Keith Guernsey’s Multiple Myeloma Story
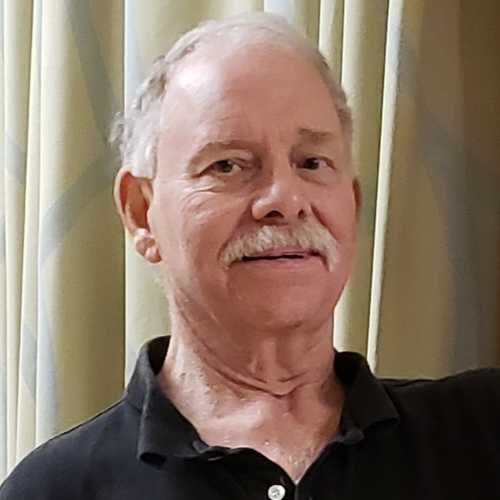
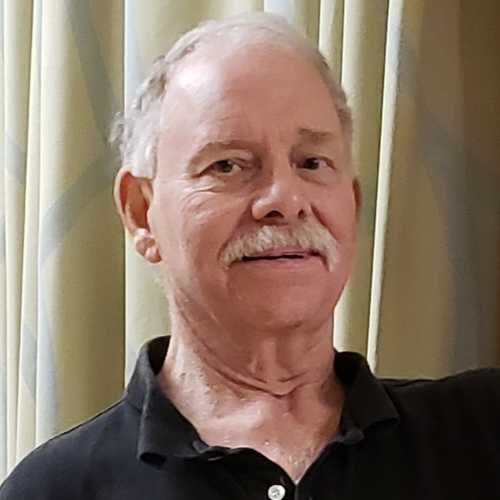
Keith Guernsey, a retired sales executive turned author, shares his personal cancer journey, including his diagnoses of prostate cancer, multiple myeloma, and melanoma. He and his wife, Susan, reside in Gainesville, Georgia, enjoying their retirement in an active adult community. Despite facing various health challenges, Keith remains optimistic and determined to live a long and fulfilling life.
Keith’s journey began with a diagnosis of prostate cancer in 2018, followed by successful robotic surgery. However, his medical journey took another turn when high levels of protein were detected in his blood, leading to a diagnosis of multiple myeloma, a rare blood cancer. Keith highlights the importance of having a strong support system, crediting his wife as his source of strength and motivation throughout his treatment.
Keith underwent treatments, including RVd infusions and a stem cell transplant, at Northside Hospital’s blood marrow transplant group. He praises the doctors, nurses, and staff for their exceptional care and expresses gratitude for their support. Despite experiencing side effects such as orthostatic hypertension, Keith remained committed to his recovery.
With the conclusion of his myeloma treatment, Keith reflects on the emotional moment when he received a certificate of congratulations from the BMT offices. He attributes his ability to recover quickly to his previous years of regular exercise and determination. Keith focuses on finding the right treatment and maintaining a positive outlook.
At The Patient Story, we chronicle real-life cancer experiences directly from patients. Read more multiple myeloma patient stories.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Keith G.
- 1st Diagnosis:
- Prostate cancer
- Initial Symptoms:
- Enlarged prostate (noticed by PCP at annual checkup)
- Treatment:
- Surgery: prostatectomy (prostate removal)
- 2nd Diagnosis:
- Multiple myeloma
- Initial Symptoms:
- High levels of protein (seen in post-op follow-up blood work)
- Treatment:
- RVd (Revlimid, Velcade, dexamethasone)
- Stem cell transplant
- Maintenance:
- Revlimid
- IV infusion
- Xgeva
- 3rd Diagnosis:
- Melanoma
- Initial Symptoms:
- Lump on the back and right clavicle
- Treatment:
- Surgery
- Opdivo
- Introduction
- Pre-diagnosis
- First cancer diagnosis: prostate cancer
- Second cancer diagnosis: multiple myeloma
- Going into a fog of denial
- Importance of having a support system
- Treatment for myeloma
- Preparing for stem cell transplant
- Side effects from RVd
- End of myeloma treatment
- How did you feel seeing that welcome home banner?
- Maintenance treatment post-stem cell transplant
- Follow-up protocol with hematologist-oncologist
- Third cancer diagnosis: melanoma
- Living life after 3 cancer diagnoses
- Words of advice
Introduction
We live on Lake Lanier in Gainesville, Georgia. I’m originally from Lexington, Massachusetts. I was diagnosed with prostate cancer in 2018, multiple myeloma in 2019, and melanoma in 2021.
I am 70 years young although, today, I feel like I’m 30. I am a retired sales executive turned author. I am incredibly fortunate to be married to the lovely and talented Susan.
We’re in an active adult community. We’ve been retired and here for close to a decade and we love it. This is our base of operations.
We love to travel, usually with our spoiled little doggy in tow. We go to St. Simons Island a lot. The only exception is when we get on a plane to go see [our] son, daughter-in-law, and two grandkids back in Boston.
Before cancer hit, I was diagnosed with a benign brain tumor called an acoustic neuroma. I had 10 hours of successful surgery back in 1995.

How did you meet your wife?
I made the most important decision of my life [in] 1996. I know it’s going to sound strange to hear that, but just going to the corner store and buying a newspaper was the most important thing I’ve ever done.
I had been alone for 15 years and I was getting bored, lonely, and in a rut. [I] opened up the personals and one caught my eye. It said, “WWWF.” I had no idea what that meant, but it stood out. I was curious.
I took a chance and dialed the number. A nice young lady answered the phone. We had a very pleasant hour-long conversation [and] talked about who we were, what we did, etc.
I finally got up the courage to ask what WWWF was and she said, “Widowed, white female.” I said, “What about the third W?” She said, “Well, it must be a typo.” Later I would learn that it was for “wonderful.”
Unfortunately, I’ve had to put her through a lot. When I say, “You are the strongest person I’ve ever known,” she kind of gets a look on her face like, “I’m not really.”
We met in ’96. About six months after we met, the first gift I gave her was to have to sit through 12 hours of excruciating brain surgery because my tumor came back. Then we had 20 uninterrupted years of wonderful times [and] lots of travel.
Then [in] March 2018, I was diagnosed with prostate cancer. I had to wait six months for the robotic equipment to be available. For me, waiting six minutes is hard, [what more] six months.
The phone rang. I don’t know why, but I had a premonition that something might be amiss.
Pre-diagnosis
What led you to visit the doctor?
[I was getting my] yearly prostate checkup. My primary care physician noticed I had an enlarged prostate. He sent me to the urologist. I wasn’t concerned, but it turned out I should have been.
I was diagnosed with prostate cancer [and] had successful robotic surgery in September. I even remember dancing out the door. If you’ve never seen an uncoordinated old guy dance, it’s a sight to behold.
First cancer diagnosis: prostate cancer
Getting the official diagnosis
It wasn’t pleasant. We were sitting down to lunch and the phone rang. I don’t know why, but I had a premonition that something might be amiss because very few people call us at lunchtime. [From] the expression on my face, Susan was just about ready to take the phone away from me.
I got my composure back. He said, “You have prostate cancer. You need to come [into] the office and we’ll discuss the options.” They talked about radiation, seeds, and all that stuff. I said, “No, I want it out of me.”
He scheduled the surgery. But again, it was six months from the time he diagnosed me to he performed [the] surgery.
Susan’s been my sole caregiver through this entire journey. God bless her. She’s just been phenomenal.
Waiting for the prostatectomy (prostate removal surgery)
It was not easy. I wasn’t pacing the floors but, short of that, we had all kinds of activities.
I’m always writing so that took up a lot of my time. That takes me away mentally from worrying about cancer.
I tend to take my cue from my doctors. I’ve been very fortunate. My doctors are the best of the best. If they express deep concern, I get really concerned. I try not to because you pass that concern along to Susan and then she’s concerned.
In addition to writing and reading, I try to do activities and keep busy. I really didn’t have a choice. You just do what you can to keep busy. Then September rolls around and you’re ready. Sort of.
Susan’s been my sole caregiver through this entire journey. God bless her. She’s just been phenomenal. She hasn’t had to call back to Boston for reinforcements of other family members, but we came close once or twice.
