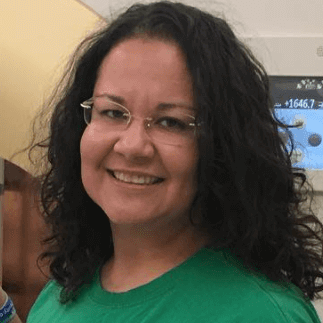
Christine’s Stage 2A Lung Cancer Story

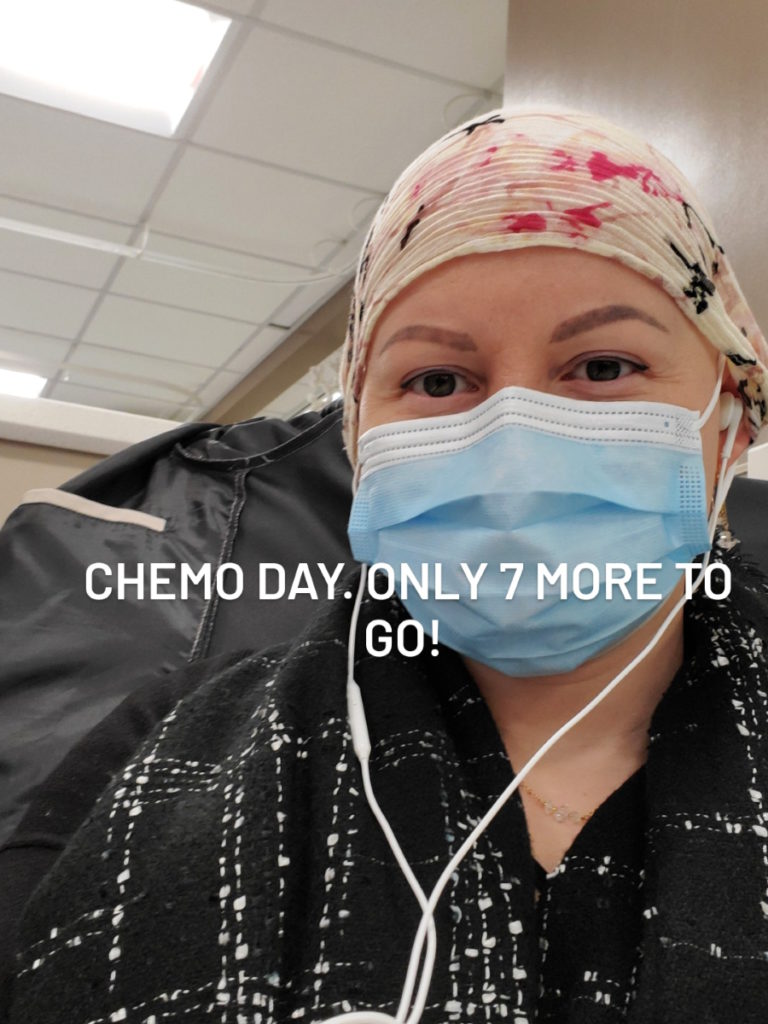
Christine’s journey began with a stage 3 triple-positive breast cancer diagnosis, which unexpectedly led to the discovery of her 2A lung cancer. Despite experiencing no symptoms related to lung cancer, it was detected during the testing process for her breast cancer. Although initially dismissed as insignificant, Christine’s persistence and intuition compelled her to advocate for further investigation. She insisted on a biopsy, which revealed that the lung nodule was not a benign or insignificant finding. The subsequent CT scan showed the nodule shrinking during chemotherapy, raising further alarms.
Empowered by her cancer journey, Christine tapped into her assertiveness and communicated her needs. She pushed for additional tests such as a PET scan and a biopsy, seeking alternative opinions when the initial results were inconclusive. Trusting her intuition proved crucial in navigating her medical care and making informed decisions. Following a lower lung resection, Christine faced complications during her recovery but gradually healed and focused on rebuilding her lung capacity and overall strength through physiotherapy. Weeks later, she received the surprising confirmation that the nodule was cancerous, an entirely separate primary cancer.
Investigation into her childhood home revealed high levels of radon gas, indicating a potential environmental cause for lung cancer. Christine emphasizes the significance of trusting one’s intuition and speaking up when something feels amiss, particularly for women. Her experience has propelled her to empower and support others facing cancer.
At The Patient Story, our lung cancer stories provide a glimpse into the experiences, emotions, and triumphs to offer support, encouragement, and a sense of community to people who are going through similar journeys.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Christine E.
- Diagnosis:
- Lung Cancer
- Staging: 2A
- Initial Symptoms:
- None; saw a lung nodule in the CT scan
- Treatment:
- Surgery (lung resection)


