Lisa’s Stage 4 ROS1+ Non-Small Cell Lung Cancer Story
Lisa is a passionate patient advocate for ROS1+ lung cancer patients after she was diagnosed with stage 4 at just 45 years old.
In her interview, Lisa talks about dealing with the stigma of lung cancer despite being a never-smoker, undergoing chemotherapy and targeted therapy, how she dealt with cancer as a parent, and the kind of support that has been the most important.

- Name: Lisa G.
- Diagnosis (DX):
- Non-small cell lung cancer (NSCLC)
- ROS1-positive (ROS1+)
- Stage 4
- Non-small cell lung cancer (NSCLC)
- Age at DX: 45
- 1st Symptoms:
- Persistent cough (months)
- Coughing a little blood
- High fever
- Night sweats
- Misdiagnoses:
- Common cold
- Bronchitis
- Irritated airwaves (to explain the blood in cough)
- Treatment:
- Chemotherapy: cisplatin + bevacizumab (Avastin) + pemetrexed (Alimta)
- 4 cycles
- Cycle = 3 weeks
- Given over ~12 hours in one day
- Maintenance chemotherapy:
- Bevacizumab (Avastin) + pemetrexed (Alimta)
- 4 cycles
- Cycle = 3 weeks
- Given over ~6-8 hours in one day
- Bevacizumab (Avastin) + pemetrexed (Alimta)
- Targeted therapy: crizotinib (Xaltori)
- Chemotherapy: cisplatin + bevacizumab (Avastin) + pemetrexed (Alimta)
Know that if you’re Googling the prognostics or predicted survival curves for stage 4 lung cancer, please set that aside. Most of that information is outdated.
These new treatments, whether it be targeted therapy or immunotherapy or customized vaccines — whatever else is coming out there — are really dramatically shifting survival rates.
Have some hope and positivity because I’m nothing if not living proof that those predictions aren’t always true.
Lisa G.
- Diagnosis
- How did you get diagnosed?
- What happened at the primary care doctor visit?
- When did your symptoms worsen?
- Describe the ER visit
- You got a second opinion from a family friend
- Describe the pulmonologist visit
- The surgeon didn't sugarcoat the diagnosis
- What were you feeling when you were diagnosed?
- What was it like being on oxygen 24/7?
- Treatment Decisions
- Chemotherapy and Side Effects
- Targeted Therapy
- Reflections
- How do you talk to your kids about the cancer?
- Any advice for other parents dealing with diagnosis?
- Seeking out professionals
- How did you find the professionals?
- What's your advice to people dealing with a new diagnosis?
- What was once considered "incurable" is changing
- How did you manage the emotional stress?
- What has helped you deal with the toughest stuff?
- Family has been a big part of the journey
- Support came from those who've been through their own trauma
- Support also came from unexpected places
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
How did you get diagnosed?
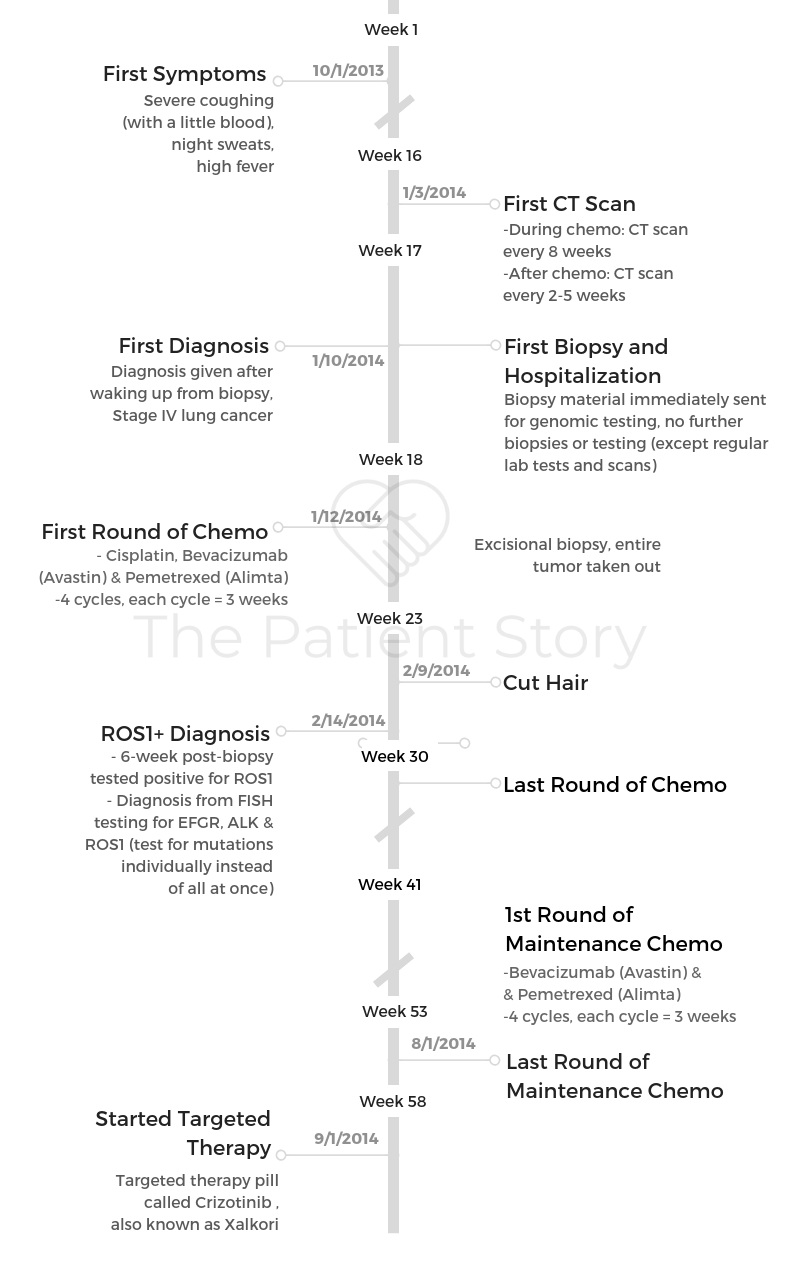
Summary: I was misdiagnosed with a cold and bronchitis for months. By the time I was diagnosed, I had 3 broken ribs from coughing so hard, night sweats, fevers, and was coughing up a little bit of blood. I had undergone multiple X-rays when I should have gotten a low-dose CT scan. That would have shown the cancer.
