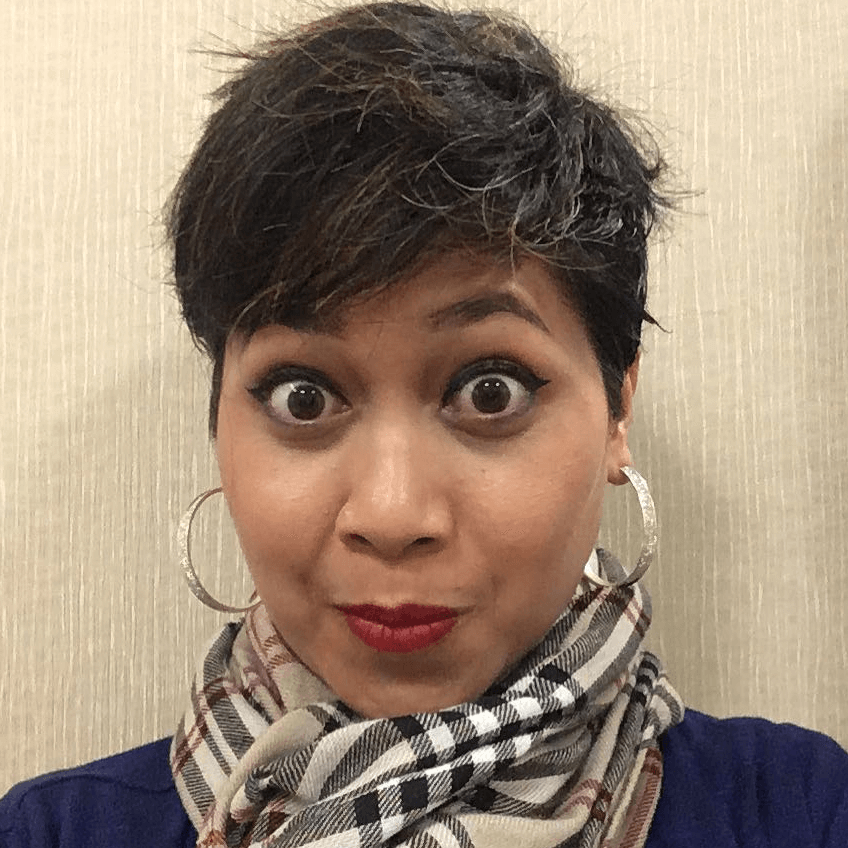
Christine’s Stage 3 Triple-Positive Breast Cancer Story

While in her early 30s, Christine discovered a lump under her left arm and breast area, eventually leading to a stage 3 triple-positive breast cancer diagnosis. Committed to her healing journey, she embarked on a comprehensive treatment plan that included chemotherapy, radiation therapy, and a lumpectomy procedure.
Throughout her breast cancer experience, Christine faced challenging decisions regarding family planning, seeking guidance from her dedicated healthcare team. She drew strength from the support of her loved ones, finding comfort in their presence and encouragement.
Christine faced the difficult decision of preserving her fertility before starting cancer treatment. Learning that chemotherapy could potentially render her infertile, she opted for embryo freezing to safeguard her chances of having children in the future.
Despite the emotional challenges and time constraints, Christine underwent the fertility treatment process and successfully obtained two healthy embryos. She insisted on completing the embryo transfers before starting chemotherapy, balancing the urgency of her cancer treatment. Within a month, she underwent fertility treatments and began chemotherapy, demonstrating remarkable resilience and determination.
Transitioning from fertility preservation to treatment, Christine embarked on a five-month journey to combat her breast cancer. Her treatment plan consisted of AC-T chemotherapy followed by paclitaxel. Initially hesitant about chemotherapy, she underwent a powerful shift in perspective, viewing it as essential for her survival.
In parallel with conventional treatment, Christine also incorporated integrative therapy for additional support. Despite the challenges of hair loss and physical side effects, she showed remarkable resilience, facing the mental and emotional struggle of redefining her identity and embracing her new path toward healing.
In addition to Christine’s narrative, The Patient Story offers a diverse collection of breast cancer stories. These empowering stories provide real-life experiences valuable insights and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Christine E.
- Diagnosis:
- Breast Cancer
- Staging: 3
- Initial Symptoms:
- Lump in her left breast
- Treatment:
- Chemotherapy: AC-T (doxorubicin, cyclophosphamide, paclitaxel)
- Lumpectomy
- Radiation


As difficult and ugly as cancer was, there was still so much beauty. And what that beauty was is that I’ve become 100% present in my life.
Introduction
I’m married to a wonderful man. We don’t have children yet. We live in a small town just outside of our largest city in Saskatchewan. It’s very peaceful here.
We love to walk. We love to get together with friends. We’re really social.
The rest of the time, I’m working. I work at home. I’m currently working with cancer survivors.




Pre-diagnosis
Initial symptoms
I was feeling quite tired, stressed, [and] pale. I was told by quite a few people that I looked quite pale. I just chalked it up to the stress of COVID and being at home. I didn’t really think much of it, to be honest. But I did find my anxiety was rising and didn’t feel very well overall.
When I was laying on my side, I noticed that the tissue in my breast had been pulled straight while the rest of the tissue was falling to the side. That was really [the] only major tip-off that told me that there was something wrong.
You could see a very distinct divot in that spot. Instantly, I felt my breast and realized that there was a very large, very hard, very stationary lump.
I wasn’t doing self-breast checks. Of course, we should be doing them, but I was so young that I thought, There was no reason for me to do this.
Reaction to feeling a lump on the breast
As soon as I felt the lump, I knew that it wasn’t benign. It was too large. It was too hard. It was too stationary. I knew nothing about cancer because of my age. I had never researched it or thought about it, but I just knew that it was cancer.
I’m up all night trying not to worry my husband. I’m staring at the ceiling, crying, and just thinking, What’s my husband’s life going to be like without me? How am I going to say goodbye to my parents? What’s going to happen here? These dark thoughts really intruded my mind for eight hours. I didn’t sleep a wink.
Family history of cancer
There [are] varying degrees of cancer in my family. We had one with stomach cancer. My great-great aunt had breast cancer. Nothing to really tip us off that a 31-year-old should be watching for it.
Appointment with the family doctor
The next morning, I got to work right away. I got a hold of my family doctor and said, “Something isn’t right.” She was able to get me in just a few days later.
She really put my mind at ease. She said, “This probably is just a cyst with your age. It’s probably nothing,” so I felt okay, but she said, “We’ll give you an ultrasound and a mammogram just in case.”


Breast ultrasound and mammogram
Two days later, I was there for the mammogram and ultrasound. The tech started off with the ultrasound and said, “We need to do a mammogram.”
We did the mammogram. The tech came in and in a very somber voice, he said, “This isn’t benign,” and that’s really all he could say.
I remember the whole room zoning in on his mouth. I could see him speaking. Everything went fuzzy. I felt out of [my] body at that moment. I don’t recall what he said after, “It isn’t benign.”
I’m grateful that she decided to go forward with these tests. I really was very fortunate.
Diagnosis
Biopsy
After that, I was sent for a biopsy. I met with the breast health center very quickly. We decided to do a needle biopsy of the axilla as well as the breast. They took samples from each spot.
I met with the surgeon and my husband came with me. However, because of COVID, he wasn’t allowed in so that was heartbreaking. He was sitting in the car.
I’m being told by the surgeon that this biopsy is truly just for protocol purposes, that we can discuss my treatment plan, [and] how long I’ll be in chemo without having any MRIs or biopsies coming back. He knows for certain that this is cancer because of [its] size.
He wasn’t able to give me an exact staging, but he did say, “I do not believe this is an early stage.” I, of course, burst into tears. I’m by myself and I’m told that this isn’t early.
Next, I asked, “How long do I have?” You don’t know how cancer works until you’re faced with it. He stopped and said, “Oh, breast cancer is curable. You’re going to be fine.” I was like, “Oh my God, really? Oh, thank God.” That was really a positive moment.
I was very fortunate. I had a very kind surgeon who really was trying his best for us and for our family.


Getting the test results
The biopsy was taken with an MRI the next day. The MRI took about two weeks to come in and the biopsy took about three/four weeks so you can imagine that period of time was absolute torture.
We’ve got all these blood tests, MRIs, biopsies, waiting, unsureness, and everything. Telling your family that you don’t really know what’s wrong, but something’s bad.
The MRI results came back as a stage 3 breast cancer tumor coming in at nearly 8 cm with at least two lymph nodes involved from what they could see from the scan, [with a] suspicion of four.
Reaction to the test results
I was unaware of what all of that meant. I spent a disgusting amount of time on Google learning what BI-RADS means, what stage 3 means, do people survive that, and all these types of things.
I did feel somewhat left in the dark in that way. The doctors were doing their best. They were moving as quickly as they could, but they were forgetting to tell me what it means.



Fertility preservation before cancer treatment
He mentioned fertility [and] the potential loss of both breasts or the nipple. Those things were really traumatic, but he just kept saying, “Let’s wait and see. Let’s see what we can do for you. We’re going to do our very best.” I was really grateful for that kindness and humanness.
We needed to do treatment. But like many 31-year-olds, I waited and intended to have children at about 31. We were in the beginning stages of trying. My husband and I were unsuccessful. Looking back, thank goodness that we were unsuccessful at that point.
When this came up, he asked, “Do you have [the] intention of having children?” I said, “Yes, I do. We were, in fact, actively trying.” He said, “Okay, chemotherapy often renders you infertile.” That was probably the biggest blow.
My husband and I were meant for children. We put all of our time in our 20s traveling, experiencing, and being with friends. We were finally ready so that was a big blow.
I asked, “What are my options?” He said that a lot of people will do embryo freezing so they’ll take your current eggs, freeze them in the embryonic state, and then should you survive this and should there be no further damage, you should be able to have those babies in the future. That would be the eggs of a 31-year-old.
Because it takes time to be able to try again, we launched straight into that.


Talking about fertility preservation options with your spouse
We were very comfortable [doing] that right away. It was a do-or-die sort of situation. We knew that we had a choice. Do we want to try to have our own babies? The answer was yes.
I was a little leery of the process because there’s estrogen involved. I had estrogen-positive cancer, but nothing was going to stand between me and my future babies. The decision was made and we decided to move forward with it.
Talking with my husband was difficult. We both really wanted to just live normally. We didn’t want to be facing cancer. We wanted to be having babies with our friends and with our families.
My friends and families are living their lives. They’re starting their careers. They’re having babies. And I’m facing this. It did feel unfair to both of us. It was a difficult conversation.
Fertility treatment process
There [are] daily medications, daily needles, lots of blood work, which I’m historically quite scared of because I have really difficult veins so that wasn’t fun, and lots and lots of appointments.
It’s a very heavy-duty time when you’re going through fertility treatments and you add in the stress of [a] stage 3 diagnosis.
It feels like a distant memory thinking back to it now because it was just so full-on for two weeks that I don’t know how I hacked that.
We have extraordinary strength inside of us that gets pulled out in periods like this. I don’t know how I got through, but we did, one step at a time.
We got to the point where I had lots of eggs. They were strained and I assume it’s because of stress. We were able to combine them and successfully come out with two healthy embryos.
One of the advantages of having later-stage cancer is that things happen quickly. A few doctors pushed back on me going through the fertility treatments. They said, “You need to get in now.”
I was so firm that I was going to finish these embryo transfers before I begin so it postponed the whole process by two and a half weeks. A few doctors were quite concerned about that, but the moment I was ready, they were ready and we moved forward.
From the time I was officially diagnosed to the time that I started chemotherapy was approximately a month’s time. That was getting the doctors in place, getting the oncologists in place, doing all of the fertility treatments, and then actually entering into the chemotherapy stage of my treatment.





Treatment
AC-T chemotherapy
I did two months of heavy-duty chemo called AC-T, which is doxorubicin and cyclophosphamide. We did that for four rounds and then we did 12 rounds of paclitaxel every week. Altogether, it was a five-month treatment plan.
Reframing personal view of chemotherapy
It was difficult for me to wrap my brain around [it]. You don’t know until you’re faced with it.
I truly believed if I was diagnosed [with] cancer, I would never touch poison with a 10-foot pole. I would leave, go someplace where I never ate sugar again, live with the monks, and heal myself. That’s what I believed that I would do.
Now you’re facing this diagnosis and the doctor says to you, “If you do what I tell you, you’ll live. But if you don’t, you’ll die.” That was such a paradigm shift for me.
I had a difficult time feeling that this was the best way. I tried my very best to reframe what I had previously said was poison. I tried to reframe it as medicine. I did lots of meditation because that spoke to me and that’s really who I am as a person.
Integrative therapy in conjunction with chemotherapy
I decided to do integrative therapy. I did a naturopathic version of cancer care in conjunction with my cancer therapies because, for me, that was how I could see this as something valuable.
Whether or not it’s for anyone is up to them. But I spoke with my oncology team and we decided that because of the way that I feel as a naturalistic person, this was going to be the best way for my mental health.
The first conversation I had with my naturopath was saying, “I hate chemo. I don’t want anything to do with it. I just want to do naturopathic, but I’m scared.”
Because it was COVID, we had to talk on the phone. It was beautiful because, on the other side of the conversation, she said that their clinic believes in an integrative approach. They believe that you should throw everything at it and they are not against chemotherapy.
Hearing that from a naturalistic doctor was so encouraging. I really think it’s what transferred me from a non-believer of chemotherapy to a believer because someone who I respected said, “Hey, this is a good thing.”


The experience of going through chemotherapy
Undergoing chemo was difficult, but there were breaks and I really appreciated that. You’d go in, have this really difficult experience for days, and then have a little bit of a break and a piece of normalcy. That really helped me a lot.
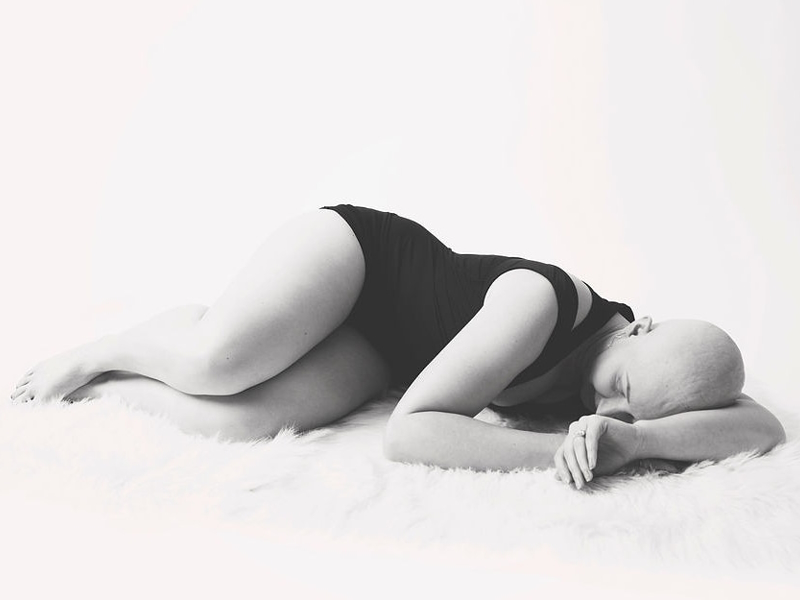
Between chemo, radiation, and surgery, the most difficult part of my journey was chemotherapy. The combination of losing your hair, puffing up because of steroids, [and] gaining weight because of the steroids really robs you of this femininity that we as females attach to.
Side effects of chemotherapy
One of the more difficult parts of my journey was [the] loss of hair, which is crazy but also not crazy because [as] women, we identify with that. I would say it felt lonely, it felt difficult at times, and no one could truly understand how hard this was for me mentally.
They could see that I was physically ill, nauseous, and tired. They could see that I looked pale. No one could truly tell what was more difficult, which was breaking down paradigms — fear of poison, fear of losing my hair, fear of long-term side effects, and who I really was now. That was probably the harder part.

Mental health support
Some really big things for me were my naturopathic appointments. I loved speaking to an oncological naturopath. Those 45-minute sessions where they explained everything back to front really helped me to understand what these were.
The doctors just don’t have time. They’re overrun, especially in Canada. They have 15-minute appointments and they have to get to the next thing.
When I was able to have those 45-minute appointments where they would speak to me about every nook and cranny, that really empowered me. That really made a big, big difference during that process.
Surgery
We finished chemotherapy after five months and then we took a one-month break in preparation for a lumpectomy.
I had a very extraordinary result; that was the term my oncologist used. My tumor shrunk from nearly 8 cm down to 1.2 cm so we were thrilled. We were so pumped.
We were able to make the decision for [a] lumpectomy as opposed to a mastectomy because that is what I wanted.


I had done a lot of research on the differences between mastectomy and lumpectomy, whether or not it is more helpful, and the grief stage that a lot of women go through in the loss of their breasts.
I already lost my hair and body size, and I knew the grief that that was giving me so I opted for a lumpectomy because I wasn’t willing to add that on.
Lumpectomy vs. mastectomy
A mastectomy, whether unilateral or bilateral, is where you remove one or both of your breasts. All of the tissue is removed. Some people get reconstruction. They’ll have expanders. There [are] different ways that people can re-enhance their chest again.
The difficult part is no nipples present unless they opt for that surgery. There can also be a loss of sensation, loss of equilibrium, [and] things like that.
It’s up to the woman what feels right for her. I don’t discourage a mastectomy [from] anybody who decides that that’s what’s right for them. But I opted for the lumpectomy because the lumpectomy was removing just the tumor.
In my case, I was lucky. I didn’t have to nick or disturb the nipples in any way. I was able to just remove the tumor. Because it was only 1.2 cm, I was left with a very small divot, which filled in with fat over [the] years. I have a very large scar, but I still have my breasts exactly as they are.
Preparing for the lumpectomy
Because of my naturopath, I had lots of preparation. I did lots of protein before. There [were] lots of supplements that were meant to help with pain, with not disturbing the cancer cells and having them spread to different parts of the body.
I also did a lot of meditations to help calm my nervous system and to help [me] believe that this was going to be a smooth transition. Of course, I had my fantastic surgeon who just had the most wonderful bedside manner and was so nurturing. I was feeling quite confident going into that surgery.
Survivorship
I do feel that there are times I’m still processing and this is three years from my diagnosis.
I had a difficult time with burns from my radiation [and] scarring from my surgeries, but the really difficult thing was the weight gain. That was so hard. It really felt like salt in the wound.
A lot of trauma around how quick the whole process was. The very definition of trauma is too much, too fast and that’s really what happened. I believe that I sustained post-traumatic stress from all that happened.





It was interesting. While I was in the process, I felt like, “I can do this.” I felt almost invigorated in a lot of ways and very positive.
But afterward, in the survivorship role, I found myself very low, very disconnected from myself and my body. I felt depressed really in a lot of ways. All of that trauma came flooding back. I didn’t expect it, but mentally, the survivorship stage was more difficult than the journey itself mentally.
Words of advice
When you’re choosing your treatment path, it truly is a difficult road. You need to be able to persevere from what you feel is right for you because it’s going to be hard.
If you align your treatment plan in a way that speaks to you, you can always draw from that and say, “I’m doing my best with what I know.” On those difficult moments, you have something to look back on and say, “I was true to me.”
Cancer teaches you a few things. It teaches you how to be self-compassionate because you have to be. It teaches you how to ask and allow people to help you because you have to.
It can be the beginning of something beautiful. I know that, for me, as difficult and ugly as cancer was, there was still so much beauty. And what that beauty was is that I’ve become 100% present in my life.
I don’t fear anything anymore because I know what fear really looks like. I’ve become completely unapologetic about who I am and what I need.
Cancer is not inherently a blessing, but I believe that you can make a choice to make this trauma mean something to you and bring you into the type of person that you’ve always wanted to be.
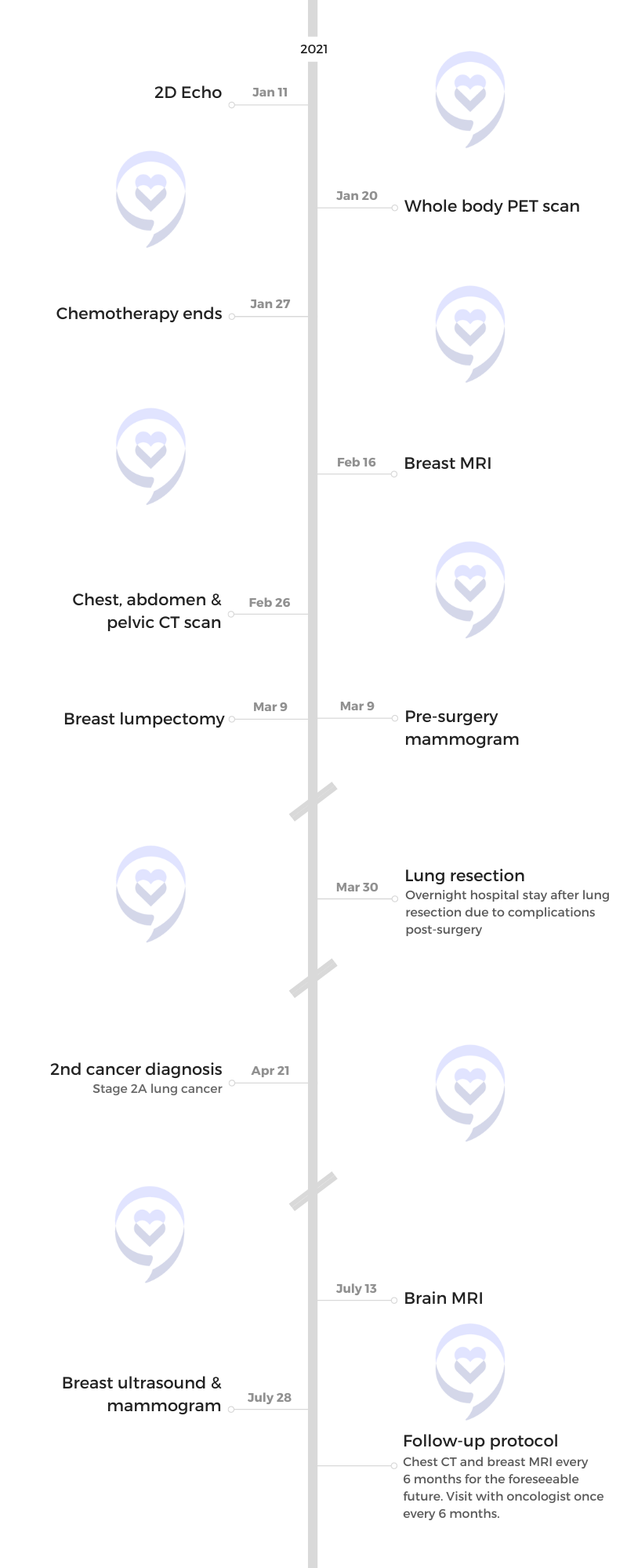
While still very much in her cancer journey, Christine was shocked to get diagnosed with a second cancer. She shares her story of finding out she had stage 2 lung cancer.
Read Christine’s stage 2 lung cancer story here »

Inspired by Christine's story?
Share your story, too!
More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation