Egg Retrieval & Freezing Before Chemotherapy and Cancer Treatment | Joyce’s Story
Joyce Yu was diagnosed with primary mediastinal B-cell lymphoma (PMBCL), a subtype of non-Hodgkin’s lymphoma. She journaled her entire egg harvesting, retrieval, and freezing experience day by day for The Patient Story below.

Joyce’s Timeline
- 7/23: Met with fertility doctor
- 7/24: Anesthesiologist phone consult
- 7/26: Anesthesiologist in-person consult
- 7/31 Met with the nurse
- 8/03: Start of hormones
- 8/07: Ultrasound/monitoring
- 8/12: Egg retrieval
- 8/13: Post-retrieval
For more patient stories and experiences with fertility preservation before cancer treatment, click here.
- Fertility Preservation Decisions
- Pre-Egg Retrieval
- How quickly did you see the fertility specialist after your diagnosis
- Please describe in as much detail as you can about that first meeting with the fertility doctor
- What were your options
- What was the next step?
- When did you first meet the nurse who would explain details of the procedure
- With cancer in your body, what were the precautions your fertility medical team undertook
- Injections Days 1-5
- Days 6-11 and Egg Retrieval
Fertility Preservation Decisions
Who brought up fertility preservation after the cancer diagnosis?
My oncology nurse navigator, brought up the effects of chemotherapy on fertility. Because I am 23, she did not want me to regret not trying to pursue the potential options out there to preserve my fertility.
Was your primary care doctor or oncologist open to the idea of postponing treatment for egg freezing?
My oncologist was supportive of postponing treatment for fertility preservation. He was comfortable giving me a months worth of time.
What were your biggest first concerns about the process?
Timing! Being able to start the process promptly so I can start chemotherapy ASAP. I knew the minimum time needed was 2 weeks for hormone therapy.
With this disease of non-Hodgkin’s lymphoma, I was worried if my body was going to allow enough time for me to go through with this egg retrieval and freezing process.
How did you decide which fertility clinic to use?
My oncology nurse navigator facilitated the process for me and chose UCSF CRM. It had the fastest turnaround time (24-48 hours) for cancer patients. I tried calling other private fertility clinics, but those would take a minimum of two weeks just to get a consult.
Pre-Egg Retrieval
How quickly did you see the fertility specialist after your diagnosis
I had a preliminary diagnosis on Tuesday, July 17. I called for an appointment on Thursday, July 19, hoping to be seen the next day.
Unfortunately, they didn’t have any openings until the following Monday, July 23, but I was still very appreciative to be able to be seen on such a short notice.

Please describe in as much detail as you can about that first meeting with the fertility doctor
I first met with the fellow, Dr. Wald, who went through all my past medical history. I then met with Dr. Rosen to discuss fertility options.
He took out a piece of paper and started making a diagram to show the inverse linear relationship of the number of eggs and age. As one ages, the number of eggs decrease. Therefore, since I’m 23, I should have a lot of eggs.
He then immediately took me to get an ultrasound to see how many eggs I had at the moment. He guessed around 10, which is relatively low for my age. We went back to his office to discuss more.
He said that post-chemotherapy, I’d be at a 20-percent risk of hitting menopause or 50-percent risk of hitting early menopause; he couldn’t give me a number of the chance of being completely infertile.
What were your options
He gave me three fertility options:
- 1) Monthly Lupron or Zoladex injections, which signal the brain to stop ovaries from making estrogen
- 2) Egg freezing
- 3) Post-treatment egg freezing.
I opted for all three since I wanted to do as much as possible to protect my chances of having a baby in the future.
Overall, I was very happy with my meeting. Dr. Rosen was very straight forward, compassionate, and sincere. He assured me that he would do whatever it takes to make sure that I can have a baby in the future.
After my meeting with Dr. Rosen, I briefly met my nurse Cathy, and I then went to see someone on their financial team to discuss insurance and costs.
What was the next step?
There wasn’t really a talk about a schedule, just two weeks of hormone therapy and monitoring carefully before egg harvesting.
