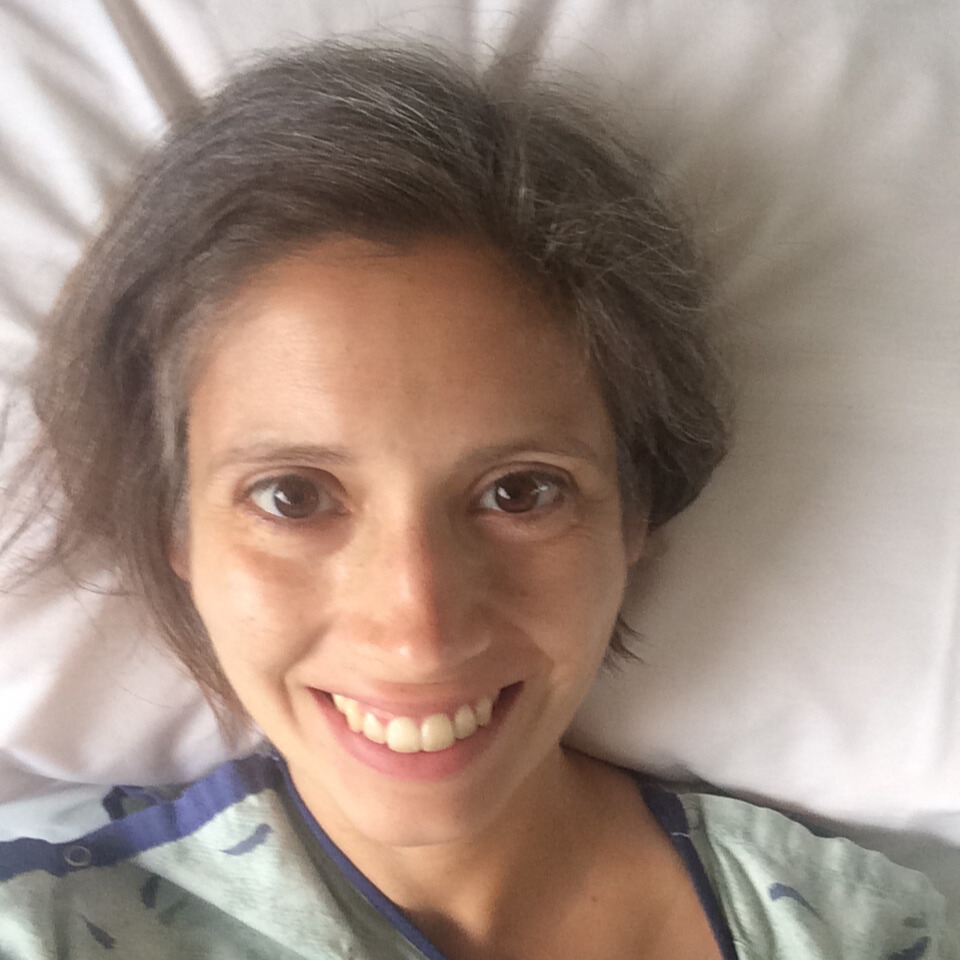
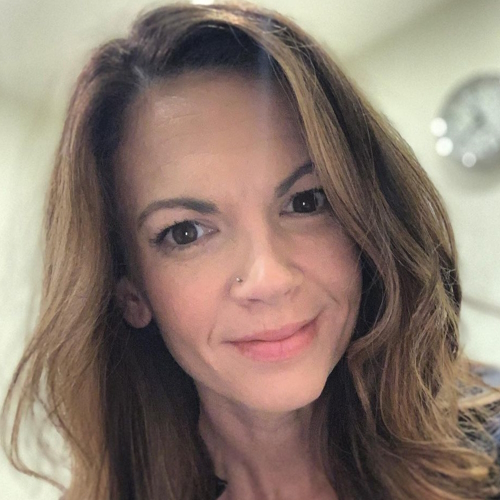
Amy’s Stage 3B Colorectal Cancer Story
Amy was told her symptoms were all in her head. As a mom of two, she began to feel “off” and tired and got some bloodwork to assess her health. After her bloodwork returned clean, her doctor attributed her symptoms to anxiety.
She started seeing a counselor and prioritized her mental health but her symptoms only got worse. After finding blood in her stool, she demanded a colonoscopy.
After the procedure, her doctor admitted he was wrong and Amy was diagnosed with 3B colorectal cancer.
She voices how advocating for health saved her life, the importance of knowing your genetics, and how she’s working to break the stigma of colorectal cancer.
She shares her experience undergoing stomach surgery, learning to live with an ostomy bag, and finding her “new normal” after cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Amy H.
- Diagnosis:
- Rectal cancer
- Staging: 3B
- Initial Symptoms:
- Feeling off
- Abdominal pain
- Bloating
- Weight loss
- Blood in stool
- Thin stool
- A massive shift in bathroom habits
- Exhaustion
- Treatment:
- Radiation
- Chemotherapy: Xeloda & oxaliplatin)
- Surgery: total proctocolectomy with ileostomy, APR reconstruction, and radical hysterectomy
Let it out, cry it out, and then get up and try to live every day the best that you can. It slowly, slowly, slowly does get better after cancer.

We all just do the best we can where we’re at. If I just do one step at a time, one test at a time, one idea at a time, I’ll get there.
Introduction
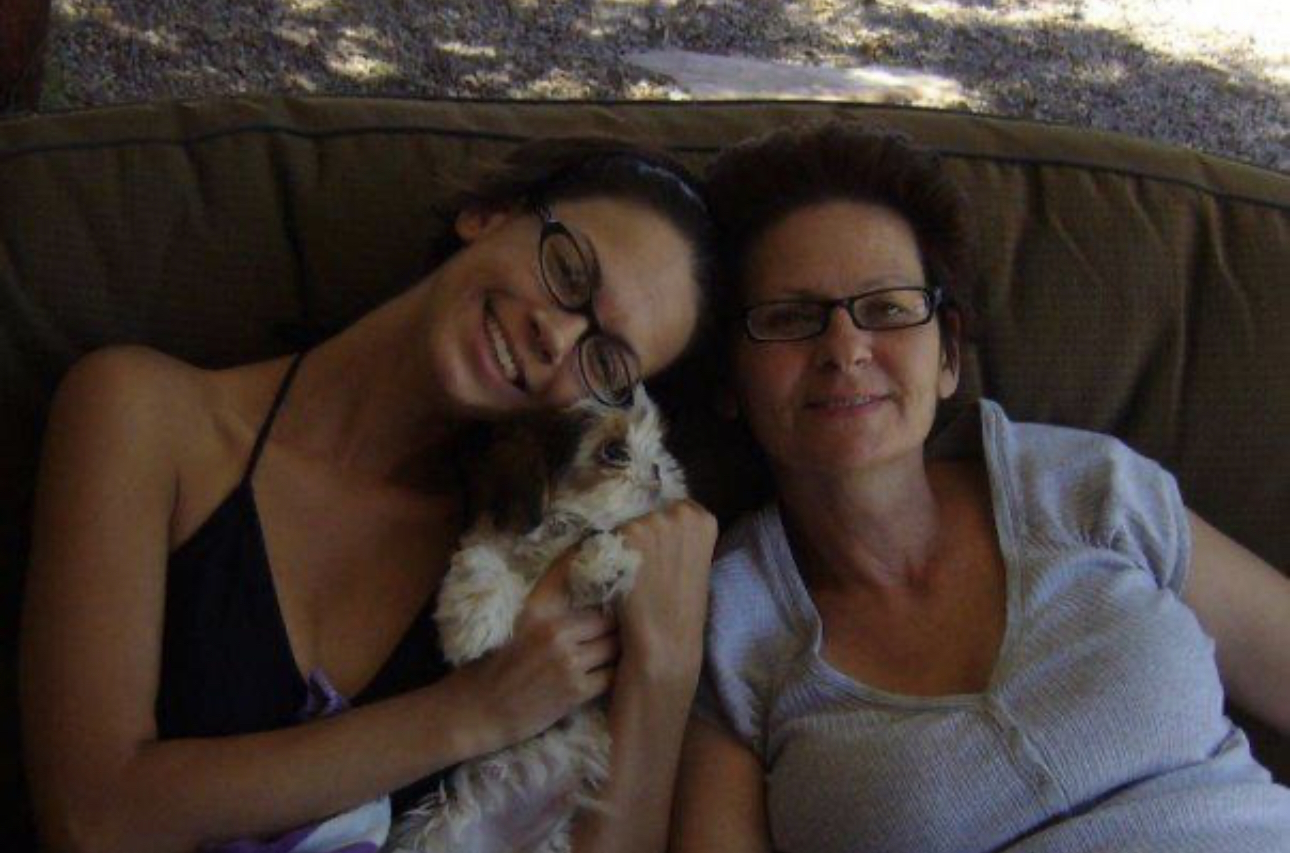
I’m 37 [and] am a mom of two young girls. Being a mom takes up so much of my life. It’s very encompassing, but I love spending time with them.
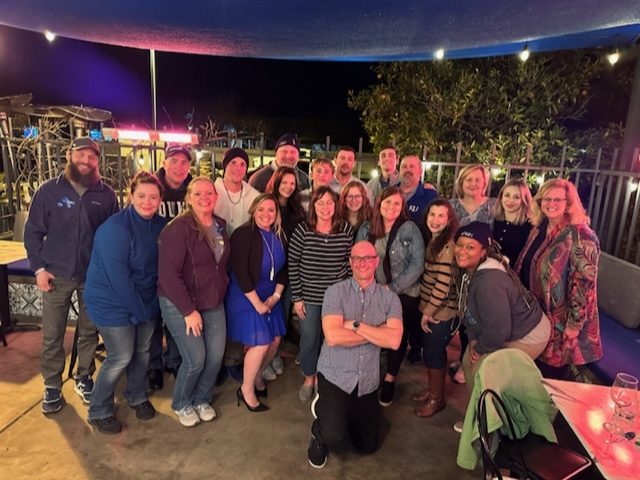
I love concerts, spending time with my friends, [and] traveling to new places.




Pre-diagnosis
Initial symptoms
About a year before my diagnosis, I really was not feeling myself — rundown, irritable, [and] not feeling good. I chalked it up to being a mom.
I saw my primary care physician and had some blood work done. Everything came back standard. My symptoms weren’t really directly [associated] with colon cancer at that time.
I sought mental health treatment, [talked] to a counselor to figure out if this was something going on in my head. I know that’s a common theme among women who’ve been diagnosed with cancer. We tend to be given this list of other reasons that it could be and then we run down that list.
My more acute symptoms came closer to my diagnosis and that entailed really intense abdominal cramping. I had a total change in my bathroom habits.
I was [losing] weight and I was not intending to. I’m a smaller person. I was looking very thin, even for me.
I went from being slow-moving in the bathroom [to] things running through me. I could tell something was up that way.
Then finally, the very serious symptom that usually pushes people over the edge: I had blood in my stool.
It was a week before our family went on a camping trip. We love these cabins in northern Arizona and we go often. That week before that, I was starting to have blood. At first, I was just like, “Let’s hope that goes away, whatever that is,” and it just continued and continued.
I remember thinking, I’m so embarrassed. I don’t even want to have to tell my husband [or] my doctor any of this, but I knew that it was going to take something serious to figure out what was going on.
At that point, I knew. I had [a] family history of cancer. My grandma [had] colon cancer when I was a baby, literally a newborn. She fought colon cancer in 1985. And so I had in my mind that this is not normal.
I went to my OB because as a woman, I feel like you just look to your OB first. She said, “No, this is not normal bleeding for hemorrhoid or post-childbirth.”
The bleeding was probably the biggest indicator that something was truly wrong, but those other symptoms can be a little vague. Knowing your family history and your body [are] really important.
It was late summer, right around August. [In] September, things started to progress. I put in to see my OB. She could see me two and a half weeks later. Saw her two and a half weeks later. She told me, “This is wrong. This is not right.”

I could feel him saying it’s so unlikely that this is colon cancer, especially colon cancer that’s causing you to bleed. But the alarms in my body and my mind were going off.
She referred me to the GI who saw me, again as it goes, two and a half weeks later so now we’re in October. [I] had to kind of fight him for that colonoscopy and basically tell him, “I don’t care if I have to write the check. I don’t care what it takes. I need this colonoscopy to know what’s going on inside of me.”
It was a little intense because I feel like I could feel him saying it’s so unlikely that this is colon cancer, especially colon cancer that’s causing you to bleed. But the alarms in my body and my mind were going off.
I remember there was a point where it was like, “Either put me on the schedule or just call your security and they can escort me out because I need this colonoscopy.” He was like, “Whoa, whoa, whoa, Miss. It’s okay. I will give you the colonoscopy.”
He was happy to do it for me. It scares me sometimes to think that had I just accepted the answer, had I not been the hard head that I am, this might have not happened in the time frame that this all happened.
I needed that colonoscopy so I could get into treatment so that I was ready for surgery because the world shifted after all of this happened.
I found myself having to really pull that backbone out and say, “Nope, I need the colonoscopy. I don’t care how unglamorous, I don’t care that I have to do prep. I need it.”
Something I’ve learned through this about colonoscopy is that’s really important to know exactly what’s going on in your colon. It’s the best way for doctors to diagnose you if you are having symptoms. Of course, if you’re 45 or older, no questions. You need to get it done.
Even with my family history [and] the acute symptoms I was showing, it was pretty startling to me, looking back, how I still had to advocate so hard. I really shouldn’t have because I had all of these things lining up.
I think it’s why I really want to get this out there. You know your body. I was telling medical professionals, “Something is wrong with me.”
To their credit, they’re going off of so many numbers, but the numbers are changing. Genetics and genetic predispositions, we’re learning so much so quickly. They’re playing catch-up.


Diagnosis of Stage 3B Rectal Cancer
Once they did the colonoscopy, to that doctor’s credit, he did come and face me to say, “No, I was wrong. You have cancer.” He didn’t use the word advanced cancer. He just said it’s not new. It’s been there.
Come to find out that it probably wasn’t. It was likely about two years. Because of the Lynch component, I think it propagates faster. It’s one of those things [of] him not knowing as much about Lynch as probably a doctor who is in GI now coming through. I’m sure now he handles it much differently and is educated, but it is hard to be that kind of person who shifts over the understanding.
It was an intense conversation, but I felt like, “I don’t even care what you think of me, Doctor. I’m going to say I need this. If I’m wrong, great. That’s the beauty of this test. We can know that.”
I was very drowsy from my colonoscopy, but he had to come out, grab my hand, and say, “Amy, it is cancer. You were right.” I know that was probably a watershed moment for him in his career, too, because he did tell me I was one of the only patients he’s ever diagnosed that was under 50 or 60.
I’ve talked to other people in the colorectal world about this since then. Sometimes, it’s a wonder if you’re not getting people diagnosed because you’re not providing the screening to them that they really should be getting. How many people slip through the cracks?
I know every person who shares their story says, “Be your own advocate,” and then when they push back, go further. Push more.



Initially, when I came out of the colonoscopy, the GI doctor told me he didn’t think it was new, but he believed that I was probably about stage 2. It was arbitrary at that time, but he was looking at the size of the tumor, where it was, and everything. They really can’t tell you much initially.
I left that colonoscopy knowing I had cancer, knowing it was not a little tiny nothing that they could have taken out. He didn’t touch anything when he was in there because he was so nervous about where it was at. Was I right on the verge of it breaking through my wall, the colon wall, or any of that?
You get thrown back out into the universe with, “Okay, now you have cancer and it’s going to take about a week for us to do this test, this test, this test, this test to say you’re either stage 1, 2, 3, 4.”
During that time in between, I remember saying, “I want to remember this time,” because I didn’t know if the cancer was everywhere. Immediately, it felt like, “Oh my gosh, my body is riddled.”
Thankfully, I was able to have those three procedures within that week’s time. I had a more intense colonoscopy then I had [a] CT and two MRIs to come out with the diagnosis of stage 3B, which means that it had not broken through that wall. It was very close. We were very close to widespread impact.


The GI doctor referred me to their person; I went a whole different way. But the oncologist I found, he’s amazing.
[He] and his team right away said, “This is Lynch syndrome. We want you to have the blood test, but you likely have Lynch syndrome. That’s why you have it so young and that’s why it’s so advanced.
“Here’s what we’re going to do if this test comes back positive. Here’s the plan.”
They never told me what the other plan would have been. It was like, “We’ll talk about it if it doesn’t come back positive,” but it did come back positive.
My tumor itself is a Lynch-related tumor, but it’s not MSI high (high microsatellite instability).
What is Lynch syndrome?
Lynch syndrome is a genetic predisposition to certain cancers. There is a list of them but most notably, it’s colon cancer.
In 2011, I lost my mom [to] uterine cancer. At the time, they didn’t quite understand the link between the two. Lynch syndrome was already being talked about, but it takes time for the information to get out there.
Unfortunately, when my mom passed, it was just like, “Well, that was a terrible thing and now move forward in your life.” Whereas if I had this information, they’d say, “Your grandma passed of colon [cancer], your mom passed of uterine [cancer] — these are Lynch family cancers.
“You need a colonoscopy now and have them every year, every three years, depending on your results of those,” and I would have caught my cancer before it became a bigger issue for my body.
The beauty of screening is some of these treatments for early, early stage cancers, especially treatable cancers like colorectal cancer, are very simple procedures. You go home at the end of them. I wish I had that information, but because I had [a] family history, I truly believed that I had something really wrong with me.
The women in my family had a rough go and I felt like, “All right, it’s my turn now,” and that was in the pit of my stomach. So my mom and my grandma did not die in vain.




Every person’s treatment plan is so individualized. But knowing that ahead of time, we went with a treatment plan that made sense for Lynch syndrome, which included a pretty drastic surgery.
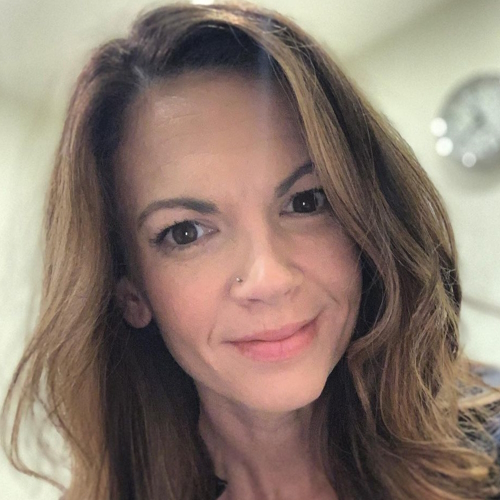
That all happened within a week. Two weeks after getting diagnosed, I went in to get tattooed on my hips and started daily radiation.
We’re well into it and need to act quickly. They moved really fast to get me into treatments right away.
I had just turned 34 in May and this was the end of 2019. I felt really young. I meet people who were in their 20s when they were diagnosed. Sometimes it feels like people didn’t even get a chance to really start their life before they were dealing with this alternative life.
But well beyond Lynch syndrome or colon cancer, understanding your genetic makeup is so pivotal to your health care. We’ve heard about it all over with BRCA and Lynch syndrome is just another one of them.
We just need to get people in tune with their family history. Ask questions. I’m sad a lot of my family members are gone, so I can’t ask them about people in the past.


Ask questions while your parents are here, especially people my age. Get that information down. A lot of people’s families hide colon cancer because it’s not glamorous to talk about. It’s embarrassing. We’re more willing to talk about poop, bathroom habits, and colonoscopies than our grandparents were so make sure you are getting the full story.
That’s really tough but it’s a sad fact. I am not that uncommon anymore and it is showing up more and more.
There [are] all kinds of theories around why and we can theorize and all of that, but I think part of how we handle this is that we start changing how we’re treating our patients, screening them, [and] hearing their symptoms.
We need to stop telling women that they’re anxious, stressed, need more sleep, less coffee, lose weight, or whatever it is.
Women know their bodies. I’m not saying anything that men don’t, but we know our bodies. We know what’s normal for us so speak on it.
If you’re feeling something different inside of you that you’ve never felt before, it doesn’t hurt anyone for you to look into what it could be.

If you’re feeling something different inside of you that you’ve never felt before, it doesn’t hurt anyone for you to look into what it could be.

Treatment of Stage 3B rectal cancer
I tend to think, Gosh, my alarm bells went off just in time to get me in for that colonoscopy so that I could start my process.
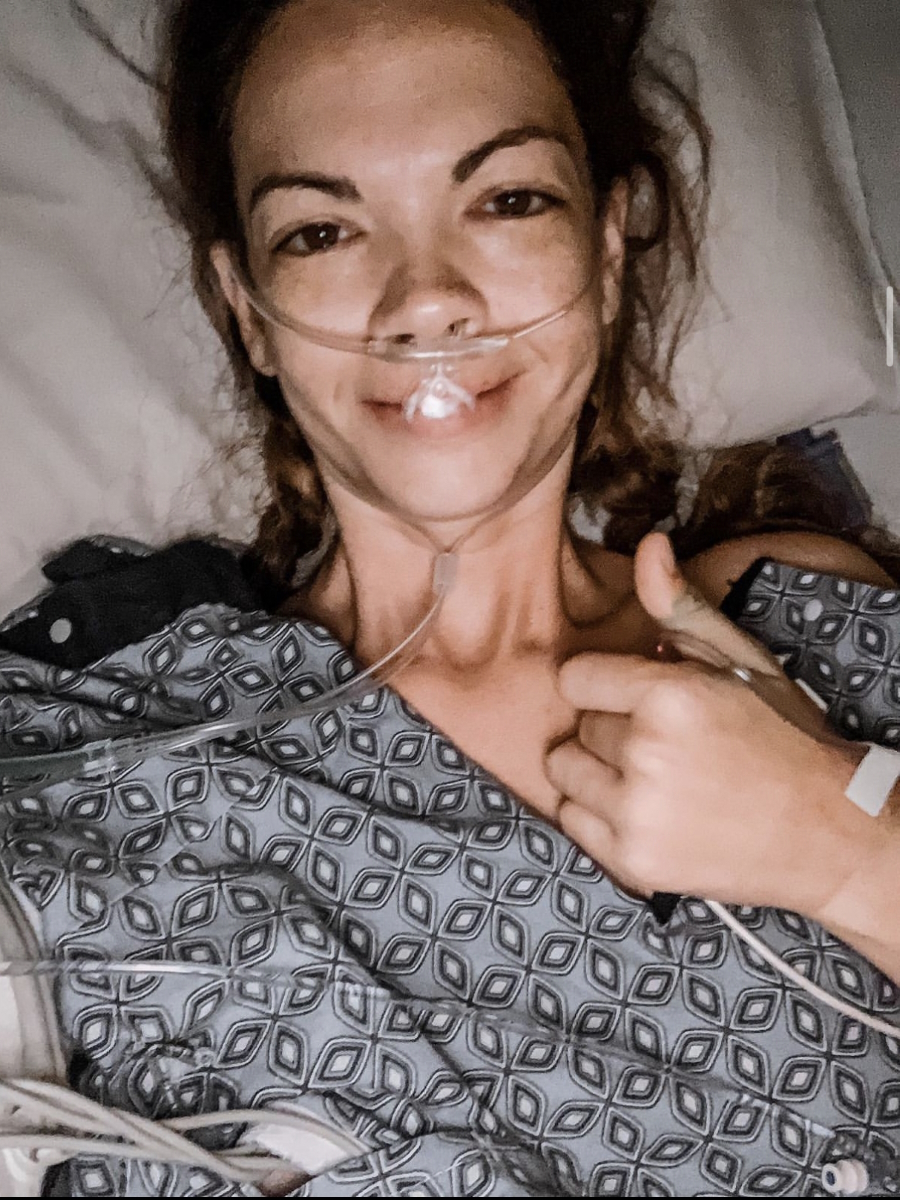
My oncologist referred to it as a marathon so we did it in three legs. The first leg was [the] initial radiation and chemo. Six weeks [and] took some time off.
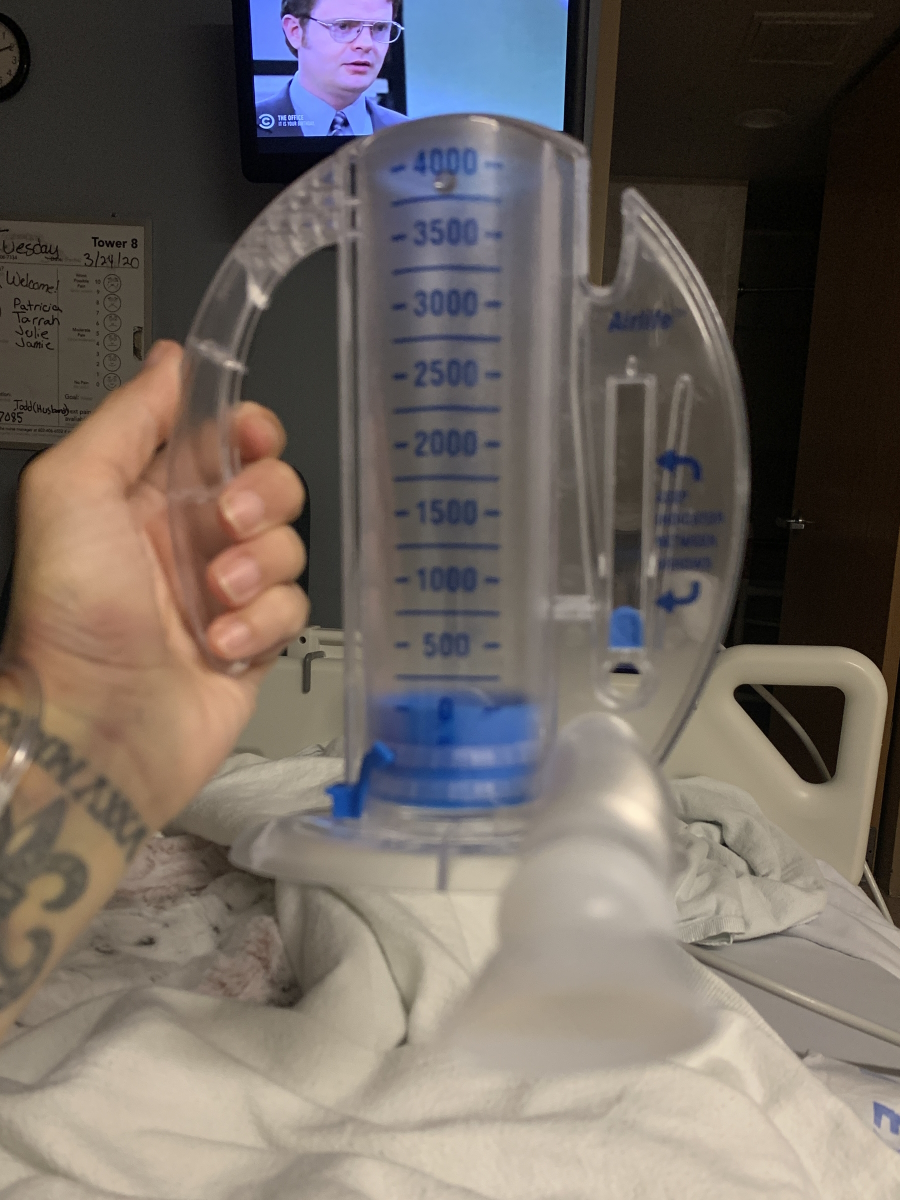
Surgery was the second leg, which is a bear. I had a 9.5-hour surgery. I had what’s called total proctocolectomy with APR reconstruction. They took everything below my small intestine and rebuilt my bottom with muscle and tissue from my abdomen. I was cut open on my abdomen. I had an ileostomy placed [and] live with an ostomy bag now.
At the same time, because of this genetic component [of] Lynch syndrome, I chose to have an elective hysterectomy. Had two kids, really fortunate to get to be a mom. Love my kids and I love children.
The idea of my life going farther, who knows what would have happened? I could not have that risk. I wanted every risk out of me. That was just the way I felt [at] that time. I said, “Take it all, doc, literally everything.”
They removed [part] of my tailbone because of where it was. They were worried about it. I said, “Don’t need it. Don’t need it.” That was tough.
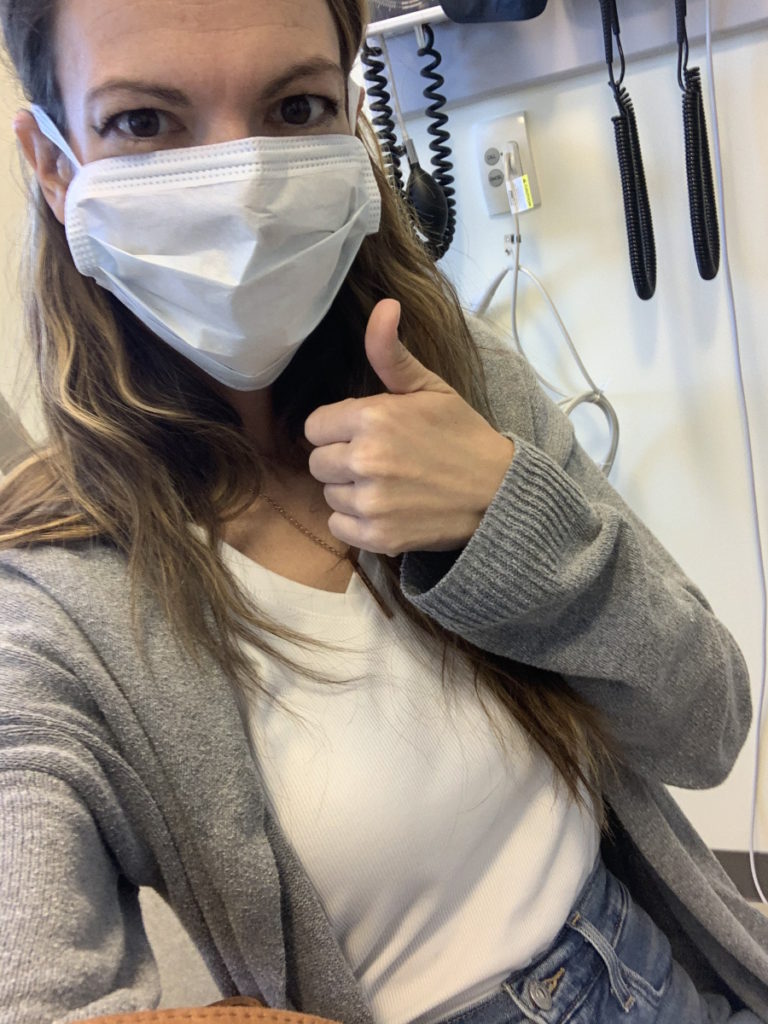
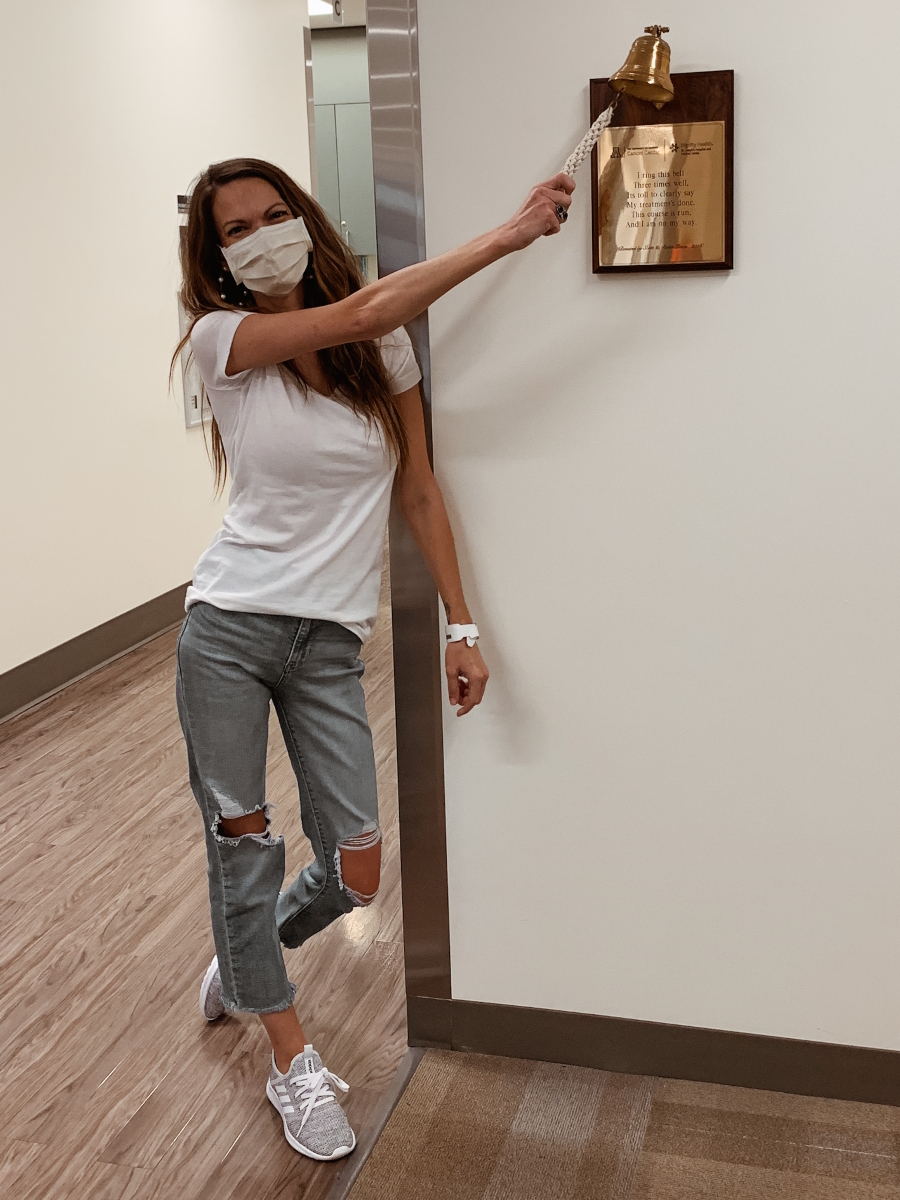
After surgery, I did have a nine-week break then I went in for IV chemo, which was just another part of the marathon. I did six treatments and slowly started to ease back into trying to be a normal person or the person that I used to be.


Follow-up protocol
I’ve learned through that process that there’s no going back to square one or to normal — not with your body, not with your mind, not with everything.
I feel really good, which always kind of worries me a little bit, but I’ve had no evidence of disease since my surgery. I’ve had all clear scans.
I do a tumor residue blood test. Thankfully, all of those have come back clear.
My ostomy works great. I’m learning, growing, and accepting that and just my body overall after everything that’s happened.





Living life with an ostomy bag
[An] ostomy bag is worn on your abdomen. Mine is connected to my small intestine so my small intestine comes out of my abdomen. There’s a tiny little piece of it called a stoma; it’s just another word for opening.
You can have a stoma for your bladder, you can have a stoma for your colon, or you can have a stoma for your small intestine. Mine is [for the] small intestine so it’s referred to as ileostomy.
Different ostomies have different schedules, but I tend to change my bag every third morning. In between that, my bag just stays on. I empty it when it’s full.
My life as far as using the bathroom is altered but the only part that’s really impacted by that is the part that happens when I close the door and no one’s in there with me.
[As] life does, it takes a really long time for it to re-settle down, but it does settle back down.



Living life with Lynch syndrome
Through talking to other people who’ve been through this, I’ve been learning how to live my life with Lynch syndrome. It’s a roller coaster.
I have to be scanned more often than the average cancer survivor. I have a myriad of tests because I have these other risk factors.
I think it’s been going pretty [well]. This is hard for anyone. It’s a total change in your perspective. What your daily life is like changes.
It gives me this new drive. I really want other people to know about this. I want other people to know about going through cancer treatments and what that’s really like so you’re not feeling like every post is only [about] the positive side of it.
When I first started sharing my journey, that was where I was at. I was like, “I’m gonna do this. I’m gonna do it with a smile. I can handle this.” There are parts of it that if I just wouldn’t let myself feel those feelings, I don’t think I would have ever come through them.
My tagline, I think, is just being authentic through everything that’s happened to me. There are parts of me that I feel have grown. I appreciate the person I am now.


There [are] other parts of me that feel like I was damaged during this. My mind is still trying to grasp: how does somebody go through this and keep going?
Part of my success in it is truly just seeing other people do it. Other people have lived this. I’m not the first person. I’m not the first person with an ostomy. We just got to keep changing how we talk about this stuff, making it less taboo.
On the other side of it, after cancer is over or after treatment is over, is the fact that this is [a] different kind of fight. Keep going and use that shifted perspective for positive things.
Shifted perspective brings me down sometimes because I see so many people walking around not taking advantage of their health or taking advantage of [the] knowledge that’s available to them.
I also feel a lot more self-assured. I feel like I can do things that I didn’t think I could do before. I’m more independent as a person. I’m more confident. I’m more willing to look at myself and say, “All right. This is the body you have now.”
One of [the] first things I wrote that really started to change the tide of how I was sharing my story was, “Are you just going to lay here and cry about this all the time or are you going to get up and live?” Got to get up and live.



Let it out, cry it out, and then get up and try to live every day the best that you can. It slowly, slowly, slowly does get better after cancer.
There are other parts that you have to have as a challenge, like going in for more screenings and staying on top of that.
I don’t think I ever heard of an ostomy before. When I was told that I was going to have an ostomy bag, I heard him say bag. I understood what he was saying about removing my colon and it was a little foggy there. But one of the first things I did was I went home and looked online.
I looked up “ostomy” on Instagram and wouldn’t you know it, there [are] a lot of really amazing people that have an ostomy. Not only are they amazing, but they’re smart enough to know that when you go looking for support.
I can go into a support group without anyone even knowing I’m there if I just look up #ostomy online. I can read about people who are doing this every day. I can see women in bathing suits owning this.
I thought, Gosh, I’m not even going in a two-piece bathing suit on my Instagram before my ostomy bag. I’ll never in a million years do what they’re doing. But seeing them made me realize that people are living with these things. It was really powerful for me.
I’m driven in this format of Instagram and social media [because] it’s so casual. People can see it and the more they see ostomy bags, I feel like that taboo comes down. We feel less like we have to hide it away or whatever.


When I heard, ostomy felt to me worse than cancer. I just was like, “You’ve got to be kidding me. My life is going to be over. I’m going to be a monster. I don’t even want this.” I just melted down.
Then I could see people living positively with an ostomy and see women my age having one, too. It feels like you hear that, you start looking at it, all the brochures are old people. It doesn’t feel like a 34-year-old woman should have this.
I slowly got my mind wrapped around it. I tell people now, “At the time, the ostomy to me seemed like it would be the worst part of this whole thing. Now, the easiest part of everything I’ve been through is to live with an ostomy.” That impacts me so much less in my day-to-day life than the mental hardship of going through cancer, cancer treatment, [and] scans post-cancer.
When people come to me and say, “I’m going to have an ostomy bag,” I’m like, “Well, take a deep breath because this is a lot to digest.” It did take me time.
Any strong, brave, out-there person handling their ostomy well had those same feelings, too. They had a moment of, “I don’t know if I can even do this.”
Why I’m out here being a loudmouth is that I live my life with an ostomy. I am a mom with [an] ostomy. I chase my kids the same. I go to concerts. I hang out with my friends. I travel. I go on airplanes. I just did the Disney cruise with my two girls. I do it all with the ostomy. It’s not the way I saw my life when I was a little girl, but it’s not the worst thing.
Just keep going. Like anything we do in life, the more you do it, the less mind-blowing it is.
Go easy on yourself. This is such a hard process.


Words of advice
My message to anyone who is either recently diagnosed or still grappling with their diagnosis is just one thing at a time. One appointment at a time. Get your questions ready [and] have yourself organized, but focus on that one step at a time.
I remember trying to see the other side of surgery in my mind’s eye. When I couldn’t see that, I thought to myself, Am I going to die during surgery? I couldn’t envision what my life was going to be like. I couldn’t see myself having the ostomy and doing it.
But when I woke up [after] the surgery was over, I just did that same thing: one step at a time. I would say, “Oh my gosh, my drain’s full. Okay, drain my drain. Okay, my bag. Now I need to change my bag. Okay, one step at a time.” I remember changing my bag for the first time with shaky hands.
Just keep going. Like anything we do in life, the more you do it, the less mind-blowing it is.
Go easy on yourself. This is such a hard process. I’ve spent — and spend, I will fully admit — a lot of time beating myself up for not handling it better, not being a better advocate, [and] not knowing the things I felt like I should have known before.
I keep coming back time and time again to: we all just do the best we can where we’re at. If I just do one step at a time, one test at a time, one idea at a time, I’ll get there. It’s allowed me to learn a lot more than I ever thought was possible and make a lot of amazing friends.

