Tina’s* Moderate to Severe COVID Story
Young & No Underlying Medical Conditions
*Pseudonym to protect patient’s identity
Fast Facts
- Diagnosis:
- COVID-19 or novel coronavirus
- 1st Symptoms:
- Sore throat
- Fatigue
- Chills
- Fever (10 days, mostly 100-101 degrees Fahrenheit)
- Nausea
- Shortness of breath
- Treatment:
- Remdemsivir
- Clinical drug trial
- Developed as possible treatment for Ebola virus infection, now under clinical testing to treat COVID-19
- Treatment Center:
- PAMF (Urgent care, 1st tests)
- Stanford (Clinical drug trial and hospitalization)
- Diagnosis
- How do you think you got the coronavirus (COVID-19)?
- When did you realize something was wrong?
- You kept working despite feeling flu-symptoms
- How did you figure out what you had and what to do?
- When did you call the doctor?
- How did you know where to go for medical attention?
- It was confusing to figure out where to be
- Outside of that mix-up, describe the urgent care experience
- Describe your second trip to urgent care
- The doctor diagnosed you with coronavirus
- A misdiagnosis happened after a set of X-rays were taken
- Diagnosis was changed back to coronavirus after blood tests
- Quarantine, Work, Family
- Emergency Department Visit
- When did you decide to go to the ER?
- How did the hospital staff receive you?
- ER doctor did not want to give you a coronavirus test
- They took your vitals and suggested sending you home
- What tests did they give you?
- You ended up getting two sets of X-rays taken
- You had dealt with a lot of different medical opinions up to this point
- Hospitalization
- Clinical Drug Trial: Remdesivir
- How did you end up on a clinical drug trial?
- How many other people were enrolled in the trial when you were on it?
- That’s when they officially gave you the coronavirus/COVID-19 test
- How long did it take to get the coronavirus swab test results?
- You moved rooms and met a new doctor for the trial
- How did he describe the trial?
- Describe the drug infusion
- Describe the “crazy dream”
- Recovery in the Hospital
- Your fever broke after the first infusion
- After the fever subsided, what were the other side effects?
- Describe the shallow breathing
- Eating became top priority
- What’s your advice on dealing with nausea and keeping food down?
- What helped you manage your breathing?
- How did you recover and reconnect with family?
- Remdesivir was a successful drug for you
- It’s in clinical trial so not widely available. You were one of the lucky ones.
- Availability of remdesivir
- How did they make the decision to discharge you from the hospital?
- Quarantine at Home
- How long was the recovery and then the self-quarantine?
- When do they consider it to be the last day of symptoms?
- When did your breathing normalize?
- What were the official instructions for self-quarantine?
- Recovering at home felt harder
- How did the medical staff check up on you when you were at home?
- The city also checked in with you
- Taking care of mental health is so important
- Dad's Severe Case of Coronavirus
- Your parents are both in the higher risk group
- Where did they get the COVID swab?
- Describe the Stanford COVID testing clinic
- How did your dad end up in the hospital?
- Your dad took hydroxychloroquine instead of remdesivir
- Your dad’s coronavirus case was classified as severe
- What was his hospital experience?
- How did they self-quarantine?
- They got a call from their county
- Final Thoughts
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis & Treatment (Remdesivir)
Diagnosis
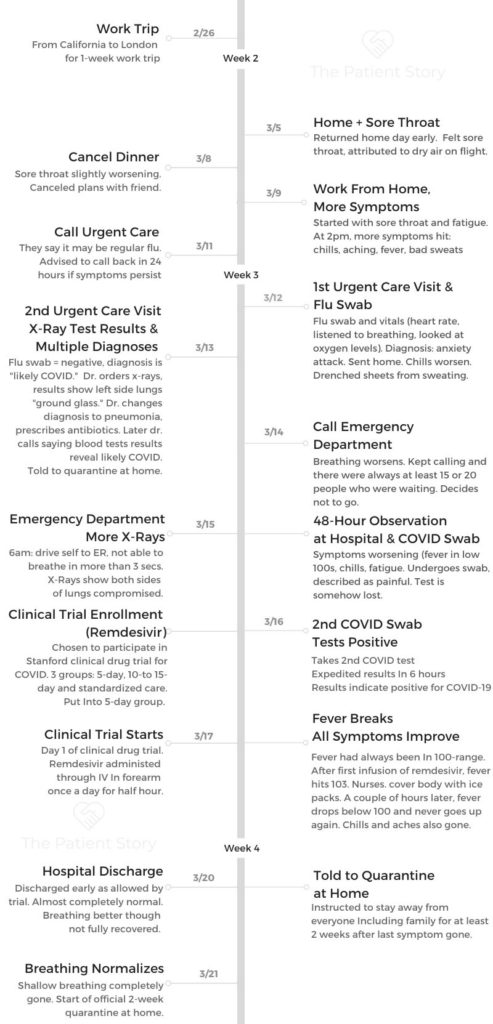
How do you think you got the coronavirus (COVID-19)?
It actually all kind of started first when I went on a business trip. I went to London and I was there from pretty much the 26th of February through the 5th of March. So a full week.
Before I went, I was asking everyone – my husband, my parents, my friends, my colleagues, boss, everyone – do you think I should go? Should I cancel? And everyone’s like, oh, I think you’re actually fine in London. I think it’s actually safer there than it is in the Bay Area. I remember when I was there, I was thinking I should be okay.
But I was feeling very scared and would wash my hands constantly. I remember on the fourth is when I actually had to present. There were 250 people there from all over Europe. No one from Italy was allowed, but it was people from all over. I remember they were shaking my hand, I was talking to all of them. They’re all in my face. I was thinking, okay, as long as I could go wash my hands afterwards, it should be fine.
My flight was supposed to leave on Friday, the sixth, but I moved it up to the fifth, Thursday, so I could leave early because that’s when stories started coming out and I was starting to panic. I got home on the same day on Thursday. I had a sore throat by that point, but I’m the kind of person that gets sick on airplanes because the air is really dry. I didn’t think too much about it.
When did you realize something was wrong?
I came home early. We had friends come over for dinner. I felt fine aside from a sore throat, which is something I usually get when I travel. So I didn’t think too much about it over the weekend.