I rarely got sick or went to the doctor, but I had had a persistent cold and cough for several weeks and finally decided to go to the doctor. I hate taking even antibiotics because I want to save them for when I really need them.
I’m not the type to run to the doctor to get those. It took a lot, probably a month, and finally I dragged myself there and went to my first appointment with the urgent care because it was over a weekend, and my friend said just go and get some antibiotics.
So that’s what I did. I went to the urgent care that just happened to be open on the weekends, and they did a quick X-ray of my lungs. They gave me antibiotics and codeine cough syrup to stop the cough. They said the X-ray looked totally clean.
This was in October. I was very physically fit. I was teaching about 5 spin classes a week and all kinds of other exercise classes, eating healthfully, and all that stuff. I took those medications and didn’t get better. In fact, I got a little worse.
What happened at the primary care doctor visit?
Then I went to my primary care doctor in mid-November a couple weeks later and said, “The coughing is getting worse.” She took a listen to my lungs, just did a quick exam, and said she thought it was still just a garden-variety type of bronchitis or something.
She gave me a different kind of antibiotic and an inhaler. It was the first inhaler I’d ever had in my life.
I never had asthma or allergies, anything like that. Now, looking back, I wish I had pushed back a little bit more and said, ‘Why are you not looking further into something and treating something I have no history of?’ But that’s what we did.
I went home with this inhaler and some other medicines and tried that for a few weeks. It wasn’t getting better. I went back again in the beginning of December, and again, same routine. She just upped the level to a more heavy-duty inhaler with steroids, and it still didn’t work.

When did your symptoms worsen?
I started coughing up blood. This was mid-December. I wanted to check in with her. I wasn’t coughing up volumes of it; I was just coughing up a little spot here or there.
It wasn’t bright red. It was dark orange, kind of brownish color. Just a little, tiny bit, not alarming like, “Oh, I really need to get myself to the hospital.” It was just like, “Hmm, I’ve never had that before. What is that?”
I went to the doctor, who said it was irritated airwaves, that I’d been coughing for months now, and it was just inflamed. She said she was not going to worry about it and suggested I go home.
It was the winter holiday, so my kids were out of school. We were going to go to my childhood home to visit my parents.
My doctor said, “Go enjoy your vacation. If things aren’t better when you come back in January, we’ll do another X-ray.” I said okay. I went home to my parents’ house in Palm Desert in Southern California.
Then it started accelerating. I was having high fever and night sweats and coughing horribly, coughing so much that we discovered later I had 3 broken ribs.
My mom said, “Go now and get another X-ray right now.” That’s what I did.
Describe the ER visit
I went into the ER in Palm Desert. They did an X-ray.
Now that I know more about all this, what they should’ve done, based on the X-ray, was sent me for a CT right then and there.
They didn’t. They said they definitely saw something on the X-ray that was not normal, but they thought it was pneumonia. They said, “We’re going to give you some other medications, some more heavy-duty cough medications, and when you get home in a couple weeks, then go get a CT.”
You got a second opinion from a family friend
Mark, a family friend who was a physician, happened to be visiting my parents during the holidays as well. He took one look at me. He’s not an oncologist; he’s not even a pulmonologist. He’s a retired gastroenterologist.
He never used the word “cancer,” but he said, “This is not adding up. You haven’t responded for months to all these medications, and you’re getting worse. Stop messing around with the primary care physician. Right now go call and make an appointment for a pulmonologist.”
Describe the pulmonologist visit
I was going home in a couple days, so at that point it didn’t make sense to seek treatment in Palm Desert. The day I got home, I went to see a pulmonologist.
He took a listen to my lungs and read my O2 (oxygen) level, which was really compromised. I can’t remember. It was maybe in the 70s at the time, and normal is 99 or 100%.