It’s not in my nature to be super patient, but I’m really trying hard to be at least a little better.
Real high levels of protein in my blood. Now, I don’t know what that meant, but the expression on my urologist’s face meant it wasn’t good.
Post-surgery
I missed the Braves game that night but, hey, sacrifices have to be made. But [the surgery] went fine. I felt great. Came home a couple of days later, jogged out of the hospital, and everything was wonderful until a follow-up lab work two or three months later.
I was ready to start the last third of my life, healthy and happy with my lovely wife at my side. We’re going to travel the world and life was so good. Then reality intruded.
Real high levels of protein in my blood. Now, I don’t know what that meant, but the expression on my urologist’s face meant it wasn’t good. He referred me to a hematologist.
I promised Susan that no matter what happened, medically speaking, I would live to be 95 so that we could dance at our 50th wedding anniversary.
Second cancer diagnosis: multiple myeloma
The hematologist was right across the hall, which is nice. Not only was she right across the hall but she was, in my opinion, the best of the best. She was really phenomenal.
We went in on March 27th for our initial discussion. Susan and I were fortunate to be accompanied by a very dear friend of ours — 40 years in nursing [and] 20 years as the assistant director of oncology at our local hospital. She was a rock and able to translate all of Dr. Nadella’s medical terminology into layman’s terms for us.
Dr. Nadella said, “You have multiple myeloma, which is a rare blood cancer.” I didn’t know until we walked into her office. You just deal with it.
Going into a fog of denial
I did [go into a fog of denial], especially when she said, “At this time, there is no cure.”
She’s a straight shooter and I really admire that about her because there’s no beating around the bush with her and I appreciate that. I’d rather have it that way. I’d rather have honesty.
She went on to say, “With proper treatment, you can still live a long, healthy, and productive life.” I promised Susan that no matter what happened, medically speaking, I would live to be 95 so that we could dance at our 50th wedding anniversary.

Importance of having a support system
We’re a team and we do this all together. It made all the difference in the world. I get my strength from her. Hopefully, she gets a little from me.
We were both in shock. We went home and mapped out our strategy to deal with it, which is day by day.
We follow the facts and we follow the doctor’s instructions. Once you’ve found what you consider the best, listen to her. She steered me on this path and I feel great.
If you go on the Internet and you say, “How long can you live with multiple myeloma,” it’s like five years. I talked to a woman recently. She’s been living with myeloma for 31 years.
If I get 31 years, I will have accomplished my goal, which is to be one of the few three-time cancer survivors to live to be 100.
Treatment for myeloma
It was every three weeks or so for the RVd infusions, but those are mostly things that can be taken at home. I was very fortunate that my system accepted those three drugs readily and I really didn’t have any problems.
I had one fall. I put my elbow through the wall. But beyond that, nothing.
After about three months, she said, “We’re going to send you down to Atlanta, to the BMT group,” which was part of Northside Hospital blood marrow transplant group, “to make sure that you are a viable candidate for stem cell transplant.” Fortunately, I was.
This is in June. Since then, I went home, [received] more treatments, packed up [our] bags mid-August to come back for nine weeks of more treatments, more IV infusions daily, and then the stem cell transplant.
The doctors, the nurses, and the staff that I have had the pleasure of working with have been phenomenal.
Preparing for stem cell transplant
He didn’t say a lot. Dr. Sohl, [whom] I was seeing, was the resident expert. He’s another great, great doctor. He did a phenomenal job.
Very, very, very easy process [of] collecting the blood and then putting it back in me. Very smooth transition.
Northside is very large. It’s not a community hospital, certainly, but it is, along with Emory, one of the two de facto standard cancer hospitals in the Atlanta area.
They treated me so well. I have been very fortunate. The doctors, the nurses, and the staff that I have had the pleasure of working with have been phenomenal. I got a chance to thank them publicly [on] the local news.
Side effects from RVd
It was such an easy process. However, there was one glitch in my treatment: orthostatic hypertension.
Your blood pressure is within normal range when you’re lying down [and] when you’re sitting up, [but] when you stand up, your blood pressure drops [to] dangerously low levels so you need to sit right back down.
It can cause dizzy spells and falls. One night, I fell six times trying to get up. I’ve been very fortunate to be a former football and hockey player who actually learned to fall gracefully if that’s even a thing — not hit my head, not panic, that type of thing.
I would caution anyone. Take your standing blood pressure or have someone take it for you. That was the real only problem.
The stem cell transplant went fine. I had a little problem after that with the medication they were giving me. They thought I was having a stroke. I couldn’t get out a word or a sentence. But it turns out, it was the mix of medications they gave me.
A doctor came in and said, “Once you sleep it off, once it wears off in the morning, you’ll be fine.” That was four years ago and I haven’t stopped talking since.
Once they tell you cancer, there’s not a lot you can do about it except get good treatment.
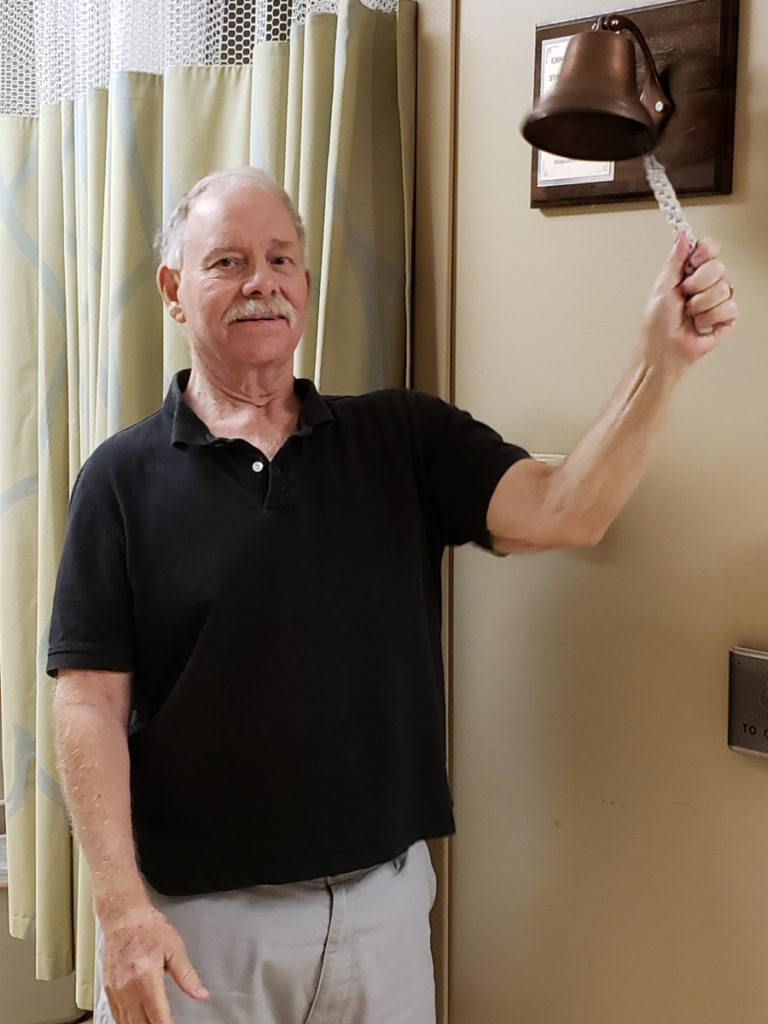
End of myeloma treatment
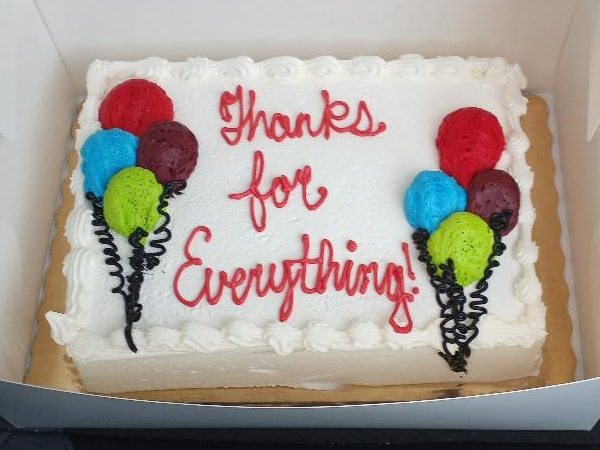
On November 1, 2019, we walked into the BMT offices for the last time. They handed me this certificate. It says, “Congratulations.”
I was trying as best I could to maintain calm so I wouldn’t worry myself and I wouldn’t worry Susan so much. Because once they tell you cancer, there’s not a lot you can do about it except get good treatment. I remained fairly calm for both of us.
We drove home and it was euphoric. We pulled into the driveway and this banner that says, “Welcome home, Keith!” was stretched across our garage door, signed by neighbors and friends. I lost it. I started crying like a baby. Susan joined me, got the walker out of the car, [and] went into the house.
After weeping like babies, we cultivated a plan to get me back to my current strength. I’m convinced that my ability to get better faster was in large part due to my six previous years in the gym — every morning for an hour — and that helped me out.
Started walking with a walker, then a cane and I was holding Susan, and I started walking on my own back to the gym, [and] running on the treadmill.

How did you feel seeing that welcome home banner?
We were done with that portion of the treatment. More than that, we had so many caring, loving friends and family members all over the country.
Emotion just swept over me. It’s often hard for me to describe but after I was all cried out and pulled it together, we sat down and started talking [about] what we needed to do to get me back to where I am today.
Nutrition and exercise were two of the largest components of that plan.
Maintenance treatment post-stem cell transplant
I was on a maintenance Revlimid, which is basically a pill a day, and I would go about every month for an IV infusion and Xgeva shot.
One of [the] problem areas of multiple myeloma is it can weaken your bones. Fortunately, I didn’t have any of that. I think a lot of that is due to the good care that Dr. Nadella and her team did.
You rely on your resources, like your medical team, and just realize that you can live as normal a life as possible with multiple myeloma or other forms of cancer.
Follow-up protocol with hematologist-oncologist
I go in either once a month or once every couple of months. I’m still in what she calls very good remission. She’s always told me that remission is almost a vague term [and] that if you ask six hematologists, you get six different versions of what remission is. It’s a moving target, so to speak.
[I had] my last treatment and I’m feeling wonderful.
I’ve talked to a number of myeloma patients who have lived a very, very long time. I know I’m under the best medical care. I have an ace in the hole.
Even with myeloma in remission, if I get 31 more years, if I get 21 more years, I’ll be thrilled. I don’t know if Susan will be able to put up with me that long, but I guess we’ll find out. But you take it one day at a time.
You do the best you can to cultivate and maintain a positive attitude. You rely on your resources, like your medical team, and just realize that you can live as normal a life as possible with multiple myeloma or other forms of cancer. You want to make sure you’re not letting it beat you. You want to make every effort to beat it.

Third cancer diagnosis: melanoma
What led to this diagnosis?
I had a lump on the back of my neck. I think I’m too old to have a pimple so I know it wasn’t that.
I had it checked and they found out that [it] was [a] malignant melanoma. I also had it in my right clavicle.
I was diagnosed in October 2021. I found the best melanoma specialist in the world, Dr. Nicole Kounalakis, and she took it all out in a six-hour operation in North Side. Again, I was able to bounce back pretty quickly because she did such a great job.
Getting the official diagnosis
It’s interesting because three different people gave me three different answers about what stage I was at.
Dr. Kounalakis’ PA said stage 2, Dr. Kounalakis said stage 3, and Dr. Nadella said stage 4 so it’s a toss-up. As long as I’m having fairly regular CAT scans and PET scans and as long as I don’t see the words metastatic or terminal, I don’t worry about it.
I’ve been told it can be sneaky. It can come back. I talked to Kounalakis and said, “If it comes back, will I need more surgery?” She said, “Yeah, you might,” and she said it confidently that if she’s not worried, I’m not worried.
Treatment for melanoma
I was on Opdivo, which is [an] immunotherapy, and I was on it for a year. That worked because, [on] October 28th, Dr. Nadella said, “This will be your final treatment,” and that’s been it.
No treatment and feeling phenomenal. It may not always be that way, but I mentally prepared myself for whatever comes next.
It’s one of those things where you don’t [have] to love it, you just got to do it.
Living life after 3 cancer diagnoses
It wasn’t bad because it gives me a chance to get out and actually see people. The medical professionals I’ve seen are phenomenal, efficient, helpful, professional, [and] friendly.
When I was a kid, [I] hated going to doctors. Now I actually enjoy it. I get out of the house. I get to meet some very nice people. They do what needs to be done and I come home.
It’s one of those things where you don’t [have] to love it, you just got to do it.
What’s been the biggest surprise after going through all this?
I’m surprised [at] how good I feel. I look at my driver’s license and it says I’m 70, but I don’t feel 70. I feel about half that [almost] every day.
There are moments [when] maybe I didn’t sleep well the night before. I would have you where I’m not quite 100%. But by and large, I’m pleasantly surprised by how great I feel.
That’s why I want to give back to my fellow cancer patients, whether it be [through] the American Cancer Society or as a myeloma coach.
Were there any moments when you felt, “Why me?”
I really haven’t because I feel like God called on me because I’m strong and with the help of family and friends, I would get through this, and I have.
Susan has a book. The cover says, “God doesn’t give you anything that you cannot handle,” and I feel that’s the case for me.
There’s always a moment of that type of thing, but I try not to dwell on it. I move past it and move on with my life. From time to time, you have your doubts. Everyone does. If I didn’t, I wouldn’t be human. But I try to minimize them, if at all possible.
Sometimes when I’m alone, I think about why did He do it to me three times. The answer I always come back to because He knew I was strong enough to handle [it].
It’s a delicate balance between keeping it moving and getting back in good physical shape and going too fast.
Words of advice
I developed a nine-point plan, which I call, “Living Well with Cancer,” which has helped me and a lot of my fellow cancer patients. I’m a myeloma coach and an Imerman Angel, so I speak a lot to new cancer patients or less experienced cancer patients.
It talks about things like nutrition, exercise, hydrating properly, [and] getting a good night’s sleep. I’ve sent it to dozens of cancer patients. They’ve all said it’s worked well for them and it’s been inspirational.
It’s not easy. I have a friend who’s a retired cardiologist who told me this. It’s easier if you cultivate and maintain a positive attitude. It goes a long way to help you beat cancer and get better every day.
You can be upbeat or you can be downbeat. It’s not easy but with the help of Susan, our little doggy, and my family and friends back in Boston, I have been able to maintain and cultivate a positive mental attitude. I’m convinced that has helped me so much.
Be patient. Get up slowly and go slow. With everything you do, be patient. Pay attention to the metrics with orthostatic hypertension.
Just be careful. Move slowly. It’s a delicate balance between keeping it moving and getting back in good physical shape and going too fast — that’s when you could hurt yourself.
Be careful. Get the best medical care you can. Keep moving, but do it slowly.
We have a finite amount of time on this planet. Do your very best to enjoy every moment, every day to the max. I know it’s not all that easy, but you have to do the best you can.
Inspired by Keith's story?
Share your story, too!
Multiple Myeloma Stories
Clay D.
Diagnosis: Multiple myeloma
1st Symptoms: Persistent kidney issues, nausea
Treatment: chemo, radiation, stem cell transplant
...
Melissa V.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Frequent infections
Treatment: IVF treatment & Chemotherapy (RVD) for 7 rounds
...
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatment: Chemotherapy (Bortezomib/Velcade), Daratumumab/ Darzalex, Lenalidomide, Revlimid) and stem cell transplant
...
Ray H.
1st signs: Hemorrhoids, low red blood cell count
Treatment: Immunotherapy, Chemotherapy, Stem Cell Transplant
...
Valarie T.
Symptoms: Nose bleeds, fatigue, back pain
Treatment: Chemotherapy, stem cell transplant
...
Julie C.
Symptoms: Queasiness, food aversions, lack of appetite, fatigue
Treatment: Stem cell transplant, chemotherapy (D+PD), bispecific antibodies (talquetamab & cevostamab)
...
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...