Tatijane’s Acute Lymphoblastic Leukemia Story (ALL)

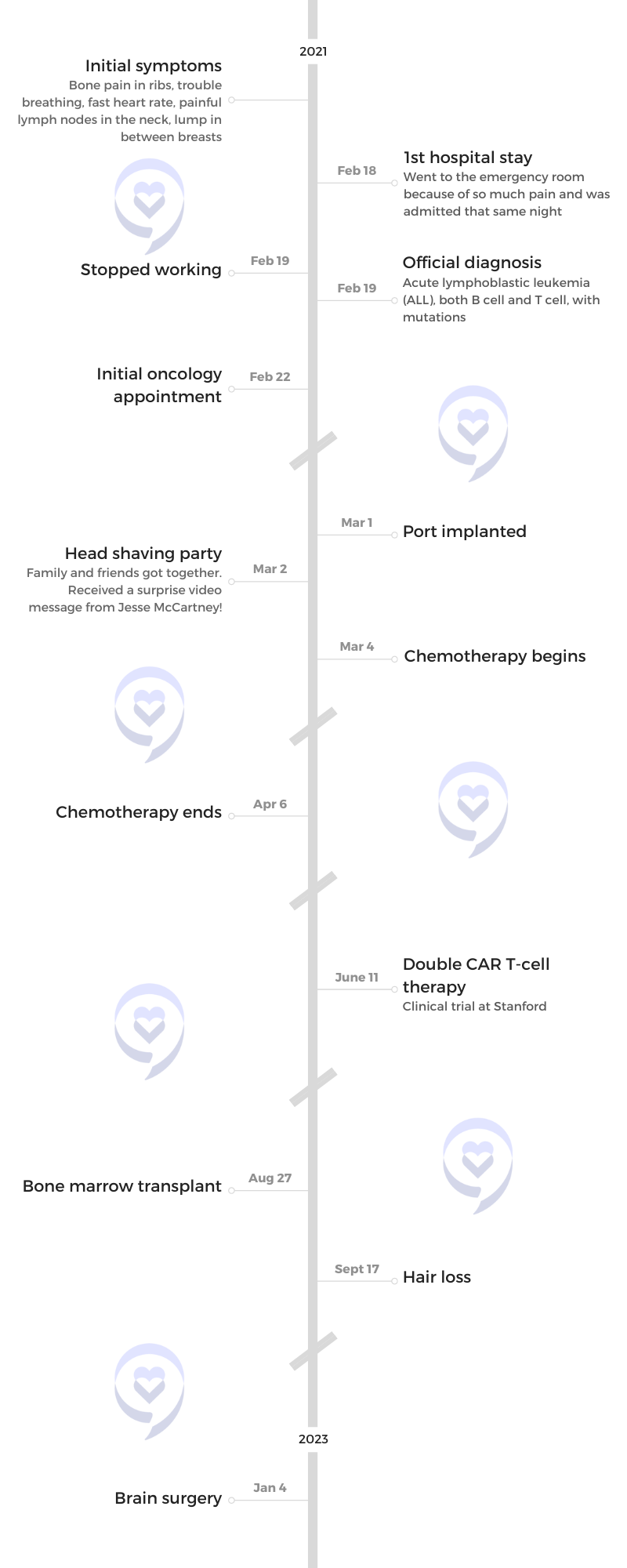
Tatijane first knew something was wrong when she started having pain near her ribs. Her pain became so severe she was rushed to the ER and was then diagnosed with acute lymphoblastic leukemia, both B and T cells, with mutations. At 24, she was then given 6 to 8 weeks to live.
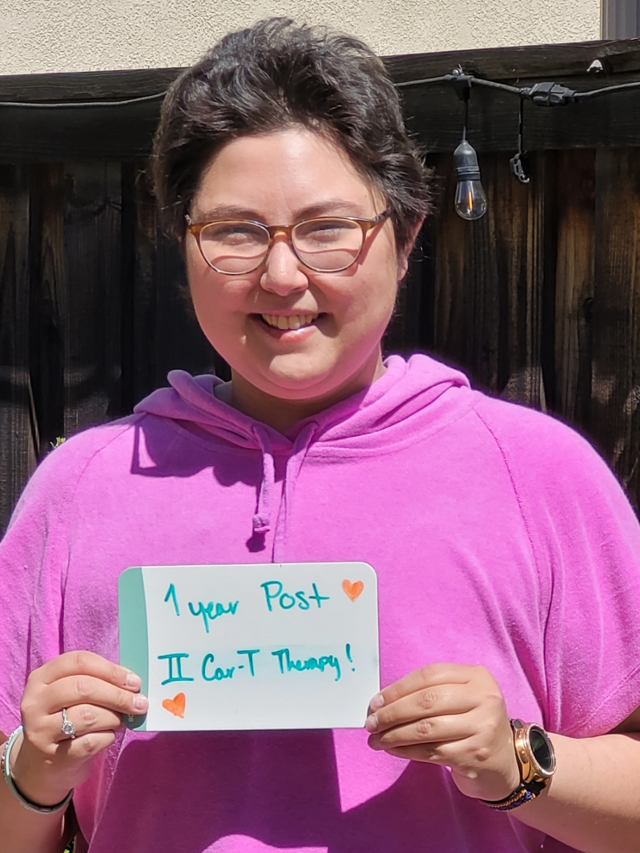
She shares how she processed her shocking diagnosis, the different treatments she’s undergone including a double CAR T-cell therapy clinical trial, and how she’s giving back to the cancer community.
She voices how she coped with three cancer recurrences, the emotional toll her diagnosis has taken on her, and how she found support.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Tatijane W.
- Diagnosis:
- Acute lymphoblastic leukemia (ALL), B and T cells, with mutations
- Initial Symptoms:
- Bone pain in ribs
- Trouble breathing
- Fast heart rate
- Painful lymph nodes in the neck
- Lump in between breasts
- Treatment:
- Chemotherapy
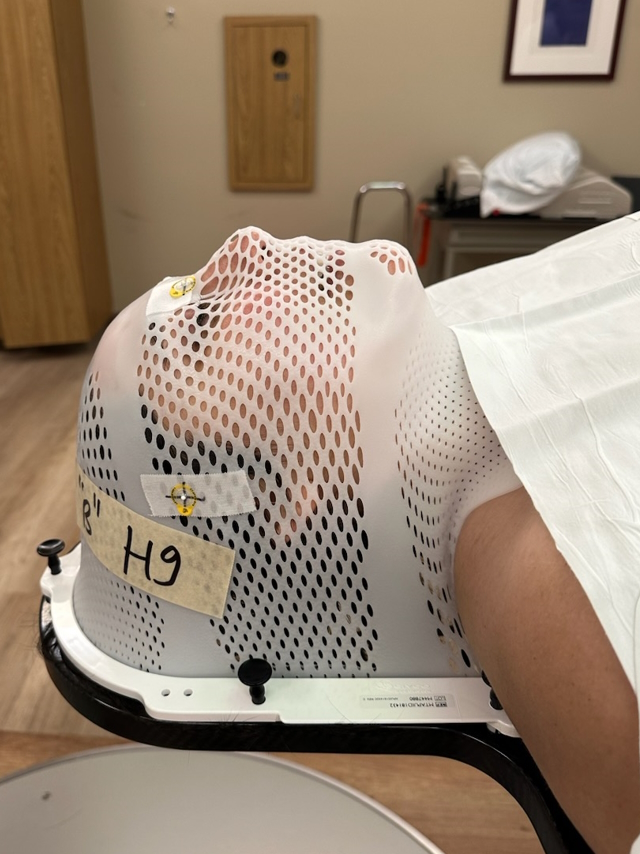
- Radiation
- Double CAR T-cell therapy (clinical trial)
- Bone marrow transplant
Even now, I still feel like death is just sitting there in the corner, waiting and watching me. I’m not a curable patient and, at some point, they say that this cancer is going to take me. But I also am pretty tough and I’m a fighter so we’ll see what happens.
Introduction
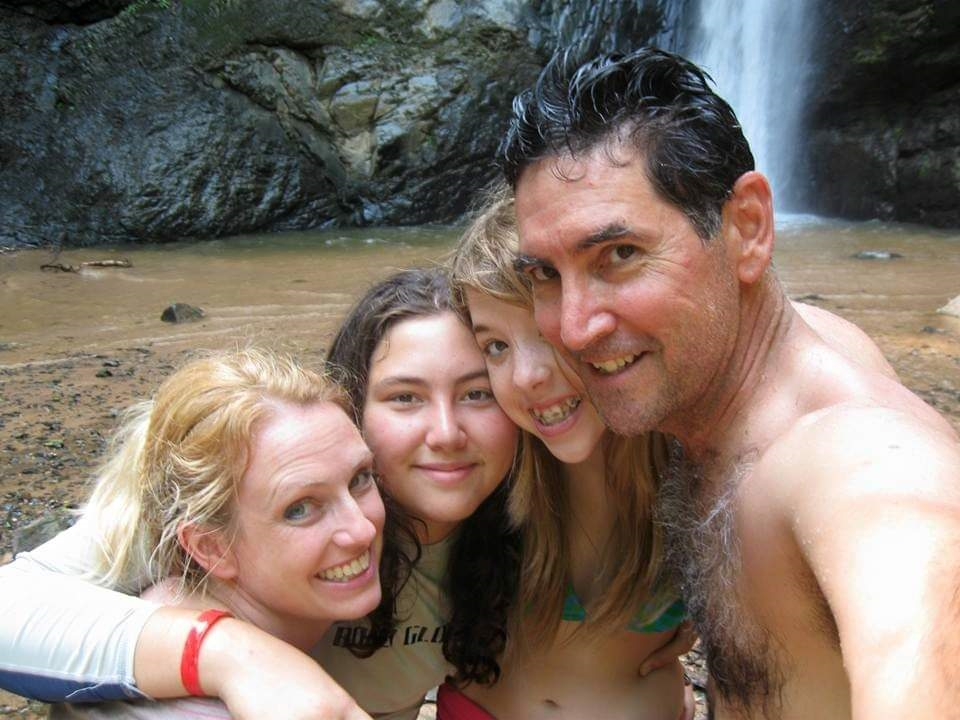
I’m an artist. I do photography, I like to draw [and] paint, [and] I did glass art for a while. I specialized in sandblasting, but I did do some stained glass.
I love music, watching TV, [and] movies. I love crafting and knitting. I like to stay very busy with artsy, crafty things.
I love mermaids. I have a mermaid tail that I actually swim in. My whole house is mermaid-themed.
I love being with my family and friends.






Pre-diagnosis
Initial symptoms
The January before I was diagnosed, I was starting to have bone pain in my ribs. I developed this mass in between my breasts. I started to get what I thought were tight muscles or little knots in my back. It was very painful, but I just kept getting massages from my family to try and get that.
I stopped eating so much because it was hard to eat. I was having issues breathing, but I was also overweight. I was 306 pounds so I thought maybe all of this had to do with being overweight. When I went to the doctors for all these issues, they said, “Lose weight and it will help.”
Then it was, “You have PCOS (polycystic ovary syndrome) so maybe that has something to do with it,” or “You have insulin resistance; that could have something to do with it,” or I also had other hormone imbalances, maybe that has something to do with it. It always came back to lose weight and it’ll go away.
On February 17th, my best friend stayed the night at my house. Then [on] the 18th, I went into the ER because I was in so much pain [that] I couldn’t handle it. I was diagnosed [on] the 19th. It all happened very fast.
Feeling like there was something more there
I didn’t think they were doing enough tests. I thought there was something else because none of it made sense. [What] does this have to do with being overweight? It was very frustrating, but it felt like I couldn’t really get any other resolutions from this.
I was messaging my doctor on the 18th, saying, “I can’t handle this pain anymore. What can I do?” He said, “Just go to the ER. It is a cyst that needs to be drained.” Nope, that’s not what it was.
Being in the ER that night was very traumatic because it was during COVID. I was in the ER by myself. They started running these mandatory ER tests.
They did a scan and saw the masses. The mass on my chest was so large, it was as if I was wearing a sports bra. It ended up collapsing my right lung and it was surrounding my heart and crushing it.
When I was diagnosed, they gave me six to eight weeks to live. I was alone in the ER getting diagnosed with that. It was so crazy.




The doctor had to come in and said, ‘I’m really sorry to tell you this, but you have cancer and it’s throughout your whole body. You would have 6 to 8 weeks to live.’

Getting the official diagnosis
My mom was sitting in the parking lot. Then maybe 10 minutes before they came in to tell me my diagnosis, I said, “Just go home,” ’cause it was already one in the morning. “I’ll call you when it’s time for me to come home.”
By the time she got home, I was calling the house phone. The doctor had to come in and said, “I’m really sorry to tell you this, but you have cancer and it’s throughout your whole body. You would have 6 to 8 weeks to live.”
Originally, they said it was non-Hodgkin’s lymphoma. It was very sad and very scary to hear. I remember trying to keep my composure. I was like, “Okay. How do we resolve this? How did this happen?” He was telling me it could be environmental, it could be genetic, all this stuff.
I remember just crying and going, “Did I do something wrong? Did I cause this on myself?” It was the weirdest. Went from mature, “Okay, how can we do this?” to then just crying.
There was no history of cancer in my family and there still isn’t [on] either side. It had to have been environmental. My family and I think we know what caused my cancer.
For it to be you weren’t listening to me and it was something this serious, that was very frustrating because it was like, ‘Could this have been caught sooner?’
Possible environmental cause
I believe my cancer had come from medication for my insulin resistance called metformin. There is a lawsuit against them. It turns out that the factory that they were getting the metformin from in India had jet fuel or something that ended up being exposed to the medication.
There have been many cases of many different kinds of cancers that developed after taking this medication. I was in the right time frame for that to be a possibility for me.
I strongly believe that is what caused my cancer [and] so does my family. It makes me sad because it was something that was supposed to help me and ended up hurting me worse than anything.
But also, if it didn’t happen, then none of this other great stuff would have happened. It’s a positive, but also a negative. I don’t want anyone else to be put into this situation.
Not getting answers when you know something’s wrong
It was frustrating. My whole life, if anything was wrong with me, the answer I always got was, “You need to lose weight.” I was used to it.
I’m used to doctors not listening to me. But then for it to be you weren’t listening to me and it was something this serious, that was very frustrating. Could this have been caught sooner?




Official diagnosis
They were thinking it was non-Hodgkin’s. But after doing more tests, they realized that it was acute lymphoblastic leukemia, both B- and T-cell with other mutations.
I understand that my cancer is one that you either have one or the other, not both. It’s not typically found in adults and it usually doesn’t grow as fast as mine does.
Treatment
They [said], “We have to get you an oncologist and we have to keep you here until we could do the next steps.”
I spent the night in the ER. The next morning, they admitted me into the hospital for about two weeks.
I couldn’t see my family and friends in person except out the window of the room that I was sharing with someone. I was on the third floor so I would look down and they looked like little ants.