Next step was an anesthesiologist consult on the phone. I spoke to the anesthesiologist very briefly for about 10 minutes before he decided that the consult should be done in person.
I was honestly disappointed because this delayed the process. I felt that they should have foreseen having the consult in person. I wasn’t able to have the in-person consult until two days later.
I was very distraught, but I’m thankful that Dr. Rosen reached out to me to assure me that I wasn’t forgotten and that they are doing the best they can to expedite the process.
For my in-person anesthesiologist consult, we went through my past medical history. He physically examined me and had me get a blood test. He also wanted me to get a chest X-ray and echocardiogram the day before the planned egg harvesting to be safe.
He personally thought that it was fine for me to proceed with egg harvesting, but he needed everyone on board, including Dr. Rosen and the head anesthesiologist. He also warned that I might not be put to sleep during the procedure. It could just be local anesthesia or the whole procedure could be canceled the day of.
It wasn’t until the following Monday that I learned that I could proceed with the egg harvesting. I was super happy and I was scheduled to meet with my nurse the following day to start the injection teachings.
When did you first meet the nurse who would explain details of the procedure
I met with my nurse, Cathy, on Tuesday, July 31 since I was planned to start the hormone injections on Friday, August 3. Dr. Rosen chose Friday for me to ensure that my egg harvesting takes place on a weekday since I have to get additional testing done beforehand.
Cathy went through the several medications that I needed to administer for the next two weeks. The medications are Gonal-f RFF Redi-ject Pen vs. Cetrotide and Follistim vs. Menopur; there are two different kinds of medications for the same purpose.
I can see that the injections can be overwhelming to do but luckily, I’m a nurse so it wasn’t bad learning the different injections, and it didn’t take long for me to learn.
She briefly mentioned the Ganirelix, which prevents premature ovulation, and the Novarel trigger that stimulates egg release during ovulation. I don’t know much about the latter two drugs, only that I have to bring the Ganirelix to my next appointment.
With cancer in your body, what were the precautions your fertility medical team undertook
Since my mass was large, everyone was concerned about putting me under anesthesia. Because the egg harvesting is done at an outpatient clinic, they don’t have the same resources as a hospital would to resuscitate me if something does happen.
Therefore, they were being super cautious, and the anesthesiologist advocated for a chest X-ray and echocardiogram the day before the egg harvesting.
Dr. Rosen was also concerned about the potential third spacing adverse effect from the hormone injections.
Third spacing can cause all kinds of problems like pulmonary edema, cerebral edema, and decreased cardiac output.
If third spacing happened, I wouldn’t be able to proceed with egg harvesting.

Injections Days 1-5
Day 1. Friday, 8/03
- Menopur, 150 IU: 10:00 PM
- Gonad-F, 300 IU: 10:10 PM
A nurse filling in for my original nurse called me in the morning at 9 AM to remind me to administer the injections tonight, any time from 6 PM – 12 AM.
I also had to inject the same time everyday within a hour window. She warned me that the first time takes about 45 minutes. I chose to administer the injections later at night around 10 PM just in case I am ever out and about before then.
When it was around 9:00 PM, I looked through the site to refresh myself on the Gonad-F and Menopur injections beforehand. I also looked at their mailed-in Gonal-F manual again.
I set up the Menopur first since the Gonal-F had to stay at room temperature for 30 minutes before administering. I’m taking 150 IU of Menopur (two bottles of 75 IU) mixed with 1 cc of saline.
It took some time for me to mix everything together and have the medication pulled back into the syringe since I wanted to make sure I got all of the medication in the syringe, and I didn’t want an incorrect dose or lose any precious medication.
When it comes to injections, I always use a bag of ice to numb the area for about 10 minutes before injecting. It helps a lot since I can barely feel anything. Injecting the Menopur was easy but I did feel the burning sensation as the medication went in, so now I do not ever look forward to that injection.
On the other hand, I love the Gonad-F pen since it was very simplified and painless. It is an auto-injector pen, so all I had to do was place a needle and set the dose before administering it.