It started to get a little bit more pronounced, the sore throat. And I remember I had a friend who was supposed to come over on Sunday, but I was like, actually, do you think maybe we can postpone? I’m not feeling so well. But it was just a sore throat. I remember on Monday, March 9th is when I had to go straight back into work [from home] and I didn’t feel jet lag, but I was feeling a bit of fatigue.
I remember specifically around 2 pm is when I started to feel the chills, which eventually led to a full blown, really bad fever.
And that was because I had to lead a call at that time. That’s when I would say I got the full symptoms. I had a fever, chills, really bad sweats. It was nonstop. And I was thinking, okay, I probably just had the flu, right. That went all the way into, I would say Thursday.
You kept working despite feeling flu-symptoms
The entire week that I was working [from home], and I was working like a crazy person by the way, I was feeling the fever for those four or five days.
We formed this COVID SWAT team at work and I was leading it. We had to put together all these playbooks on how companies should respond to some of this coronavirus and how they should reallocate their budgets. It was crazy.

I was working 12 hours a day. I think that just made things a lot worse because I was very stressed out.
And I had this crazy fever and I was taking Tylenol and I wasn’t sleeping. It was crazy.
How did you figure out what you had and what to do?
I went online. I Googled coronavirus. I was in denial because I had a fever but I didn’t have a dry cough. Whenever I tried to take a deep breath there was pressure in the back of my throat trying to force myself to exhale immediately. I was in denial because it was there at a very, very small amount, but over the weekend got worse.
I visited many sites cause I was very paranoid about what was going on. I went to the CDC website but it lacked depth and information. It just said the same thing – an infographic thing showing icons of people who had a fever, shortness of breath and dry cough. I already know this. You need to give me a little bit more information. I need to see all the gradients of that information.
I finally found a website saying if it’s a fever, it’s a low grade fever and it usually is between 100 to 100.7 or something.
When did you call the doctor?
Wednesday the 11th. I actually called urgent care saying I actually was traveling, I went to London. I have these symptoms. I have a fever, a sore throat, I’m not quite coughing, I don’t have shortness of breath. But I wondered if I could have COVID?
They’re like call us on Thursday because if this flu doesn’t get better by three days, which is when most of us get better, then maybe you should come in.
How did you know where to go for medical attention?
I had gone to urgent care in the past when my kids didn’t feel well and urgent care is very close to where I live and so I just went there.
They’re the ones who told me that if your breathing changes at all, you need to go to the ER because coronavirus works very rapidly. Within five or six hours the entire situation could change into something very, very bad.
It was confusing to figure out where to be
The part that I think was very badly managed was the urgent care. I was getting different information. One nurse told me to come in and when I came in, they’re like get the hell out of here. Then someone said well if we knew you had it, we would tell you to use the back entrance.
There’s a back entrance where someone walks you in, they give you a mask afterwards and they throw on a full hazmat suit. There is a whole procedure that you should be following that they had, but they failed to tell me that.
So I just felt a lot of people didn’t really know what’s going on because it was happening so fast that the information wasn’t scaled.

Outside of that mix-up, describe the urgent care experience
I called them on Thursday and the nurse was like, you should come in and we’ll take care of you. So I went into urgent care.
A physician’s assistant sat me down and took my heart rate. She listened to my breathing, she looked at my oxygen levels. They took a swab for the flu. She’s like you’re just having an anxiety attack. You’re panicking, you’re fine. Trust me, you’re healthy, you’re young, you’re fine. She sent me home.
Then the entire night, I had chills. I was sweating so much and I drenched my entire sheets, my blanket, everything. I’m thinking this is day four. Flus are supposed to be gone out of your system after 72 hours. So I knew something was not right.
Describe your second trip to urgent care
I call urgent care again. They’re like, okay, this time you can come in. We’re not going to give you a hard time. Someone will see you. When I went in, I was wearing a mask.
They called pretty quickly to just do my vitals. My blood pressure looked like it was on the low side but still okay. They are checking my heart rate and all these things and then they say go back and wait until the doctor called me.
The doctor diagnosed you with coronavirus
I remember the doctor actually called me on my cell phone because he said he was trying to minimize the amount of time he spent with me. That was what they were directed to do with all the people who potentially had COVID. So I just sat in there and the reception was so bad he could barely hear me, but I remember he said that I should go to the hospital right away cause he said it sounded I had COVID.
I’m like, how could you say that? The woman yesterday thought I didn’t have it. All they do is do my blood pressure. He’s like, well, because I saw your flu swab – it’s negative.
I’m like, oh my gosh, it’s negative and I still have a flu – what’s going on. He said clearly it’s not the flu and also your blood pressure, it looks low and then you told them you were dizzy. I just said I was a little dizzy because I had been sitting down, lying down all day and he’s like, you need to go to the hospital right away. I said I can’t just go to the hospital – I have children. He asked are you saying you refuse to go?
He then said he couldn’t really hear me and would come into the room. I’m so glad he came in because it was just night and day. It was much more calm. He was like, I’m pretty sure you have COVID based on the fact that you’ve had a four day fever, you don’t have the flu.
He listened to my breathing and he said that’s not normal breathing. That really freaked me out because no one ever said that about me. “Your breathing sounds diminished.”
At that point I realized that he was right. I was in denial. There was this pressure in the back of my chest that was forcing the air out and I couldn’t take a deep breath. And as soon as he said that, I was very much aware of it.
A misdiagnosis happened after a set of X-rays were taken
The doctor made me do a series of X-rays just to see what was going on. He came back within maybe 10 minutes because they were pretty quick.
He was like, actually you don’t have COVID, you have pneumonia. It’s on the left side of your lungs. You have these things that look like ground glass that’s making the X-ray harder to read.
Those are the classic signs of pneumonia and he says, I’m going to give you antibiotics, you’re going to go pick it up and you’re going to head home.
So I went to CVS, there was a very long line, people were buying up all this stuff. It was the start of the panic, right? Because it just started with the shelter-in-place announcement.
I waited forever to get my prescription. I walked out and then I went home and I realized that there were a bunch of messages from me from the doctor.
Also, my own doctor called because she had seen the results, too. So both sets of doctors are now calling me.
Diagnosis was changed back to coronavirus after blood tests
Long story short is both doctors called me at the same time [after they saw] the blood work that they took when I was in urgent care had come back.
The doctor said, actually I take it back. You don’t have pneumonia, you have COVID because your blood work is showing that you have really low white blood cells, as well as red blood cells. That’s what COVID does. It really lowers your blood cell count.
The thing that makes it look a little strange and makes it seem it’s not coronavirus is that it’s only compromising the left side of your lungs. In most cases it would be both sides. It’s not very normal for someone your age to have it so that’s why we’re just a little bit concerned right now.
At that point I was full blow having a panic attack. Am I going to die? Do I have pneumonia? Do I have coronavirus? I don’t know. And they wouldn’t give me a COVID swab because Trump was making it very hard for testing. I think even now, they didn’t have any tests at PAMF when I went in. They couldn’t give me one.
Quarantine, Work, Family
What were the instructions for quarantine?
They said act as if you have to quarantine yourself. They told me I couldn’t share a bathroom with anyone in my house. That I shouldn’t even share utensils. They said to use plastic ones. They said I should wash my clothes separately. I should, if I could, stay at a completely different place than family.
I was very fortunate. We have a guest house with a separate kitchen and a bathroom. So I just literally locked the door because my kids are trying to come in and I’d completely isolated myself. My husband kept trying to come in to help me, but they said to keep him away.
I also didn’t eat for three or four days because the nausea was so bad. I couldn’t keep food down. It was so crazy. I remember I was vomiting. It was very miserable staying by myself.
And then the doctor that had seen me in the urgent care was like, I’m going to call you in the morning every day. I’m going to just check it on you. He was so helpful.
When did you call the Emergency Department?
It was a Saturday. I remember that. I was just in the guest house all day just wondering am I going to die? What’s happening? I kept calling the ER to see how full it was because the one thing that doctor told me before I hung up was if you find that your breathing changes and you suddenly have a hard time breathing, you have to go to, you have to call 911 right away because this thing gets bad very quickly. It can be literally five or six hours and something bad could happen. For some reason this thing just really can destroy your heart very quickly and if you’re not breathing normally, even worse than you are now, you have to call mainly because all those things can start having a domino effect.
I remember just being like, that’s so scary. Maybe I should just go to the ER. So I kept calling and there were always at least 15 or 20 people who were waiting. Okay, I can’t go.
How did work react to your diagnosis?
I was in touch with my work and I told my boss, I have coronavirus. He was just horrified. He was like don’t even think about work. I’ll be the person to manage everything. Any kind of next steps need to be taken, I’ll help you manage that.
The next step was that I’d go on short term disability for as long as the doctor thought I could be out. He said I think that you should need three weeks just to be at home. And so I was like, okay, this sounds good.
You learned that you had given the coronavirus to family members
My mom called me [during my quarantine]. She and my dad were renovating their home and so they stayed with us for the week and they’re helping to care for the kids because my oldest daughter’s school was shut down.
My mom was telling me that her and my dad both had these coughs and they had fevers. Because they’re older and my dad has serious heart problems, they went to Stanford and they gave them COVID swabs because Stanford hospital actually at that point was making their own.
Their tests came out positive.
I gave it to my parents. I was just so horrified that they had actually gotten it and I kept apologizing to my mom because the whole week all she was doing was cooking for me, caring for me, telling me not to work so much. And now she had the coronavirus and my dad has really a pretty serious history of heart disease. I was horrified.
To this day, I haven’t really processed it. I don’t even allow myself to fully think it through cause I think that it’s just too much to unpack. It was a pretty horrible feeling to know that I’ve given this potentially fatal virus to my parents who are in that high risk group.
Emergency Department Visit
When did you decide to go to the ER?
On Sunday morning I told myself if there is no one waiting at the ER at Stanford, I’m going to go. And I called and they said there’s no one waiting. It was 6 in the morning. I drove myself over. I was very aware of the fact that I couldn’t breathe and it was worse than before. I was really timing how much I could take a breath in before I felt I was going to just cough it out because it was so much pressure.
It was three seconds. I couldn’t breathe in for more than three seconds. I originally was trying to stay calm. I remember thinking, I could die, right? This is so crazy. I’m 37. I don’t know why this is happening.
So I remember telling myself, okay, just come on, drive to the ER. I remember the whole time I was driving this car kept following me and I was wondering why they’re going to the ER. There was another guy with a mask and both of us came in for the same reasons. He looked like he was my age. This guy was also telling the security guard that he was traveling and he also felt he had caught a virus.
How did the hospital staff receive you?
They made us both wait for the nurse to come in. Both of us got checked in. They put me in this emergency room. I remember everyone on that floor were very old and they were all there for COVID.
I was thinking I’m the only young person here. Then the doctor came in and he looked very young. And he was pretty lax about it. He said I don’t think you have it. You just look well to me. You look fine, you look like a healthy person, you honestly don’t have COVID.

ER doctor did not want to give you a coronavirus test
He said anyone could have coronavirus, but the fact is we can’t just give swabs to people right now cause we don’t have enough. So the fact that you look fine, you’re young, you should just go home.
He’s like just quarantine yourself and just monitor your breathing. If it gets worse then come back. I’m like what kind of BS advice is this? You don’t understand.
My parents are positive. They did an X-ray and they already saw that my left side of my lungs is compromised. How can you just tell me to go home? My breathing is getting worse. He’s like, you look fine. I was like you’re just basing this on appearances – just being so frustrated.
They took your vitals and suggested sending you home
He was like, okay, we’ll do some vitals on you, check your oxygen levels, your blood pressure. Then they were like everything’s fine. You should just go home because actually you’re going to be way worse off here. There are people here who actually have coronavirus and you can get it. We want you out of here so you don’t get sick from something even worse.
He kept trying to convince me that I didn’t have it. I’m like, that’s so crazy. Cause if my parents have it and I told you I was traveling how could you possibly deny me even a test? So I was just feeling really frustrated.
My urgent care doctor, the one that I saw Friday who gave me a cell phone number, he’s kind of been a hero throughout all this to call me. He’s like, I think we should bring you back in and do some more labs. We’ll do the X-rays, run the labs again, we’ll see how it’s going. And then as soon as he hung up and after the ER nurse did all her stuff, that same ER doctor came back in and he’s like we’ll run some labs. Something changed his mind.
What tests did they give you?
He was like yeah, we’ll run some labs, we’ll do your blood work, we’ll do a full blood panel and we’ll do another X-ray .
The nurses had to put full protective gear on each time they entered your room
I noticed that every time the nurses came in they were wearing full hazmat suits. I don’t even know what you would call it, it’s called, if you really call it a hazmat suit, but a full body cover and goggle and mask.
Every time they came in they would suit up. It would take them minutes to suit up. And then as soon as they left, I saw they had a changing room with a window. They would take it off, throw it away, they throw away the goggles, they look like they are brand new. Threw everything away. The shoe covers.
Finally they came in and they did my X-ray.

You ended up getting two sets of X-rays taken
They came in and they’re like, actually what we see is that it’s on the right side of your lungs. I’m like that’s so interesting because earlier they said it was the left side.
They said maybe the doctor just saw it wrong, just got it wrong. He said left when you’re looking at the right.
Is it more likely that it just spread? They’re like well it’s possible, but it’s not likely. So they said let’s do another set of X-rays.
At this point, I’m thinking what the hell is going on? So they came back and they brought the X-ray machine to me. I didn’t even have to get up. They literally brought in this huge machine. They did another X-ray.
I waited another couple of hours and they came back. They said actually it’s spread to both sides [of your lungs] now. They said it so matter of fact and normal.
Both sides of my lungs now have what appeared to be ground glass is how they called it.
It was caused by pneumonia. So COVID can cause pneumonia in moderate to severe cases. And it turned out that I had a pretty moderate to severe case.
You had dealt with a lot of different medical opinions up to this point
This all happened on Sunday. It was just a lot of waiting around. People telling me:
– I don’t have anything
– I’ll give you labs.
– It’s on my left side [of my lungs]
– It’s on both sides
It was just so much back and forth. It felt nobody really knew it was going on and they’re almost in denial that I had it. It’s they didn’t want another case to deal with and they just, honestly at that point they hadn’t seen anyone really my age who had it and that really terrified me, personally.
Hospitalization
The decision was to keep you for observation
COVID actually gave me pneumonia and it actually compromised my breathing. At that point, they’re like okay, we will give you a COVID swab. We’re going to keep you here and we’re going to check you in as an inpatient. So they kept me in the ER room for another four to six hours after.
They transferred me into what was called an observation room where they keep you, if they expect to observe you for just up to 48 hours.
They thought we’ll watch you for 48 hours, see if it gets worse. If it does, then we’ll keep you as an inpatient, in which case you go to a different room. But otherwise if you get better then you go home.
Describe the 48 hours in the observation room
A series of different doctors came by. They were very kind. The one on the first night told me that they’re responding to their patients who are there for COVID, as well. One of them was actually 37. The doctor told me that he was very, very sick for two days and then they gave him the clinical drug called remdesivir and then he got better and went home. He said, so you should be fine, you’re young.
Stanford has a lot of resources. It was a nice room. You have your own room, bathroom, shower, TV and you could call for food and they bring it to you anytime.
How was the healthcare staff – the doctors, the nurses?
Every nurse is different. Some nurses, they made me feel a human, they were telling me stories about their kids. They would come and chat with me and they ask how he’s feeling. they would just make jokes and I felt like, okay, I feel I can get through this.
Some nurses were like we’re not supposed to be in here for very long to minimize contact. If you want something, please ask for it all at once so we can just cluster it.

I realized that the reason why they were doing that was for a good reason – for their own safety, but also because they were trying to save the PPE personal protective gear. Because every time they came in they had a suit up. It was literally protective gear for their shoes, a full body suit, goggles. Every time that they left they would throw all of it away. Even if it was for a five minute temperature check and blood pressure check, they would throw it all away.
So I felt really bad. I tried not to call them very much. It was me in the room for pretty much most of the day, maybe someone coming in every six hours to give me Tylenol because my fever at that point was just raging. It was a raging, raging fever.
Describe your symptoms, including the fevers
I would be so freezing cold. They kept bringing me sheets that were just freshly pressed and hot and some nurses were so kind, they would wrap it up on your body. It felt so warm and immediately after it’d be sweating buckets.
It was so crazy. Also they saw from the blood panel that my liver was inflamed. So they wouldn’t give me Tylenol less than six hours apart because that would make my liver even more compromised. So on top of all that, there was this liver problem.
I was very horrified. I was like I don’t even care if my liver is compromised. I don’t want the fever to be affecting me the way it was because it was just the worst feeling. I really felt I was in hell because I had this fever that was just raging. My parents, I don’t even know what the hell was happening with them. I didn’t bring a charger. So I had no way of understanding what was going on in my family. Can’t talk to anyone. I didn’t even learn until much later that there was a landline that I could use.
All this time my breathing was getting worse. I was kind of timing it. When I drove to the hospital, I could do shallow breathing up to three seconds. Right at that 3 seconds was hard. It was all shallow breathing, but my oxygen level was still at 97%, which is what they wanted it to be.
It was all shallow breathing. I just couldn’t do any kind of deep breathing at all. And it was really scary, because I’ve had a panic attack before. The way that for people to kind of manage that is to do deep breathing. But I couldn’t even do that. I would turn on the TV, just try to lose myself and watch some stupid stuff they had on TV. I remember they were showing a whole day of programming on native Americans. It was very moving. I tried to draw myself out of my own misery and tried to think about, wow, there’s this whole history of people that suffered in this country because all these horrible decisions made by all these other people.
I was just trying to really think about lessons that can be learned, from that as well as the lessons that we’re learning now from COVID. There’s a lot of tie ins. I was just trying to think of a bigger picture and that really helped me to calm down.
Medical staff = heroes
There’s this one male nurse that came in and it wasn’t even clear who he was. He just came in because I think he could tell that I was freaking out. He geared up and he just came in and said, Hey, I just want to tell you, stop watching news and don’t panic and don’t even think too much about what the doctors tell you.
I know they told you you have ground glass in your lungs. It’s a little bit opaque and it’s compromised, you have diminished breathing because that’s what pneumonia does. There’s nothing permanent, right? You’re going to be fine. You’re young. It’s really if you’ve had a history of some kind of chronic illness that you’re actually going to be compromised.
That was the kindest thing anyone had ever done at that point. He was just telling me this to calm me down. One of many people throughout that have just been so kind to me, so many lessons about just how to manage during times like this.
I remember afterwards felt a lot better and then he gave this human touch when you were completely isolated for so long.