He said, “Go down and get a CT immediately.” That day, he sent me down for a CT. Again, I didn’t appreciate how abnormal this was because I didn’t go to the doctor a lot.
I went right back upstairs to this pulmonologist, whom I had just met, and he pulled up the images of the CT. When he pulled it up, both my lungs were just covered, totally whited out. That’s really bad.
But he never said the word ‘cancer.’ It wasn’t even on my mind because I wasn’t what I thought was the typical lung cancer patient.
He said, “We need to go get a biopsy.” I think it’s something called sarcoidosis. He really downplayed it, so I wasn’t freaking out. We made an appointment for the next week to get a biopsy.
Luckily, my family friend Mark was going to be in the Bay Area. He came with me to that biopsy, and I was diagnosed right as I woke up from the biopsy.
Mark was there in the recovery room with my husband, able to translate the information that was being thrown at us.
The surgeon didn’t sugarcoat the diagnosis
I hope other people have better experiences. When I woke up, I had my husband near my bed, and this family doctor friend, Mark. At the very foot of the bed was the surgeon who’d done the biopsy, who I’d only met once before at the pre-biopsy appointment.
Obviously, as I was being wheeled in, he was in the room, but I never really built a relationship with him. There he is at the foot of my bed. It’s 8 on a Friday night. He wants to go home. I don’t blame him, but he just said, “Looks like stage 4 lung cancer. There will be an oncologist who will show up in your room tonight and good luck. Goodnight.”
And he just left. So it was not great.
What were you feeling when you were diagnosed?
It’s such a shock and so overwhelming and so foreign to be diagnosed with something that I’ve never researched.
I’d never known anybody who had it, knew nothing about it at all, even just basic medical terms. I was out of it.
I had never even had anesthesia before in my life, so I was just waking up from that and a little out of it and the shock of the diagnosis.
I think I was probably scared to go home, but I didn’t understand that it would be unsafe. I couldn’t differentiate between that, whereas having Mark there really helped.
They were ready to send me home after that biopsy, and Mark was there saying, “No, she’s tachycardic (high heart rate).” I didn’t even know what tachycardic meant at the time.
He ended up talking to them and saying, “You can’t release her.” I ended up being in the ICU for a week, so it’s crazy.
I shudder to think of what it would have been like to be sent home in that condition. I was on oxygen. They were going to send me home without oxygen.
I ended up being on oxygen for almost 2 months. When I finally came home from the ICU, I just brought the tanks home with me. I am so grateful that he was there to help.

»MORE: Patients share how they processed a cancer diagnosis
What was it like being on oxygen 24/7?
The hospital set this all up. They contract with a provider, who comes in and sets up a compressor in the house. It’s this thing that looks like a portable air conditioning unit.
I got this really long hose, so I could walk anywhere in the house. It’s like having a leash. It’s a hose from the compressor that’s kind of noisy, so we set it up in the living room so it’s not near the bedrooms.
Then I had this hose going all through the house, to my bed or wherever I was walking in the house. Of course, it’s always in the way, people are tripping on it, getting caught in doors, pain in the neck — but then you don’t have to have a tank that you’re switching out. It’s compressing oxygen from the air in the house.
When I wanted to leave the house, which wasn’t very often in those early days, especially because of the oxygen, I had this portable tank that I could either wheel. Eventually, I got one that was in a little backpack-type thing that I could carry on my shoulder.
To be honest, those almost made me a little bit nervous, so I was a bit housebound those first couple of months.
Treatment Decisions
The diagnosis was out of left field because you never smoked
I learned the hard way. Even though I had already heard the year before of a younger patient who got diagnosed with lung cancer, I still thought, “Wow, that’s so weird.”
I didn’t even have to think it would ever happen to me. It was just, “That’s weird, and these unusual things happen one in a million.” Then when it actually happened to me and I started finding out more about lung cancer and finding other fellow lung cancer patients, I realized this is not what I thought it was at all.
Lung cancer is on the rise in never-smokers. It’s on the rise in younger people. It’s on the rise in women.
It’s not the stereotypical haggard smoker, had a 2-pack-a-day habit for decades. That’s not the typical patient anymore. Here’s the statistics I have heard.
About 20% of the newly diagnosed patients are active smokers. That leaves 80% who aren’t. A big chunk of that, about 60%, are former smokers, but a lot of those former smokers quit decades ago, so they think of themselves as long-time non-smokers.
Who knows? Some of those people, I’m sure their smoking history has to do with their lung cancer diagnosis, but some of them maybe not. We’ve never examined that because of the stigma and the assumptions that lung cancer is only and always due to smoking.

How did you decide which hospital to go to?
When I went in for my biopsy, cancer hadn’t even been discussed. I thought I was just going in for an outpatient procedure, and then we would deal with that, whatever the results were after.
When I woke up, I was admitted to the hospital immediately thereafter and told it was stage 4 lung cancer and that we needed to start treatment immediately.
I spent the next day doing baseline scans, and then they started my chemotherapy right there in the hospital 24 hours later.
I didn’t have time to research doctors or hospitals and pick where I wanted to go. I still don’t even know quite how that happened. An oncologist just showed up in my room and was like, “Here’s our plan, and do as I say, or this isn’t going to work out. This isn’t going to go well for you.”
