Carmen’s Stage 1 Papillary Thyroid Cancer Story
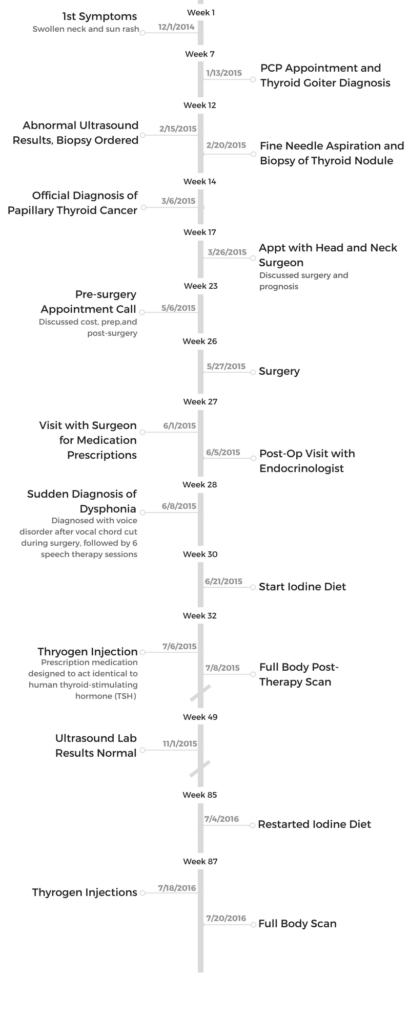
Carmen shares her stage 1 papillary thyroid cancer story, undergoing thyroidectomy, hormone replacement therapy (Synthroid), and radioactive iodine treatment.
In her story below, Carmen also highlights navigating life after a cancer diagnosis, including guidance for students dealing with treatment, how she advocated for herself as a patient, and how people were able to best support her through treatment. Thanks, Carmen!

- Name: Carmen Y.
- Diagnosis
- Papillary thyroid cancer
- Age: 26
- 1st Symptoms:
- Swollen neck
- Treatment:
- Thyroidectomy
- Surgical removal of entire thyroid
- Hormone replacement therapy (Synthroid)
- Radioactive Iodine Treatment
- Thyroidectomy
- Diagnosis
- Surgery (Total Thyroidectomy)
- What tests and scans did you undergo before surgery
- Describe the thyroidectomy surgery
- Waking up from surgery
- Were there any side effects after the surgery
- How long was recovery supposed to take
- Describe the vocal cord complication
- What did you have to do to recover from the complication
- Describe the speech therapy sessions
- Vocal cord specialists offered alternative treatments
- Any permanent repercussions from the cut vocal cord
- Radioactive Iodine Treatment & Synthroid
- Quality of Life
- How was life after treatment
- How did this impact school
- Any advice to students who have to deal with a diagnosis?
- How was dealing with insurance for treatment
- How did you manage your emotions through diagnosis and treatment?
- Did you have to advocate for yourself during treatment?
- People played a huge role in your experience
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You’re going to be okay, better than okay. You’re going to be stronger than you ever imagined.
Take all the time in the world to recover and focus on yourself.
Carmen Y.
Diagnosis
How did you get diagnosed
My grandma had just passed and we were all stressed about putting together her memorial service. I went to the doctor’s just to make sure everything was okay. The doctor ordered a blood test for thyroid levels. The test came back normal.
Three years later, people around me in the medical field recommended that I go check out my slightly swollen neck. I couldn’t even tell myself, but I decided it was time to go check on it once and for all.
I was 26 at the time and had just gotten kicked off my dad’s insurance. I wanted to make sure that I had insurance before starting my “thyroid” journey. I knew it was going to cost a lot if anything serious was found.
How did you decide where to go for diagnosis
I already knew that I wanted to go to Kaiser for everything because I grew up with Kaiser. I didn’t do much research.
It was also very convenient for me since it was a “one-stop shop” and the main building was a 15-minute drive from my parents’ house.
What was the exact diagnosis and staging
Papillary thyroid cancer. It had not spread to the lymph nodes or the other side of the thyroid. It stayed mainly on the left thyroid.
The cancer did not spread.
It was primarily in my left thyroid, but they recommended that I removed my whole thyroid to be cautious. The final pathology report indicated the cancer was present in the left lobe of the thyroid.
How were you feeling when you were diagnosed
Everything prior to the diagnosis was already leading me up to cancer. Knowing that I had to do a biopsy after the ultrasound, a phone call and office visit after the biopsy usually means there’s something more to the results.
I was pretty prepared for the diagnosis and just really wanted to know what the prognosis and next steps were. I also felt really bad because my endocrinologist broke the news to me and I told her it was okay. She said I was the nicest person ever. I told her I felt bad that she felt bad more than anything else.
How did you break the news to your loved ones
Definitely the hardest part prior to the procedure. It was really hard to come up with an easy way to break the news to anyone. Of course it was easier to tell people before the procedure.
I had to figure out all the steps of the treatment before I could tell people about my diagnosis. I also picked the timing to tell certain people.
»MORE: Breaking the news of a diagnosis to loved ones

What was your doctor’s recommendation on treatment
My endocrinologist and head and neck department head’s recommendation was for total thyroidectomy (total removal of the thyroid). Here’s what my doctor (Head & Neck surgeon) sent me prior to meeting for the first time discussing surgery:
Purposes and benefits: Remove thyroid cancer
Alternatives: no other recommended ones
Risks:
- Hoarseness: A change in the voice quality may occur due to injury to the vocal cords or to the nerves that stimulate the muscles which move the cords. This may be mild or severe, temporary or permanent.
- Bleeding (hematoma): Rarely, significant bleeding may occur during or postoperatively requiring transfusion. A hematoma (a collection of blood under the skin) rarely develops after surgery. A hematoma can cause compression of the trachea or airway that may lead to airway obstruction which if not removed may cause suffocation. Emergent re-operation may be necessary to remove the clot.
- Breathing: Airway obstruction may be due to bleeding or injury to both of the nerves that move the vocal cords resulting in paralysis with the cords closing off the airway. A person with bilateral vocal cord paralysis will have decreased exercise tolerance and might require further surgery. Very rarely, a tracheostomy is needed to obtain an airway.
- Pneumothorax: The chest cavity may be violated with removal of a large thyroid gland. An air leak into the chest cavity can cause collapse of a lung. Additional surgery may be required for this problem.
- Hypothyroidism: Thyroid hormone replacement may be necessary even with partial removal of the gland. This may be temporary or permanent.
- Hypoparathyroidism with hypocalcemia: Low calcium can result from compromise of the parathyroid during thyroid surgery. The parathyroid glands usually are located on the surface of the thyroid gland and are responsible for maintaining blood calcium levels. Low calcium can manifest with features including excitability, spasms, convulsions and arrhythmias. Calcium supplements may be required. This is usually temporary, but may be permanent.
Surgery (Total Thyroidectomy)
What tests and scans did you undergo before surgery
It always starts with the lab test for thyroid levels. Every lab test I had taken prior to surgery indicated that my thyroid levels were normal. However, there was a mass that was detected by the ultrasound.
- Ultrasound – My first ultrasound was very uncomfortable. I am someone who absolutely hates having anything touch my neck. I hate wearing turtle necks. So having an ultrasound on my neck was a big annoying thing for me.
Basically you lie down and they make you put your head on a pillow to position your neck to be propped up as high as you can for the ultrasound. Then they will pour the ultrasound gel on your neck so that the device can smoothly go over the area. I guess the neck area is a very difficult area to look around.
Also, I had some experience in the ER looking at x-rays and different views. So I was trying really hard to watch the girl while she was doing the ultrasound. I was trying to read what was going on in the screen which may have strained my neck even more and got me more annoyed. - Biopsy – Doing the biopsy was very interesting, I may have been a bit nervous not because of the procedure but because of what followed it. Because of what my mom went through with breast cancer, I knew that a biopsy basically gave you split roads. It’s the telltale of cancer or not.
My endocrinologist had me lie down and positioned my neck to be as “open” as possible. She then looked through the ultrasounds to see which side my nodule was. She stuck a needle into my neck and extracted fluid.
It’s like a prick, honestly. She did it twice. Many people may be afraid of this even though it’s equivalent to a blood draw, only on your neck. My dad went with me for this one.

Describe the thyroidectomy surgery
Before surgery was really about scheduling and details. I wanted to make sure that I educated the people around me about the surgery.
My number one worry was that they would worry. So I made sure I had long conversations and discussions to reassure people that this was a short procedure, outpatient and that I had a great prognosis.
I wanted to make sure I planned out my schedule before and after to take care of everything in case I was going to be sick and woozy for about a week.”
The day of the surgery, my brother and my dad brought me in. They went to work after I went in and told me to call right when I came out. I texted my friends, I joked around with my parents. I asked my surgeon for a picture of my thyroid.
My anesthesiologist talked to me about what was going to happen. I asked her what I could do in case I got nauseous right after. They wheeled me into the operating room (OR).
I remembered I wanted to take advantage of this exposure to the OR as much as possible. I tried to read everything on the whiteboard, I talked to my surgeons and slowly counted to ten as my anesthesiologist gave a scenario of blasting off a spaceship.
I had not too much fear, I told myself, I was going to sleep and when I woke up, I would have a scar on my neck and no thyroid.
Waking up from surgery
I woke up with the doctor in my face telling me all was well. He said, “Dad will be on his way,” and that I would see him for a follow-up soon.
He then told me something went wrong with my vocal cord and that I would be seeing a speech therapist after.
Were there any side effects after the surgery
I was a bit foggy. But the nurses were able to call my dad to come get me. They wheeled me down to the parking lot and I slowly got into the car.
The car ride home was ten minutes but it felt like forever. I was basically lying down in the passenger seat. It just felt like I was trying to get from one bed to another.
Side effects, there was not so much. My neck area was bandaged and my mom was waiting for me at home. It was really hard to turn my neck.
Here was what my doctor wrote to me: “Every patient recovers at a different rate. After thyroid surgery, most patients take between 1-3 weeks to recover. Routine activity is fine just no heavy lifting more than 10 pounds.
You do not necessarily need to stay home during that time. You will not need to stay in the hospital unless a problem occurs. I generally would not recommend travel immediately after surgery but, you should be okay after about a week.”
How long was recovery supposed to take
They tell you that thyroid surgery takes three days to a week to recover. I don’t doubt that it could be done. After all, I signed up for summer session to take two weeks later.
However, I did not realize that the stitches would take the longest to recover.
My mom was a bit nervous about it so basically I couldn’t wet it for about a month. The doctor told me to rip off all the bandaids the week after. But I still had a saran wrap around it for at least two weeks.

Complication: Vocal Cord
Describe the vocal cord complication
During my first follow-up appointment with my surgeons, I really wanted to find out why they cut my vocal cord. I was angry that there was a complication.
I was also angry they forgot to take a picture of my thyroid. They told me that because my thyroid was so inflamed, it was very tender. They had trouble taking it out and accidentally cut my left vocal cord. They repaired my vocal cord during surgery but it was not working after that.
At every mention of my left vocal cord, my heart sank. There was nothing I could do. I asked them when I would get my voice back and how I would get it back. It felt impossible at that point because at that moment I had trouble saying it out loud.
What did you have to do to recover from the complication
I went through a lot of speech therapy appointments. I was so grateful for my cousin who drove me to and from all my appointments. I was at Kaiser so much they no longer asked for my ID to check in.
My speech therapist understood my frustration. We had a voice specialist come in to take a look at my vocal cords and offer options.
Describe the speech therapy sessions
These were regular sessions that went from weekly meetings to biweekly to monthly meetings. The doctor would teach me techniques of breathing and speaking from my diaphragm. He taught me exercises like blowing bubbles with a straw and blowing up a balloon.
Basically, my left vocal cord was cut and repaired during surgery. However, that does not mean that it would automatically move again. My nerve no longer works to control that left vocal cord, it is paralyzed.
In order to talk or make noises, the left and right vocal cords come together to meet in the middle of your windpipe to create different tones and sounds. Because my left vocal cord was paralyzed, there was gap between where my left and right vocal cord were supposed to meet.
Therefore, I would not only not be able to speak, I also had trouble drinking liquids. If I drank too fast and it fell through the gap, I would get short on breath really quick. Speech therapy was to help me train my right vocal cord to move closer to my paralyzed left vocal cord so they would meet and I could talk.
Through the practices, my right vocal cord would slowly move over to compensate for the left vocal cord. After six months, my right vocal cord would move over already and I would be able to speak. However, I was warned that my voice would never be the same again.

Vocal cord specialists offered alternative treatments
Many specialists came to see my case and to offer faster alternatives that might help me speak faster. These alternatives all involved another procedure. They offered to inject fat into my left vocal cord to bulk up the cord so that the right vocal cord did not have to move over as much to meet the left vocal cord.
However, there was no guarantee as to how long the left vocal cord would stay fat. Another option involved surgery to move the right vocal cord over to compensate for the distance without me having to do speech therapy to move it. I declined all these options and just worked harder on my exercises.
Once I got my voice back, I celebrated with Blue Bottle affogato that morning after my final speech therapy session. It became a tradition for me to go to the Blue Bottle cafe after every “successful” or “good” appointment.
Not too many people noticed that my voice had once been out. They all said I sounded the same. I joked around to say that everyone better have taken advantage of the six months I had to shut up. I have a reputation of talking too much and too loud!
Any permanent repercussions from the cut vocal cord
My left vocal cord is permanently paralyzed so my right vocal cord has moved over to compensate for the left vocal cord paralysis. I was told my voice will never be the same. It is true. I am currently taking very long to recover from days of yelling or when I strain my voice.
Recently, due to constant yelling and perhaps not enough rest, my voice has been hoarse for about five months. I haven’t had any problems until now.
Three Sharks seasons have passed since my thyroidectomy and it has finally caught up with me. In the past six months, I have noticed that my voice doesn’t recover as fast as it used to. I would lose my voice for two days because of the Sharks games that I was going to and the concerts in between. Then I would take another two days to regain my voice.
Now one week at the office and another weekend in retail and I notice my voice will be gone. My high notes cut out and I can barely whisper. I visited with a speech doctor four months ago when I did my lab test and finally agreed to see my primary care provider for check up. She told me there was nothing wrong with my right vocal cord except for it being sore.
She told me I needed to rest my voice. It has been difficult and I am afraid that I have permanently damaged my one and only good vocal cord.
Many people have asked me if I am actually sick and just sound like I have a cough. They have forgotten that I only have one working vocal cord. My mom is concerned and once we started talking about it, it turns out, she did not even realize I only have one good working vocal cord. I think this may be the beginning of another new battle for me.

Radioactive Iodine Treatment & Synthroid
Describe the radioactive iodine treatment after
Probably one of the most difficult times during my whole thyroid journey aside from speech therapy.
During this time, I was frustrated with the low iodine diet. I am such a foodie and never thought that I would ever go on a diet. I definitely underestimated how difficult a strict diet was. I could not eat rice, limited amount of meat, steer clear of sea salt and anything that hinted at iodine. Basically, I should not eat out.
In the beginning, I thought I would be fine if my mom just bought me cases of salad and I just poured sesame oil as dressing. After my first meal of salad, I was hungry. So hungry!
I would go out and think that I would find something on the menu that I could eat. No, I could not eat anything. There was a risk of MSG or sea salt or iodized salt in the food. I got really frustrated my first few days.
The only thing that kept me sane for those first three days was that I could still have coffee. This was also the time when my body recalibrated and I was sensitive to caffeine and adopted black coffee in my life.
I learned to meal prep and ask restaurants ahead of time if it was okay to bring my own food when my friends insisted on going out.
If restaurants did not allow me to bring my own food (for medical reasons) I would bring my own food and eat in the car before going to the restaurant to enjoy friends’ company. I would just sit and drink water.
People say I lost weight. I did not care. I just wanted food back in my life! People would not be used to my diet nor would they remember about my pill. My relatives stayed with us for a month (from China) and they would ask me every morning with no fail whether I wanted to eat the moment I came out of the bathroom from washing up. I had to repeat:
- I could only eat one hour after my pill.
- I could only eat certain things on the low iodine diet. This first time on the diet tested my patience to the max.
The second time I was on the diet a year later, things were a lot easier. I knew exactly what I was getting myself into.
Some friends who vowed to do the diet with me a year ago backed out the second year. Some friends asked why I was so serious and so strict on this diet. I told them, it was either I cheat on the diet and cheat myself or just die. I was not willing to put my own health on the line. This was not about losing weight, it was about making sure my thyroid no longer existed.

Do you have to undergo more tests
Yes, at first I had to do blood tests every three months to monitor how my thyroid was doing and if the thyroid replacement pills (Levothyroxine) was the accurate and correct dosage.
After about three times or nine months I went to doing lab tests every six months. The most recent one, I kept forgetting and it suddenly turned into a year.
Once I readjusted dosage per my endocrinologist, I was told to go back to do blood tests two months after the adjustment to see how the medicine was working in my body.
As far as scans go, a year after my first radioactive iodine treatment in July 2015, I had to go through another “low iodine diet” and have a scan done with nuclear medicine. The scan came out clean and I wasn’t as closely monitored.
Describe the pills you have to take for the rest of your life
Levothyroxine are the pills that serve as thyroid replacement for me. Because the thyroid is a gland that is very important to maintain homeostasis for your body, it is very crucial for the accurate amount of Levothyroxine to be taken after thyroidectomy.
Here’s the schedule: Levothyroxine is to be taken at the same time every day, one hour before your first meal or first bite of the day. It should be taken every day.
If you accidentally skip one day, you are advised not to take two to catch up but since it’s a hormone that takes time to regulate your body, skipping one day may not be a big problem. I have missed one day since I have started taking the pills.
Dosage: Based on age, weight and of course your thyroid levels (from lab tests), the endocrinologist will prescribe a dosage that is supposedly fitting for you. If there are symptoms that show up after difference in dosage, they will adjust accordingly.
Based on your dosage, you can either have hyperthyroid or hypothyroid. Usually the symptoms are not severe because your endocrinologist will have a ballpark area of how much Levothyroxine you need.
However, this was one of my main concerns when I first started taking the thyroid replacement. Because I knew what the thyroid did (from previous classes I took) I knew that I could gain weight, have depression, have hair falling out and be fatigued if I had too little Levothyroxine (hypothyroid).
I have not experienced much of this. Right now is probably the only time I am noticing mild forms of this. I am gaining weight more than usual but it’s so mild that I can’t tell if it’s because I haven’t gone to the gym in too long and have been having too many sweets.
My hair is shedding a bit more than usual, but nothing too unusual from girls always leaving their hair everywhere. I also have mild form of bad memory though I’m also not sure if it’s because I’ve been doing so much and also getting older. I have not had any problems other than that. ”
The Levothyroxine pills usually only come in pills of certain increments. To get the correct dosage that my endocrinologist recommends, she usually tweaks it by the week so that I get my correct dosage if calculated by the day.

For example, six months ago, I was taking 112 milligrams every day. Four months ago, I did my blood test and she reduced my dosage to 104 milligrams a day. After that, she reduced my dosage to 96 milligrams a day.
Did you have any hair loss
I dealt with very minimal hair loss due to hypothyroid function. This means that I started to lose hair because of losing my thyroid.
I also experience a bit of hair loss when my dosage of Levothyroxine (thyroid replacement pills) is too low. It is a very mild bit of hair loss where you can’t even tell.
Quality of Life
How was life after treatment
There haven’t been many long term effects on me other than my voice. Life after treatment in terms of school had an immediate impact for me. I did sign up for summer session of school that would have started a week after.
There was no way I was going to head up to Davis, commute back and forth from Davis to Sacramento in the week after my procedure. I could not even shower by myself. I had to take baths and my mom helped me wash my hair every other day.
How did this impact school
The good thing was that I had already completed all my classes for my communications degree (I kind of planned it out). I only had to retake some Anatomy and Physiology classes that I signed up for summer school. I wanted A’s and B’s to apply for nursing school so there was no point in taking a class if I wasn’t going to excel in it.
I opted to take the second summer session for Anatomy & Physiology 2. The ironic part of this is that we actually study the thyroid and briefly touched upon the Iodine treatment I had went through.
Prior to starting summer classes, I did email my professor regarding my situation and that I would be minimally speaking in class because of my voice. There were minimal impacts that affected my studies and I managed to get a B+ in that class.
Any advice to students who have to deal with a diagnosis?
NOTE: Treatment should be determined between patients, caregivers, and the professional medical staff.
For me, academics was my priority at the time of figuring out if I should go get my thyroid checked out. I hate myself for being so logical and having to plan out everything accordingly.
I knew that thyroid cancer, which I thought was my worst case scenario before I got any medical advice, was a slow-acting cancer. It was not going to affect my health immediately if I was not going to take it out. So I waited until I was almost done with all my classes to plan for surgery.
First, if you’re a bio or pre-med student, you already know what you’re getting yourself into. I would recommend consulting with your doctor regarding the timeline. Yes, thyroid cancer sounds very scary but all the conversations revolving around such a diagnosis almost always starts with “this is the best kind of cancer to have.”

If the symptoms are not apparent and not urgent, I would recommend asking your doctor/endocrinologist/medical expert to work with your timeline as a student. I would definitely not take the school year or the middle of classes to go through the procedure.
If you can wait, wait to take the summer off to take care of it. A summer is really all it takes to take care of your thyroid (of course it’s per case).
How was dealing with insurance for treatment
Insurance was probably the biggest hassle in my mind. But it was actually a lot easier to deal with than I thought. I got Covered CA in almost two days and set up a Kaiser appointment. I did end up paying for about 10-percent of the procedure which was about $3,000.
How did you manage your emotions through diagnosis and treatment?
I am someone who generally wants to deal with everything logically if I am emotionally and mentally stressed. My previous work in the emergency room really prepared me to handle my own diagnosis.
Although I only worked in the ER for about four months (as a scribe), the amount of the exposure I had working with the patients and the providers really opened my eyes to the medical field. I was a scribe so I had to basically memorize charts including patient history.
I worked in the ER in the Sacramento area, including the Elk Grove area and downtown Sacramento. Therefore, I came in contact with a lot of the older generation and low-income population.
Thyroid cancer was something that was very common on their charts. In the ER, I saw people who were waiting there for 20 hours, some who had their tongue cut off and still had to wait four hours, some who were told they had cancer at 1 in the morning with no follow up.
I learned about prioritizing patients and what a doctor really does. I saw people fighting for their lives while some people were so drunk on the street that they just wanted a meal in the hospital.
I came across patients who were there for the sixth time with their family because they cut themselves.
I was very humbled by this experience. I promised myself that I would take care of myself and reminded myself that there wasn’t much to complain about. I also promised myself to never go to the ER unless I was really dying.
So with immediate emotional and mental stress, I always tell myself to be patient and that the world is so much bigger.
I have been working retail for about 12 years now and some days, I almost want to quit or lash out at customers. But I also know that at the end of the day, I am only selling clothes. There’s nothing significant about arguing with a customer about anything. I really try to look at the bigger picture and kill people with kindness because that’s probably the most productive thing you can do out of anger.
Did you have to advocate for yourself during treatment?
The time that I felt like I had to advocate for myself was my first primary care provider appointment regarding thyroid cancer. At the time, I did not suspect that I had thyroid cancer but I really needed an ultrasound to see what was going on. My PCP insisted that it was a goiter and that it was common amongst Asians.
After the fact, I talked to a lot of my friends in the medical field (a majority of them were nurses) who said that you really have to be proactive about your own health. Even doctors aren’t always sure of what is and what is not going on with your body.
Once you have an odd feeling or even suspect something is going on, it is really better to go and check it out to be sure. Early prevention (as cliche as it sounds) is really what saves people, spreads awareness and is a better story to tell.
»MORE: How to be a self-advocate as a patient

People played a huge role in your experience
My endocrinologist made all the difference in the world for me. She is the kindest person. She genuinely cared about my body and my emotional health. She made everything very easy for me and was always there for me. It was very easy to communicate with her and she even gave me her personal cell phone number.
My surgeon, as recommended by my endocrinologist, was very friendly and relatable. Although I understand that he did not perform the surgery and is a very busy man (since he’s the head of the head and neck department), I would not have wanted anyone else as the point person for my surgery.
My mom still nags me about everything I eat to this day. She is also a cancer survivor (breast cancer two times).
There are certain foods that she firmly believes are bad for cancer patients. I may not believe her, but I just listen as a daughter. She made me realize how blessed and fortunate I am to have a home to fall back upon. She took care of me like a caregiver during my recovery time. I remember constantly thinking that I was going backwards in life because instead of providing and supporting my parents, I fell backwards to having them take care of me like I was a child again.
She never told me that this was okay, but everything that my parents did for me during that time told me it was okay to grow slower and build my life slower than everyone else.

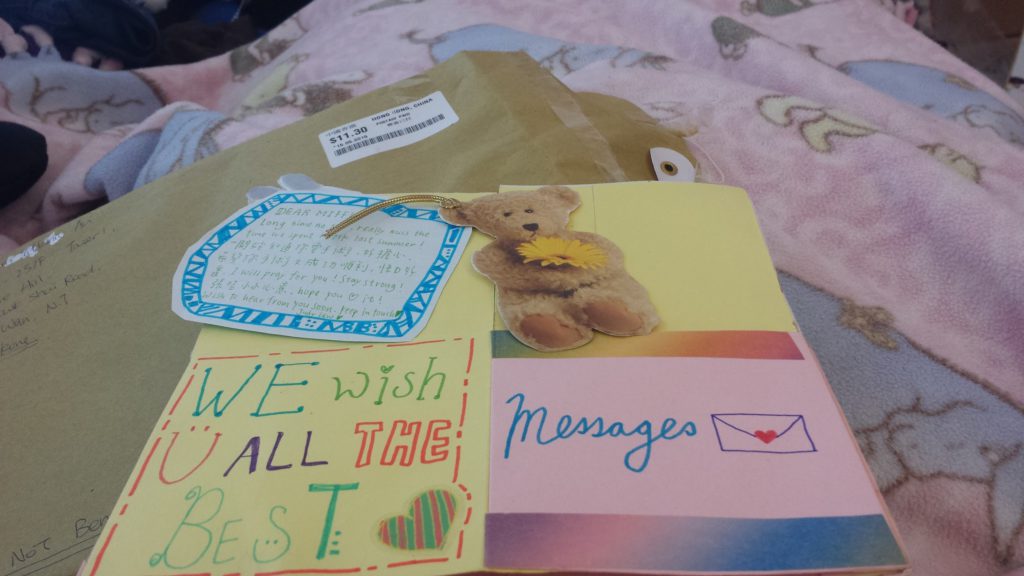
My cousins are just like siblings to me. They took me out to eat the things I could eat. At a point when the only good thing I could still eat was ice cream, there were deliveries from Yogurtland every other day. There was absolutely nothing to do, they brought over a cricut machine and gave me arts and crafts to do.
My brother waited on me hand and foot. He even gave me a mini stick to bang on a metal box to call for his attention. One of my cousins surprised me and brought me to the Taylor Swift 1989 concert with floor seats. My voice was barely recovered, but I screamed loud enough!
My friends. I remembered after telling one of my best friends that my dad and brother went home after I had my surgery and came back to pick me up after, she quickly said, “If I knew that was the case, I would’ve come and stayed the whole time to wait for you.”
They didn’t come visit right after but they knew I needed my own recovery time. One of my other friends was my plus one for a wedding that was two days after my radioactive iodine treatment.
During that time, I was supposed to still be in isolation in case I spread my radioactivity to anyone. I asked him if he could bring me to the wedding and I would sit in the back so I wouldn’t make him radioactive in case anything happened. He brushed off any precautions and insisted that I sit next to him on the passenger side.
The people in my life mattered so much during my whole medical treatment.

Inspired by Carmen's story?
Share your story, too!
Thyroid Cancer Stories (Under 55)
Carmen Y., Papillary Thyroid Cancer
Cancer details: Most common kind of thyroid cancer
1st Symptoms: Swollen neck
Treatment: Thyroidectomy (entire removal of thyroid), radioactive iodine treatment
...
Jamie K., Papillary Thyroid Cancer
Cancer details: Most common kind of thyroid cancer
1st Symptoms: Difficulty swallowing, lump on neck
Treatment: Thyroidectomy (entire removal of thyroid), radioactive iodine treatment
...
Sarah J., Papillary Thyroid Cancer, Stage 1
Cancer details: Spread to lymph nodes
1st Symptoms: Enlarged thyroid
Treatment: Thyroidectomy (entire removal of thyroid), partial neck dissection, radioactive iodine treatment
...
Nancy, Metastatic Papillary Thyroid Cancer, Stage 2
Cancer details: Spread to lymph nodes
1st Symptoms: Lump in neck
Treatment: Thyroidectomy (entire removal of thyroid), radioactive iodine treatment
...
Greg S., Metastatic Papillary Thyroid Cancer, Stage 2
Cancer details: Spread to lymph nodes
1st Symptoms: Fatigue, lump in neck near Adam’s apple
Treatment: Thyroidectomy (entire removal of thyroid), radioactive iodine treatment
...
Jenna C., Metastatic Papillary Thyroid Cancer, Stage 2
Cancer details: Spread to lymph nodes
1st Symptoms: Hoarse voice, painful talking, lump in neck
Treatment: Thyroidectomy (entire removal of thyroid), radioactive iodine treatment
...
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation
...