One doctor was so kind as well. He treated me like a human being. I was like, I’m sorry, I’m so sorry I’m exposing you to this. Are you scared about being around people like me? He said no, not at all. This is our job. you just need to stay strong. We’ll do the rest.
And he told me about how he was born at Stanford hospital and how it would work here since he was young. And I was just feeling so grateful. He was just telling these stories. I got really very emotional.
Clinical Drug Trial: Remdesivir
How did you end up on a clinical drug trial?
One evening someone came in and said there’s a clinical drug trial for something called remdesivir. It’s made locally by this company named Gilead. [The doctor told me] there’s some people who were very, very ill, very ill, who were on a respirator who took it and you saw these turnaround for them very quickly.
Of course it’s not risk-free. Everything has a risk. But I’m like, absolutely sign me up. And so at that point they say we’re going to give you an inpatient room because you’re going to be on a randomized either 5-, 10- or 15-day treatment.
How many other people were enrolled in the trial when you were on it?
They said enrolling 30 people at Stanford and about 600 worldwide in the clinical trial. Clinical trial aside, I think Stanford is just trying to make it more broadly available.
That’s when they officially gave you the coronavirus/COVID-19 test
They gave me a COVID swab, which if you haven’t gotten it, stay away. It is the worst feeling in the world. It feels like they’re putting an ice pick up your nose. They put it up both nostrils all the way up till it feels it’s hitting your brain and they pull it out and it just, it’s so painful.
How long did it take to get the coronavirus swab test results?
Long story short is they had actually wasted several tests on me because they took it and for some reason they got lost. They never got the results back. And so they’re like, okay, these are precious. We can’t waste them anymore. We just need to confirm that you actually have this cause until it’s confirmed we can’t give you a clinical trial.
And so they did a test, they accelerated the results and I got it back within something like six hours.
You moved rooms and met a new doctor for the trial
They moved me to a new room. It was a nice room, just you have your own bed, you have a bathroom and all that stuff.
I remember at this point there was a new doctor and she was just so competent, so kind. And also the infectious diseases doctor, the one who is administering the clinical trial, came in and talked to me every day. He would come in and just see how I was doing. He would shake my hand, his hands were gloved, but he would make close contact and tell me to grip harder when I had my strength back. And he was such a kind man.
How did he describe the trial?
It’s something you get with an IV. He said that there’s three randomized Groups A, B, or C where you either get a 5-day clinical trial of the drug or the second group would be 10 to 15 days. And the third group would be something where you just get their standardized care.
I was part of Group A and I got the 5-day trial drug and then he said that it’s not guaranteed to work first of all, but second of all, there’s nausea, vomiting, diarrhea, all those wonderful things were part of the side effects.
Describe the drug infusion
The clinical drug was administered once a day, it was a small packet of liquid that would be transferred in a half hour. They put the IV into my forearm. It could be anywhere, they were trying to find a good vein but for me that was the only place they could find. It would take 30 minutes to drip through. The impact I felt was almost immediate.
I remember after it had run its course, maybe 10 minutes after, my fever hit a very all time high. It was when I hit the 103. It was maybe a little bit above. I was hallucinating. I literally had this crazy dream, I don’t even know. It felt like it happened.
Describe the “crazy dream”
I had this dream, Jean-Claude Van Damme was literally killing the viruses. He was hand knifing them, splitting them open, doing the splits and kicking them. I was fighting alongside him. It was the craziest thing. And I remember one point, I was so hot, I was so exhausted. I’m like stop fighting! He’s like we have to keep fighting – there’s more of them!
At some point I kept calling the nurse and I kept pushing the button and they came in the room, I’m still pushing it. They’re like why are you doing that? I told them because was my fever was so high. And they realized okay, we need to give her some Tylenol because this is crazy. I said I didn’t have any Tylenol because it was affecting my liver.
Recovery (with Remdesivir)

Recovery in the Hospital
Your fever broke after the first infusion
[After the remdesivir infusion] the nurses covered my body with ice packs. An hour later the ice packs all melted. But at that point, my fever went down to 99.9. Then I remember that was the turning point because thereafter my fever stayed below a hundred for the next three to four days.
That’s why I feel so hopeful about the future for everyone else.
I can only speak from my experience. Within that same evening that I got the full transfusion, I had that crazy dream where I was hallucinating. I felt it was really helping my body to fight off the infection because 10 to 30 minutes afterwards, my fever really raged. It really got up to a high point. My body was just fighting it over the next few hours.
My fever had never been more than a low-grade fever. It hovered between 100.3 and 100.7 which is what the doctor said was classic COVID – you have a low-grade fever. Every time they came in it was always between 100.3 and 100.7, I was on Tylenol.
When I was on remdesivir it got up to 103 and I think it was because my body was okay, let’s do this, let’s fight this thing out once and for all. That happened after my first clinical trial drug experience.
I kept getting it around the same time, around 5 o’clock until I went through my entire clinical trial drug treatment.
After the fever subsided, what were the other side effects?
The chills, the aches, the night sweats were all related to the fever so those all went away. That was a huge amount of progress because at that point I had had it for over a week. I felt so much better and just knowing that okay, maybe I could do this. I think I’m going to be fine.
That was the first time I really thought okay, I think I can beat this. The part that was scary though is my breathing hadn’t changed. It was still really hard to do more than three seconds, any more than three seconds of breathing. So it was all still very shallow.
Describe the shallow breathing
I couldn’t take a deep breath at all if I tried to. I felt I had to cough. It felt like my lungs were going to collapse if I tried to breathe, take a deep breath.
When I say shallow breathing, I couldn’t breathe in for more than three to four seconds.
But my dad could not even do that. When he was on the oxygen machine, he was low. Stanford says they want to see above 93%. That’s what they consider to be good. Mine was always at 97%.
Eating became top priority
This is actually pretty important. The doctor told me my only job was to eat half of what was on my plate, if not all of it. She said your body needs to get proteins. Proteins create enzymes. I had to eat all the food on my plate. So even if you don’t want to eat, you need to. Not eating is actually going to hurt your immune system so you need to keep your body going. You have to eat food, you have to keep your digestive system going, keep eating even if your fever’s going and you don’t want to.
I wasn’t doing that that first week I had it so I remember I would force myself to eat. It wasn’t a pleasant process but I remember the day after I got the first treatment I was starving. I ordered orange juice, two bowls of oatmeal, a whole bunch of food for lunch and dinner. I remember feeling okay this is good my appetite is back.

What’s your advice on dealing with nausea and keeping food down?
Everyone’s going to have a different experience but for me, ordering the same thing for every meal helped me. Planning it out, having your routine. Every morning I would order oatmeal and drink orange juice. The orange juice was very helpful against the nausea and the oatmeal was very bland so it was easier to keep it down. I had the nausea before the clinical trial.
What helped you manage your breathing?
I couldn’t do anything but shallow breathing for almost two weeks. But that really was what it was. Sometimes you don’t even realize you’re doing shallow breathing. When you realize you’re doing shallow breathing is when you start to panic. It’s like I can’t take a deep breath. I trained myself to not think about it.
[The medical staff] told me my homework was to just get up and walk around. Don’t just lie in bed all day, get up. They told me when I ate a meal, don’t lie in bed and eat it, sit up, sit in a chair and eat it. Your lungs expand.
That’s probably something important to know. Maybe for people it’s to sit up with your back really straight. When you’re done eating, don’t just go lie down, walk around. Just try to get exercise.
So I would just pace around the room. That was pretty much what it was over the next three days of me being on the clinical trial.

How did you recover and reconnect with family?
I was slowly able to get up. I was able to walk around. I remember looking out the window and just seeing the first signs of spring. They had a beautiful garden with all these tulips that I was looking at.
And I remember just feeling very overwhelmed by how beautiful it all was. And how flowers are so beautiful. They don’t live very long.
And I was just thinking about how that’s very similar to the human experience. You have your peak and then it goes down after that. So you just have to enjoy every moment. I was having all these thoughts.
At that point I also learned I had a landline, so I was able to finally call my parents. That’s when I learned, my dad had gone to the hospital, my mom was home, she’s terrified, just calling my husband and him saying he had fever symptoms as well. But the kids luckily didn’t have any.
It was just too much to think about. So I remember being like, just one step at a time. The doctor, not the infectious disease doctor, the other one that I had gone after I checked into the inpatient room, she was so kind and called my mom. My mom called my husband every day. just to see how they were doing and checking in on them. And so I felt very good about that.
Remdesivir was a successful drug for you
I can only speak from my own experience, but I thought that was an incredibly powerful [medication]. And I just feel that [medication] could be the one to save people. It’s all because they were telling me not only about my own experience. They’re telling me about other people who have taken it.
There was somebody who was very, very sick for two days, very sick – worse than me. And then they took it and then they were able to go home shortly after. So I feel it was something that was not only helping me, but it was helping other people.
It’s in clinical trial so not widely available. You were one of the lucky ones.
It’s not that easy to get remdesivir apparently at other hospitals. Cause my poor dad, who I infected, was at Washington hospital in Fremont and they gave him hydroxychloroquine which you may have heard about in the news. It is something that is used to treat malaria. It’s something you take orally. I told him he should ask them for remdesivir and then my mom told it to the nurse.
My dad was on a ventilator so he wasn’t really able to do a lot of communicating on his own. So my mom told the nurse and they said that’s a last resort. We don’t just give that out. And so I realized that Stanford is a very well-resourced hospital. A lot of places are not just gonna give it to you. I’m feeling very sad at that point, but really thankful for my own experience.
Availability of remdesivir
I’m jumping timelines but after I was discharged, the research coordinator who was working for the infectious diseases doctor called me to check up on how I was doing. I gave her all the details, I was feeling a lot better.
I asked is this going to be more broadly available? She said this is still a clinical drug trial but everyone we’ve given it to has had a similar reaction to you which is that they’ve gotten better quickly. It turned a lot of cases that were severe into moderate to mild ones pretty quickly.
Everyone who’s coming to Stanford, we’re giving it to people, not just people with COVID, it covers a broad range of cases. You don’t just have to necessarily be testing positive. It could be even if you haven’t gotten your positive test back, we might be able to give it to you and do something about it because they’ve seen it make such a big difference.
I felt very good about that. That there’s a [drug] at least I know personally that worked for me, sounds it’s working for other people, that you can get this broadly at Stanford.
How did they make the decision to discharge you from the hospital?
They discharged me that day because they felt they also saw a lot of progress. They don’t need to just keep coming every day to take my temperature and to throw out their PPE. I have COVID, but I can go home and I can self-manage. I could be an outpatient. They said they would just call me and every day check in. So they gave me some paperwork to fill out.
Quarantine at Home
How long was the recovery and then the self-quarantine?
Three weeks for recovery. And actually the three weeks was something that I had to kind of push for cause at first the nurse said two weeks and I’m like, ah, I feel I need more than that because two weeks doesn’t feel like enough time, it just flies by. She’s like, okay, I can write three weeks. And if anything, if I feel better, I can always go back earlier. But I would at least have the room for three weeks.
The quarantine was for two weeks after my last symptoms disappeared. So I’m still in quarantine right now.
When do they consider it to be the last day of symptoms?
It would be the day when my breathing got back to normal cause that’s still a symptom. My breathing was not back to normal when I left, almost the same as it was when I came in.
I know for a fact the entire time the oxygen machine attached to my finger never dropped below 97%. And even though it was shallow breathing, [I didn’t] need to just be [at the hospital].
When did your breathing normalize?
[The breathing recovery] felt slow but it was very fast because I remember when I got home it was March 19th the first day of spring. I love fall and thought it was the best season of the year. But now I like spring as the best season of the year because that was the day I got a second chance at life after discharge.
I was driving home. There were signs of spring everywhere. All these things, all these beautiful flowers and things are brought to life. And so I really liked that.
The 19th is when I was discharged. That was Thursday. By Saturday, I was counting the seconds. It was going up to four seconds, five, and slowly I could feel like I was able to [breathe] again.
I felt it was slow because all of Thursday, all of Friday, I was like I can’t even easily just take a deep breath or walk without feeling winded. But by that Saturday I was like, okay, this is getting a lot better.
What were the official instructions for self-quarantine?
They told me that I have to be by myself in a unit with my own bathroom. You shouldn’t be sharing a bathroom with other people. And I was thinking it’s probably hard for a lot of people.
