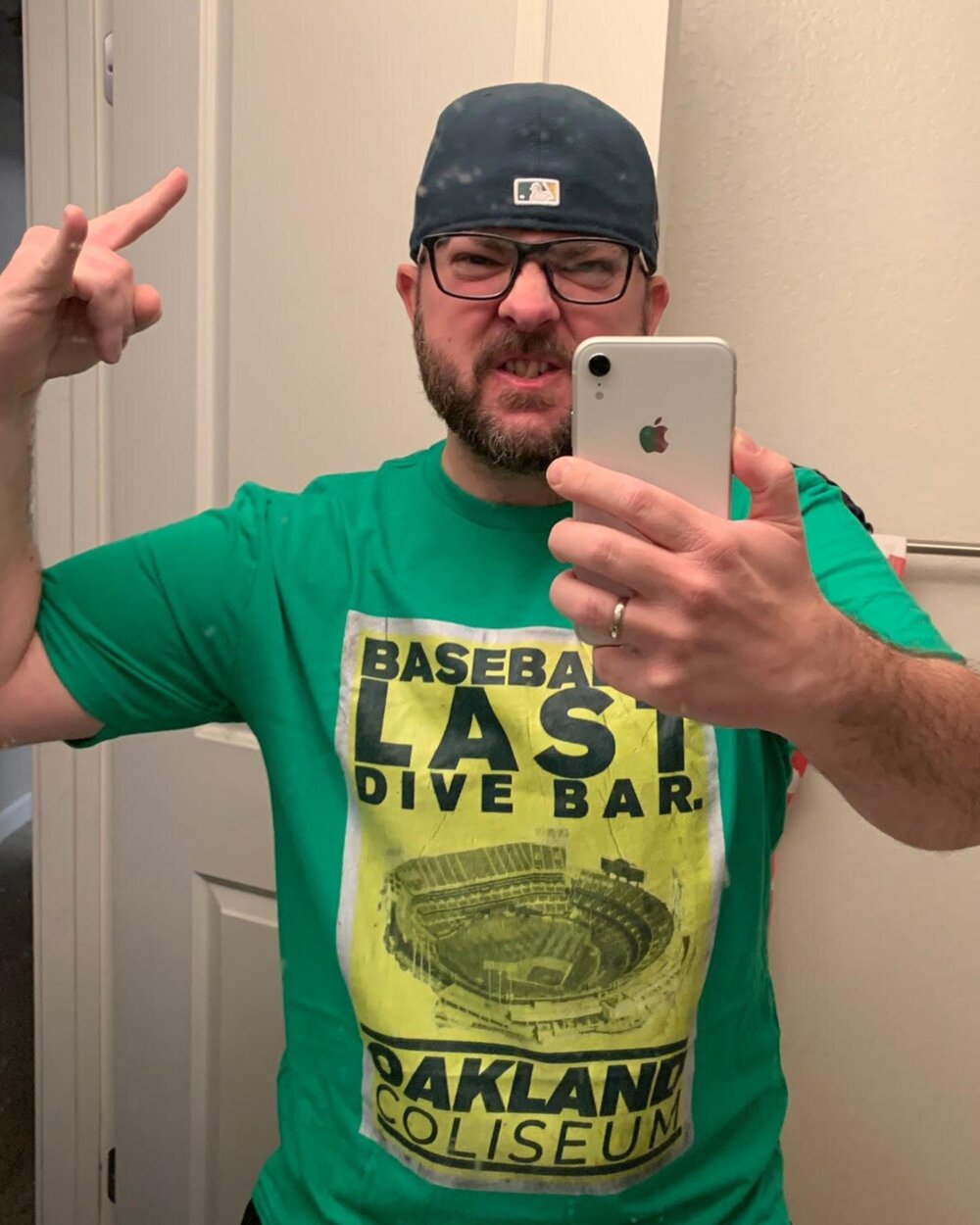
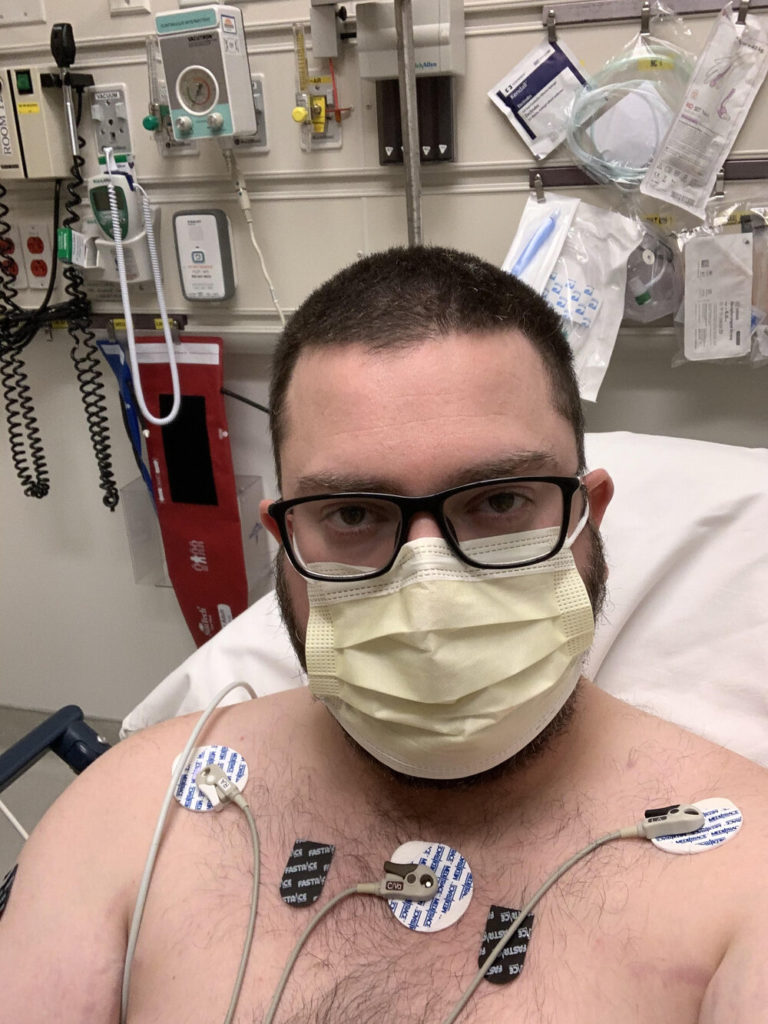
Justin’s Moderate COVID-19 Story
Listen to what your body says because so many times, we just put our heads down, grind on and we continue working or charging through our day
Justin Wilhite
Fast Facts
- Diagnosis:
- Likely* COVID-19 or novel coronavirus
- *No official COVID swab or test taken
- 1st Symptoms:
- Persistent headache immune to any medication
- Dry cough
- Fatigue
- Chest discomfort (lung area)
- Pain when breathing
- Easily out of breath
- Treatment:
- Tamiflu
- OTC medication
- Inhaler
- Status:
- Recovered
- Diagnosis
- Getting Medical Treatment
- When did you go to the hospital?
- How did your first doctor appointment go?
- What medication(s) did they give you?
- What effect did the medication have on your symptoms?
- You ended up back at the ER
- Did you ever get a fever?
- Safety protocols had drastically changed the second time at the ER/hospital
- Did you ever get a COVID-19 test?
- Describe the prednisone (steroid) prescribed to you
- How long were the ER stays?
- How were your oxygen levels?
- How did they classify your case?
