Connie’s Relapsed Refractory Multiple Myeloma Story
Connie is a self-described Wyoming cowgirl — not the rough type, but someone who balances it with gentle self-care. She’s happily married to her high school sweetheart, Greg. Together, they’ve raised 3 wonderful children.
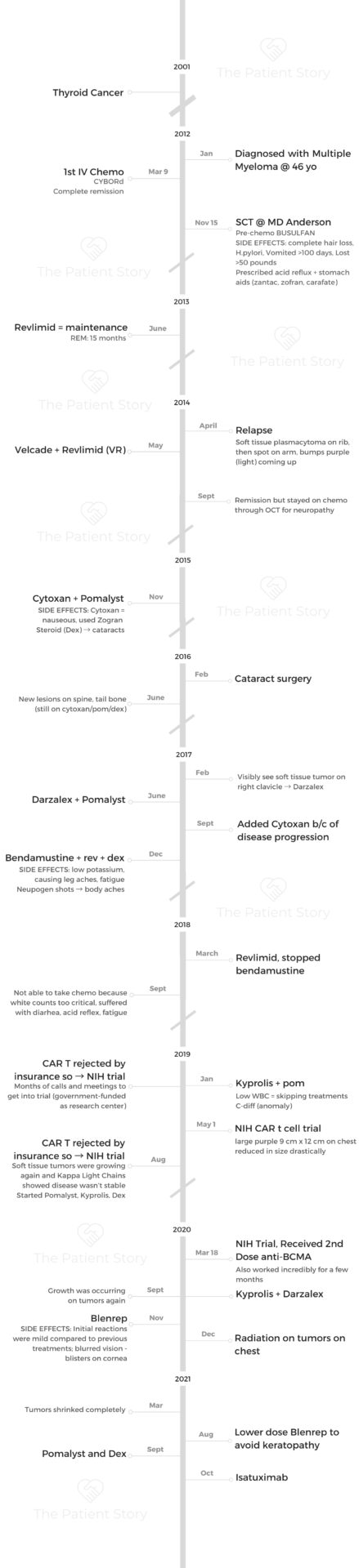
In 2001, she survived thyroid cancer. In 2012, at age 46, she found herself with yet another diagnosis, this time, the rare blood cancer multiple myeloma.
In this video series, Connie shares her story of diagnosis, numerous treatments and clinical trials, relapse, and the side effects she endured. Connie’s journey is not yet over; it is a continuous quest for treatment while living life to the fullest with her family.
Explore her inspiring 3-part story series below. Thank you so much for sharing, Connie!

- Name: Connie H.
- Diagnosis (DX)
- Multiple Myeloma (Relapsed/Refractory)
- 1st Diagnosis:
- Age at DX: 46 years old
- Symptoms
- Chronic pain on ribs, shoulder and hips
- Cough, bronchitis
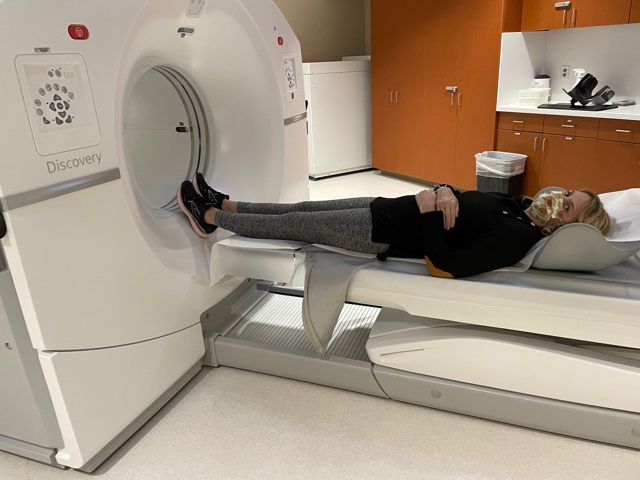
- Tests for DX: CT scan, Bone marrow biopsy
- Treatment:
- Stem Cell
- IV Chemo (CyBorD)
- Busulfan
- Velcade + Revlimid (VR)
- Cytoxan + Pomalyst
- Darzalex
- Bendamustine
- Kyprolis
- CAR T cell therapy
- Blenrep
- Isatuximab
- VIDEO: Multiple Myeloma Diagnosis
- VIDEO: Multiple Myeloma Relapse & Clinical Trials
- VIDEO: Living with Multiple Myeloma
- More Relapsed/Refractory Multiple Myeloma Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
VIDEO: Multiple Myeloma Diagnosis

About me
I sometimes think I have the identity in our small community as the lady with cancer, and I don’t like that. I’ve been married for 36 years to my high school sweetheart, Greg, and we have wonderful, amazing children. I’m proud to say that they’re all doing very successful careers right now.
I was raised on a ranch in Wyoming. I’m a Wyoming cowgirl, and yet I balance that with liking to be pampered a little bit with a pedicure and things like that. I’m not a totally rough-type cowgirl from a big family.
I was in pretty bad shape, but I had made excuses for it.
My first multiple myeloma symptoms
I had a lot of chronic pain, and I guess I didn’t think that anything serious was going on. one day maybe my right side would hurt, and then the next day the left side, and then maybe I would have a headache when I walked a lot.
I would get a pain in my shoulder, in the back. My chest was tender, and I had a cough. I actually went to the ER once with pain in my chest. I had slight bronchitis, so I ended up getting treated for that.
I had slipped on the ice, and so my hip hurting had been attributed to that. By the time I actually went to the doctor, I had 4 broken rib, a small hole in my sternum and lesions in my skull and spine.
I was in pretty bad shape, but I had made excuses for it. I just thought that I was a busy mom and that’s why I was so tired. I was actually working at a hospital, so once I did go to see a doctor, she actually said, “I’ve seen you limping down the halls.” She sent me immediately for a CT scan.
»MORE: What is multiple myeloma?
Multiple myeloma diagnosis
It did take a while because I was at a small community hospital, and I had thyroid cancer in 2001. Originally, they thought it was metastatic from thyroid cancer, which would have been actually worse. In some ways, I got the better of two evils when we found out it was multiple myeloma.
I went to a little larger facility and had a bone marrow biopsy. That’s when they determined that it was multiple myeloma.
It had been well over 11 years since my thyroid cancer, and I had really put cancer away on the top shelf. Maybe I should have thought all these aches and pains would have been cancer, but I never thought about cancer.
Thyroid cancer is so curable that I just was only having yearly checkups. It was just a big shock to find out that it was multiple myeloma. I was only 46 years old then.
Living life while undergoing treatment
I don’t think it was always a cloud. Cancers truly do make you think about how you should treasure every day. For the most part, I was trying to do that.
You don’t want to be down worrying all the time. Yet, any time a scan came up or whatever, then you got nervous and thought about it more.
First thing to do when you get a cancer diagnosis
Accept the support that people do want to help. Sometimes we just want to handle it all ourselves or try to be strong. I’m a people person, so I knew that I needed to be surrounded by friends and family. That really helped me get through.
I was always really honest with my kids. They weren’t little, though. My daughter was a freshman in high school, my oldest son graduated from law school, and my middle son was in college. They were old enough to understand, so I didn’t hold anything back. I think that that’s good because they can’t help you if they don’t know what’s truly going on.
Deciding on the course of next treatment
I always knew that Dr. Weber was going to do what was the very best for me — and the cutting edge, the newest treatment available that fit my type of multiple myeloma.
She would discuss that with extramedullary multiple myeloma that had gone to the tissue, you might have better results, for instance, with Revlimid than something else. We usually treated it pretty aggressively, though, but still keeping in mind that it was important to not damage your kidneys and monitor the white counts. I did have a lot of treatment choices, but she picked because she’s the expert.
Revlimid was almost the only treatment when I started. Besides it being really a harsh chemo, it just seemed like with every BiTE (bispecific T-cell engager), every 6 months, something new is coming out, and I was fortunate to get to try the new combinations.
They definitely took into account that I was young. But one thing that I had to get used to was that it was necessary for me to take pain meds on a regular basis. I didn’t really want to, but that was going to balance out and allow me to do what I needed to do and not live in pain.
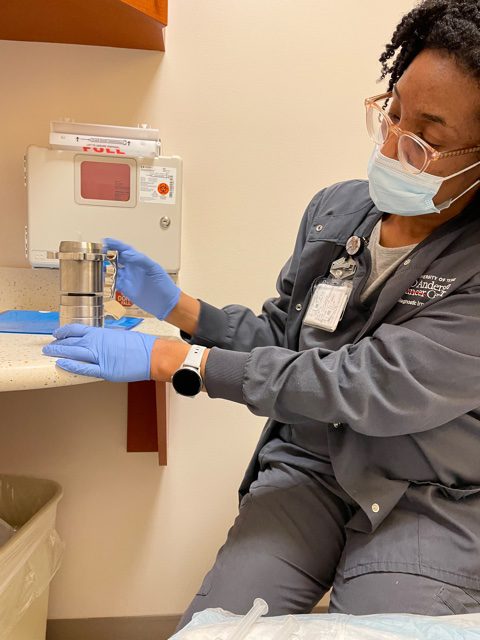
What to expect with the stem cell transplant
A stem cell transplant is pretty hard to go through, but I just sort of looked at it as the normal suggestion, the standard of care pretty much all multiple myeloma patients are doing.
If someone else can do it, I can do it. I also knew that a lot of people were older than me going through multiple myeloma.
I always want to know everything about it. I would say ask your doctor lots of questions.
I could have had the stem cell in a smaller facility, but when we asked how many stem cells they did a year, they said about a dozen. Instead, I chose to go to MD Anderson that does 6 or 7 a day. I wanted where it was a common thing and where the nurses only worked in stem cells so that I would have really very top level of care. That was important to me.
I don’t really remember exactly what the schedule was for the pre-chemo, but I know that it was a really tough one. The only time I lost my hair was from that chemo treatment.
It definitely makes you very sick, and the goal is to get your white count down to zero so that then they can give you back your stem cells that hopefully aren’t corrupted with cancer anymore. You really have to be quite sick for them to bring you back and start getting healthy again.
I was in the hospital for almost a month. I got to be home for Christmas; we flew home on December 18th. I know that the doctors were a little bit hesitant to let me go, but they knew that it was going to do me really good to be home for Christmas. I spent Thanksgiving in the hospital and my husband Greg was with me, but our 3 kids were with their grandparents.

It was just really hard to even have a holiday away from my family.
»MORE: Read more about stem cell transplants
Chemo side effects
I had extreme nausea. I had nausea for a hundred days. I associated food with evil because almost every time I tried to eat something, I threw up. I was existing on a few bites of yogurt a day, maybe a piece of apple, and I would try to drink water.
I ended up losing about 50 pounds with the stem cell and I continued to lose weight.
It was really fortunate that my family provider found out that I had H. Pylori because I started to get well soon after that. It was causing a lot of acid reflux and vomiting, not the stem cell transplant side effects.
»MORE: Read other cancer patient experiences with chemotherapy
Ask how sick you’re supposed to be. I think it’s always a good idea to share with your oncologist just how sick you really are specifically and whether you’re not eating.

They need to know that, because maybe they haven’t really noticed. Unless you tell them, they can’t notice that you haven’t really eaten at all.
The main oncologist that I’ve had out of MD Anderson was always very honest with me, and I appreciated that. She said more than likely it will come back, but using the maintenance therapy will keep it away longer.
The Revlimid wasn’t very hard on me at that time, and I had a very good quality of life then. I still had a lot of pain because of the damage that was done to the ribs and in the back from the earlier myeloma. I still had some of those lesions and a lot of bone pain, and so I wasn’t able to work or do some of those really normal activities.
I could enjoy going to my daughter’s sporting events and socialize with my kids, go to football games, or things like that. I just wasn’t able to go run or something.
It was a lot of pain. Since your feet are a little bit numb, then you might not feel even when you bumped it. That’s why people get infections in their toes and stuff.
It is a huge problem with cancer, but you can work around it. Actually, I’ve been successful with gabapentin to treat neuropathy.
We were really cautious with things about neuropathy, especially during the beginning. I didn’t even realize that that wasn’t going to go away and become a really big problem.
I remember the first time I felt some neuropathy. It was from Velcade. They pulled the chemo from me because not being able to walk — that feeling in your feet is just supercritical. I have neuropathy now, but it’s never gotten as advanced as a lot of people I know. I have a family member that suffers a lot from neuropathy.
Again, telling your doctor if you’re having even small symptoms of neuropathy is important.
Revlimid side effects
The Patient Story: You were in remission, but then there was the neuropathy issue. The next year, November 2015, you’re on Cytoxan and Pomalyst. Your first time with Pomalyst, you had nausea. You had Zofran to help combat that, right?
I do remember my doctor telling me to think of Pomalyst like a cousin to Revlimid. That was actually positive to hear because I hadn’t had a lot of side effects with Revlimid. It was nice that it was a pill because that means one less trip and sitting in a hospital getting IV.
When you talk about quality of life, I think it’s awesome. If you can get your therapy in a pill form and just take it at home and that your weeks aren’t lined out like chemo Monday, chemo Tuesday, that’s better. Just taking a pill every day is easier, if possible.
Dexamethasone side effects
At first, when I just started seeing things more gray and shadowy and a little bit hard to see, like at night driving, I just thought, “What if the cancer’s gone into my eyes or brain?”
I have to admit, that point caused a little panic. I was so relieved when I found out it was cataracts and could just easily be fixed. I had double cataract surgery, and it was a breeze.
VIDEO: Multiple Myeloma Relapse & Clinical Trials
Symptoms of 1st Relapse
When they started to grow a little more, I had one little spot on my side, on the rib area. It was not even as big as a quarter, and it wasn’t really purple at that point. It didn’t really look the way multiple myeloma often looks, where it’s more purply. That came later.
It was sort of slow growing, too, but it did start to grow. Then I got one on my arm, and it was finally biopsied. Then they knew that it was cancer. It eventually showed up in a PET scan, too, and it had other spots.
Another relapse
It started out as the size of a pea. It was a little tumor on my clavicle. Actually, it wasn’t picked up originally on the PET scan either, but that’s where it was both a blessing and a curse because I can actually see the tumor and see how I’m doing and and know to get treatment early because it really was my best diagnostic tool.
With my kappa light chain multiple myeloma, it doesn’t always show up in the blood test — at least not until it’s a little more developed. Yet, we could see this growing. That new symptom meant it’s time for a different treatment.
Does it get easier or harder?
It gets harder every time. I wish I could say that it got easier, but even though you know it’s incurable, you just get so hopeful.
Maybe you can get used to a chemo and the routine. I’ll take an anti-nausea pill once a day, and that works. I can take this rest reflex and have my regimen down.
You know what to expect. But just about the time that you’re into a routine, boom, it changes and you’ve got to change therapies as well.

Just being told again that it’s been in a partial remission, and then it would come back in my spine or something. I would think, “Here we go again.” I’m back to being concerned that it’s going to be aggressive or if that other treatment is going to work. It’s just mentally challenging. It’s like a roller coaster.
I always feel better once I get a plan in action. Even once I know the treatment and I start doing it, then I’m okay again. I have to have a plan out there. It’s really like waiting in limbo because lots of times you’re waiting on the doctors to decide what treatment is best for you or for insurance approval or just rescheduling.
Coordinating care with MD Anderson with an oncologist that was closer to me usually took an extra couple of weeks, even just for the doctors to communicate and decide.
New treatments
What Darzalex and Pomalyst were like
I never thought I would forget, but honestly, lots of times now, all the chemos have blurred together in their side effects.
I didn’t have a lot of trouble with Darzalex until it was combined with a different treatment later, as I recall. But the Darzalex with Pomalyst wasn’t as bad.
Cytoxan is one of the worst, but the side effects are treatable with Zofran and stuff. I’m one of those people that will go ahead and take the anti-nausea meds for the acid reflux and the different things if they’ll help. I’m not one to say, “Oh, I don’t really need it. I can tough it out.” Cancer’s tough enough.
With everything to go through, I say accept the medications and use them the way they’re designed to be used. With pain, too. You don’t have to live in a lot of pain if you just monitor it correctly.
I was neutropenic a lot, so I would have Neupogen shots quite regularly. Being neutropenic makes you really tired and ache all over, especially your legs, plus your immune system is jeopardized. It was scary to be going out in public.
That’s where you had to balance whether you should go to a social event with all your friends or you should stay home. It’s like the things people are doing on a regular basis with COVID, but I was doing that years ago.
You have to make those tough decisions of whether to go out and about and enjoy something and wear a mask, or maybe best just to stay home. I did miss some important events because of not wanting to be around crowds during flu seasons.

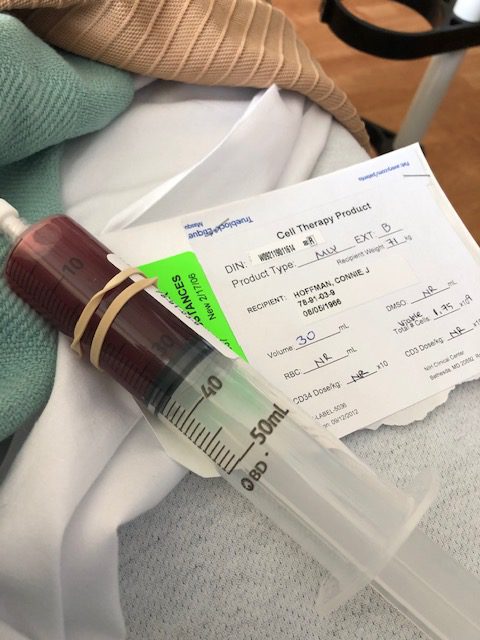
CAR T-cell therapy trial
Both clinical trials showed some success. It was just not as long as I would have hoped.
When you put into perspective that you’re there at the NIH for a few weeks — plus for a clinical trial like that, you needed to go monthly for the first 6 months — traveling from Wyoming to Maryland, it is quite a feat in itself. I did get months of not having to take another chemo, and they have given my body, my kidneys, a little bit of time to heal.
My main problem was being neutropenic. My white counts were low with the CAR T-cells, but I was running out of options. What the CAR T-cells really did was bought me time until research could come up with another new therapy.
In 2019, I had the CAR T-cell in May, and the treatment I ended up going on that fall had just been FDA-approved in August. It wasn’t available for me when I needed something back in March and April. The CAR T-cells just didn’t work as well with me as they did with a lot of the other patients, as far as long term. They worked very quickly, and the pictures are proof of that.
It was incredible to watch a huge tumor just shrink away like daily. You’d look in the mirror and go, “Wow, it’s shrunk again.”
That’s the blessing and the curse. I had this pretty ugly-looking real skin tumor. It’s visual, but at the same time, then you get to see the good when that cancer goes away.
What the CAR T-cells really did was bought me time until research could come up with another new therapy.

Second NIH Trial
I was so surprised when I got a call from National Institutes of Health (NIH) that they were going to do the same CAR T-cell therapy again and that I fit the requirements. The first trial was trying to find which dose and which amount of cells was the optimal amount and not to give you too much or too little.
When they thought they had found the magic amount, that’s what they wanted to do in the second CAR T-cell. It was still the same type of trial, just a much higher dose than I got the first time.
I was the first person ever to do the second dose of this beast anti-BCMA. It was a little bit scary being the first. At the same time, I had already had one CAR T-cell, and it was going to be basically the same, just with a different dose. That was maybe going to be a little bit harder with side effects, but they weren’t even sure if that was the case.
I slipped in under the radar. I had it in March 18th, just when COVID hit. I arrived at the end of April at NIH, and they quit taking patients. I was one of the last patients, probably because I came from Wyoming. If I hadn’t come from so far, they might have sent me home. At least I made it in to be able to do that.
Infusion reactions
I think there were a lot of factors there. I honestly was just a little bit down then, too, and just didn’t have that motivation to take on being sick. I needed a little bit of a break.
Things did work out, though. I ended up finding something that worked better: the Blenrep. Even when I said enough on the other one, I knew that the Blenrep was on the horizon. We were just waiting for it. I’d heard really good things about the Blenrep, except for the visual toxicity.

Blenrep side effects
It was pretty seamless. There was, of course, some fatigue and everything. That was around the holidays then, so I was tired anyway. Oftentimes, you have to counter whatever’s going on in life with that.
I did radiation right after the Blenrep. It was the first time they decided to do that, mainly for palliative care because of the pain. The tumors were so large to do the radiation, but the radiation ended up as a bigger success than they thought it would be.
They didn’t really know whether it was the combination of the radiation and the Blenrep, because then I ended up going almost 7 or 8 months without needing any other treatment.
»MORE: Read other patient experiences with radiation therapy
Stopping Blenrep
I only had one treatment, and then my eyes got so bad that I couldn’t have another treatment. Then there was lots of follow-up with having the eyes checked. I actually had blisters on my cornea. It caused really bad blurred vision.
At first, it was with what we’ve all become as users of phones and computers. I thought that won’t be that bad if it’s not total vision loss. When you can’t read a text or anything, I became a little more techie as far as being able to learn from audio and even have the phone read audio. It taught me a few things, but you couldn’t do things like Facebook and read emails.
That part only lasted a few weeks. Then the part where seeing in a distance like driving was harder for longer. I’m experiencing that again now because I had Blenrep in August, and now I’m experiencing a little bit of blurred vision at a distance again.
Once you’ve had a reaction, they will let you have it a second time once you’re recovered. That’s what I finally got to do a second time in August.
But I had a reaction again. Now, even though Blenrep did work to treat the multiple myeloma, I can’t have it anymore.
That’s the way it should be: to be cautious and not let someone lose their vision over it.
What’s next?
I’m also waiting for another new novel chemo. I was waiting for it to get approved. It’s that kind of run-around between the health care facility and the insurance.
I find it so important because this time I delayed a little bit. That getting on the phone and staying on hold for an hour or however long it takes to get hold of the insurance company and say, “I thought that this would be approved.”
I actually did get approval for isatuximab, but I haven’t had a dose yet.
Waiting for the new clinical trial
I’ve been more tired than normal. I think I realized that with the Pomalyst I had forgotten, but it reminded me that it causes back pain.
I’ve definitely had some more back pain and a little bit of nausea, but because of the steroids, I’m eating better, which I probably needed to. I just hadn’t been that interested in food, but the steroids have made me crave food again. I actually think I probably needed to eat better, so that’s a positive.
I still have a lot of bone pain, but overall, I’m doing okay. It’s amazing, because 9 years out I’m still better than when I first started out.
I just had a PET scan yesterday, so I won’t know until tomorrow what the results are. My PET scan before this didn’t show a lot of disease except for in the skin on my chest area, and there weren’t any new bone lesions.
The change that they measure had gone up significantly. They were way out of line, so there’s definitely myeloma showing in the blood in a significant amount. Probably not doing that well. I definitely needed to get going on treatment.
VIDEO: Living with Multiple Myeloma

Quality of Life
How have you been able to manage the emotions?
Faith is very important to me, for sure. There’s no way I could get through this without knowing that God definitely does have a plan. I have been able to see blessings through this.
You do live your life a little bit differently and make sure that you focus on having some really fun times when you can.
It is difficult for sure, though, to keep going through and finding the new treatments. Then you have to realize there’s only one alternative, and that’s there wasn’t a new treatment or that you get worse and couldn’t have a treatment.
Multiple myeloma research is amazing right now. The fact that there have been this many treatments that I could try is actually a blessing. But it is difficult to always be switching.
It is difficult for sure, though, to keep going through and finding the new treatments. But then you have to realize there’s only one alternative, and that’s there wasn’t a new treatment or that you get worse and couldn’t have a treatment.
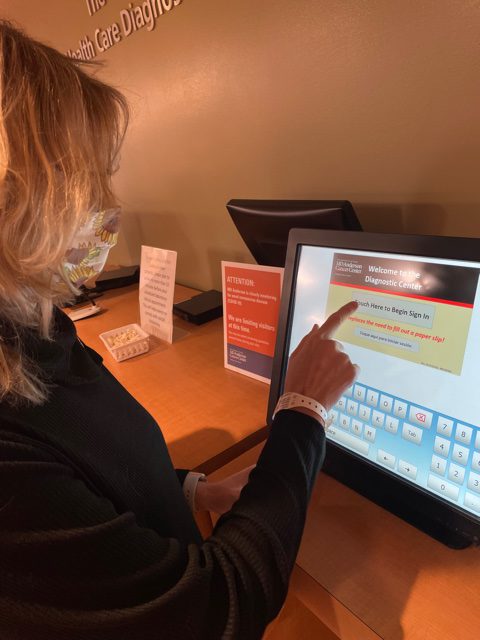
Traveling to get treated
It meant that I really needed to accept help from people that were willing to drive me — lots of family and friends — because lots of times after the chemo, I didn’t feel well enough to drive.
My blood pressure would drop or something, so it did mean getting rides. Those chemos were twice a week or every week with a week off. That was a lot of driving.
I have been able to have some treatments at the hospital right in our town, but they have just a very small chemotherapy setup. It usually depends on whether it’s a therapy that my oncologists think I can have in a small town and be able to handle if there’s a side effect. For the new one that I’ll be having, they want me to do it in Billings, Montana, which is 180 miles away.

Tips for dealing with your insurance
I usually try to get the phone number and the lady’s name. If you can get their name and if they’ll give you a direct line, then you can tell the hospital personnel that’s doing the finance research where or who to call. I try to usually make their job easier by hooking them up together.
Not always will they give their direct line, but still, work until you get to the person that’s really in charge of it.
Last time, I found out that interns had been contacting the nurse, the actual office, and they weren’t contacting the correct lady.
You just have to try to be nice, even though it’s really frustrating sometimes. It’s usually not anyone’s fault. It’s just there’s a lot of miscommunication in health care.
We talked about electronic medical records and all these things, but we are so far away from having any type of really good system where it’s all coordinated together.
It’s especially difficult for someone like me because I’m dealing with a hospital right in my own town to have labs, then a hospital where I’ll have my chemo and test sometimes, then traveling to MD Anderson or NIH.
Sometimes it’s considered locally even if it’s 180 miles away. I’d be dealing with three facilities and having to coordinate the communication between them.
What can you say to those beginning their myeloma experience?
Take one day at a time.
I know that’s sort of simplistic, but it is true because if you start focusing too much on the unknown, it won’t work. You have to focus on what you’ve got to do just that day, what fun you can have, and how you can make that quality day.
It’s better not to look too long-term, because with multiple myeloma, it’s probably going to change. You’re probably not going to be able to make a plan out there. Any minute, something can happen, and then you need a different therapy.
Doing those follow-ups when they’re scheduled is really important. Do things in a timely manner because they can help you catch it right off.
Take one day at a time. If you start focusing too much on the unknown, it won’t work. You have to focus on what you’ve got to do just that day, what fun you can have, and how you can make that quality day.
What’s your advice for people looking to join a clinical trial?
Talking to your local oncologist might help. They might not. They might know.
The website that I went to was ClinicalTrials.gov. You can pull up any trial in the whole U.S., or you can just pick an area or pick your cancer and narrow it down.
Then just be brave enough to call the numbers or submit something online. There is, of course, a lot of background information that they’re going to want, and you will have to send them labs and different scans. Really, your oncologist will end up sending the records, too, so it’s not all on you.
When I went through a trial, there was a patient care coordinator assigned to me, and she called me almost daily to update me. It was a lot, but you really have a whole team that’s looking out for you. It is so different than when you’re going to a regular facility for just chemotherapy, because you’re part of a trial.