Cancer is just the worst club to be a part of, but truly, the best people I’ve met are cancer survivors. So if you are there, find a support system. It doesn’t need to be big, it doesn’t need to be grand, and it doesn’t need to be the things that we see on TV, social media, or any of that.
Find a few people who get it. Talk to them. Go easy on yourself and just keep going. This is hard, but it’s doable. Life is worth living.

Cancer is just the worst club to be a part of, but truly, the best people I’ve met are cancer survivors. Find a support system.
Inspired by Amy's story?
Share your story, too!
Rectal Cancer Patient Stories
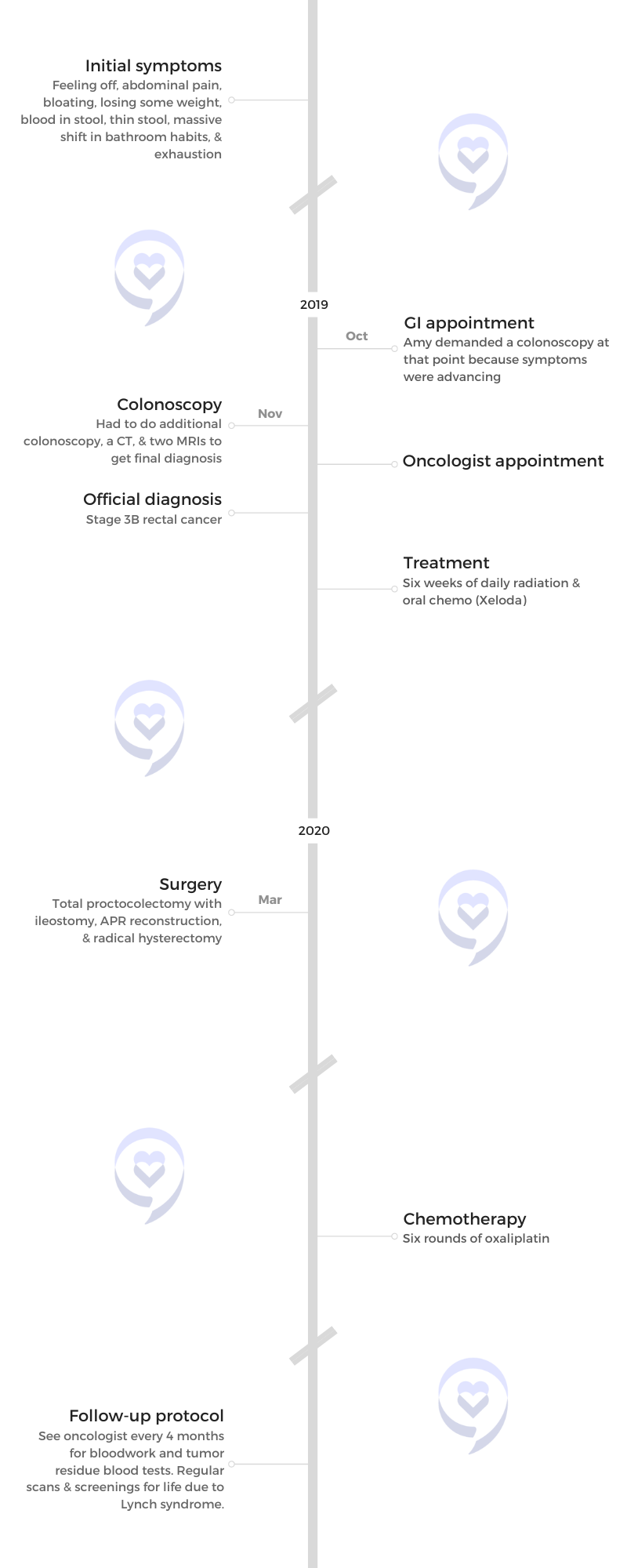
Joanna H., Rectal Cancer, Stage 3
Cancer Details: Rectal adenocarcinoma
1st symptoms: Rectal bleeding, bloating, stomach aches
Treatment: FOLFOX chemo, radiation
Catherine P., Rectal Cancer, Stage 3
Cancer Details: Rectal adenocarcinoma; 98% of rectal and colon cancers are adenocarcinomas
1st Symptoms: Rectal bleeding, constipation, bloating
Treatment: Fertility treatments, chemo, radiation, tumor resection surgery
Jackie S., Rectal Adenocarcinoma, Stage 3B, Lynch Syndrome
Cancer Details: Rectal adenocarcinoma; 98% of rectal and colon cancers are adenocarcinomas
1st Symptoms: Blood in stool, constipation
Treatment: Chemo, radiation, surgery, immunotherapy
Maria A., Rectal Cancer, Stage 3C
Cancer Details: 7cm mass found
1st Symptoms: Fatigue, weight loss, fast heart rate, bladder infection
Treatment: Chemo, radiation, surgery for tumor removal
Justine L., Rectal Cancer, Stage 3B/ 4
Cancer Details: Metastasized to stage 4
1st symptoms: Increasing bowel movements (up to 20/day), some rectal bleeding
Treatment: Chemoradiation (oral pill capecitabine + radiation), colectomy, FOLFOX chemo, SBRT radiation, cancer ablation, Y90 (radioembolization)
Amy H., Rectal Cancer, Stage 3B, Lynch Syndrome
Symptoms: Feeling off, abdominal pain, bloating, weight loss, blood in stool, thin stool, massive shift in bathroom habits, exhaustion
Treatment: Radiation, chemotherapy (Xeloda & oxaliplatin), surgery (total proctocolectomy with ileostomy, APR reconstruction, and radical hysterectomy)
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Ananda P., Rectal Cancer, Stage 3B
Symptoms: Intermittent rectal bleeding
Treatment: Surgery, chemotherapy (FOLFOX)
Jelena T., Colorectal Cancer, Stage 3
Symptoms: Blood in stool, change in gas
Treatment: Chemotherapy, radiation, surgery