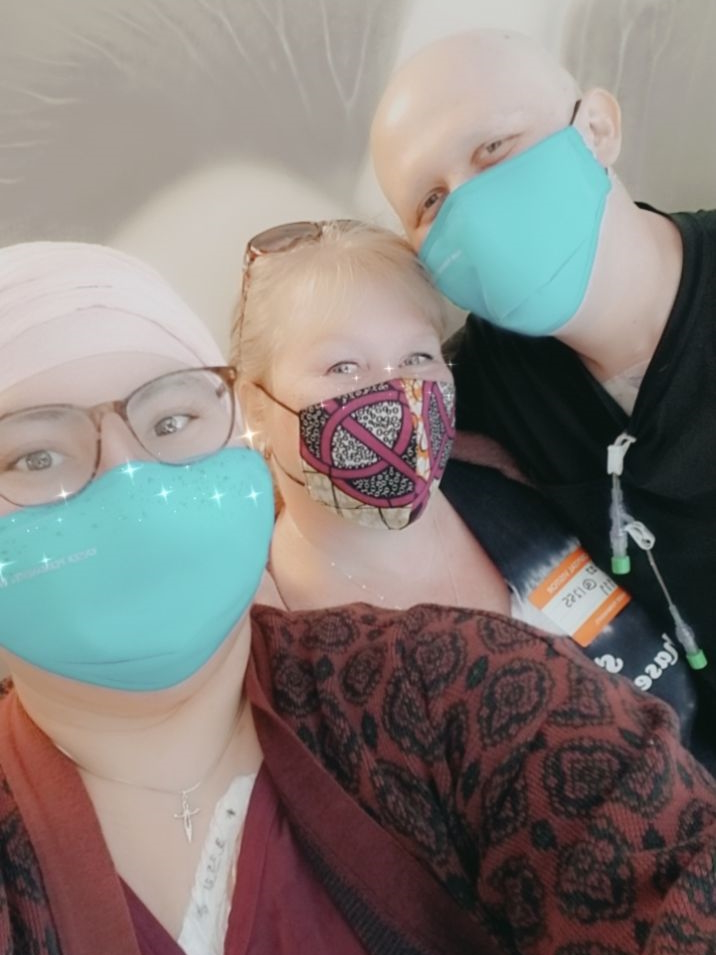
I was having such a tough time and I was crying. Luckily, one nurse, the head of that floor, came in to talk to me. She actually allowed my mom — if she had her COVID vaccinations, took a COVID test beforehand, wore a mask, all that stuff — to come in.
It was the first time I saw her since going into the ER. I just cried and hugged my mom. That was all I wanted to do because it was such a scary moment. I will forever be so grateful to this woman because for her to let me do that was the best thing ever.


Treatment plan
I got my oncologist. I was released from the hospital for about four days, just enough time to pack.
I started my stay in March. It was [a] six-step plan. I don’t remember what it was called, but the first step was being in the hospital, getting different types of chemos around the clock in a way. I got spinal tap chemo, chemo through the veins. I did radiation as well. I did that for the whole month.
We checked my body with a PET scan and I was actually in remission. It was so exciting. Then they started step two.
Halfway through, the mutations figured out the treatment plan and mutated to fight against the treatment so I was no longer in remission. Because of that, we couldn’t finish the six-step plan.
Luckily, my oncologist was talking to Stanford and they had a double CAR T-cell therapy trial going on. I said, “Yes, I will do anything.” I know that it was a trial. But knowing that going through this could possibly cure me [and] also help other people in the end, that was super important to me. My whole life, I just wanted to help people.