They said you need to be in your own room. No one should be in there for any reason at all. The way that they were coming into the [hospital] room with the full body protective gear, throwing it away. They said it shouldn’t be any different for anyone coming in to see you.
So I went back to the guest house. My husband was not anywhere near me. The kids would come and look in the window and see me, but that was it. Through the window.
The door has a big window and so they would just come and say hi. But I locked the doors so they couldn’t come in. I ordered food every day. I was in no shape to cook. You wash your clothes separately. And they said that I should use plastic in terms of eating. Don’t use the same silverware.
Recovering at home felt harder
I remember coming back was actually a really hard experience as well cause in the hospital you don’t have to think about anything – you’re taken care of.
If anything happened, the machine would start beeping. People would bring food for you. They would check your temperature. You didn’t have to deal with real life coming back, seeing the kids, knowing they’re out of school, knowing my dad’s in the hospital. Knowing that I’m not at work right now and I’m managing these people who have no idea what the hell they’re supposed to do.
But I remember before I left the hospital, I wrote down on my iPhone some lessons that I learned. And I remember just being very true to myself, being like I’m not going to forget this.
How did the medical staff check up on you when you were at home?
A discharge nurse would call me and she was just kinda checking. I was in outpatient care. So she called me twice. She checked on my breathing, she asked me if I had any questions. She asked if I wanted to talk to the infectious diseases doctor about the clinical trial but I didn’t really have any questions. It was a very short call.
The city also checked in with you
The day I got back, I remember someone from the city of Palo Alto called because they saw my COVID test. They said they were calling everyone who had a positive test just to document where they’re living, their address. I don’t know why, just to know which houses, maybe they’re gonna put a big black X on my house!
They called me and they asked me a bunch of details. I gave them all the information. I asked why are you asking for this information? They said we just need to document how bad it was in our own county.
Taking care of mental health is so important
A bit of an aside, I felt really guilty. I even had nightmares when I came home about work and I was having calls and I needed to be productive. And so I literally woke up, I was like, I’m going to call my boss and tell him I’m better and I can work from home.
I’m seeing a therapist. She told me three weeks sounded like not very much time at all. She said you need to not feel guilty about this. You’ve earned the right to take time off after something like this.
She said your homework is to not feel guilty. She gave me a series of exercises on how to manage the anxiety and the guilt over this. I was feeling really guilty about not being at work and being productive.
So over the past week, I’m actually managing a lot better and just allowing myself to take this time off. No one’s giving me a hard time. A lot of people are just very sympathetic. I think they’re just trying not to overwhelm me.
Dad’s Severe Case of Coronavirus
Your parents are both in the higher risk group
My mom and dad are both over 60. My dad has serious heart problems that he’s been managing with the help of a lot of drugs. He sees a cardiologist regularly. My mom is pre-diabetic, so they’re right in that group.
Where did they get the COVID swab?
They got the COVID swab that was made specifically by Stanford.
March 2nd is when I started exhibiting symptoms. On the 7th is when my parents got tested. And then I think on the 12th is when they got the results back. So it was five days. They were confirmed to have coronavirus. So at that point, my dad, uh, was at home. He didn’t go to the hospital yet. He went to the hospital there shortly afterwards because of the 103 fever.
Describe the Stanford COVID testing clinic
They went to Stanford hospital. Stanford is actually making their own tests and so they’re able to do it a bit more liberally. But they won’t just give it to you either. Someone there told me that they ran out of one of the chemicals needed to make the test and so they were running short, themselves.
But they had a COVID clinic right outside. There was a pretty long line. So my parents went late at night on Saturday because at that point they were both exhibiting symptoms.
They were both just worried. And so they said they would give them a test but they had to wait in line. So they just waited in the car cause it was very windy. By the time I called them, they actually put them in an ER room because my mom was saying she was feeling tightness in her chest. And my dad already had all these publicly documented cause he’s been to Stanford before, so they brought them into an emergency room. They were there for five hours. He left at 5:00 AM.
My dad, they did the full blood tests. They did an X Ray. Their lungs were clean and so they didn’t have any issues like the ones that I had, but they were showing the classic coronavirus blood work results, which is your white and red blood cells are very low. And one protein was very high.
So even though they didn’t get the test back, they were like you guys have it, you need to go home and you need to quarantine with all the same instructions that I just shared with you. You need to have your own bathroom. Do not go anywhere, for as long as it takes.
How did your dad end up in the hospital?
My mom called 9-1-1 and told them that they had to take him to the hospital and they actually didn’t want him there. They were like it’s just a fever. He’s okay to just continue to stay at a home as an outpatient. But she’s like you don’t understand. He has bad heart problems. He has a really high fever – it was 103 at that point. I, after having gone through myself and know how bad that was, can’t believe they didn’t want to take him in. But my mom was insistent on taking him.
So he went to Washington hospital and when they checked his breathing, they were really worried because he was only getting 88% oxygen on his own. When they put him on a ventilator and they gave him oxygen, he was only at 90 to 92% at any given time. That’s still below that 93%. I heard that’s what Stanford wanted.
Your dad took hydroxychloroquine instead of remdesivir
They were very concerned and they gave him hydroxychloroquine. They said they did have remdesivir there but they said that’s only a last resort. I’m not sure why. Maybe they don’t have a lot of it but they never gave it to him at any point, which I think was really a shame. I think that would’ve helped a lot because it helped me.
Hydroxychloroquine is something you take orally and it didn’t seem it had an immediate effect. But over the course of his four-day stay at the hospital, he seemed to be getting better and he actually was discharged. He came home and he’s been doing well ever since.
When he left, he was breathing at about 93% on his own, which is actually still very scary if you think about it. But he really wanted to come home. He didn’t want to be in the hospital and the doctors felt he was doing better to at least be an outpatient.
Your dad’s coronavirus case was classified as severe
My dad had a severe case. Luckily he’s fine now, but he had to be on a ventilator. He was at 88% oxygen level. That’s considered pretty critical. And so they put him on an oxygen machine.
Even on the ventilator, he was only hitting 90, 92. So that was really scary. That’s a totally different story than me. I was able to do shallow breathing the whole time and I was able to get enough oxygen to keep it at a good level.
What was his hospital experience?
His hospital was a way worse experience. The nurses were not very helpful. They didn’t share information freely. We were trying to get him transferred up to Stanford and they said they would start the paperwork. They never did it during his stay and so it was not a good experience.
It was very different [from mine]. They wouldn’t give him the remdesivir even though they had it. They said it was a last resort, which I don’t understand because he had what they classified a severe case. I’m so grateful that he’s okay now he’s at home and he’s breathing, he’s walking around.
How did they self-quarantine?
They’re on two different floors. They’re not sharing silverware and all that stuff. They are sleeping in their own rooms and they have their own bathroom, but they’re definitely sharing a common eating space.
They got a call from their county
Someone called them from Alameda County the same way that Palo Alto called me and they said that they would have someone come by to check on them to make sure that they actually didn’t leave the house because they had to be quarantined. They got that call a couple of days after they got the positive test, which was on that Thursday the 12th.
Final Thoughts
Keeping some humor
I remember there was some humor too. [At Stanford] at some point they brought in an old charger they got from lost and found. And I finally looked at the news. In Santa Clara County. There’s been 26 more cases of confirmed coronavirus.
And I realized that my parents were two of the 26 because they got tested at Stanford. I’m like oh my gosh, they’re statistics! My mom was even joking about it and she’s like everything we do is so dramatic. So we were still trying to find some humor in it.
What are you walking out of this with?
What I’m coming out of this with is not a criticism of anyone. I’m walking out of this with so much gratitude because so many people I met at the hospital from the doctors who were caring for me to the very first doctor who thought I had it, called me everyday and gave me his cell phone number, to the nurses who treated me I was a human being, risked their lives everyday coming in, potentially exposing themselves.
I have nothing but gratitude for them. I feel there’s nothing they could have done any differently. They’re doing the absolute best they can. This is probably a shock to their system to have to care for someone who has this virus, someone at my age, who’s getting it at a pretty moderate to severe level.
How would you have managed this experience differently?
I would have taken it a lot easier on myself.
I know a lot of people in this day and age in Silicon Valley and all over the world really push themselves to do their best, to put their best foot forward and prove they add value and all these things.
But you need to put your health first. If you’re seeing all these signals: you have a fever, you’re not breathing right. Even if it isn’t coronavirus, you need to put your health first. I’m pretty sure pushing myself that hard made it all that much worse.
he hard way. If something were to happen to me, my company will continue to go on. Whatever goals other people have, they’ll find someone else to do it. But my children only get this one mother. I only have this one life to live. Why would I put myself on the line for something like that? You need to put your health first. It’s the only life that you have.
You enter this world with nothing. You leave with nothing. Everything else in between is just an experience. You just have to have gratitude for the entire thing. I would have had more faith that I was going to be okay. The entire e time I was going to be horrified I was going to have to say goodbye to my children. I had all these crazy thoughts of what’s going to happen to my daughter after this experience? She’s not going to have a mom, she’s so attached to me. I was thinking all these crazy thoughts. I wish I had more faith that I was going to be okay.
I wish I had more respect for my body growing up. Like a lot of people in life, I always had a very hard time with body image. In the end my body is what saved me. It kicked this virus out of its system. After everything it has been through, it still did that for me.
I’m just so grateful for the fact that my body can do all these things. I’m never going to mistreat it again. Never look upon it as anything other than this amazing miracle – children came from it, I was able to beat this virus from it, it’s a miracle.
That’s something I will do differently, wish I had done differently and will continue to do differently: just respect my body and love it the way it is because it went through so much this week and got through it. Even my dad in the state of his health, he got through it. Our bodies keep fighting for us. We just have to get out of the way.
What’s your message to people who still aren’t convinced about the seriousness of coronavirus?
A lot of people are not taking coronavirus more seriously. When I go walking in the yard, I see a lot of people walking around. When my husband went to take the kids for a walk on Sunday, the Palo Alto farmers market is still open, people are flooding it and buying all these things.
It doesn’t seem a big deal because a lot of people get it and they’re asymptomatic but a lot of people I went on the trip with, none of them have stepped forward and said they have coronavirus probably because they’re asymptomatic. Everyone’s telling me everyone’s freaking out, wish people would stop panicking, stop hoarding.
Well I almost don’t blame people for trying to stock up on things because after having gone through this, it is a big fucking deal. I gave it to my whole family! I couldn’t breathe more than just shallow breaths for almost 2 weeks. I had a fever for 10 days. That is crazy. I’m considered a young person and I got it, and gave it to my whole family. Can you imagine if you got it and gave it to your whole family? It is a big deal. Just because you’re asymptomatic doesn’t mean other people will be.
We should all stay calm, but you shouldn’t judge people for feeling panic either because it is actually a big deal. You don’t want to go through it.
I actually thought I was going to die. My dad was in the hospital. I didn’t know what was going to happen to him. I gave it to my husband who was watching my children. It is a really serious thing. People should really stay home. Just because you’re not showing it doesn’t mean you don’t have it and you can’t give it to someone who takes it worse. That’s one thing they told me – everyone reacts to it differently.
I was thinking why am I in my 30s and why do I have this? Everyone reacts differently. Someone could be completely asymptomatic and the next person could get it. There are people in their 20s and 30s who get it. Don’t assume because you don’t have it bad that other people won’t. My husband did not have anything other than a bit of a fever one day then it went away. He’s older than me – 6 years older, so he’s 43.
Just because it’s not a big deal for you doesn’t mean it’s not a big deal for someone else.
I hope this experience can show other people that actually it is very scary. You could be relatively young and get it. I had what they called a moderate to severe case. Otherwise a healthy person, I don’t smoke, I don’t have asthma, no chronic issues, but it still affected me pretty badly. I had access to a very good hospital system that gave me this drug that helped but not everyone’s going to have access to that.
Coronavirus Stories
Justin Wilhite
Infection: Community spread
Home: Sacramento Area
1st Symptoms: Persistent headache (resistent to Tylenol + OTC medications), chest pains
COVID-19 Test: Not taken
Case: Moderate
Treatment: Tamiflu, OTC medications
Status: Recovered
...
Tina Baker’s Story Pt. 1 (Diagnosis & Treatment)
Infection: Work trip to London
Home: Palo Alto, CA
1st Symptoms: Sore throat, major fatigue
COVID-19 Test: Positive
Case: Moderate to severe
Treatment: Clinical Drug Trial (Remdesivir)
Status: Recovered, back to work (from home)
...