Introduction
I’m a survivor of both breast cancer and lung cancer in the primary stage.
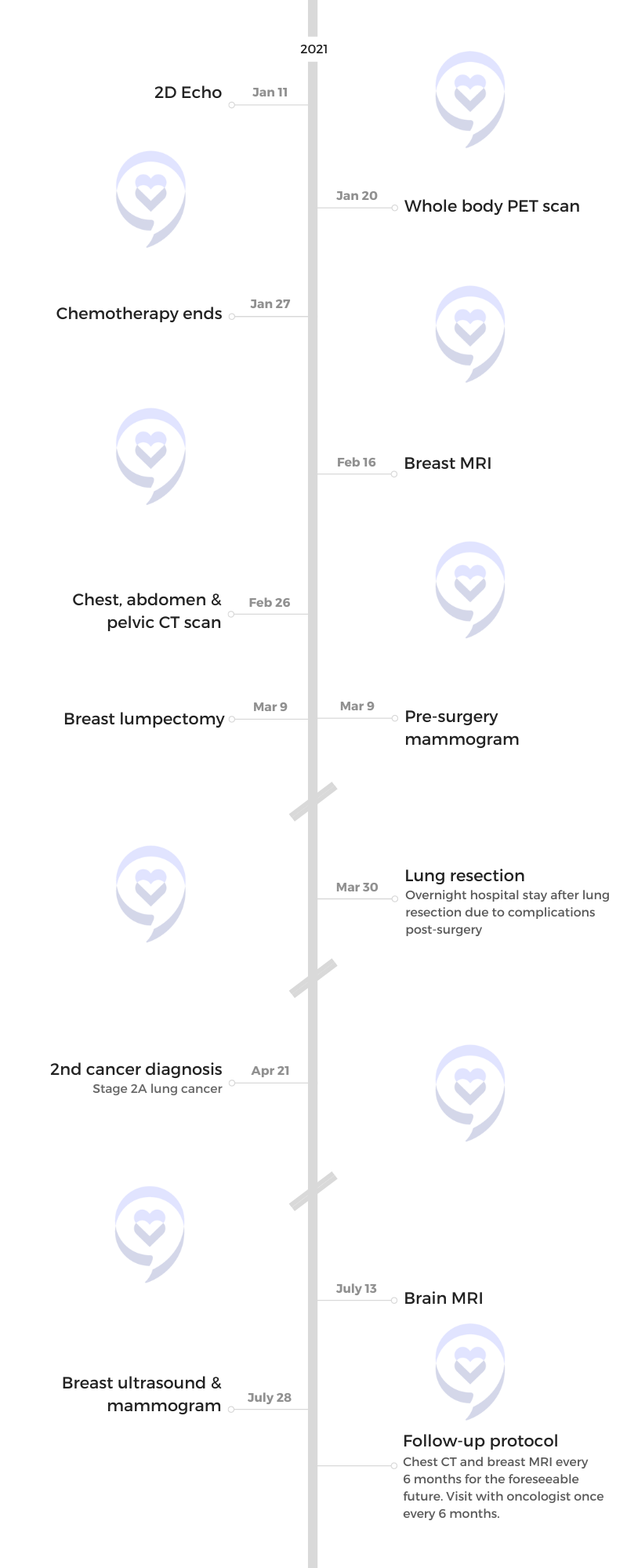
While going through my breast cancer staging and getting everything done, we were doing secondary testing in CT form. During that time, we noticed there was a nodule on my lung.
It was quite scary for a long time because I understood that this could very well be stage 4 breast cancer. I really had to advocate for myself as we went through the process to find out what this nodule really was.
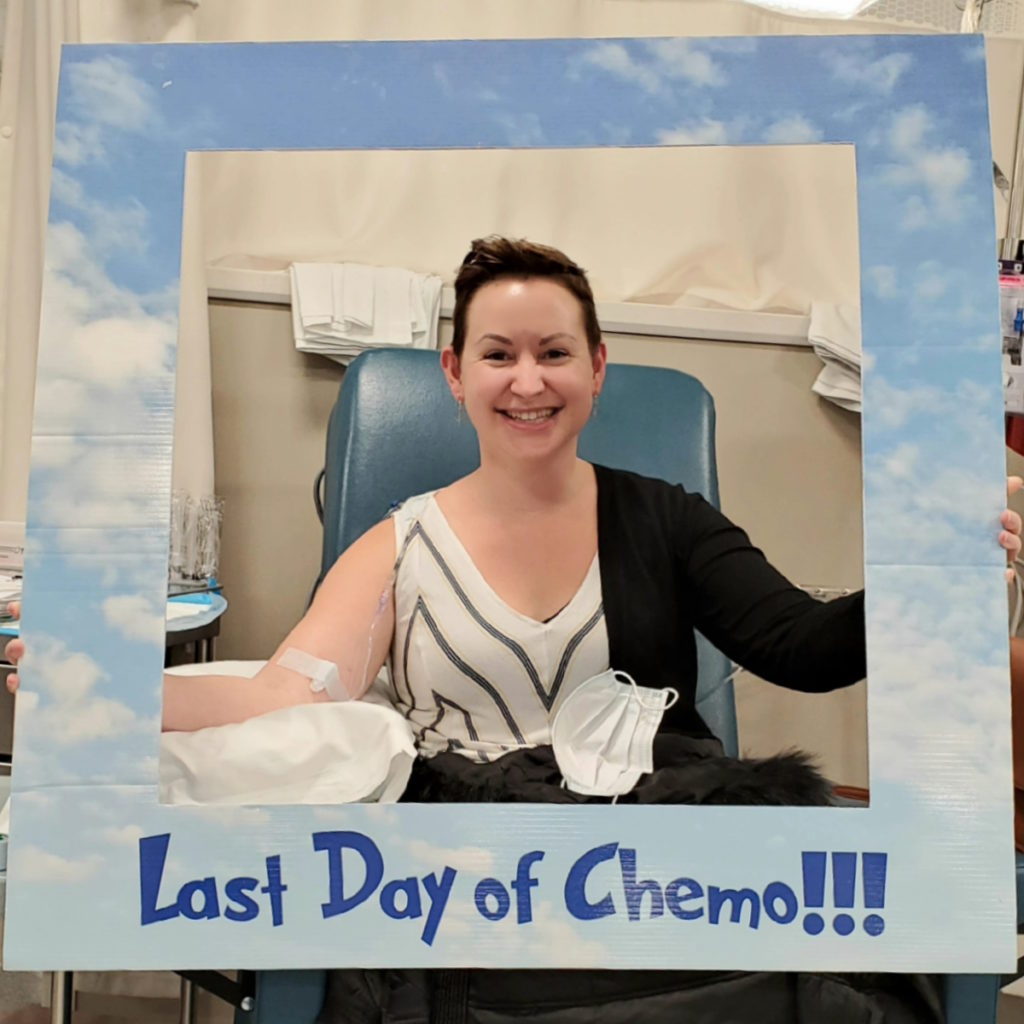
From the time that I was diagnosed with any type of cancer to when I was in complete remission from both cancers was about a year’s time.


