K., Prostate Cancer, Stage 4
1st Symptoms: Inability to walk
Treatment: Chemotherapy, monthly injection for lungs
Mical R., Prostate Cancer, Stage 2
Symptoms: No symptoms, caught at routine physical with PSA test
Treatments: Radical prostatectomy (surgery)
Jeffrey P., Prostate Cancer, Gleason 7
Cancer Details: Diagnosed at 59, biopsy had not detected it
1st Symptoms:None, routine PSA test, then IsoPSA test
Treatment:Laparoscopic prostatectomy
Theo W., Prostate Cancer, Low-End High-Risk
Cancer details:
Low-end high-risk prostate cancer, early kidney cancer
1st Symptoms: PSA level of 72
Treatment: Surgery, radiation
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Cancer Details: Staged Gleason score 9
1st Symptoms: Urinating more frequently middle of night, slower urine flow
Treatment: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Gleason 8/9, Stage 4A
Cancer Details: Staged Gleason 6/7 pre-surgery, post-surgery changed to 8/9, PSA level at 27
1st Symptoms: Urination changes, brother's prostate cancer diagnosis
Treatment: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Al Roker, Prostate Cancer, Gleason 7+, Aggressive
Cancer Details: Aggressive but caught early
1st Symptoms: No symptoms, caught at routine physical with PSA test
Treatment: Radical prostatectomy (surgery)
Steve R., Prostate Cancer, Gleason 6, Stage 2-4
Cancer Details: Started at stage 2 and gradually progressed to stage 3, and then to stage 4 with metastasis to lymph nodes
1st Symptoms: Rising PSA score
Treatment: IMRT (radiation therapy), brachytherapy, surgery, and lutetium-177
Clarence S., Prostate Cancer, Low Gleason Score
Cancer Details: PSA levels fluctuated but were never extremely elevated, cancer contained to prostate
1st Symptoms: No symptoms, caught at routine physical with PSA test
Treatment:Radical prostatectomy (surgery)