Day 3. Sunday 8/05
- Menopur, 150 IU: 09:45 PM
- Gonad-F, 300 IU: 10:08 PM
Takes me about 25 minutes now! I haven’t noticed any side effects or injection site reactions yet, just the same burning sensation with the Menopur.
Day 4. Monday 8/06
- Menopur, 150 IU: 10:00 PM
- Gonad-F, 300 IU: 10:09 PM
I’m getting better! Takes me about 20 minutes now! I’m starting to feel a little bit more bloated. I don’t know if it’s because of what I ate today or just side effects.
I’m also definitely more emotional. I cry more easily depending on what my mom says. My mom tried to reassure me multiple times that everything will be okay, but I just ended up breaking down because it got too much for me.

Day 5. Tuesday 8/07
- Menopur, 150 IU: 9:56 PM
- Gonad-F, 225 IU: 10:08 PM
I went in for my appointment at 9:30 AM for blood work and an ultrasound. I’m always happy whenever the medical assistant can get my vein the first time around.
Nurse Practitioner (NP) Katrina did my ultrasound. She started by checking my endometrial lining, and she said that it looks good. I’m not quite sure of the measurement or what would be a good measurement, but I’ll be sure to ask her next time.
Next was counting the follicles, starting with my right ovary. There were 8 follicles of various sizes. Katrina measured each one, and the medical assistant entered the measurements on the computer. On the left, there were 10 follicles of various sizes.
The biggest follicle was 15 mm. Katrina was pretty happy with the results and how my body was responding to the hormones so far. Since the biggest follicle is over 13 mm, she had me start the Ganirellix injection in the room to prevent premature ovulation.
My nurse called back with feedback from Dr. Rosen and results from my blood work. She had me decrease Gonad-F to 225 IU, stay with the same dose with Menopur 150 IU, and start Cetrotide injections daily in the morning.
My estradiol level is 1153. Again, I am not sure about the significance of that number. My nurse let me know that I will probably have to come in every day or every other day for monitoring, so my next appointment is tomorrow at 9:45 AM.
I’m feeling super tired for some reason today, going through a headache. My NP, Katrina, did warn me that one of the side effects is a headache. I wish I didn’t have to go through hormones today, but I still got them done.
Also, I went on the educational website again since I’m starting the Cetrotide new injection tomorrow morning. It seems easy; everything I need is pre-packaged. There’s a pre-measured vial, so all I need to do is mix the solution, change the needle, and inject.
Days 6-11 and Egg Retrieval
Day 6. Wednesday 8/08
- Menopur, 150 IU: 10:04 PM
- Gonad-F, 225 IU: 10:08 PM
I took my first dose of Cetrotide to prevent premature ovulation this morning at 9:30 AM before my CRM appointment. I’m always excited for new medication, and I’m glad it was easy and painless.
I went to CRM this morning at 9:45 AM for my daily blood work and ultrasound. Unfortunately, the medical assistant couldn’t get my vein the first time around and had to poke around. She took me to do my ultrasound instead first.
My follicles definitely grew over a day. My largest follicle now is 18 mm. Overall, half of the follicles look ready to be harvested whereas half are still growing. My NP, Katrina, said that we will probably look at egg harvesting over the weekend, which is great news to me.
I’m glad things are moving quicker than expected, and I’m responding well to the hormones. I still need official confirmation from Dr. Rosen for an official date, so I’ll see how things progress tomorrow. For now, I have a scheduled echocardiogram on Friday, just in case.
I’m feeling tired and getting blurry vision for some reason at this time before my injections. I really cannot wait until I am done with all these injections. The finish line is the only thing pushing me going.
Today, I started to notice several minor injection site bruising and soreness. The bruises aren’t bad; they’re just the size of pen marks.
The good thing about bruises is that I know where all my past injection sites are and I can easily choose injection sites around those bruises.
Day 7. Thursday 8/09
- Menopur, 150 IU: 10:30 PM
- Gonad-F 225 IU: 10:45 PM
I took my second dose of Cetrotide this morning before my CRM appointment at 10:00 AM. During my ultrasound, a bunch of new follicles grew, but unfortunately, they won’t be mature enough for the egg harvesting in time.
This was my worst night yet. I felt super sick. I threw up. My arm experienced severe nerve pinch pain from my tumor, and I had extreme discomfort in my chest.
Also, the additional intense migraine from the hormones did not help. I had to take a Tylenol and Advil, both of which didn’t help. I had to lie down for the rest of the night, and I ended up missing my routine times for injections.
I just did not care at that point anymore about what time to inject. As long as everything was within the hour, I was okay with that. As soon as I felt a little bit better, I hurried up and got everything together to inject myself. Then I ended up staying upright for most of the night so the sickness would subside.
I cannot wait for these hormone injections to be over; the side effects are getting overbearing. I was super close to calling it quits and taking myself to the emergency room, but I’m someone who does not like to give up.
Day 8. Friday 8/10
I took my third dose of Cetrotide this morning at 9:30 AM before my CRM appointment. My largest follicle is now 20 mm! I learned that I will also be triggering tonight at 9:00 PM with HCG 1,500 units first and Lupron 80 units subsequently!
I’m excited since this means no more hormone injections, no more painful side effects, temporary stop on lovenox injections, and egg retrieval 36 hours later on Sunday at 9 AM!
Today, I also went to get a chest X-ray and echocardiogram both at UCSF as a precaution measure. The chest x-ray was super easy, just two snapshots with a front and side view. The echocardiogram took about 25 minutes.
The two injections tonight were super simple. For the HCG, I had to mix 3.3 mL saline solution in my 5,000 unit vial and draw up 1 mL to inject. For the Lupron, I just drew up 80 units to inject. Both were quick and easy.
Day 9. Saturday 8/11
Nothing too eventful today; I went to CRM for more blood work. Best part of today is having to do nothing. NO INJECTIONS!
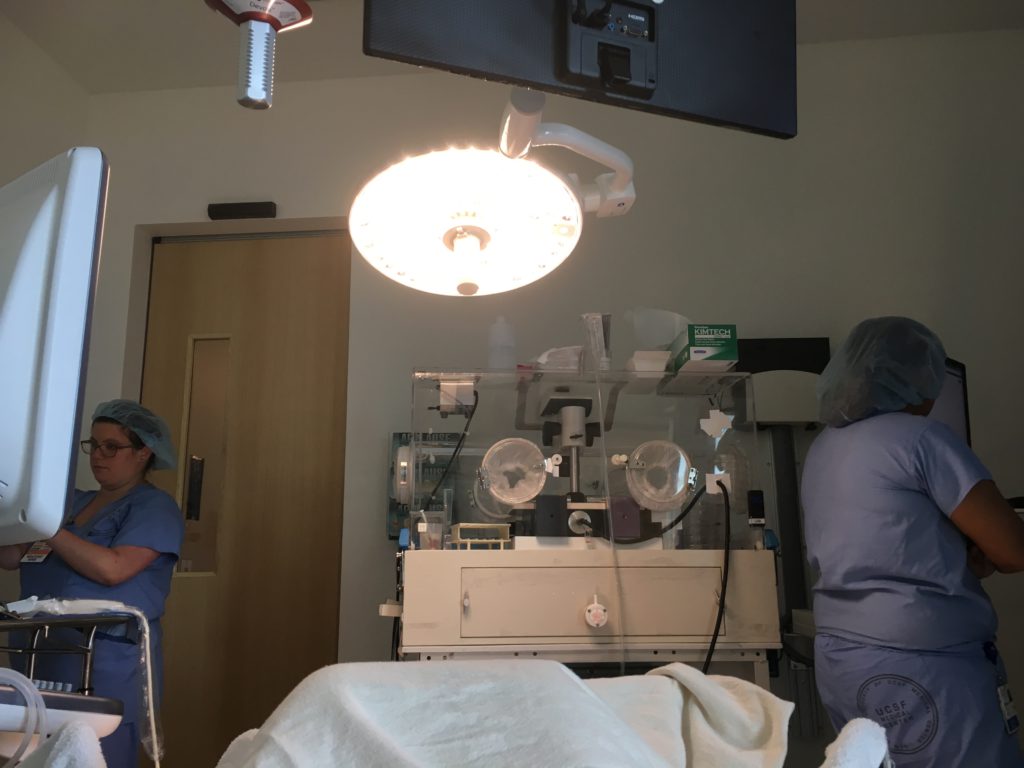
Day 10. Sunday 8/12 – Egg Retrieval
After midnight, I could not have anything to drink or eat, so I stayed up until then to make sure I was well hydrated for the next morning. I barely slept the night before egg retrieval.
It was a combination of nerves and excitement. I’ve been waiting for this very day for the past three weeks, and it’s finally here! My egg retrieval was scheduled for 9 AM, but I had to be there at 7:45 AM to be pre-oped and get prepared.
When I got there, I was taken in to the “pre-op” area, where I met my nurse. She went over what to expect. I was told to show up in comfy clothing, but my nurse had me immediately changed into one of their gowns.
Next was meeting Dr. Cedars, Dr. Rosen’s work partner, who would be extracting the eggs, and meeting the anesthesiologist, Dr. Cui. They both went over everything once more separately and answered questions.
I learned that I would be undergoing conscious sedation. Dr. Cui listed a bunch of IV medications that I can’t quite remember. I know one of them as propofol. I just know them altogether as twilight anesthesia, where it’s not general anesthesia but medication-induced sleep so I would be breathing on my own.
After we were done with questions, my nurse brought my parents in the room to wait with me, and my nurse placed an IV in my right hand. She hooked me up to a bag of saline fluids and gave me 1000 mg acetaminophen beforehand for pain management afterwards.
Once it was 9 AM, the nurse manager took me to use the restroom before being brought into the procedure room. I laid down on their gurney with my legs spread open facing Dr. Cedars. She was very calming.
Dr. Cui hooked me up to 4L of oxygen. It was too much of a dose for me so I asked him to lower it to 2L, which felt much better. The nurse manager started infusing medications into my IV, and the next thing I know, I woke up groggy in one of the recovery bays. It was about 9:25 AM.
I felt like I just had a good nap. I didn’t feel any discomfort. The heater pad on my stomach felt nice and soothing.
Dr. Cedars came back in to check up on me, said that I did well, and said that she probably retrieved 23 eggs, which is great! She said that the only painkiller I could take is acetaminophen 1000 mg since I’m at high risk for blood clots.
For the next two hours, I stayed in the recovery bay with my parents. The nurse gave me water and crackers, checked my vital signs multiple times, and disconnected my IV after I was ready to be discharged. I felt pretty much okay overall.
I could walk, but it wasn’t the most comfortable thing to do. It felt like someone beat up my insides, and I was semi-sore. The effects of the anesthesia last about 24 hours in the body, so I did feel the effects of it the whole day as if I was hung over.
I spent the next two hours at an all-you-can-eat hot pot place since I was starving and to celebrate that I passed this part of my cancer journey. It was nice to just sit and stuff my face with lots of protein to recover.
Afterwards, I spent the rest of the day either on the sofa or in bed with a water heater pad on my stomach. It wasn’t that bad.
It honestly just felt like a really mild period that I had to be careful with when it came to position changes. If I lie down a certain way like on my side more, I would feel the soreness more.

Day 11. Monday 8/13
The next day, there was slight discomfort and more bloating, where my stomach was rock hard but overall, not too bad. Dr. Rosen called me to let me know that 22 eggs were retrieved and 16 were mature. I’m pretty happy about that.
All I really need is one to work its magic. He warned that I will be bloated for the next two weeks or so. For the first time ever, I cannot wait to get my period so all the bloating can go away and I’ll be closer to my old self.
Overall, I am very happy with my egg harvesting journey, even though there were many moments where I thought I wouldn’t be able to proceed. It took less time than anticipated, typically 10 to 15 days, since my body responded really well to the medications.
I’m hoping that I will never have to resort to using these eggs and instead donate them to someone in need.
However, I’m very glad and fortunate for this journey and that I have the extra insurance for whatever happens in the future.
»MORE: Read more cancer patients’ experience with fertility preservation and cancer treatment