I wasn’t given options. Later on down the line, I was lucky. It turned out that oncologist who showed up did a great job for me.
»MORE: How to be a self-advocate as a patient
What made you switch to a lung cancer specialist?
As I got my bearings, I started to research and found she was a general oncologist. I wondered if I should get myself to a thoracic oncologist who specializes in lung cancer.
I eventually found out I tested positive for a genomic alteration called ROS1-positive (ROS1+), and I wanted to be with someone who had other patients that had that same diagnosis.
I started looking away from the community hospitals and toward Stanford and UCSF, which were accessible. I did some second opinions there a few months after my diagnosis at both of those places and eventually shifted to one for a few months. Didn’t love it.
Why did you switch back to a smaller hospital?
I had these great ideas of, “Oh, if I just go to [a major hospital], everything’s going to be great there.” It’s not that the doctors aren’t brilliant there, but I definitely felt like a number.
The emphasis on research there overshadows the patient care in my experience, so I ended up shifting back to a community hospital, where the nurses knew my name.
I had my oncologist’s phone number, and he was responsive to me and just accessible. Not that the other doctors aren’t responsive, but you don’t have the same kind of access. There’s just so many layers you have to go through to get to the doctor, and the doctor’s not in clinic very often, one day a week.
I ended up shifting back to a general oncologist in a community setting, but having established relationships at the academic centers so I can consult them when I have to make some major decision in my care. For the day-to-day labs or even the regular schedule scans, it’s so much better for me to be at the community setting.

Advice on building the relationship with your doctor
I struggle with finding the right balance in building the right relationship with my oncologist and my care team because there’s all this pressure.
Constantly, patients are given the message, “You have to advocate for yourself. You have to push. You have to come in with all your research.” I do all that, but also you want to be deferential.
These are the experts. I don’t have a medical degree. This sounds embarrassing to say, but you want to be liked. You want your doctor to care about you and smile when you enter the room and not like, “Ugh, this person’s constantly arguing, pushing, and questioning.” It’s been a process for me to learn how to balance those 2.
I definitely advocate for myself, but I also try to have some deference and build a relationship.
My advice is find the right match but also always, always get second opinions and create a sort of team.
Here’s whom I go to for my regular care, but maybe if I have questions, maybe I have some expert who’s very specialized but wouldn’t be great for my day-to-day care or is even available for that.
That person knows about me, so when I need them, I can reach out. I have other people on the team that fill other roles. I have a therapist I see for my emotional stuff because that’s not what an oncologist does.
The one thing I think is most important for me and the doctor is that they will listen and also agree to work and accept that I have these other people on the team.
What I found doesn’t work for me is a doctor who wants to be in charge and doesn’t want input from me or anybody else. That would be probably a suggestion for other patients is to look for doctors who have expertise but are also willing to listen to others.
Chemotherapy and Side Effects
Did you choose treatment?
I wasn’t given choices. I definitely had to sign off permission, so I guess technically I had a choice not to sign. Basically, the oncologist came in and said, “You’re relatively young. You’re healthy and fit, so I think you can tolerate a really aggressive chemotherapy prescription. I want to start as soon as possible.”
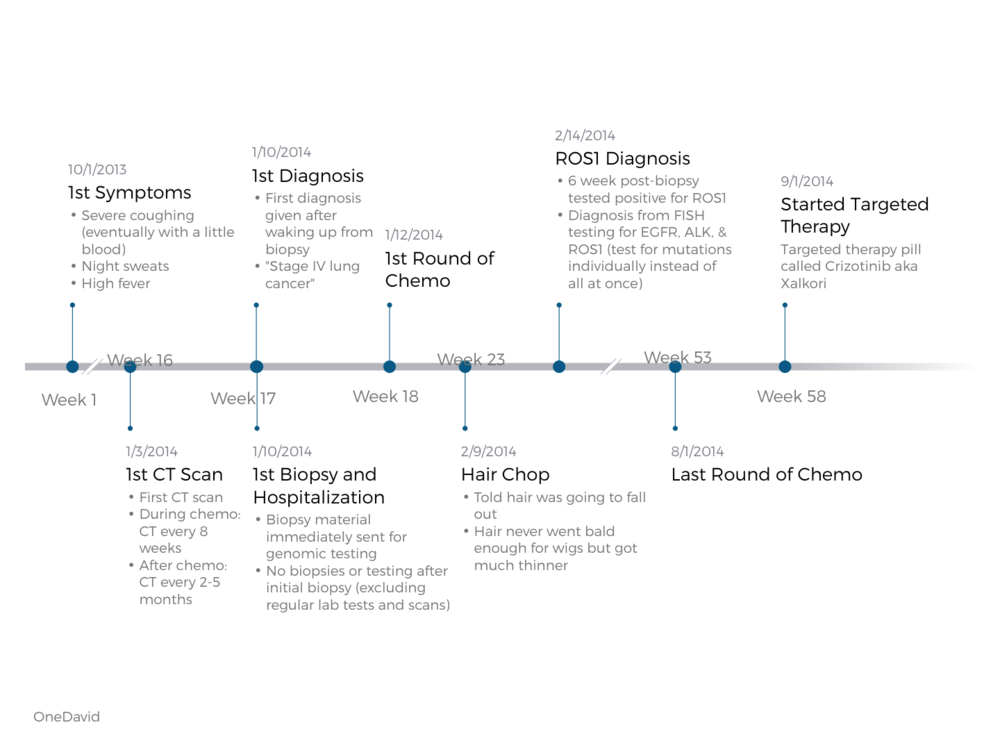
Here’s what the 3 drugs are. It was cisplatin, Avastin and Alimta. Cisplatin is so toxic they actually have to infuse you with a whole bunch of saline before and after to wash your kidneys. It’s actually a 12-hour infusion because of the before and after, in addition to the infusion itself. She’s like, “I think you can take it, so we’re going to start that immediately.”