It’s a big deal. There’s 6 or 8 people that are assigned to you and a team of doctors that care what happens every day.
Jump in with both feet.
For me, the trials bought me time and gave my body just a little bit of a break from the routine of chemo.
Even mentally, too, it gave me that new hope. I got to see those tumors be zapped away, even though they did come back. The visual of watching them go away and knowing that was going to help.
Shortly after, I did the second CAR T-cell trial, not the BCMA but some form of CAR-T approved by the FDA for multiple myeloma.
I hope that somewhere down the line, someone else will be able to have a CAR T-cell and they’re not going to have to jump through all the hoops. It’s an easier process than a stem cell transplant, for instance.
Jump in with both feet. For me, the trials bought me time and gave my body just a little bit of a break from the routine of chemo.
Getting support from clinical trials
It’s government funded through the National Institute of Health, so all of the health care is covered by the government, all of your scans and all of that.
None of that is out of pocket because you’re saying that you’re going to be a guinea pig, in essence. Then it also depends on your income and different things.
For example, my flight was covered, but I needed a caregiver and my caregivers’ weren’t. There was even a stipend for hotels and food. Then it varied from one trial to the other. You had monthly follow-ups for the first 6 months that you had to go and be there for almost a week.
Every month, I have to have a bone marrow biopsy, for instance, and that’s a lot to go through. Their tests were extensive. It was all covered for scientific research, so it was rather interesting, too.
»MORE: Learn more about the process of clinical trials from one program director
Advocating for yourself as a patient
I think it’s really important to be willing to call up and hopefully know the nurse’s name or the main contact in your oncologist’s office and be able to call them when you’re not feeling well, because maybe that stomach ache is something more. Maybe that leg pain is due to low potassium.
Sometimes, when you go ahead and make that call, they’ll order labs and find out what’s going on.
Everyone has some personal thing that they’re struggling with. I always struggled with the low white counts. The labs would never show absolute neutrophil count, but I learned how to calculate it myself with what was given. Then I could say my absolute neutrophil count is low. I got to the point where I gave myself shots of the meds.
The patient advocacy comes in all forms, and it really is the communication with your doctor, the nurses, everyone along the way.
Even though using the patient portal, most facilities now let you send them a quick email through the patient portal and look at your labs.
I think it’s important to know what’s in your charts better than they know it. Know the names of your chemos, know the prescriptions, what you’re on them for, not just the names of them.
Patient advocacy comes in all forms, and it really is the communication with your doctor, the nurses, everyone along the way.
For other people going through this, they’ve made leaps and bounds with multiple myeloma with research in it.
It is not curable, but I’m sure you can still live a good life.

Inspired by Connie's story?
Share your story, too!
More Relapsed/Refractory Multiple Myeloma Stories
Theresa T.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: IgG kappa Light Chain
Initial Symptom: Extreme pain in right hip
Treatment: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
Donna K.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: None, found by blood tests
Treatment: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T, selinexor-carfilzomib
Connie H.
Diagnosis: Multiple myeloma, relapsed refractory
1st Symptoms: Chronic bone pain
Treatment: IV Chemotherapy, CAR T cell therapy
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
Beth A.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: Non-secretory (1-5% of myelomas)
1st Symptoms: Extreme pain between shoulder blades, sternum, head, burning sensation
1st Line Treatment: VAD chemo, radiation, stem cell transplant
RR Treatment: 8 chemo regimens, successful combo→selinexor+bortezomib+dexamethasone
Scott C.
Diagnosis: Multiple myeloma, relapsed/refractorySubtype: IgG lambda (majorityof myelomas)
1st Symptoms: Pain in hips and ribs, night sweats, weight loss, nausea
Treatment: Clinical trial, chemo, kyphoplasty, stem cell transplant






One reply on “Connie’s Relapsed Refractory Multiple Myeloma Story”
Wow what an amazing lady. She must have such a zest to live. I admire her. She is an example to those who want to give up . Loved her story. She will be in my prayers Michelle