Double CAR T-cell therapy clinical trial
We went to Stanford [and] did a double CAR T-cell therapy. I did it in June and it was fantastic.
Dr. Muffly at Stanford, who was doing the trial, [was] the one that talked to me and became my primary over there.
I did actually have neurological problems through it. There were side effects, but in general, the process is very easy and it was very interesting to learn. That put me in remission for a little while.
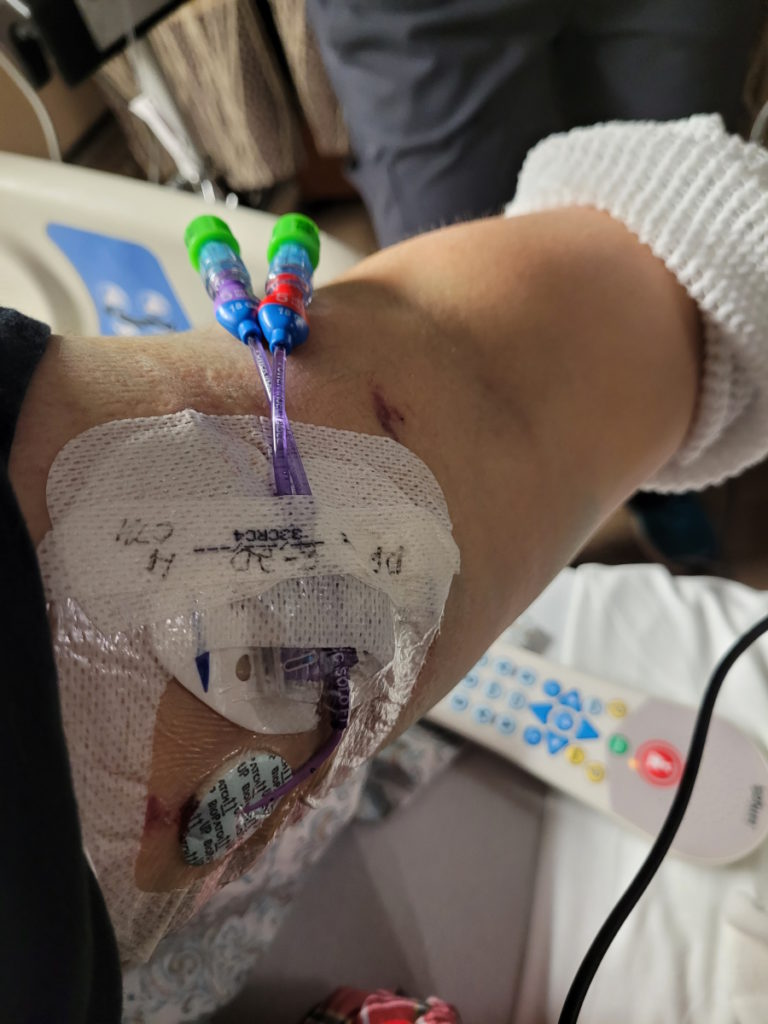
Two weeks before I went into the hospital for the double CAR T-cell therapy, I went in as an outpatient and they took the T cells out. It was a very easy process. It was just like giving blood if you’ve ever done that. They just take the [T cells] out and put the remaining blood back into your body.
What they did with the T cells was make them like little ninjas. You get put inpatient and when they put the CAR T cells in my body, it was just like getting any other infusion. Then you just hang out and see what happens.
They watched you. They do neurological tests every day where they ask you questions. You have to write your name every day as well to see where you are [and] if you’re going to have a neurological issue. They watch for other side effects as well. But for the most part, it’s just easy.
I was in remission for a short time. Then I came out of remission. The cells that they were attacking were C19 and C21. My body figured out the treatment plan again and changed itself to then attack the CAR T so the cancer began to grow back.
It was only maybe a month or two. It might not have even been that long because I got my double CAR T-cell [on] June 11 then I got my bone marrow transplant [on] August 27. It wasn’t that long in between.
The process of joining a clinical trial
There was a lot of paperwork. They go through that information with you. I remember being in the office and it ended up being like an hour and a half meeting instead of a 30-minute meeting because there was just a lot to go through.
They explained how the process worked as [simply] as they possibly could so that was nice.



Honestly, the bone marrow transplant was the hardest treatment I have been through.

Bone marrow transplant
We tried a bone marrow transplant. They knocked everything out of my body. At that point, I was [at] Stanford for about four or five months already for the double CAR T and then another five to six months for the bone marrow transplant.
Honestly, the bone marrow transplant was the hardest treatment I have been through.
They already knew that I needed a bone marrow transplant prior to the double CAR T. They just thought that they would get a little bit longer before they can give it to me, but it really wasn’t that long.
They [paired] with Be The Match to find a match for me and I ended up getting the perfect match. They were a year younger than me, but that was all I knew.
I did four days of radiation, twice a day. It was [the] full body but also localized to the lung area and sternum area. I also did heavy-duty chemo for about four days to maybe even five days. Then they gave me the bone marrow, which was the big bag.
My donor went above and beyond to be able to be my donor. They got a tattoo a few months prior to being asked to be my donor because they had no idea. They told me, “They can’t be your donor now unless you say that it’s okay.”



My donor got all the information to show this is a good location where I got it, all the stuff was clean, [and] all this other stuff, went above and beyond to still be my donor. I was like, “Of course, yes, they could still be my donor. Let’s do this.” The fact that they did that was so amazing to me because that really showed they really wanted to help.
They gave me the bone marrow and that was a three-hour process, I believe. Then I just hung out in the hospital as the side effects started.
With a bone marrow transplant, you get graft versus host disease. To treat graft versus host disease, they give you steroids. They did that and immunosuppressants.
They figured out that my cancer feeds off of those. I was in remission and then I wasn’t because the steroids and the immunosuppressants caused my cancer to grow.


I think that one was maybe two months. I got to go home a week before Christmas after my bone marrow transplant. I was not in remission at that point, but it was low enough that they could deal with it.
Then after that, I was put on experimental chemo, called navitoclax, paired with venetoclax, which is a normal chemo. I was on that for seven months. I did really [well] and then my body figured it out.
Now I’m on Blincyto. I’m on my two-week break. After two weeks, I get put into the hospital for two days and start round two on the day that I get admitted.
I’m watched for two weeks, get sent home for the remaining four weeks of treatment, and then go to the infusion center every week to get my bags changed. Then two-week break and then back in the hospital for round three. They want to do this for as long as my body will allow it, basically.
I was trying very hard to be positive, but it was difficult during that time.

Side effects
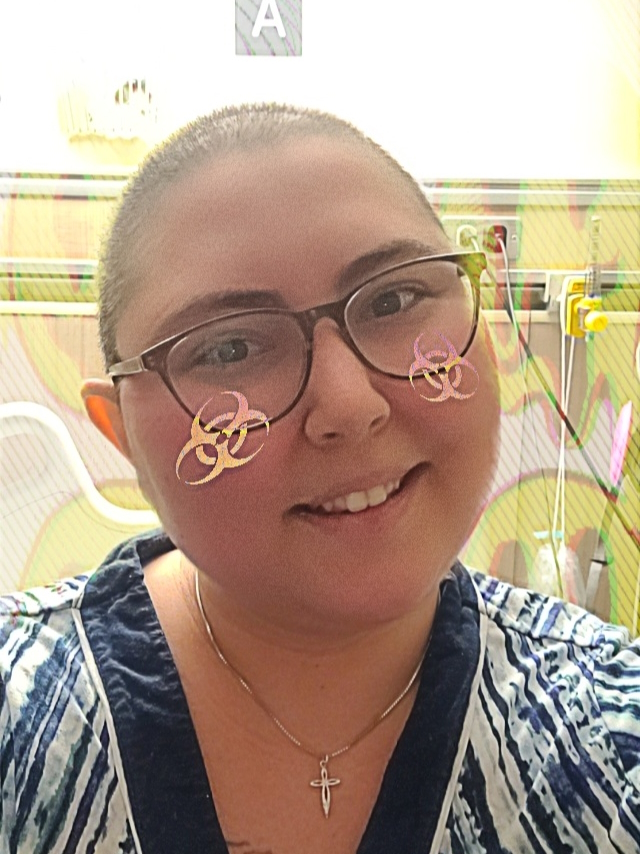
With every other treatment I got, they promised me my hair would fall out. Then when I did the bone marrow transplant, they said, “Your hair is probably not going to fall out.” Then my hair fell out. I was so excited because [I’d] been waiting for it.
I wanted to take control of my cancer. I did a head-shaving party with my family and friends. Jesse McCartney actually ended up doing an inspirational video for me. My family and friends got together and made that happen for me so it was super fantastic to see that. I’ve loved him since I was five. I actually cried.
My depression hit me really hard at this point. Although my family [was] coming to see me, I was alone and I just didn’t feel great.
They would give me medication for nausea and other side effects. I did get really bad mucous.
When the mucositis hit me, it went from my mouth to my butt and it was so painful. I was fighting the doctors on the pain meds because I was so afraid of becoming addicted. Not that I’ve ever been, but I was fighting them on it and I was like, “No, I have to do it myself.”

I got to the point where I couldn’t talk because I was in so much pain. My lips were so swollen and they were bleeding. I ended up getting on pain meds, which were very helpful.
I decided that I’m not going to fight doctors on it anymore, which is funny because I just fought my doctors on pain meds for my nerve pain, but then I gave in at some point.
I also got C. diff at the same time plus side effects from the radiation and chemo, including nausea, vomiting, [and] diarrhea. Smells change. Smells can trigger nausea and sickness. A lot going on. I did not feel good.
I was trying very hard to be positive, but it was difficult during that time.
I’m also very happy it happened the way it did because that was the hardest treatment. I was in so much pain. I probably lost the most weight during that treatment because I stopped eating completely.
They had to feed me through a tube in my PICC line, which is the hardest weight loss program ever. I ended up losing 100 and something pounds [from] being diagnosed to the end of my bone marrow transplant.

Managing the side effects
For nausea, Gin Gins® from Trader Joe’s. I don’t know if other places sell them, but those helped me so much. Also having unused coffee grounds, near the door or any place [where] the smell could get through, helped. I would sometimes put it on the table by my bed so that would help me not get nauseous.
Chewing on ice helped me a lot. Ginger ale. There is something called magic rinse that helped with my throat and my mouth. I would just swish that and swallow it. It numbed it enough so that I wouldn’t have the pain for a while so that was nice.
Having a latrine next to my bed, as opposed to walking to the bathroom, helped. Trying to do things to keep my mind off of it also helps so I did a lot of crafting, a lot of drawing, and stuff like that.
Mental health
I think my depression started the day I was diagnosed. I already had really bad anxiety before [my] diagnosis, but it also got worse. I’d been like this throughout the whole treatment.
I’m a very happy and positive person. I believe that that is what’s been helping me also get such good results from my treatment. But it is okay to also have that dark side along with your bright side. It’s like yin and yang.


During my bone marrow transplant, my depression was really, really bad and that is when the Stanford psychiatry department came to talk to me. They ended up telling me that I actually had PTSD, anxiety, and depression, which made a lot of sense.
I was having really bad nightmares about me dying, which would wake me up and then I would be up for a long time. I couldn’t go back to sleep afterward and I was scared to sleep. Then during the day, I was just so unhappy.
I wasn’t eating because I also have body dysmorphia that I recently learned about, but apparently, I’ve had it my whole life. It was all just piling up.
Then the anxiety with scans and bone marrow biopsies that any time I hear bone marrow biopsy or spinal tap chemo, I instantly get really bad anxiety. I have panic attacks constantly. This is something I deal with now.
I will be fine throughout the day. I’ll be happy. Then, for example, I will have to go to the grocery store to go get something and I will have a panic attack because of germs. I wear a big pink HEPA mask and I would sanitize my hands, but I’m so scared of getting sick and doing something to mess up whatever treatment I’m on that I react to it.
During the bone marrow transplant, my depression hit me so hard that when I was in the apartment [after] I was released [from] the hospital, all I did was sleep. I was awake for maybe 30 minutes a day. That’s how it was for a couple of months. It was really bad.
It hit me so hard. I didn’t get on medication or anything to help any of it until recently, but it was also because I wanted my body to feel. I wanted to figure out a way to get out of it myself. I don’t know why.



I’m a very happy and positive person… But it is okay to also have that dark side along with your bright side.
Reaction to PTSD diagnosis
I didn’t really understand what that meant. I did research afterward because I didn’t know that ordinary people could get PTSD.
Hearing that, looking into it, and realizing that was the cause of my nightmares — in a way, it’s helpful to have a label on what’s wrong with you.
But having a label doesn’t change it and it doesn’t fix it. You just know what it is and that’s it. It was nice to know, but it also didn’t really help fix it. It just gave it a name.
Taking care of mental health
I ended up going to therapy and two different group therapies, which helped me. My therapist is independent and then the group therapies, one of them is for blood cancer and one of them is an AYA program.
AYA is through UC Davis and then the blood cancer is through Sutter, I believe. But they allow people from everywhere to come and join, which is fantastic.


I also did get put on medication for anxiety and depression.
With my therapist, we worked on the things that were causing nightmares. Death and the 6 to 8 weeks to live [were] causing a lot of anxiety. Yes, I outlived that, but when is it my time?
Even now, I still feel like death is just sitting there in the corner, waiting and watching me. I’m not a curable patient and, at some point, they say that this cancer is going to take me. But I also am pretty tough and I’m a fighter so we’ll see what happens. We’ll see who’s right.
Having to work through accepting death as a potential because with life is death so just accepting it helped the nightmares go away. Doing work like that I think helped a lot.
To be in these support groups and also talk with people that know what you’re going through and understand was super helpful and beneficial for me.
I wish I knew them [earlier]. In that first year when I was going through all these treatments and going in and out of remissions, I would have loved to be in these support groups and this excess support besides my family and friends.

Words of advice
Your emotions are completely validated 100%. You don’t have to be positive all the time. It is great to be positive, but [not] toxic positivity.
I thought in order to survive this cancer, I had to be positive all the time and hold the darkness in and that’s not how it is. It’s okay to let them live together. It’s okay to scream and cry and have those emotional moments. It’s very cathartic to do that sometimes.
Go to online programs. I found my blood cancer group therapy through Wellness Within. Finding cancer links to help you, whether you’re AYA or not, is very helpful.
Be completely honest with your caregivers, but also with your doctors on how you’re feeling. It’s okay to say I need therapy. It’s okay to say I need help sleeping. Whether you want to do it naturally or through something else, it’s okay to just tell them everything.
At this point, I’m an oversharer because I tell everyone everything that I’m thinking and I’m feeling.
I have found that when people ask, “How are you doing?” It’s easier for me to say, “Emotionally, I’m this. Physically, I’m this. Spiritually, I’m this.” That has been the easiest way to answer that question instead of just going, “I’m fine. I’m happy.” I’ve compartmentalized everything.
Know that you can do it, even when times get hard. You are a fighter and you can do this. You got this.



You are a team with your doctors… How is your team going to run well, if you’re not honest with each other?

Advocating for yourself
Knowing that your life is your life. No one can do it better than you. It’s okay. You’re not annoying the doctor if you are pushing them and saying, “No, no, no, there is something wrong. Please test for this.” Even if you don’t know what to test for, push for it because it’s your health in the end and your life and that’s the most important thing.
When I first got diagnosed, I was so worried about annoying the doctors that I didn’t want to tell them if I had a side effect. I was like, “Oh, I’m okay, I’m fine,” and put a smile on my face, and that wasn’t the case.
I realized that was hurting [me] more than anything. I was so uncomfortable that it was unnecessary. Just being able to advocate for myself and be like, “Okay, here’s how I’m actually feeling. What are your plans? What are your ideas on this?”
You are a team with your doctors. They are not working for you, you are not working for them. You’re a team and that’s just how it is. How is your team going to run well, if you’re not honest with each other?
You have to lose that filter. You’re going to have to tell them everything. You’re going to show them your whole body and that’s okay. Again, it is your life so [advocating] for yourself is the most important thing that you could do.


Giving back through participating in clinical trials
For me, one of the things that helped is knowing that doing these clinical trials can help me, but even if it doesn’t help me, I’m helping scientists, future patients, current patients, [and] doctors learn more, potentially putting these treatments on the map for the future. That to me is fantastic.
In these trials [and] in treatment in general, you meet some pretty great people. I’ve become friends with people that have gone through the trials after me.
My Stanford doctor said, “Hey, they’re going to do this treatment. They’ve never done it before. Can you talk to them?” I’ve made some of the bestest friends that I’ve had that understand what I’m going through and I understand what they went through.
Cancer sucks, but there’s been so much good and positivity that [has] come from it. Being a part of these trials, meeting these people, and knowing that I’m helping [have] been one of the biggest, positive things that have come from it for me.
Whoever is out there battling cancer, you can do this. I know that it’s frustrating and it’s hard, but just don’t give up. The fight is worth it because the fight is you. You are the fight and you are completely worth it.
All feelings, whether negative or positive, are okay to feel.




It’s frustrating and it’s hard, but just don’t give up. The fight is worth it because the fight is you. You are the fight and you are completely worth it.

Inspired by Tatijane's story?
Share your story, too!
Acute Lymphoblastic Leukemia Stories
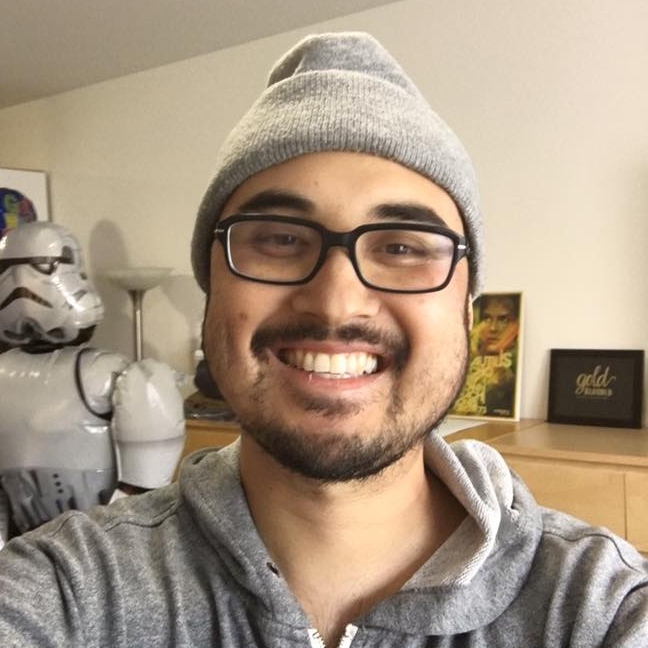
Evan L., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Extreme fatigue, easily bruised
Treatment: Chemo infusions, chemo pills, spinal taps, cranial radiation
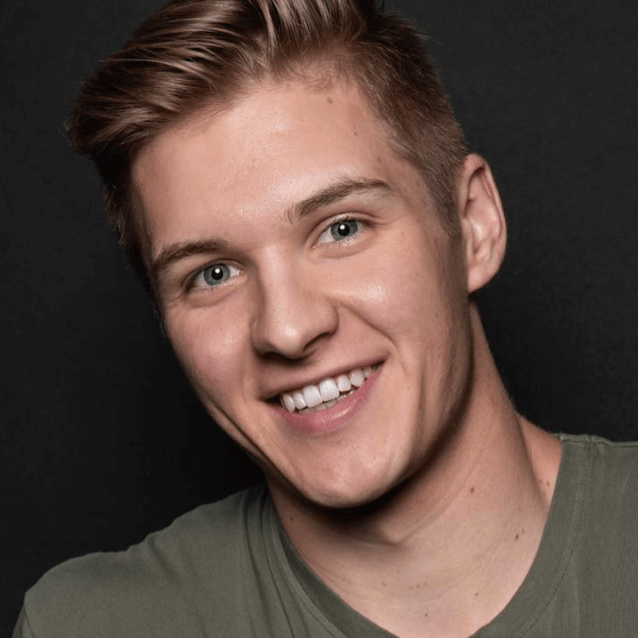
Casey H., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Lump on throat, extreme fatigue, shortness of breath, bruising easily
Treatment: Chemo, immunotherapy, radiation, stem cell transplant
Veronica B., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Mild shortness of breath and palpitations
Treatment: Chemo, targeted therapy, double cord transplant
Christine M., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatment: Chemotherapy, bone marrow transplant
Ciara T., Acute Lymphoblastic Leukemia (ALL)
Cancer details: Treatment without blood tranfusions
1st symptoms: Fatigue, shortness of breath, night sweats, petechiae
Treatment: Chemotherapy
William Y., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Extreme fatigue, achey hands
Treatment: Chemotherapy, CAR T-Cell therapy
Lauren J., Acute Lymphoblastic Leukemia (ALL)
1st symptoms: Extreme fatigue, easily bruised
Treatment: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
1st symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatment: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)
Anna T., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-negative (Ph-ALL)
Symptoms: Heavy period for a few hours, fatigue, feverish, sweating, bruises on legs
Treatment: ECOG 10403
Tatijane W.
Symptoms: Bone pain in ribs, trouble breathing, fast heart rate, painful lymph nodes in the neck, lump in between breasts
Treatment: Chemotherapy, double CAR T-cell therapy (clinical trial), bone marrow transplant