Pre-diagnosis
I don’t believe that I felt any symptoms in regard to lung cancer. I truly believe that I wouldn’t have found it either without the first primary cancer. Lung cancer is one of those scary things that once you start feeling symptoms tends to be a little bit advanced.
In a way, I was quite fortunate that breast cancer led to more testing. During that process, we found another cancer that may not have been found for many years.
Two months into my breast cancer journey, we did the CT scan. I was so far along in my breast cancer journey that they wanted to test other areas of my body to see if it had migrated. We tested the liver, brain, chest, abdomen, pelvis, and reproductive organs.


In all of those tests, everything came back negative except for this lung nodule that popped up. At first, the doctor said it could be a fatty tissue deposit, it could be an air tissue deposit, it could be all kinds of things that are really standard and normal, and not to worry.
However, I was not at all comfortable with it. My breast cancer was on my left side and it was in the lower lobe of my lung on the left side, which was directly behind the breast.
I spent a good five months really thinking that I have stage 4 breast cancer. I don’t know what this is going to be like. I had to push a bit to get it biopsied because they really said, “We’re just going to watch it. It’s nothing.”
They redid a CT scan in preparation for my surgery. We realized that it got smaller during my chemotherapy so that was a clear indicator that it’s changing. It’s not just a fat deposit or an air deposit.
What was crazy about all of this is that in the process of trying to deal with breast cancer, they forgot that they gave me a CT scan and didn’t check it. I was all prepared for my surgery and no one knew except me, who checked my own health records, that this was changing.
I literally called my oncologist on the cell phone and was like, “Have you seen the CT scan?” He was like, “The what?” I’m like, “The CT scan that I made you give me?” He then went in, read it, and was like, “Oh. I gotta make some phone calls.” It was wild. I started falling through the cracks.

They were so busy with the process of my breast cancer that they just didn’t think to check it. They had forgotten that they gave it to me.
I was just frustrated one night [so] I checked it and I realized it changed. That’s when I started making phone calls and setting off alarms.
The original scan done two months into my breast cancer journey showed 1.4 cm in size. When we went in for surgery, we realized that it had changed to 1.1 so it got smaller in five months of chemotherapy.
Advocating for yourself
In my past life, I was a very strong people-pleaser. If the guy in the white coat told me not to worry, I would just listen.
When this all happened and I started checking my own scans, I really pulled out a version of me that [lay] dormant for a long time. I got really, really unapologetic about who I was and what I wanted.
I called my oncologist and said, “Hey, I don’t know how I got your phone number, but I need to talk to you.” I really found it quite empowering at that time to say, “I want a PET scan. I want that done. I want a biopsy. We’re doing this.” Really brought out a version of me that I didn’t know prior to this.
Pushing for testing
In a very short period of time, I got a call from a lung oncologist saying, “We want to give you a biopsy, get that PET scan that you asked for, and all of these things.” It really kicked into high gear because we were really, truly running out of time in a lot of ways. We had my breast surgery scheduled so we needed to really hit this hard.
I did a bunch of testing in a short period of time. The lung biopsy, which was very uncomfortable, came back inconclusive. They weren’t able to get it because of where it was and what it was attached to. They weren’t able to get around the rib in order to test it.
At first, they said, “It’s probably still nothing.” I was like, “Nope. Who am I talking to next? Who else do you have in your arsenal? Because I’m not accepting that.” They said, “Who else do you need to speak to?” A surgeon would be the next natural step.
I got in contact with the surgeon and his bedside manner wasn’t the best. He was like, “People your age, it’s probably a fat deposit or an air pocket. It could have changed in size because of the scan itself. I don’t feel that it’s really anything. But if you want, for your peace of mind, to remove it, I’ll do that for you.”
When I spoke to the surgeon, it was right in this period of time [when] we were really hitting the stage 3 breast cancer hard.

Being in tune with your body
I think that we all have [the] ability to be intuitive about our own bodies. I can’t speak for men, but I know that women truly know what’s going on. We know what’s going on in our relationships. We know what’s going on in our friendships. We know what’s going on in our bodies.
There’s a part of us that, from a young age, was told don’t make a scene, be the good girl that everyone wants [us] to be, and don’t speak up so we don’t. We push it down.
Cancer gave me the ability to hear that small little voice that says, “Hey, there’s something wrong here,” and communicate it.



Lung resection
He decided that he was going to remove it for “peace of mind,” as he said. Because of its proximity to the breast, I was still in this place where it could very well be stage 4 breast cancer and I just was not comfortable with that.
My PET also came back inconclusive. There was really no reason at all to take this nodule out other than an intuitive inclination that I’m not okay with leaving it there.
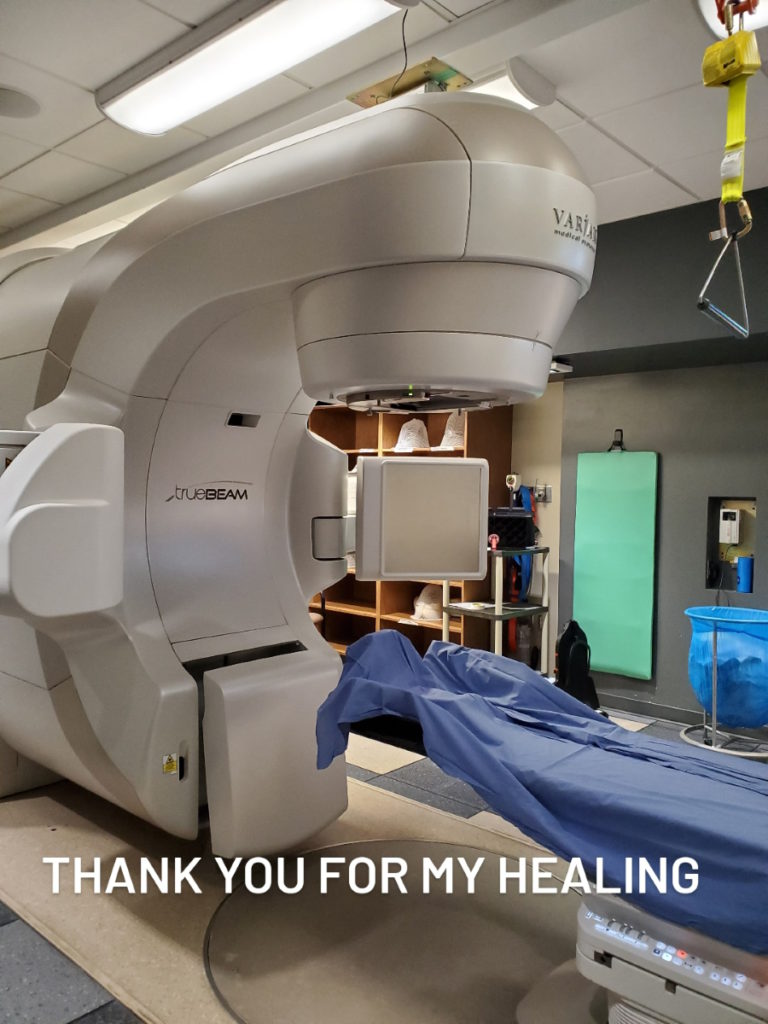
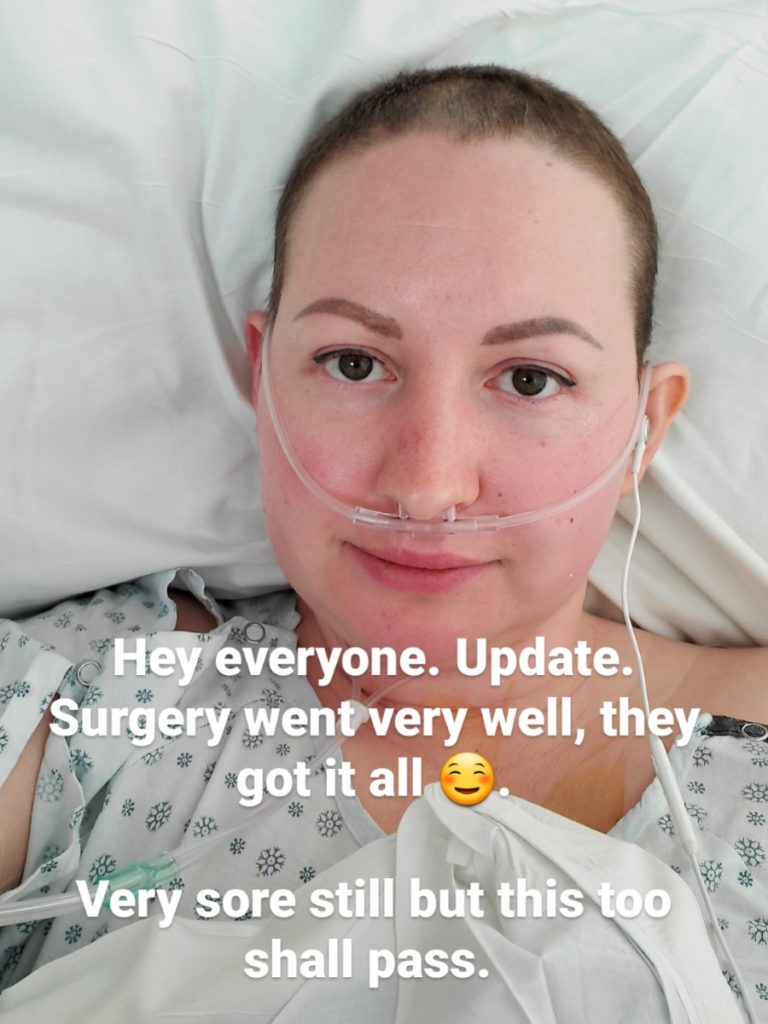
Within two or three weeks, I was scheduled for a lower lung resection. It was about a month’s time from my breast surgery to my lung surgery. Very quick turnaround. They did a laparoscopic surgery in my lung to remove this nodule.


Trauma from the surgery
Everything that I went through was so difficult. But the trauma that I don’t know that I’ve really dealt with was this surgery. I feel it deeply when I speak about it.
When I woke up from that surgery, which was supposed to be quite smooth, I had a reaction of some kind. I don’t recall what the medical term is but it’s a spasming of the lung [where] the patient can’t breathe in deeply.
You wake up drugged, confused, and can’t breathe. The most natural thing to do as a human is to breathe. The scariest thing to lose is breath and it was a very scary time.
It was pretty crazy. It was 45 minutes of me not knowing. They spoke to me, but I don’t know what they said. I know that they said things like, “This will pass,” or “You’ll be okay,” but I don’t recall them saying that. I just remember sipping for air and it’s difficult to remember it.
It’s like the lights would get bright then dim then bright then dim. I remember thrashing, panicking, and not really knowing what was happening.
My husband wasn’t allowed in the hospital because of COVID. He didn’t know what was wrong with me and if I was okay. No one would give anyone any answers. It was awful. It was scary.
Healing from the lung resection
I stayed an extra night in the hospital than they had expected me to based on that reaction. That spasming did a lot of inflammatory damage just from that tensing.
Once I started to heal from the resection, I was able to go home and start working on my lung capacity as well as trying to get my arm strength and my upper chest capacity up. I was doing all kinds of physio all at the same time.
After about two to three weeks, I got a call from the surgeon and he said, “Have you ever smoked?” I said, “No, I haven’t. Why?” He goes, “Well, it was cancer. You were right. It was cancer.” I was like, “Mm-hmm.” And he said, “I’m shocked. I didn’t expect it to be.”
I said, “So what does this mean? Do I have stage 4 breast cancer?” He said, “No, it’s wild because it’s actually second cancer that you had at the same time as your breast cancer in its own primary way.”

Post-surgery plan
I was very fortunate to catch it very early. They’ve never given me an official staging, but from what I understand from my oncologist, he believes it was a 2A, which tends to be completely asymptomatic.
I was really fortunate to have it removed with clear borders right away. There was no treatment plan because we were already following with left-side radiation for my breast and the lung tumor was directly behind my breast on the left side. The radiation took care of what they would have done.
After asking if I had smoked, the surgeon also asked me if I’d ever heard of radon gas. Never heard of it. He said that they’ve tested it for genetic markers and there is none. They said this has got to be environmental.
They asked if I have any way of testing my childhood home for radon gas so that’s what I did. I got connected with the lung association in my province. We tested my childhood home and it came back high.
We believe that the reason that this cancer [was] expressed is because I was already in a breast cancer state so it allowed another cancer to come through that was lying dormant, that we believe is caused by radon gas.



Words of advice
It’s so important to listen to your intuition, to whatever version of speaking that’s coming through to you that says, “Hey, there’s something wrong here.”
We, as women, get ourselves into so much trouble pushing that down because we want to be the good girl and it’s just not serving you. It’s not serving anyone around you.
Speak your mind. Speak your truth. If something says this isn’t right in whatever capacity that is, especially in cancer, stand up and say no. Learn to be the powerful person that you are.
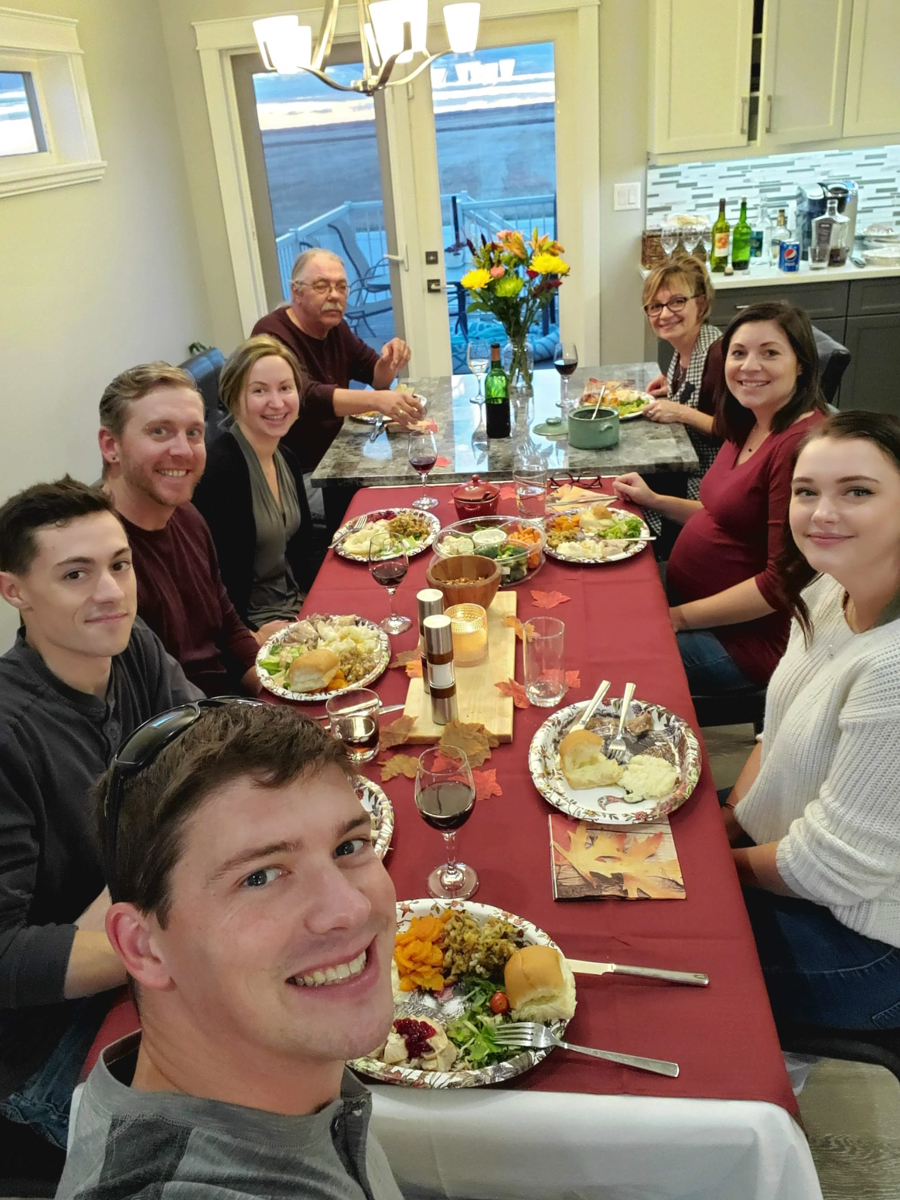
In my life, I’ve always wanted to do some things that I thought, Someday I’ll do them, and one of them is coaching. I always wanted to be in mentorship. I wanted to be in psychology. I wanted to help people, but I felt too small. Who am I to be this?
When I had my breast cancer save me from lung cancer, I just said, “There’s a reason I’m here. There is a reason that I am put on this earth. I’m one of the lucky ones. I got to keep my life.” For that reason, I just live every part of life [to] its absolute fullest.
I launched my career. I now help women going through cancer and I don’t apologize for any of it.
I travel the world. If someone said, “Hey, let’s skydive,” I’d say yes. At this point, there’s nothing in this life that I’m willing to wait for. Because whatever this was that allowed my breast cancer to catch my lung cancer, it was heaven-sent.

Bad things happen to everyone. Sometimes it’s cancer, sometimes it’s divorce, and sometimes it’s [the] loss of somebody you love. So many things that it could be.
Every single time, there is a way to take that pain and alchemize it. There is a way to turn that pain into power. I invite you to do that, to not fall victim to the situation that happened to you, but instead to transmute what you went through into the version of you that you’ve always wanted to be.
I’m so excited to help people. That’s really all I’ve ever wanted to do. Now I’m living my purpose and connecting with people and I’m really grateful.


When she was 31, Christine found a lump in her left breast and was then diagnosed with stage 3 triple-positive breast cancer. She shares the story of how her cancer journey began.
Read Christine’s stage 3 breast cancer story here »

Inspired by Christine's story?
Share your story, too!
Lung Cancer Patient Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza