Mantle Cell Lymphoma Treatment
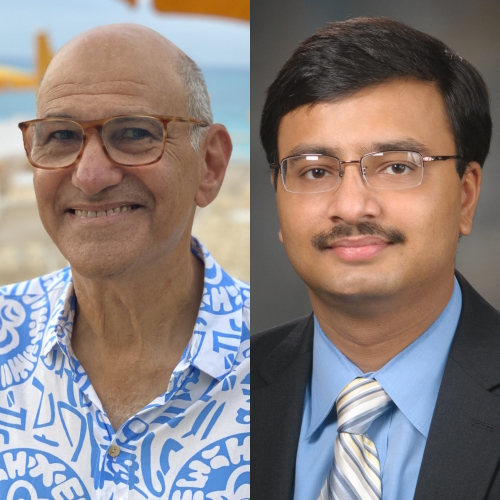
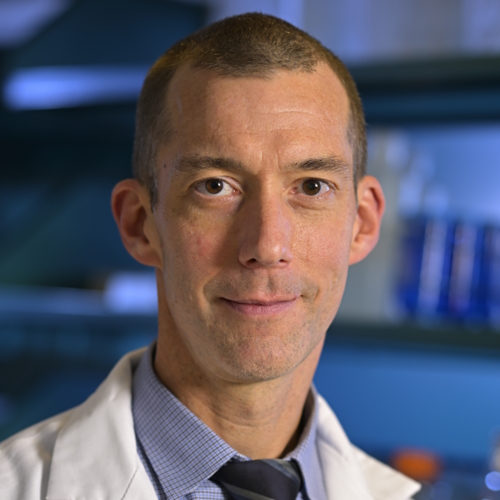
David Miklos, MD, Ph.D
What’s the latest in mantle cell lymphoma transplant? Hear from David Miklos, MD, Ph.D, an experienced and passionate specialist in blood and marrow transplants, as well as immunotherapy research.
As Chief of BMT & Cell Therapy, and Clinical Director of the Cancer Cell Therapy program at Stanford University Medical Center, Dr. Miklos spends his time not only seeing patients but also focusing on the latest science in cancer therapies.
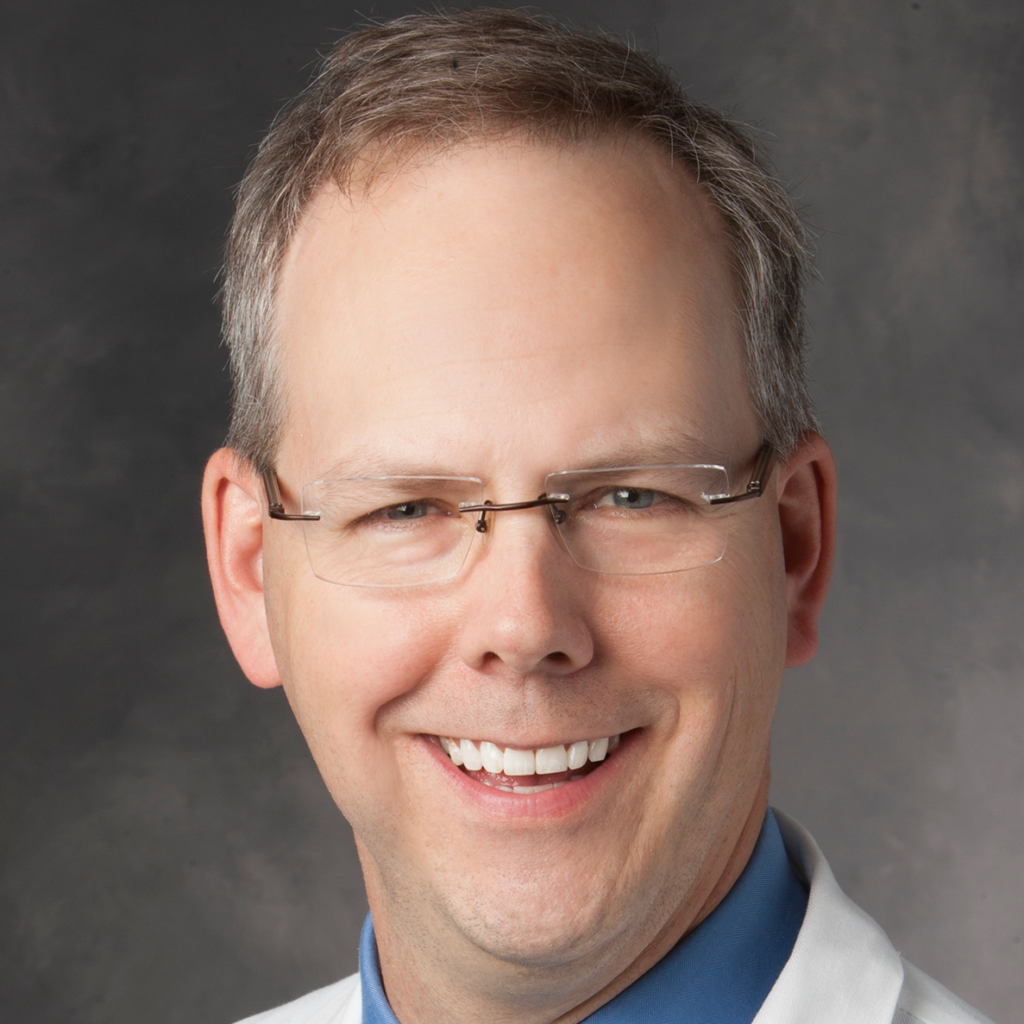
- Name: Dr. David Miklos
- Specialty: Blood and marrow transplant
- Roles:
- Chief of BMT & Cell Therapy
- Clinical Director Cancer Cell Therapy, Stanford University (2016 – Present)
- Experience: 25+ years
- Provider: Stanford Medical Center
We’d like to cure more and more diseases. What is cured?
People ask me all the time, ‘Am I cured?’ The difference between remission, where we have no measure of your cancer anymore on a scan or bone marrow or blood test, and a cure, is time.
Dr. David Miklos
- Video: Dr. Miklos on Mantle Cell Lymphoma Treatment
- Mantle Cell Lymphoma Treatments Have Improved
- Small molecule inhibitors
- Role of allogeneic bone marrow transplants
- Role of CAR T therapy
- Newest study: ZUMA-2 clinical trial
- New clinical trial
- What are the drawbacks of this newest therapy
- Balance between therapy efficacy and adverse effects
- Why patients should consider clinical trials
Video: Dr. Miklos on Mantle Cell Lymphoma Treatment
Mantle Cell Lymphoma Treatments Have Improved
Mantle cell is kind of the story of my life. An interesting story. When I was training back at Harvard in 1995, mantle cell lymphoma was first being recognized because we needed some antibody test to be able to tell the difference of these immature lymphocytes.
The very first patient I actually diagnosed was a person who had lymphadenopathy in my internship clinic, where usually I was treating diabetes or hypertension. The therapy was terrible.
Using CHOP chemotherapy had only a three-year overall survival. Rituximab added very little benefits to those patients. But there was development of small molecule inhibitors that are interfering with the signal from the b-cell receptor to the division inside the nucleus.
Small molecule inhibitors
These are drugs your people have heard of like ibrutinib, a drug that targets the Bruton’s tyrosine kinase (BTK) inhibitor. There are also other drugs.
Ibrutinib was the first and certainly the most widely-used drug. A pill you take once a day that covalently links and binds and inhibits the BTK molecule. That cell was done. The importance of that therapy where everybody responds, and yet, there are patients with about a 20- to 25-percent risk per year of progression.
Once we lose that very special target, we can go onto some other medicines like venetoclax, which has also shown benefit in the mantle cells.
But we’ve been looking for something better.
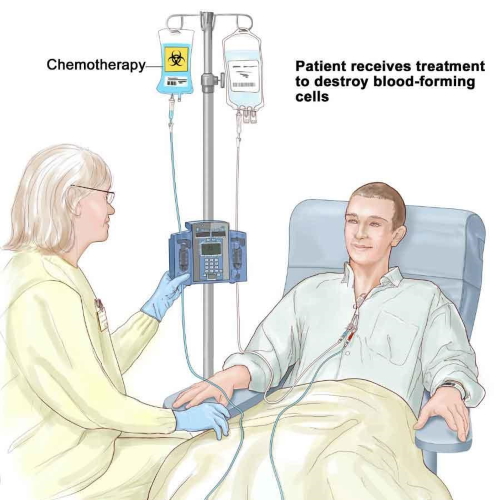
We’ve tried high-dose chemotherapy. I’m a stem cell transplanter, so the notion of using high-dose chemotherapy with stem cell rescue or what your patients will know as an “auto transplant” has provided much benefit to the patients of mantle cell lymphoma.
It moves out the expected overall survival from three to six years or more. There’s a role for maintenance rituximab, FDA-approved, and has benefits in patients, and the small molecule inhibitors, ibrutinib, venetoclax, which we just discussed.
But where’s the home run?
Where’s the targeted immunotherapy that is going to eliminate this cancer and provide the patient a long term cure?
Role of allogeneic bone marrow transplants
Some of your patients may have had an allogeneic transplant which is truly the immune therapy of some else’s immune system.
Maybe it’s a brother or sister or HLA-identical donor whose blood destroys the white cells, red cells, and regrows and reconstitutes the normal blood system.
In the process of getting rid of the patient’s blood system, it gets rid of the white cells, the lymphocytes, the b-cells, and the mantle cell lymphoma.
The allogeneic transplant is an immune therapy. I am an allogeneic transplanter and will talk about the major side effect of allogeneic transplant which is graft-versus-host disease (GVHD).
That means the immune response is not only attacking the blood and cancer, but it’s also sometimes attacking the skin, the gut, the liver, causing detrimental, inflammatory problems that can be the real bane of the existence of the patient.
The quality of life and the difficulties with organ involvements across the whole body has been seen. Those patients are really dependent on immune suppression.
So where’s the home run? The home run is, again, CAR T.

Role of CAR T therapy
The axi-cel therapy was the first FDA-approved treatment in large cell lymphoma. That company is called Kite. They were purchased by Gilead. They brought forward a very similar construct.
The actual molecule that is placed into the patient’s lymphocytes is exactly the same as what’s been used for the last three years in large cell lymphoma. So it binds the same CD19 again, same story, here comes the CAR. We’re going to bind and we’re going to then kill the cancer.
It’s prepared in a very special way because mantle cell frequently has lymphoma in the blood, so we have to separate the lymphocytes away.
That’s the unique difference between Tecartus and Yescarta. Otherwise, they’re nearly identical therapies.
And the prep to do this is the apheresis, the places where you’ll receive the therapy, the lymphodepletion chemotherapy, and the three days before we put the special cells in. It’s all the same. The follow-up stay in the hospital, seven to ten days, staying locally for 28 days, it’s all the same.
The expected toxicities of cytokine release syndrome, that’s the fever, achy, flu-like symptoms, or the confusion and neurological problems that can follow patients who have had the cytokine release syndrome, again, very similar incidents.
Newest study: ZUMA-2 clinical trial
Here’s the excitement: the excitement is in that study you addressed called ZUMA-2, which began in 2017, there were 60 patients treated and this overall response rate was 93-percent.
The overall complete response rate, couldn’t find the cancer, was 67-percent.
Two-thirds of the patients, 28 days after given this Tecartus infused in their body, had no measurable cancer, a complete response. That response has remained durable. The publication that is responsible for the FDA’s approval showed 27 months of follow-up in patients.
That’s just over two years, so let’s not get carried away. We have two years of follow-up and in that population, the response rate was 43-percent remaining in complete response and 67-percent overall response.
So it’s very durable. Probably even more durable than what we saw in the original treatment with axi-cel in large cell lymphoma. There are similar side effects and it still needs to be done inside the hospital at centers that have experience managing patients with CAR T therapy. The higher response rates and they appear to be very durable treatments.
These are for patients who had had three lines of therapy previously, so they probably had CHOP, or bendamustine and rituximab, they probably had ibrutinib as one of the therapies. That trial required they had a drug that targeted the Bruton’s tyrosine kinase (BTK).
The FDA, when they made the approval of this therapy in July, recognizing what a game changer the therapy offered patients, did not require patients go through three lines of therapy.
The FDA has authorized the treatment in second line and I think that’s because they really want to help patients achieve long-term disease-free survival and benefit.
Now, physicians will have to decide who should receive BTK inhibitors and who should go right on to CAR T-cells, and that’s discussion with the patients and the families. That really is still being worked out.
»MORE: Read patient experiences with immunotherapy

New clinical trial
We’re going to be doing a new trial where we’ll be looking at patients who’ve had ibrutinib upfront or who have not had ibrutinib yet, and using the same therapy to see what the true incidents of benefit is in that second line.
But in the meantime, there are centers that can provide commercially-available therapy with Tecartus today. If somebody’s gone through all the available therapies, that’s a lifesaver.
As we decide whether we should use CAR T-cells in second line, that’s an individual decision at this point for the patients and their doctors.
What are the drawbacks of this newest therapy
I think we have to make sure the therapy does not cause more toxicity than the patient’s need warrants.
What I think is going to happen is we’re going to see less CHOP chemotherapy up front. We’ll probably be shifting more to the kinder, gentler bendamustine-rituximab, and maybe even in combination with ibrutinib in the first-line therapy.
The intent of that is to really clear the disease, make sure we get the highest response rate possible with the lowest toxicities, and frequency of going into the hospital with side effects like neutropenic fever. We want to avoid that.
I think that’s where the field is moving. Then the key decision, and I’m the Chief of Transplant (at Stanford) so I don’t want to malign my own therapy.
But whether or not auto transplant continues to be important in the management of mantle cell versus going right on to a targeted cellular therapy, is really the next question.
So that decision needs to be made. What we’re trying to judge is what’s the risk of the patient having cytokine release syndrome or really high-impact, really debilitating neurological toxicity.

Balance between therapy efficacy and adverse effects
A grade three neurological toxicity is when the patient is really unresponsive in the hospital, just lying there, eyes open, frequently having expressive aphasia, can’t talk, can’t find the words, can’t attend. That period of time lasts usually two to three days and patients are being treated with steroids.
Young people, like us, we may have the ability to have the reserve to get through something like that and easily bounce back.
But if you were 80 years old, having a similar treatment options, and trying to decide, I imagine the ibrutinib therapy would be the more appropriate, at least until it’s not working.
While patients are receiving those better-tolerated, maybe not curative therapies with very good efficiency or efficacy, we’re working on new therapies. We’re working on kinder, more gentler therapies, with less toxicities.
The companies we’re mentioning here are fully committed to trying to improve these treatments. Whereas maybe the drugs you took for your blood pressure and your diabetes are still the same drugs after 20 years, these drugs will not be the same drugs after five years.
We will be moving the development curve cycle into a very rapid change, because knowledge is what is going to drive the next therapy.
As we learn how to help the patients, how to improve the treatments, what happens as the universities will quickly disseminate through pharmaceutical companies to the patients’ care.
Why patients should consider clinical trials
It’s a very exciting time. It’s these small clinical trials that are able to demonstrate clinical benefit, but at the same time, we’re collecting blood samples and lymph node samples that allow us to test questions like:
- How did it work?
- How did the CAR expand?
- Did it go into the lymph node?
- Did the lymph node stop making the target?
- How do we make this treatment better?
We call that the virtuous cycle of correlative clinical trials and that’s what these large academic centers are all about. We’re trying to turn that cycle as fast as we can.
That’s a partnership with our patients, so when your patients go to a cancer center and the doctor says, “We have a clinical research trial and we have the standard of care,” it’s important to listen closely.
There are very good treatments in the upfront use of tisa-cel, axi-cel, and soon, liso-cel, so we want to be able to offer those therapies to people with 60-percent complete response rates.
But if you are having a recurrence of disease after that therapy, or that therapy is not appropriate, then it’s important to consider participating on a clinical trial in order to get access to the more promising treatments.
That’s the hardest conversation. Bring all your friends, bring your family to the doctor’s visit. You’re going to need lots of ears to be listening to why you should do this or could consider these other options.
Your doctor should be making recommendations, but you, too, have to participate as you consider the benefits and the risks.
Dr. David Miklos’ Full Interview on Video
Other Oncologists
Dr. Christopher Weight, M.D.
Role: Center Director Urologic Oncology
Focus: Urological oncology, including kidney, prostate, bladder cancers
Provider: Cleveland Clinic
...
Doug Blayney, MD
Oncologist: Specializing in breast cancer | HER2, Estrogen+, Triple Negative, Lumpectomy vs. Mastectomy
Experience: 30+ years
Institution: Stanford Medical
...
Dr. Kenneth Biehl, M.D.
Role: Radiation oncologist
Focus: Specializing in radiation therapy treatment for all cancers | Brachytherapy, External Beam Radiation Treatment, IMRT
Provider: Salinas Valley Memorial Health
...
James Berenson, MD
Oncologist: Specializing in myeloma and other blood and bone disorders
Experience: 35+ years
Institution: Berenson Cancer Center
...
Jacqueline Barrientos, MD
Role: Hematologist, researcher
Focus: Chronic lymphocytic leukemia (CLL), lymphoma, 17p Deletion (Ibrutinib, Acalabrutinib, Venetoclax), IgHV mutation
Provider: Northwell Health (NYC)
...
Dr. D. Ross Camidge, M.D., Ph.D.
Role: Thoracic oncologist, Director of the Thoracic Oncology Clinical Research Programs
Focus: Lung cancer, small cell (Immunotherapy), EGFR (Osimertinib), ALK (Alectinib), ROS1 (Crizotinib), BRAF (Dabrafenib & Trametinib), NTRK
Provider: Univ. of Colorado
...
Edmund Tai, M.D.
Role: General oncologist, hematologist
Focus: Specialist in treating Chinese-speaking patients
Provider: Sutter Health (Bay Area, CA)
...
Irene Ghobrial, MD
Role: Clinical investigator and professor of hematological oncology
Focus: Multiple myeloma, Waldenström’s Macroglobulinemia, early screening, clinical trials
Provider:Dana-Farber Cancer Institute (Boston)
...
Tim Fenske, MD, MS
Role: Hematologist-Oncologist
Focus: chronic lymphocytic leukemia (CLL) & leukemia and lymphoma | CAR T, targeted therapy
Provider: Medical College of Wisconsin
...
David Miklos, MD
Date: Jan. 2021
Focus: Who benefits from CAR T, ZUMA-2 clinical trial, Stanford's CAR 22 Work
Provider: Stanford Medical
...
Kimmie Ng, MD, MPH
Role: Gastrointestinal oncologist
Focus: Young-onset colorectal cancer, microbiome
Provider: Dana-Farber Cancer Institute (Boston)
...
Farrukh Awan, MD
Role:Hematologist-oncologist, associate professor
Focus:Leukemias, Lymphomas, BMT
Institution:UT Southwestern
...
Kerry Rogers, MD
Role: Hematologist, researcher
Focus: Chronic lymphocytic leukemia (CLL), Hairy Cell Leukemia (HCL)
Institution: OSUCCC-The James
...
Nina Shah, MD
Role: Hematologist-oncologist, researcher
Focus: Multiple Myeloma
Institution: University of California, San Francisco (UCSF)
...
Rafael Fonseca, MD
Role: Interim executive director, hematologist-oncologist
Focus: Multiple myeloma, new drug development
Institution: Mayo Clinic
...
William Wierda, MD, PhD
Role: Hematologist, Med. Dir., Dept of Leukemia
Focus: Chronic lymphocytic leukemia (CLL), other leukemias
Provider: MD Anderson
...
Latest on CLL Treatment (2022)
Featuring: Nicole Lamanna, MD; William Wierda, MD, Ph.D
Hosted by: Michele Nadeem-Baker
Topics: Pirtobrutinib, new oral combinations, venetoclax updates, CAR T
...
David Miklos, MD, Ph.D
Role: Hematologist, researcher
Focus: How MCL treatments have improved, importance of clinical trials
Provider: Stanford Medical Center
...
David Miklos, MD, Ph.D
Role: Hematologist, researcher
Focus: Role of allogeneic BMT, response to graft versus host disease (GVHD)
Provider: Stanford Medical Center
...
CAR T Cell Therapy in Myeloma
Dr. Fonseca shares his insights on emerging T-cell therapies for multiple myeloma, describing the role T-cells play in our bodies and then focusing on chimeric antigen receptor (CAR) T-cell therapy and bispecific T-cell engagers.
...
Joseph Mikhael, MD
Role: Dir. Myeloma Research, CMO at International Myeloma Foundation (IMF)
Focus: Multiple myeloma
Provider: TGen/City of Hope
...
Ruben Mesa, MD
Role: Executive Director, Mays Cancer Center; Prof. of Medicine
Focus: Myeloproliferative neoplasms (MPN)
Institution: UT Health San Antonio MD Anderson
...
Srdan Verstovsek, MD, PhD
Role: Director, Clinical Research Center for MPNs at MD Anderson; Section Chief, MPNs; Prof., Dept. of Leukemia
Focus: Myeloproliferative neoplasms (MPN)
Institution: MD Anderson
...
Saad Z. Usmani, MD
Dr. Saad Usmani, Chief of Myeloma Service at Memorial Sloan Kettering, talks about CAR T-cell therapy, bispecific antibodies, novel therapies and combination therapies.
...
Vincent Rajkumar, MD
Dr. Vincent Rajkumar, a hematologist oncologist at the Mayo Clinic, talks about drug pricing and the impact of high prescription drug costs on patients and families.
...
The Doctor Talk w/ Dr. Gasparetto & Dr. Richter
Role: Dr. Cristina Gasparetto (Duke) and Dr. Joshua Richter Mount Sinai discuss latest relapsed refractory multiple myeloma treatments
...
Dr. Samuel Washington, MD, MAS
Role: Assistant Professor of Urology, UCSF
Focus: Treatment disparities in bladder cancer treatment
Provider: University of California San Francisco
...
Multiple Myeloma in 2023
Long-time myeloma patient and advocate, Jack Aiello, leads the conversation with Dr. Joshua Richter, Multiple Myeloma Director for Blavatnik Family Chelsea Medical Center at Mount Sinai and Dr. Muhamed Baljević, Plasma Cell Disorders Research Director for Vanderbilt-Ingram Cancer Center.
...
Matthew Matasar, MD, MS
Dr. Matthew Matasar, chief of blood disorders at the Rutgers Cancer Institute of New Jersey and RWJBarnabas Health, sat down with Dr. Samantha Spiegel, a Hodgkin’s lymphoma patient, to discuss some of the most exciting news coming out of ASH 2022.
...
DLBCL in 2023
The Patient Story founder and DLBCL advocate Stephanie Chuang leads the conversation with Dr. Josh Brody, who leads the Lymphoma Immunotherapy Program at Mount Sinai’s Tisch Cancer Institute, and Dr. Lorenzo Falchi, an oncologist at Memorial Sloan Kettering Cancer Center.
...
SABCS 2022 Highlights
Top breast cancer doctors Dr. Paolo Tarantino with Dana-Farber Cancer Institute and Dr. Lola Fayanju with Penn Medicine discuss the big highlights from this year’s San Antonio Breast Cancer Symposium.
...
Relapsed/Refractory Multiple Myeloma Highlights from ASH 2022
Multiple myeloma specialists Dr. Ajai Chari with Mount Sinai in New York and Dr. Sandy Wong with the University of California San Francisco discuss the big buzz at this year’s ASH: bispecific antibodies.
...
Myelofibrosis Highlights from ASH 2022
Dr. Serge Verstovsek and Dr. Naveen Pemmaraju discuss cutting-edge treatments and therapies, and combination therapy as a focus in treating myelofibrosis.
...
Newly Diagnosed Multiple Myeloma Highlights from ASH 2022
Dr. Caitlin Costello and Dr. Sagar Lonial discuss treatments for newly diagnosed multiple myeloma patients.
...
High-Risk Smoldering Multiple Myeloma Highlights from ASH 2022
Patient advocate Jack Aiello and hematologist Dr. Shaji Kumar discuss what high-risk smoldering patients can do to delay or possibly avoid progression to active myeloma.
...
DLBCL: The Latest in Treatment and Research
Discover the latest DLBCL treatments from two top lymphoma doctors and a diffuse large b-cell lymphoma survivor who is also a doctor.
...
Chadi Nabhan, MD, MBA
Dr. Chadi Nabhan shares how he got involved in the Monsanto trials, what he learned from the, and why he decided to write a book about the whole experience.
...
CLL Highlights from ASH 2022
Patient advocate Andrew Schorr and hematologist Dr. Nitin Jain discuss the latest treatment and developments in CLL coming out of ASH 2022.
...
Research on Black Myeloma Patients, Access & Disparities
Patient advocate Valarie Traynham and Dr. Shakira Grant discuss the barriers many Black patients face, how it impacts their care, and what can be done to help improve their outcomes.
...
Testicular Cancer: What Patients Need to Know
Medical oncologist Alok Tewari, MD, PhD, who specializes in cancers arising from the genitourinary tract, discusses what patients need to know about testicular cancer.
...
Lynch Syndrome: What Patients Need to Know
Medical oncologist Michael Hall, MD, MS, discusses Lynch syndrome, what cancers patients would be more at risk for, and who should get tested.
...
The Role of Bispecific Antibodies in the Treatment of Multiple Myeloma
Hematologist Alfred Garfall, MD, MS, from Penn Medicine discusses with multiple myeloma patient advocate Jack Aiello the advancement of immunotherapy for multiple myeloma, the difference between CAR T-cell therapy & bispecific antibodies, and the role of bispecifics in the myeloma toolkit of immunotherapies.
...
How to Build a Strong CLL Team
Nicole Lamanna, MD, from Columbia University Medical Center, Spencer Bachow, MD, from Boca Raton Regional Hospital, and CLL patient Lisa P. discuss the importance of building a strong support system and collaborating effectively with multiple doctors.
...
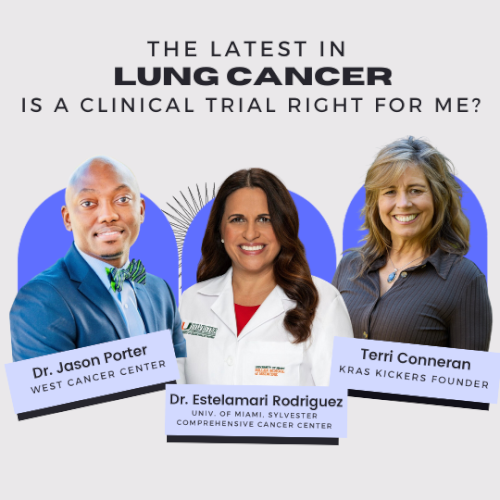
The Latest in Lung Cancer Treatments: Is a Clinical Trial Right for Me?
Leading experts Estelamari Rodriguez, MD, MPH, from the University of Miami Sylvester Comprehensive Cancer Center, Jason Porter, MD, from West Cancer Center & Research Institute, and Terri Conneran, founder of KRAS Kickers, discuss the latest in lung cancer treatments and ongoing clinical trials.
...
The Latest in Multiple Myeloma Treatments: What Clinical Trials are Available to Me?
Patient advocate Cindy Chmielewski, experts Dr. Carl Ola Landgren and Dr. Caitlin Costello, together with clinical trial nurse Christen Hawthorne uncover groundbreaking insights on the latest multiple myeloma treatments and clinical trials.
...
Clinical Trials and You: How to Navigate Treatment?
Patient advocate Ruth Fein Revell, experts Dr. Angela Fleischman and Dr. Ruben Mesa, together with clinical trial nurse Melissa Melendez delve into the cutting-edge realm of myelofibrosis clinical trials.
...
Let’s Talk CLL: Patients & Doctors Discuss the Latest LIVE
Patients, care partners, and a panel of CLL experts including Dr. William Wierda, Dr. Nicole Lamanna, Dr. Adam Kittai, and Jackie Broadway-Duren share the latest in CLL research, clinical trials, treatments, and comprehensive care strategies.
...
The Latest in Multiple Myeloma: Understanding Promising Treatment Options
Patient advocates Cindy Chmielewski and Jack Aiello, and experts Dr. Rafael Fonseca and Dr. Susan Bal discuss promising multiple myeloma treatment options.
...
The Latest in Hodgkin Lymphoma: Treatment Options in 2024
Dr. Matthew Matasar, chief of blood disorders at the Rutgers Cancer Institute of New Jersey and RWJBarnabas Health, discusses some of the most exciting news coming out of ASH 2023.
...
Optimizing Quality of Life: Reducing Toxicity in Hodgkin Lymphoma Care
Dr. Andy Evens from Rutgers Cancer Institute discusses how to reduce the toxicity of Hodgkin’s lymphoma treatments so patients can live their best lives after cancer.
...