- Isolation at Home
- Type 1 Diabetic Perspective
- Helping Others
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
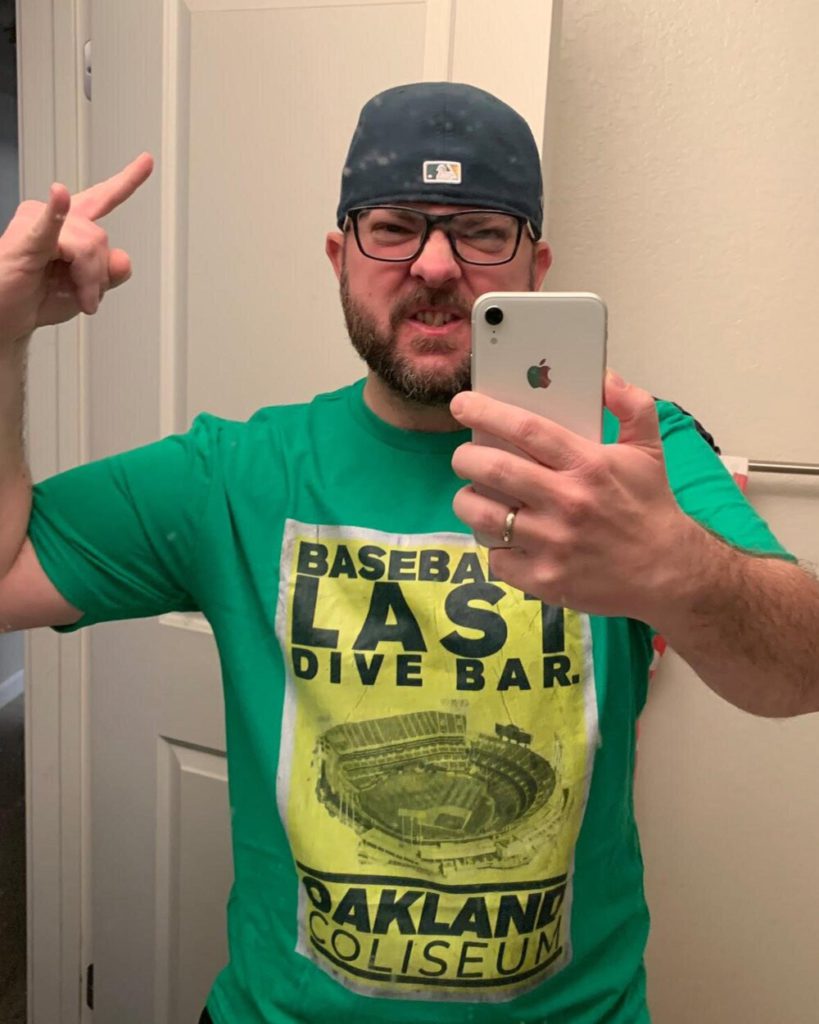
The very first day I felt symptoms was March 4 and it started off with an all-over-the-head headache.
It’s a strange headache because it’s literally all over your head. It’s your forehead, it’s on top of your head. It’s behind your head and your temples and a little bit on the neck. It was all over. It was instant. It wasn’t terrible, but it was noticeable.
Then later that evening, I could feel my lungs as I was breathing, and [pain] started between nipple to nipple and it was like a straight line. That’s what I felt for about a week was just a straight line of discomfort. It hurt in that direct area so it was about an inch, inch-and-a-half. The only way to say it is between my nipples. That’s the only place that hurt – right in that area. It was discomfort on the 4th.
Progressively between the 4th and the 11th, it started to hurt upon breathing, inhale and exhale. Then by the 13th it hurt all over. So it had spread to my whole lungs, from the very top of your lungs up here by your collarbone to the very bottom, down at the bottom of your ribcage and all the way to the back near your spine.
So on inhalation my lungs would hurt and then exhale, they would hurt. And it ended up being the whole lung. And then between the 13th and the 16th, the pain was just worse.
Describe the sharp pains you felt while breathing
I liken it to having pneumonia. Going outside when it’s cold, and taking a deep breath. It would be like that, but double, triple that that sort of pain is the best way to describe it. It’s very uncomfortable, painful, and nothing makes it better.
That’s the only thing I can liken it to because it’s such an odd feeling. It’s not a natural feeling. And it’s nothing you get with the flu, or a cold or a respiratory infection, or even bronchitis because most of those are generally bacterial.
Describe the cough
Everything was dry, I’d have a dry cough And there was no phlegm when you inhale and exhale because with with asthma or any one of those bacterial infections of your lungs that I described, there’s a rattle. The lungs were angry and inflamed. And there’s nothing else that I know of that is like the symptoms of breathing with this coronavirus.
Laundry list all the symptoms
The first day that I had symptoms, it started as a lung discomfort. The feeling of [pain for] an inch and a half line between my chest and my nipples. It stayed like that until the 11th. I knew something was wrong with me because it began to hurt when I breathed.
It was the all-over headache and that started in the morning. I noticed it and it was a really odd headache. So I took a Tylenol and didn’t get rid of it. That would be the story of the entire 29 days.
I’ve had symptoms of COVID-19 and nothing really helps with the symptoms. Whether it’s the breathing or the headache, nothing degrades the effect upon your body. So you literally just have to deal. And that’s probably the worst thing about it because, you know, we’re all used to taking pills, cough syrups or whatever, when we’re sick to alleviate our symptoms.
With this, there’s nothing. There’s nothing that alleviates the symptoms. Tylenol is almost a waste of time. And with me, Motrin or ibuprofen made it worse. And you can’t take any sort of powerful painkillers, because most of those are opioids, and opioids degrade your breathing. When you’re already having trouble breathing, you don’t want to end that mess on top of it.
Shortness of breath pretty much at all times. The shortness of breath upon exertion is something up until very recently I was dealing with and so I couldn’t walk 10 feet without feeling like I sprinted across the street. I likened it to running a marathon. I’ve never run one but you see how exhausted people are at the end of those. And that’s how I would be walking the 10, 20 feet from my bedroom, to the bathroom or from the bedroom to the couch and I would just need five minutes to catch my breath.
When you move it’s terrible, no energy. So a high degree of lethargy which saps your will, if that makes sense. It just takes your energy from you. There’s a difference between being sick and having energy and being sick and feeling like this might be it and this is one of those feelings that this might be it because there was no energy. I’m short of breath upon doing anything – sitting up in bed, talking, walking to the bathroom to the couch, eating. And that’s that’s pretty much it for me.
When did you first contact a doctor?
My wife and I emailed our physician. He was out of town. So a backup physician emailed us a form letter describing COVID symptoms.
The 13th comes around and now it hurts all over my lungs or hurts to breathe, inhale, exhale, the headache is non-stop, it’s 24-7, and it’s all over your head. 24-7.
Nothing gets rid of it. Not laying down. Nothing gets rid of the lung pain you can’t lay down, you can’t stand up and then on top of it and prevalent almost from the beginning is shortness of breath upon exertion.
When did the shortness of breath worsen the most?
It had started a few days prior but it wasn’t noticeable. I noticed I was just getting more tired before the headache, before anything else.
Upon reflection, do you know how you got COVID-19?
I got it in the community. That’s what the ER said. And with my own small bit of medical knowledge, that’s pretty much what I figured.
There wouldn’t be anything that I could have done differently. Because like I said, late February, early March, this was a Chinese-centric disease. And like a lot of diseases, like Ebola or something along those lines, they just sort of stay where they begin, and they don’t really infect the world. Or if they do, it’s to a much lesser degree.
Getting Medical Treatment
When did you go to the hospital?
On the 13th I was sitting on the couch watching TV and I almost passed out just sitting down. Out of nowhere. At that point, my wife was in the kitchen, cooking dinner, doing dishes after dinner or something like that.
I said I’m going to pass out and she goes, ‘Okay, that’s it. You’re going to the doctor.’ She had seen me progressively slide to ill health for the past week.
For about four months we had been talking about this because I’m part of the medical field – I’m a certified medical assistant – so stuff like this is of interest to me. About a week prior to seeing symptoms, I told her, I might have this by everything I’m feeling.
We had had discussions so then by the 13th later that evening, I said I almost passed out and that had made sense. By everything I have read coming out of China, people would walk down the street and just pass out and then they would just be on the ground. So we call the after-hours advice nurse. They set me up with an appointment.
How did your first doctor appointment go?
I went to that appointment and the doctor didn’t even really look at me. He just sent me to the emergency room. He was pretty positive based upon ‘what you’re telling me and how you look’ [so I] went to the ER and they did a whole test on me.
They drew blood work, did X-rays, looked after me and then said, we think you have the flu, but we can’t test you for the flu. And we can’t test you for COVID because those tests are for people that are dying.
I was so frustrated, my wife was frustrated. So they said, ‘Okay, if you feel worse then come in.’
What medication(s) did they give you?
They gave me an inhaler. They gave me Motrin, they gave me Tamiflu, and I took Tamiflu for two, three days. I took Motrin for about 16 hours. And because of the Cymbalta I can’t take a lot of Motrin because of the way your body metabolizes that it could affect your kidneys.
I took about 200 milligrams as a very small dose and I spread it out over over a few hours, took it three separate times. And with each time I took the Motrin I felt worse. So on my own, I stopped taking the Motrin.
What effect did the medication have on your symptoms?
All of my symptoms, my headache, my breathing, the lethargy and the shortness of breath upon walking – all of those were worse and the inhaler also hurt my lungs when I used it.
The doctor likened it to if you get a cut and you put alcohol on the cut, it burns. Well the same thing with your lungs when they’re inflamed and something is attacking them. You’ve just put medicine on your lungs, and it’s going to burn as it’s doing what it’s supposed to be doing.
So I stopped the inhaler. I stopped the Motrin after about 24 hours. And then I was still continuing the Tamiflu, but nothing was alleviating the symptoms. And this didn’t feel like any flu I had ever had because I had just recently gotten over the flu during Superbowl week. So I was pretty well aware of what the flu felt like and this was not the flu. The flu you get the body aches, you get the chills, you get the snot, you get just tired and lethargy. I think almost everybody had the flu at one point in time or another. And this wasn’t that and it so I ended up feeling worse.
You ended up back at the ER
By the 16th I went back to the ER. And if I thought I felt bad on the 13th night…
I got home later that day and I and I told my wife, I hope I make it because it doesn’t right now it doesn’t feel like I’m going to and that was one of the two times that I felt that I might die having this by how I felt.
Did you ever get a fever?
No, no fever. I felt hot. Even the two times I was at the ER and multiple times being home, I said I am so hot. Let’s take my temperature and it was always just about normal. So I always felt hot. I thought I felt hot to the touch. My wife would feel me, the ER doctors would feel me to take my temperature and say, ‘No, you’re fine.’ But I was hot.
That was my overall feeling almost the entire time – I felt hot, but I never actually had a fever. I know that there’s people that I’ve spoken to that actually were running mild fevers, and that’s the thing. It’s a mild fever. It’s 99, maybe 100.
Safety protocols had drastically changed the second time at the ER/hospital
Between the 13th and the 16th, on the 13th, my wife was able to come into the emergency room with me, go into my room and be there the entire time without a mask on. The personnel at the hospital, most of them had masks if they were in direct contact with patients, while other personnel that weren’t in direct contact with patients did not have masks.
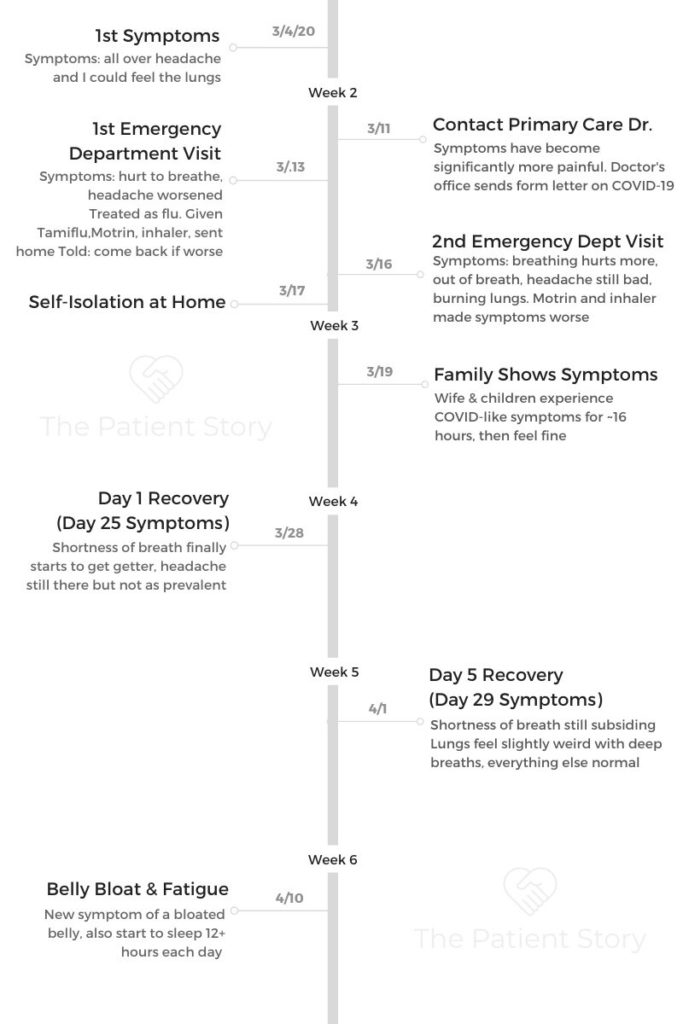
On the 16th, when we came up, my wife couldn’t even enter the hospital. So I was doing everything on my own. Every single personnel, they had booties on their shoes, they had a disposable smock on. They had a clear plastic face shield, either an N95 mask or a surgeon’s mask, goggles, and gloves. That was every single medical personnel walking around, taking paperwork, whatever that was.
The 13th when you went to the ER, I wanted to ask if people were already taking precautions when they’re seeing you. They were but it wasn’t as in depth as the 16th. On the 16th anybody would walk into my room masked.
In three days, it had completely changed. Only one person was allowed in my room at a time. And when they came in, they had to wear everything I just described.
And then they would immediately take that off and throw it away with a garbage can that was right outside the door. So life had completely changed between then and the 16th.
Did you ever get a COVID-19 test?
I never got a test because I was in front of the big wave that’s happening now. So I got sick before everybody else basically. And tests were still very rare. They were for the people that were dying, because while I was there, someone had come in and they were infected by others, and then others had come in before me and had passed away from the virus, so it was on top of everybody’s mind on the 16th not on the 13th.
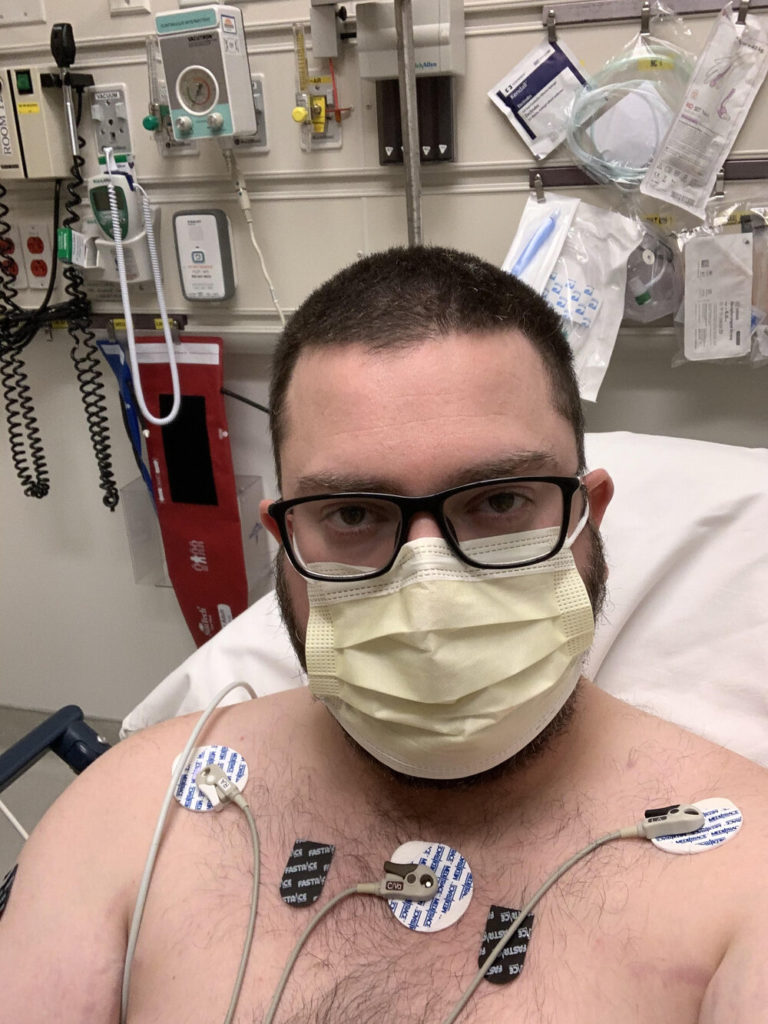
On the 13th, they did an X-ray for pneumonia and came back negative, as well as a bunch of vitals for blood work on the 16th. Oh, [there] was an EKG to make sure that there were no heart issues. Same thing on the 16th. They did an EKG, X-ray, a lot more blood work than they took on the 13th and they gave me an influenza test. All them came back negative.
I don’t have any details on the bloodwork but due to my symptoms, how sick I appeared, and how the same symptoms I had had progressed, my ER doctor was on the phone with the CDC and the infectious disease doctors. They’re at the hospital I was in.
Through the process of elimination, they were 100% positive I had the COVID-19 and we’re very confident in making that assumption based upon not having a test.
Describe the prednisone (steroid) prescribed to you
I was prescribed prednisone (steroid) to help with the lung inflammation. They gave me the prednisone at the hospital, and then they sent me home with about a five-day prescription and it seemed to help.
After about Day Two or Three being on the prednisone, I could begin to breathe without constant pain. It was still there, it was adult pain, but I could inhale and exhale without just just feeling terrible, without that weird cold feeling pneumonia kind of icy spiking pain.
How long were the ER stays?
Both nights I was probably in the ER for a total of 10 to 12 hours both times. I was probably in the ER for about six hours on the 13th and probably about six hours on the 16th. And I wasn’t there for an extended stay because my vitals were stable.
I wouldn’t have giant spikes in blood pressure or giant bottoming out in blood pressure. So they were worried about a 30 to 50 point spread either way after hours of taking my blood pressure.
How were your oxygen levels?
My oxygen was always good. The lowest my oxygen ever dipped was about 96 which is still fairly normal. So they were happy that my body seemed to be fighting it without the issues. They had seen people have the real trouble that needed oxygen and intubation.
How did they classify your case?
I had a moderate case, a serious case. The only thing I didn’t need was a hospital stay.
So both days [at the ER], my vitals were well enough that they felt okay sending me home without any serious issues. The only thing that was ever raised was my pulse. And my pulse was anywhere between 100 and 125 sitting or laying down, because I would do it myself. And there at the hospital it was all about that. That didn’t come down probably until a week-and-a-half from March 4.
Isolation at Home
What were the instructions on self-isolation at home?
We had self (isolated) a little bit prior to that, but nothing serious because remember, this is late February, early March. And at that time, it’s still a Chinese-centric disease. It had just sort of started showing up in Washington and Italy, but it wasn’t what it is now.
So we had heard about it, but what are you going to do? We still had to live life, still went shopping, we still got groceries, we still did things as a family.

But once I got back from the hospital on the 16th, that’s when they said we need you to stay home for two solid weeks. And then for me, they wanted me to stay away a couple of weeks after the symptoms had subsided.
Did your family ever experience COVID-like symptoms?
My wife and my 17-year-old and my nine-year-old, they got a quick 16-hour weird cold like thing. It came and it went.
This is why we were all quarantined (isolated). Nobody had gone outside, and they all got sick. My wife got chest pain, so we got worried about that. And then it came and went. So we’re thinking that that was their COVID symptoms.
What was the follow-up communication with your doctor?
They have changed all of the meetings with their physicians to telephone and/or FaceTime meetings. And I did have a one-on-one with him a couple days later, but he’s going off the same information that everybody else has and it’s at this point still changing daily even so far into this.
Type 1 Diabetic Perspective
Your experience as a diabetic helped you realize something was wrong many days before your symptoms got obvious
About a couple of weeks before developing symptoms, my blood sugars were spiking really high and generally that happens when I’m sick.
I couldn’t understand because I wasn’t feeling sick. So my blood sugars spiked during the day and then dropped off at night.
That’s not normal for me. For any one of your people that watches your videos and if they’re diabetic, that’s an important thing to kind of watch out for because it confused me, because I had never experienced anything like that either.
There were some days where I would eat, give myself insulin, and it would be like I didn’t give myself insulin. It didn’t make any sense and nothing was bringing [the sugar levels] down. This was a couple of weeks before I actually started having physical symptoms of the virus.
As a T1 diabetic, was there any extra concern about impact of coronavirus?
Absolutely. I was worried about it because I rarely ever get sick. I never really ever get a cold. I rarely ever get the sniffles, maybe a little bit of allergies here and there. But I don’t get sick.
But if I were to get something, I usually get things like this. So it’s just my luck. And I was worried about it, and then I ended up getting it.
Were doctors concerned about your diabetes?
I was more worried about the diabetes than any of the doctors have been.
It’s a concern because the diabetes affects all of your body systems at once. But it’s not worse than someone with asthma or COPD, or any other lung issue that someone could acquire or have.
So in terms of medical, yeah, they were worried, but it wasn’t an overall driver like if I had asthma, which I don’t or if I smoked, smoking is a huge thing. A lot of the deaths that they see are people that smoke but are overall healthy or run a lot and that’s I guess it’s just using your lungs and getting a deep down in there. But the actual diabetes itself, that wasn’t top of the mind concern for them.
Helping Others
You got a lot of attention on social media with your story. What’s been the most common question?
They’re like, ‘Hey, I had a weird headache, and I could feel my lungs, too. That’s really weird. When did that start for you?’ Or, ‘Hey, about this day or about this time – did you have these issues, too?’
I’ve always tried to be as open and honest with everyone that has questions. Somebody asked me about my blood type, because one of their family members is needing antibodies because they have it really bad. They’re hospitalized and intubated. It looks like they’re not doing well. And they were in my local area here.
But it’s usually, ‘Hey, does it feel like you have allergies at the very beginning? And I’d say yeah, that’s what I thought it was because everything was blooming, and then it just wouldn’t go away.’
And a lot of, ‘Hey, I got a low grade fever and this and that. What do you think?’
And I’m like, ‘Make sure you talk to your doctor but based upon what you’re saying, it feels exactly like what I what I had when I was going through it.’
What’s your takeaway after experiencing coronavirus?
I think if you’re not heeding the government warnings, if you’re not heeding what you see on the news, what I’m saying, what you’re reading on Twitter, you’re really doing yourself a disservice and those around you. It’s not whether it makes you sick because you can be a vector for it. You know, like a mosquito, you can be a vector for it.
In fact, [you can infect] your mom who has COPD or someone with cancer, or infect your grandfather who’s just old, but he’s healthy, and you can kill those people. So I think at this point in time, not heeding those warnings, you know better now.
You’re just being detrimental to other people’s health, because that’s what this is all about. It’s about others’ health, not yours. Because if it’s in the air, and I think they’re slowly coming to that determination, officially, nothing you can do about that. That’s why they’re trying to separate everybody as much as possible.
So if you’re still going out and running in a crowd or going shopping and not heeding any warnings, you’re not being honest with yourself. And you’re not taking other people’s health into consideration because at this point, it’s a community issue. It’s a county issue state, federal, you know what I mean? It’s, it’s bigger than you and your life.
What’s your overall message to others about coronavirus?
Because there are doubters out there that think this is overblown, that say I’m just going to keep going to the bar, this isn’t that big of a deal, my personal belief is no one’s trying to steal your liberty. So stay home and listen to your body. Those are probably the two best things you can do. Because if this thing is airborne, you’re going to catch it and if you do catch it, let’s hope it’s not very, very bad.
But listen to what your body says because so many times, we just put our heads down, grind on and we continue working or charging through our day. This is serious because it’s a respiratory issue. It’s not just going to make your body feel bad or inflame your sinuses or something simple like that. This is going to affect your ability to live.
So if you do start showing signs and symptoms, listen to what your body is telling you and don’t fight through and don’t grind because you can go from alive to dead in just a few days if you get a bad case of this.
And at the same time, heed all the warnings. The officials are telling you. They’re coming from, I would say a point of love, which is weird to say about government officials but love of people and country and state, trying to look after the citizens. This is the ultimate thing that an elected official can do to look after their citizens is [provide] the best information available that they have and try your best to keep your citizens alive and safe.
So literally stay home is what I’ve been telling everybody and listen to your body. If it hurts to breathe, listen to that. If your head hurts, listen to that. If all of a sudden you get up, you walk to the bathroom and you feel like you’ve been running but you’re not, listen to that. If your heart is racing, listen to that.
Those are all things that could potentially save you.
Follow Justin on Twitter
Inspired by Justin's story?
Share your story, too!
Coronavirus Stories
Justin Wilhite
Infection: Community spread
Home: Sacramento Area
1st Symptoms: Persistent headache (resistent to Tylenol + OTC medications), chest pains
COVID-19 Test: Not taken
Case: Moderate
Treatment: Tamiflu, OTC medications
Status: Recovered
...
Tina Baker’s Story Pt. 1 (Diagnosis & Treatment)
Infection: Work trip to London
Home: Palo Alto, CA
1st Symptoms: Sore throat, major fatigue
COVID-19 Test: Positive
Case: Moderate to severe
Treatment: Clinical Drug Trial (Remdesivir)
Status: Recovered, back to work (from home)
...