- Treatment cycle:
- Chemotherapy: Cisplatin + bevacizumab (Avastin) + pemetrexed (Alimta)
- 4 cycles
- Cycle = 3 weeks
- Given over ~12 hours in one day
- 4 cycles
- Maintenance chemotherapy: bevacizumab (Avastin) + pemetrexed (Alimta)
- 4 cycles
- Cycle = 3 weeks
Given over ~6-8 hours in one day
- Cycle = 3 weeks
- 4 cycles
- Targeted therapy: crizotinib (Xaltori)
- Chemotherapy: Cisplatin + bevacizumab (Avastin) + pemetrexed (Alimta)
How many cycles of chemo did you undergo?
I underwent 4 cycles of chemotherapy with cisplatin, bevacizumab (Avastin), and pemetrexed (Alimta). Each cycle lasted 3 weeks.
The infusion was the first day for about 12 hours. The first was one right there in the hospital, and it takes about 12 hours. I tolerated the first one pretty well.
Because they know cisplatin is so difficult to tolerate, they give you all sorts of stuff before and after you take it. It’s not just steroids, but there’s an extra drug called Emend that you take to prevent nausea. I was on all kinds of things to help ameliorate the difficulty of tolerating the chemo.
For maintenance chemo, they just took out the cisplatin. It was still 4 cycles, 3 weeks each. The infusion was shorter at around 6 to 8 hours on that first day. Altogether, I was on chemotherapy for 8 months.

What were the side effects of chemo?
The nausea’s the one that jumps out in my memory. It’s all the side effects of the things that are supposed to treat the side effects.
Those steroids are brutal. They interrupt your sleep; they make you a little crazy emotionally. Speaking of emotional, I wouldn’t call that necessarily a side effect of chemo as much as a side effect of being thrown a total curve ball in your life, but I think it’s really important part of treatment.
In addition to your prescription for your medications, I wish they gave everybody a prescription to go visit palliative care and to also go visit a social worker, therapist, or some emotional support like that. I think that’s really key to coping with this, and it has actual ramifications in terms of how well you tolerate your treatments and how your quality of life is.
Specifically, the first cycle went pretty well. I didn’t get that nauseous. The second one also, but these things accumulate. By the fourth one, I was really feeling it. I definitely remember barely being able to walk out of the infusion lab by the fourth one.
That triplet with the cisplatin, I only did 4 rounds. Every 3 weeks, I would go in for that. Then they shifted to what they called “maintenance chemo,” and they took out the cisplatin but left me with the Avastin and Alimta, which was much more tolerable but still had side effects.
I was still taking anti-nausea medication and steroids. Then it caused high blood pressure, so I had blood pressure and all these things. You know how it goes.
The first week after the infusion, make no appointments. Just plan on being home pretty much and get yourself a nice Netflix subscription and whatever.
Then you start to feel better, and I was myself by the third week. That was a good week. You live your life on this, ‘Okay, everything I want to do I have to compress in week 3.’ You go through that whole thing every 3 weeks.
Please rate the side effects you got from chemo
Everyone tracks differently. Lisa rates her side effects with chemo an 8 out of 10. This indicates that she happened to have a more difficult experience.
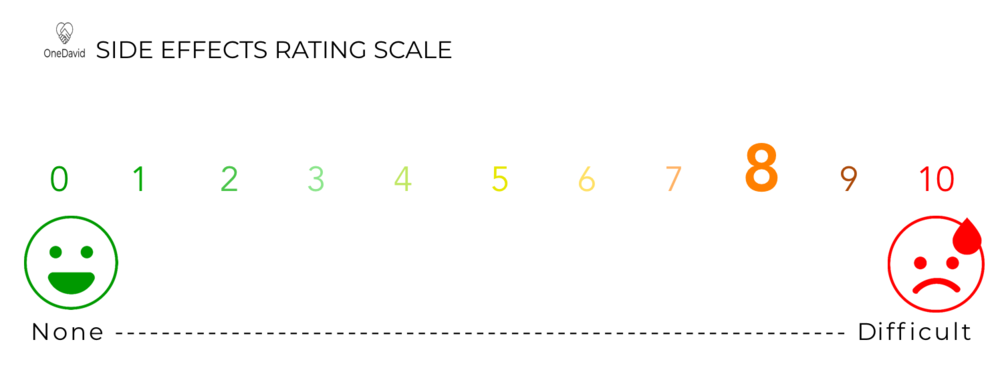
As for her experience with side effects on the maintenance chemo, Lisa rates her experience at a 6 out of 10, making it better than her primary chemo, when she also had to get the Cisplatin drug infusion.
»More: Patients discuss various side effects
How did you respond to chemo?
I would go for a scan [depending] on how the symptoms were going and such. The triplet with the cisplatin, I had a good response to, so my scans started improving pretty drastically. I never got to a place where there was nothing on the scans, but it was much improved so much that after about 2 rounds of chemo, I was able to come off the oxygen (tank).
It was quite a sight. I was always the youngest person in the infusion lab usually, but I was the worst looking because I had the oxygen tank. I had the hose in my nose, schlepping the tank around. If I’d have to go to the bathroom, I’d have the pole with the infusion stuff and my oxygen tank.
I was just a mess of cords and whatever. The triplet worked really well, but it’s not tolerable long term. Then I went to maintenance chemo, and the symptoms started creeping back after a few months. I started coughing, and the scans started showing the cancer returning. After 8 months, it was clearly not working anymore.
Luckily, really luckily, I had found out earlier that my cancer tested positive for ROS1. We knew that there was a targeted therapy drug that I could take for that, so that’s when I switched. I’ve been on that ever since.
Did you lose your hair?
They told me I would. Cisplatin typically does make people lose their hair, so I did the whole wig shopping thing. Those are expensive! I regret it because actually my hair thinned quite a bit, but it never fell out completely.
»More: Patients discuss hair loss after cancer
I cut it short, then went wig shopping, and was all ready. Now it’s still sitting in my closet unused. For me, I didn’t end up completely losing my hair.
I probably would have cared more if it actually happened, but when they told me that it came along with all this other news that was more terrifying, I was more focused on what I am going to tell my kids. My prognosis was about 9 months, so the hair was low priority on that scale.
Targeted Therapy
How did you learn about the targeted therapy drug?
I had my biopsy at El Camino Hospital, the local hospital here in Mountain View. My biopsy was done on January 10, and I found out later that starting on January 1 of that year was when they started testing all the lung cancer biopsies that came through the pathology lab there for ROS1.
Without me even having to ask for the genomic testing, they had instituted a process where they did that automatically just a few days before my biopsy.
It took a few weeks for those results to come in, so I didn’t find out until after I started chemotherapy. They decided to keep me on the chemotherapy train until it stopped working since we’d already started that treatment course.
I knew pretty early on that I was ROS1-positive and that there was a targeted therapy. The complication was the targeted therapy was not FDA-approved at that point, so the doctor, the community hospital general oncologist I’d been working with, had never used or tried to use that targeted therapy on my type of cancer because it wasn’t even FDA-approved at that point.
I was doing my own research and had found that it was already in phase 3 trials in the U.S. The results had been so compelling it had been fast-tracked with the FDA. Insurance was already approving it for some patients out there.
I asked her to prescribe it and submit it for insurance approval so we would have it available. She was a little reluctant at the time, so I advocated for myself.
Self-advocacy as a patient
My doctor told me after this chemo not to worry. She was trying to reassure me to not worry and that I had other chemotherapies that we could try.
I was like, “No, no, I really have been hearing great things about this targeted therapy. Let’s look into that.”
»More: How to be a self-advocate as a patient
How were you feeling at this point?
My doctor told me I had stage 4 lung cancer, but she never said, “That means you have this prognosis, this many months.” Of course, I avoided Googling that explicitly for awhile.
Finally, I worked up the confidence to do that, and it’s not good. But those numbers are out of date at this point. The targeted therapies are really changing the survival curves dramatically.
I’m the kind of person that needs to know more. I know some patients prefer not to know anything and have kind of a gatekeeper — might be a spouse or just a friend or whoever — sift through that and give them whatever they need to know, but I need to know it myself, directly.
I did a lot of research on my own. Sometimes that’s hard to read, but for me, in the end, knowledge is more helpful rather than less.

Were there any targeted therapy side effects?
With targeted therapy, when I switched to it, I almost had a more difficult time the first 6 months. It made me more nauseous than the chemotherapy. I just remember being on my bedroom floor every morning for months.
I didn’t have the bad weeks. Eventually it evened out, I got a handle on the side effects, and my body adjusted. I didn’t have a bad week then good week. It was consistently. I never got to the lows or the highs. That took some adjustment. I’ve lived with this medication.
Luckily, I feel so grateful. I’ve been on this medication almost 4 years now.
There’s chronic things. I have edema. I have some nausea. It’s totally under control most of the time, but it’s just part of my daily life. There’s these certain things that I live with and am never rid of, whereas with chemotherapy, ironically, there was the good days where the very best days were actually better than the targeted therapy days.
Please rate your side effects from the targeted therapy
How long have you been on the targeted therapy?
I’ve been super, super fortunate. Knock on wood here, because I was put on this targeted therapy called Xalkori in September of 2014. I was told that the median effective time for the drug would be 12 to 18 months, and I’m still on it. I’m approaching the 4-year mark on this medication.
I’m clearly on the outlier end of the spectrum, which is great, but it’s also nerve-racking because I know that I’m kind of winning the lottery, and my number might come up — and not in a good way — at some point.
I don’t know that many people. The further out I go, the less people I know ahead of me. I know a lot of people on this medication, but I’ve gone from looking out and saying, “I want to be one of those people that’s 4 to 5 years on this drug,” to, “Now I’m the one everybody else is looking at, and I’m losing the people ahead of me.”
That’s my particular struggle right now. How do I confront that now? I’m feeling good right now. Luckily, I have no symptoms that are causing me great concern. Of course, that doesn’t always correlate with how the scans go, but I’m optimistic right now.
This is the longest interval for the whole period since I was diagnosed. I was getting scanned every 2 to 4 months, 2 to 3 most of that time. Last year, I shifted to every 4 months for a couple cycles. This is the first time I’ve gone 6 months, so it’s been a big one!

Reflections
How do you talk to your kids about the cancer?
Having a diagnosis like this when you have young kids at home is, in my view, the hardest part of it. The world turns upside down.
I came home on oxygen and sick. My mom basically moved in for months. It was a radical shift. There was no hiding it from the kids, for better or for worse.
I don’t necessarily think it was for worse because it’s a strange place to be now, where I appear normal, yet I know I’m still dealing with a very scary situation. That’s a strange thing for me to wrap my head around, let alone young children.
In a way, having this tangible thing — it is real, and you can see it — I think helps process. It helps everybody face it and deal with it.
I have had friends who went straight into targeted therapy, and it’s like, “Mom was sick, and now she’s better.” When they did get worse, it was like another trauma. My family didn’t have that experience.
We had to face it head-on. I definitely contacted therapists and social workers to help us figure out how to help the kids deal with this. Still, 4-plus years into this, we still have them visit people.
Not as constant. It’s not as intense as it was in the first year, but it’s still something that is very much part of our lives. We try to cope with it. We have a library of books and tools, anxiety tools, from coloring books to stress balls to games.
This whole stable of support systems, whether it’s their teachers at school, the therapists we’ve hired, or the doctors that know about it. Things like that.
Any advice for other parents dealing with diagnosis?
I think it’s different, depending on the kid. You have to have some level of deference and let the kid lead. Not to the extent of ignoring it entirely. I have 2 kids. One that likes to talk about it and know all the details, and one kid that barely asks any questions at all.
I communicate with them totally differently. The one who wants to know the details I share. The one who doesn’t, I don’t necessarily get into the nitty-gritty, but I actually make sure to weave it into the conversation a little bit so we’re not in a denial situation. I think that you have to know your kid.
Seeking out professionals
I don’t think you can do this without an expert’s guidance because you don’t know how to do this until you’ve been through it. There’s no way you can have experience with it.
Seek out a professional. If the professional doesn’t work, don’t give up on professionals. Find another one, because they’re all so personal.
We all need different types of personalities and support. The first social worker at the hospital wasn’t a match for our family, but eventually I did find the right person. It takes trial and error sometimes, but it’s so crucial.
How did you find the professionals?
There were a few sources. The hospital has social workers on staff, but those people ended up not being a match for our family.
We got really lucky. There were social workers at school that first year, and those people were really good. They switched out the next year, and the replacement was not good.
I ended up having to do some research, talking to friends and family, finding people outside the system just privately. It can come from a lot of different places.

What’s your advice to people dealing with a new diagnosis?
My number one advice to any lung cancer patient is to go get genomic testing. I don’t care who you are. Even if you have a history of smoking or you’re an older patient, whatever it is, everyone should get genomic testing because you never know if your cancer is going to turn out to have one of these targetable mutations. If it does, your survival statistics change drastically.
Your quality of life. There are these things I have to deal with chronically, but overall I live a pretty normal life.
I carpool my kids to school. I do take exercise classes. I travel. I do 90% of what I was doing before, so it’s as close to normal life as you can possibly get with this type of diagnosis. Much closer than the chemotherapy, where I’m tethered to the infusion every few weeks and on that roller coaster.
Also, find your people.
Once you know your genomic mutation, if you have one — or even if you don’t, if you’re considered wild type — go find the people with that. There’s groups with everything now.
I’m part of a ROS1+ group. There’s a group for EGFR-positive (EGFR+) patients, for ALK positive (ALK+), for KRAS. There’s hundreds of types of lung cancer out there now. The more specific you can search for and find those communities, the better information you’re going to get back.
You find those people, and you’ll immediately be plugged into all the current clinical trials, who the world experts are, where the conferences are, and the side effects for our medication.
All that great information is going to be at your fingertips really quickly, rather than wading through all the general information about cancer or even just lung cancer. Find your very specific sisters and brothers out there.

What was once considered “incurable” is changing
I have a friend that re-labeled “PTSD” (post-traumatic stress disorder) to “OTSD” (ongoing traumatic stress disorder) because I think the medical field hasn’t quite caught up to the realities of this new category of patients.
Those of us that have been given diagnoses that are what they would call “incurable.” In the past, say, a decade prior, people receiving that diagnosis would probably pass away in less than a year, so it was this dramatic diagnosis with no good treatments, and then the patient would pass away.
Of course, they’d have PTSD, but they didn’t have to go on living their normal lives. They were just immediately plunged into the chaos and panic until it was over.
For those of us living for years with these diagnoses and often on targeted therapy, or now immunotherapy is doing this as well. CAR T is now out there. There are all these breakthroughs that aren’t cures but are extending lives for years beyond what they used to.
There’s this whole new population that has to live with the knowledge that they have this very severe diagnosis and yet proceed with living, right?
I’m not in the crisis stage, where I’m on oxygen and housebound anymore. I’m out in the world living my life while also carrying this invisible burden.
There’s so many ways that that has played out. It’s a whole process that I’m constantly evolving with. For a long time, it felt very strange to be out in the world. I just remember being in line at the grocery store and thinking nobody knows what I’m dealing with.
I look normal. People are treating me normally, but I’m not normal. I might not feel well, or maybe I feel okay, but I have all this emotional stuff.
There’s just all this trauma and knowledge [of] the very vivid recent experience of the rug being ripped from out under your feet and knowing that that could happen at any time in such a visceral way.
As much as people say, “Make the most of today. We all die.” There’s a difference between intellectually knowing that and experiencing that and the trauma of that. Living with that is something that I’m constantly a work in progress trying to figure out how to proceed.
How did you manage the emotional stress?
I think I’m getting better at it. I honestly do embrace life and say, “Okay, I have this.” Lots of people have difficult things they live with, whether they’re living in some war-torn place or in poverty or a serious diagnosis. We all have our struggles, and this is mine currently.
How am I going to go on living my life and planning for things in the future and getting comfortable with that? Like, okay, I’m going to plan a trip for 6 months a way. That blew my mind initially, and now I’m getting used to it.
What has helped you deal with the toughest stuff?
I have all kinds of tools that I use. A lot of them, you’ll hear about over and over again.
If I had a nickel for every time somebody told me to meditate… I suck at it still, like so many of us do. I don’t love meditating, but I try.
I’ve done all the other easy things. Get the coloring books and the fun books to read, the magazines, whatever calms you, whether it’s your favorite TV show, movie, book, or coloring books.
We have this great alternative bookstore in Mountain View called East West, and they have fun things. Stress balls to squeeze, or I have this Play-Doh.
You can spend your money however you want. You can get magic crystal necklaces or mala beads to play with. I have it all in a toolkit like that.
I think that’s great. That’s fun, but really it’s about a mindset and shifting my mindset, accepting where I’m at and the possibility that I could be there for a while, and allowing myself to live my life today.
It took a lot of time, a lot of talking with friends and therapists, reading books, and figuring out how I can proceed with this

Family has been a big part of the journey
Cancer didn’t just happen to me. It happened to my whole family. Everybody’s been really supportive of me, but they all have had their processes, too.
I’m sure it was terrifying. It still is terrifying for my husband to face the prospect of losing his partner potentially and what it would be like to raise kids as a single parent. My mother is obviously distraught at the possibility of losing her daughter — both my parents.
I don’t know what it’s like to be in one of those roles, but I can appreciate that everybody has gone through this. It affects all of us a little differently.
Support came from those who’ve been through their own trauma
I was a little bit surprised at which friends showed up and which friends didn’t. That’s not a judgment on them, but a lot of times it had to do with whether they had some relevant experience of not this diagnosis, [but their own trauma].
I have 2 friends who had lost a parent to ALS. I have one friend whose husband had a cancer diagnosis a few years prior. They just had some frame of reference for facing mortality and dealing with a trauma of this magnitude.
Friends who didn’t have that frame of reference tried to show up a lot of times but just didn’t appreciate what I might need or want or what boundaries are appropriate or inappropriate. It’s interesting how that plays out.
It’s hard because on the one hand, I want to say, “Push the boundaries.” I tend to be introverted. I don’t like asking people for help, so I mostly appreciate it when somebody is a little pushier and just says, “Hey, I’m going to come over with this meal. I’ll just leave it here if you want to talk or don’t want to talk. Come in if you do want to talk.” But they would take the initiative.
Support also came from unexpected places
I think you have to listen to how you’re feeling with that relationship.
There are people I had no relationship with that reached out. There was this one woman. I taught these fitness classes. She was a regular in my classes, but I didn’t really know her.
She reached out. She brought a meal, and a lot of people did that. It was amazing the people that show up are so generous. I didn’t differentiate her from the other people that were dropping off meals. She did it a few more times. Then she asked to go for a walk one day when I was feeling up to it. We did that.
Come to learn, she’d lost her husband to brain cancer. She gets this, so we’ve grown close. If you don’t [know] the person at all, don’t be pushy.
Sometimes, if you know you have that connection, you can understand, You’re getting some symbiotic relationship conversation going. Then keep going with it.
If the person isn’t responding to you, at some point, you have to know maybe it’s not personal. It’s just if I’m not feeling good, I don’t want you stopping by every other day.

Inspired by Lisa's story?
Share your story, too!
Lung Cancer (Non-Small Cell) Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza