Rick’s Stage 1 Seminoma Testicular Cancer Story
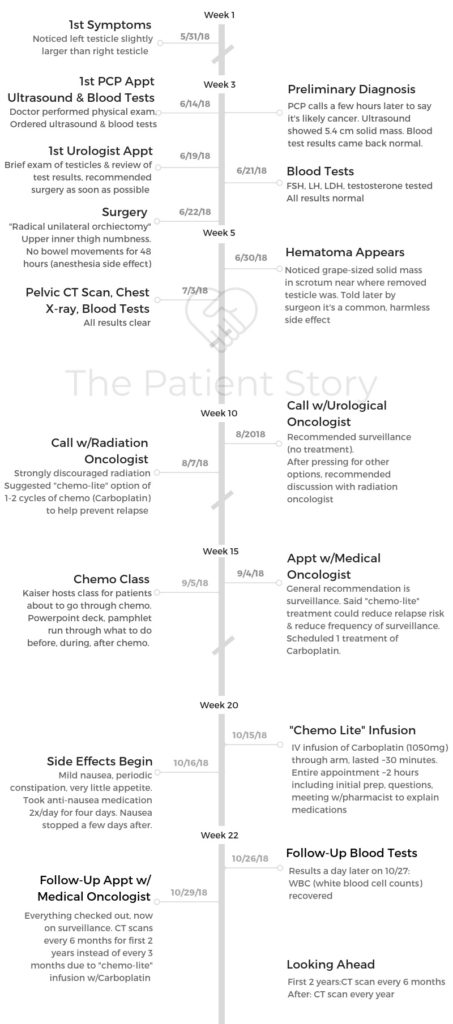
Rick shares his stage 1 seminoma testicular cancer story, how he approached treatment decisions, and describes undergoing treatment, including an orchiectomy (surgery) and “chemo”-lite.
In his story, Rick also highlights the topics most important to him during the cancer experience, including determining which doctor’s recommendations he would rely on, preserving fertility, the ability to work during treatment, and the importance of patient self-advocacy. Thanks for sharing your story, Rick!

- Name: Rick H.
- Diagnosis (DX):
- Testicular Cancer
- Seminoma
- Stage 1 (localized)
- Age at DX: 34
- 1st Symptoms:
- Noticed size of one testicle larger than the other
- Dull pain
- Medical Team:
- Primary care physician → urologist → surgeon → urological oncologist → radiation oncologist
- Tests:
- Primary care physician examination
- Same day blood work & ultrasound
- Treatment:
- Orchiectomy (surgery to remove testicle)
- “Chemo Lite”: 1 chemo infusion of carboplatin (reduce chance of cancer returning)
- Diagnosis
- Treatment Decisions
- What physicians did you see?
- How was the first appointment with the urologist?
- What decisions did you have to make before treatment?
- Did you consider getting a prosthetic (testicle)?
- Describe the tests you went through
- Describe the ultrasound
- How long did it take to get results
- Did you consider getting a second opinion?
- Surgery and Side Effects
- After Surgery
- You had to undergo more tests after surgery?
- Did you have to advocate for yourself?
- What decisions did you have to make after surgery?
- You went with the radiation oncologist's post-surgery recommendation over the urological oncologist's. Why?
- Describe the recommendation of undergoing "chemo-lite"
- Why did the radiation oncologist know more about treatment options?
- Was there discussion about whether to remove the other testicle?
- When were you able to work again?
- How did your diagnosis impact your life perspective?
- Fertility
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
The fortunate thing if you have this type of cancer is we’ve got incredible technology now and treatments, so the survival rates are incredibly high.
The path towards treatment is relatively linear. There’s not a whole lot of difficult choices you’re going to have to make, but there are some risks in different therapies.
So it’s important to be an advocate for yourself and important to study the different options that you have throughout the process.
Rick H.
Diagnosis
What were your first symptoms?
I didn’t notice a lump or anything. What I did notice was, “Oh, one testicle feels very slightly larger than I think it should be.” It was only very slightly, so of course I did what everybody does: I went to Google and searched.
All of the Google results say totally normal for one to be bigger than the other. All the results just kind of say that.
But then I took a step back and just thought, ‘I’ve been alive for 34 years. The fact that I’m noticing this completely unsolicited, the fact that I’m just noticing it means that there’s probably something worth getting checked out.’
Within a couple days of noticing it, I scheduled an appointment with the doctor for about a week later. He took a look and scheduled me for an ultrasound.
Describe the ultrasound
I was able to get an ultrasound on that day. I went over, got the ultrasound, and that’s where I kind of thought something might be off, because usually as a technician is doing something, they can see the results.
I asked how it was looking. She was very quiet and said, “Oh, your doctor will tell you your results.”
I figured there’s probably something a bit off at that point, but wasn’t sure what yet. Afterwards I saw a message from the doctor that I should go in and I should schedule an appointment with the urologist because they found a mass.
»MORE: Patients describe dealing with scanxiety and waiting for results
How did you get diagnosed?
I immediately responded to the doctor asking questions and then he called me. I felt like maybe he should have called first, but I called and we talked about it.
That’s when he said there’s a mass.
They can’t diagnose it until they’ve actually taken it out, but it’s pretty much guaranteed to be cancer because that’s pretty much all it would be as a solid mass there.
It was also very large. The cutoff for some risks is around like four centimeters. It was like five-and-a-half centimeters. What I noticed was basically just like it took up the whole size. People describe it as being like a lump, but it basically filled up the whole thing and then expanded.
Then I got an appointment with the urologist. I was able to get that for the following week. I think my doctor’s appointment was on a Thursday and then the urologist was the following Tuesday.
During that time period, in between, somewhere during that course of that week or so, I started to notice a little bit of like dull pain, so I think it was starting to grow even more at that point. I went into the urologist.

How did you process the cancer diagnosis?
I don’t tend to get super emotional about things. I try to take a mindset of like, worrying is a bad waste of the imagination, so I don’t try to get stressed about things.
If you have control over something, then do what you can, and if you don’t then learn to let it go. And so in the case of this, the stressful part was I didn’t know which things I had control over.
When I got the diagnosis, I didn’t know the boundaries of what I could do. I could talk to like 100 people. I could go out and spend every waking hour contacting physicians.
But maybe that won’t do anything. Maybe there’s no decision to be made. That’s why the way I actually responded is literally just went on Amazon, found good reviewed textbooks on the topic and ordered them.
I started reading a bunch online. Because that was something I could do, learning about what the options were.
People I talked to, even just a day, or a couple of days after, said, “Oh, you’re pretty cool-headed about this.”
For me, there’s no point in worrying. What’s going to happen is going to happen. I can do what I can to try and make things have the best possible outcome.
»MORE: Patients share how they processed a cancer diagnosis
How did you break the news to your loved ones?
With my parents, I wasn’t sure about when to tell them about it because I didn’t tell them right afterwards. I didn’t want them to freak out because I didn’t know very much yet, so I wanted to learn more. I told them a couple of days before the surgery.
I would have waited until afterwards, because I wanted to wait until I knew more, like what subtype is it? What are the risk factors? I wanted to wait until I knew that stuff before telling them because otherwise, I knew they were just going to get worried. I can take this mindset of I’m going to not worry about things until happens, but I know that they won’t.
I wanted to wait but I also didn’t want to create a situation where maybe some complication happens during surgery, or something bad, and that’s the first they hear about it is. So I let them know before the surgery.
I told them, “First of all, I’ve been diagnosed with a medical condition, but I just want to emphasize, this has a really high survival rate. It’s 95-plus-percent. It’s very treatable.”
I described the cancer and went through it. I just tried to manage it so they weren’t freaking out. They obviously still freaked out.
I think it can affect your friends more than you – almost.
I’ve talked to a couple of other people who had testicular cancer who said that. You almost have to manage your friends’ mental health because they’ll look at it and it’ll make them think about things in their life. I think my friends have gotten very emotional about things.
And yes, for the week afterwards (I’m doing a startup) and my co-founder came over and set up the office in my apartment. We just worked out of there so he could help take care of anything that I needed.
When you’re in the middle of it, I guess you can get caught up in just doing what’s next. And I think that’s probably a better way to be. To just be like, “Okay, well this is what I can do.”
But yes, I think for me the stronger emotional thing I felt was when I talked with friends afterwards, and just saw how much they really cared. That was something that I think you don’t get all the time. Yes, one of my friends was like, “Yes, it sucks that you have to get cancer for you to tell people how much you care about them.”
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
What physicians did you see?
- Primary care physician
- Urologist
- Surgeon
- Urological oncologist
- Radiation oncologist
I had several doctors: my general physician who prescribed the ultrasound and the blood work and then based on that, referred me to the urologist. The urologist referred me to the surgeon and to the urological oncologist. It’s somebody still in the urology branch at Kaiser but they have a specialty in oncology.
So then I had my surgeon who was a completely different person but also in the urology branch at Kaiser. Yeah so I went from general physician to urologist, urologist to surgeon, and then surgeon to urological oncologist.
The urological oncologist then was the one who I’m talking with now, and then he’s subsequently referred me to a radiation oncologist and that’s a whole separate path there.
How was the first appointment with the urologist?
We didn’t really do very much. He took a quick look and was like, “Okay, yeah. I already looked at your ultrasound, so we’re going to have to remove it.” The procedure is called an orchiectomy.
The first thought I got when I first got the call about the mass was, “I hope that I don’t have to lose a testicle. I hope that they can just take the tumor out.” It turns out that’s absolutely not how it works.
There’s no way for them to leave it because of certain risk reasons. When I went in, it was just kind of guaranteed that’s what was going to happen. I had done my own research at this point, so I knew that when I went in.
He told me they’d have to remove it, and also because it’s kind of large, they wanted to do it really quickly as soon as possible. They did an urgent appointment. It was Tuesday afternoon I was there. It was that Friday I was going to do it.
What decisions did you have to make before treatment?
I guess one fortunate thing about this type of cancer is that there aren’t that many decision points. There’s only generally like four types of treatment.
There’s the surgery, the orchiectomy, and that’s basically if they see a solid mass, there’s no question, you’re just going to be getting the orchiectomy. I’m not an expert on that, but generally there’s the orchiectomy, and then there’s three other options post orchiectomy.
There’s the Retroperitoneal Lymph Node Dissection (RPLND). So that’s actually physically removing those lymph nodes. Then there’s the radiation and that’s just like locally irradiating the abdomen and maybe the thoracic cavity, depending on where they’ve seen spreading in the lymph nodes.
Then there’s chemo, which is chemotherapy where you’re actually infusing drugs into the body and you’re doing that on a regular basis. That can generally, it seems like it’s around 3 to 4 months of chemo that you do for that.
So those are the things that you would do. So the decision points you have are one, do you do the surgery or not? Generally you just do the surgery, there’s no question about that and then afterwards it depends on the results of the biopsy in terms of what they would recommend to do.
There weren’t a lot of decisions to make. The only decision at that point is whether or not you want to get a prosthetic put in.
There’s a lot of misinformation and weird stuff online about that, too. There’s some people who say that it’s great and it makes you feel normal, and some people who say it’s weird and bad and there’s this whole mixed thing.
The doctors recommended against it, but I also kind of feel like doctors tend to err on the side of whatever’s going to reduce their risk. If you’re adding a foreign object in the body that just inherently increases the risk of any procedure, so it can ruin your record as a surgeon if a complication happens as a result of something that you stuck in there.
Did you consider getting a prosthetic (testicle)?
When I had the call with my surgeon the night before, I just asked him like, “Oh, well do you have any options for like interesting, cool prosthetics? Like do you have one that has a wifi hub or that can like glow with LEDs or have a speaker in it or something?” And it turns out they don’t have anything like that, so we don’t have that technology yet.
Definitely different for different people, but I think like getting a prosthetic at that point is just kind of putting lipstick on a pig. So, it’s not really worth it. I decided not to.
»MORE: Fertility preservation and cancer treatment
Describe the tests you went through
I did an ultrasound and blood work on the same day. So I went up to the imaging office and they told me to wait for them to come out. I said “Oh, is it going to be a little while? I could go do the blood work while I’m waiting.” So I went to the blood work and when I came up they were ready for me with that.
For the blood work there’s a few parameters they look at. There’s a few tumor markers that they look for. The parameters are not super specific necessarily so if you don’t see them it doesn’t mean that you don’t have cancer, it’s a better sign if they’re negative but they usually do it as a baseline to see if things have changed before and after the surgery.
So I did that as a baseline. All the tumor markers came up negative. For the tumor mass, it’s mainly the size they look at.
Describe the ultrasound
It was my first time going through an ultrasound like this. it’s basically what you would imagine for a pregnancy ultrasound where you are putting the gel on and then rubbing the thing, except on testicles. So just like that.
There wasn’t any shaving involved, so it was just put the gel on and then it takes a little while because they have to basically scan the whole thing going all the way up. They do both testicles for comparison purposes and also to check and see if there’s cancer in the other one.
I think it probably took 15 to 20 minutes, something like that. There was one technician doing that. There was no pain or anything.
How long did it take to get results
That was pretty quick. From when my appointment ended I think I heard the message back from the doctor within a couple of hours of that.
Did you consider getting a second opinion?
I did get a sort of second opinion. One of my good friends from high school and college, her fiance’s a urologist, but just getting out of training.
I had a text thread just with him, and he was telling me, “Oh, this is a standard operation. You should just do it. This is a standard thing. This is easy.”
For me, I was thinking initially, “Do I care who the surgeon is who does this?” It seems like a pretty important surgery, right? If they mess it up, that could be bad. I did consult just to check and see how normal these things are and how easy.
That’s another thing for the surgery, the orchiectomy. Apparently, as far as surgeries go, it’s one of the more straightforward kinds. From what I’ve heard, it’s almost anybody can do it.

Surgery and Side Effects
What happened before the orchiectomy (surgery)?
The day before [surgery] you get a call from your surgeon. He asked if I have any questions. The most important things are just telling me that I can’t eat or drink anything for certain windows of time beforehand because when you go through general anesthesia, it messes with your digestive tract and if you eat something and it gets stuck in there, it can cause significant problems. So the main thing is confirming that I don’t do that.
Then the second thing is asking whether or not you want a prosthetic put in. There’s lots of misinformation online about whether, or not, you should get a prosthetic.
There are people who get it and say that it’s great, people who don’t, and generally, the prosthetic is just this, like a silicone ball full of saline.
So, it’s similar to getting a breast implant. They would insert it back through the canal that they pulled the testicle out, they insert this one in, and then they effectively stitch it into there. So, they stitch it so it’ll hold them in place.
What is “preserve the nerve?”
My urologist said that when the surgeons are cutting through to get through the muscle to access the inguinal canal, apparently there’s a nerve they can run into that deals with your touch sensitivity. Basically in the upper inner thigh, and sort of like that groin type area. If they cut that, then you just lose feeling there.
My urologist just told me that there’s a bunch of surgeons who just, if they see it, they cut it. The reason being that some patients apparently can feel pain after the surgery, and they’d rather people be numb than have pain.
He said that the surgeons at Kaiser, at least in his office, they say preserve the nerve. They don’t cut the nerve. That was one thing I told my surgeon beforehand. I said, “Oh, preserve the nerve.”
I wasn’t sure if it really got through, but I’m pretty sure the nerve was actually cut during my surgery, because I’ve got that numbness as it’s described. I’m pretty sure it was cut, but there’s apparently a chance the feeling could come back at one point.
They won’t tell you straightforward if they cut it. I messaged saying like, “Oh, I’ve got a numbness. It seems like it’s possible that maybe it was cut. Is it that the feeling won’t ever come back, or do you think it will come back?” He just responded a message saying, “Oh, yeah. It’s possible.”
The fortunate thing is if you do get this numbness, it’s in an area where you never really notice it anyways. It’s not something that’s super noticeable.
Describe the prep before the orchiectomy
I needed to get there a couple hours before the surgery. My surgery ended up being significantly delayed. I went in and first thing they do is put in your IVs. They do basic vital signs and all of that stuff and then you’re just sitting, waiting to get prepped.
You sit in the bed with your IVs in and then eventually your surgeon comes and you meet your surgeon. You also meet your anesthesiologist in this process.
The anesthesiologist meeting is quick. They ask you as series of questions that you’ve already answered beforehand with the surgeon.
They ask you questions about allergies and whether you’ve had anesthesia before because they’re concerned of whether you could be allergic to it. They ask whether you’ve eaten and all of those kinds of basic questions.
Everybody you talk to will also ask you the same things. They ask you your name, your date of birth, what operation you’re having done today, and which side.
I said this probably like a dozen times throughout the course of the day. I was like, “My name’s Rick, here’s my birthdate, I’m having an orchiectomy, left side.”
You have to repeat that information over and over again.
I also had things I was trying to remember to tell the surgeon because I wanted to like let them know like, “Oh, remember to preserve the nerve.”
I wish that I had had like something I could have written a note down on because there were like some notes that I wanted to give to him.
Then when the surgeon came in he looks at the site where the incision is going to be. The surgeon actually shaved the site there and then he signed my leg. He signed his name on my left leg, and I think this is all a precaution to make sure that they do the correct side.
He asked me the same series of questions, like what’s your name, what’s your date of birth, what operation are you having, which side, and so actually signed his name and I had the signature of his name for like several days afterwards. You’re not allowed to wash either. You can’t do like any showers or anything.
They shaved, signed the leg, asked the series of questions again, and then, he left to go prep in the operating room. I was in this waiting area where there’s all these beds and on one side of the room, they said recovery.
One side of the room is everybody whose just had their surgery done and they’re just kind of like in recovery and then, the other side is where are like getting prepped to go into the operating room (OR). Eventually, they wheel your bed and you kind of like get wheeled through some hallways. Then you’re in the OR and it all happens pretty quickly.
They pull you in and they say that you’re gonna be falling asleep very quickly. I didn’t feel anything personally. They just kind of started administering the medicine and then I don’t remember. The next thing I remember is just waking up in the recovery room.

What do you remember coming out of surgery?
I think they still had morphine or something going into me and so you’re kind of recovering. You don’t really have much pain at that point because of that.So for me it was fortunate. The surgery all apparently went well and there was nothing significantly wrong.
Then afterwards you just chill there for up to an hour or two or something, just until you’re comfortable moving.
After that they can bring you out. They have you sit down and they check your vital signs again and stuff. They wait until you’re ready to stand on your own and they get you into a wheelchair.
Then you go out and I was able to go take an Uber home. Not by myself. So, you have somebody with you, but I think I would have been fine to do it by myself. You want somebody with you just in case because you’re still under the medication.
»MORE: Read more patient experiences with surgery
What were the side effects?
I didn’t feel it right away. I went home that night and was fine, went to bed, and then I woke up in the middle of the night with just a lot of pain.
I’m guessing whatever local anesthesia they administered must have worn off. They gave me some medication to take afterwards. I took one of those, but then I actually switched from that the next day. Some friends brought me some weed gummies.
A friend showed up the next morning with a bunch of those. I just ended up doing the cannabidiol (CBD) ones. They don’t make you high but they are supposed to help with pain.
I was doing about 10 milligrams of those every two hours during the day. That seemed to work fine. I did that for the course of four to six days after the surgery for pain.
»MORE: CBD, Cancer & Treatment Side Effects
Describe the pain after the orchiectomy
It’s mainly around the area of the incision. I’m not sure how much of it is due to the superficial cut in the skin and how much of it is due to cut-through muscle or what. But it’s just a pretty significant stinging pain.
Basically, if you lift your leg, or bend, or any movement like that is pretty painful. It’s a lot of using your arms to lift up. And so it’s just very slow to move around and when you transition from sitting to standing, when you’re doing any bending at all there’s a lot of pain.
The pain starts off being just a pain all the time, and then eventually it’s just when you’re moving. But then it starts to go away, and you can move more.
Describe the recovery process
I didn’t really have to bandage anything. They use this glue type, like an adhesive bandaging thing. Over the course of the first couple of weeks that just fell off on its own. I think it’s 24 or 48 hours without showering.
There was no pain when you first showered?
The water on it wasn’t necessarily painful because it’s got that adhesive layer over the top covering the wound.
The other thing is for about a month you can’t do any physical exertion. You can’t do any significant lifting of weights, or running, or anything. No riding bikes, none of that. It’s just very limited physical activity.
You can generally walk around. I think it was maybe three or four days after the surgery that I hobbled out, I actually left the apartment and hobbled around. But you walk very slowly. I never used crutches.

After Surgery
You had to undergo more tests after surgery?
Maybe like two weeks after the surgery, I went in to do the CT scan. So they do a CT scan and x-ray of the abdomen and the thoracic cavity.
What happens afterwards is you get the data, confirming what the size of the tumor is from actually taking the sample out for pathology. Then from pathology there’s a bunch of other things that they look at.
They take all that information and decide treatment from there. From the pathology, they give you the subtype. For me, it was seminoma.
They also give you the size of the tumor and then another really important thing they look at is whether it started to spread already.
Leading away from the testicle there are these blood vessels. In those vessels they can find cancer cell and so they call that a lymphovascular invasion.
I had a lymphovascular invasion in mine which means the cancer had started to exit the testicle and started to leave.
The CT scan came up negative, so it was all clear. They didn’t see anything in the lymph nodes so that’s a good sign.
It means that if it has spread, it’s too small to detect by X-rays yet. So it could be there but it might just be in the blood vessels or it might just be too small.
Did you have to advocate for yourself?
I think it’s always important to be an advocate for your own health and to get second opinions and to find somebody who you trust, who can like give you guidance, who isn’t necessarily just trying to preserve their own medical career.
If you can find somebody who can help, that’s important but it’s much more important probably for other cancers where the treatment is less obvious, and with this cancer it’s very fortunate.
If I’d have gotten this 40 years ago, I’d have a ten-percent survival rate. Because the introduction of new treatments it’s now like 95-percent-plus survival rate.
Another thing: Doctors give a little bit flippant responses sometimes. I think it’s the nature of the ecosystem. Doctors are just really overworked and they just have a lot of stuff to do. Their job is to keep you alive.
There’s somebody I talked to who went through similar cancer, and his point on this was it’s easier to get someone a psychiatrist than it is to resurrect them. I think the psychology part is important.
They measure on questions like, “Do people survive? What are the outcomes?” The system’s not set up properly to deal with all of the emotional things, probably.
» MORE: How to Be a Self Advocate
What decisions did you have to make after surgery?
The fortunate thing is it’s not a case of am I gonna survive or not. It’s more of a case of what’s going to be my quality of life post all of my treatment.
There are decisions to make around that but not a lot of decisions, whereas other cancers there could be like lots of different treatment options, lots of different paths that you can go down.
You went with the radiation oncologist’s post-surgery recommendation over the urological oncologist’s. Why?
I talked with the urological oncologist, had a phone call with him, and he said that what Kaiser does is after you have your surgery, you do your CT scans, and after you do another set of blood work after the surgery, which also came up negative for me.
The blood work and the scans all came up negative, which is a good sign. The scans are the better sign.
But they have a meeting with Kaiser for testicular cancer patients. One of the radiation oncologists called it a testicular cancer conference, but they basically get several of the clinicians together and they review all the cases that have come up in the last month or so.
After that happened, I had a call with the urological oncologist and so he said that his recommendation was surveillance.
There are several different paths you can go down for this cancer.

After you’ve done the surgery you can either do another surgery to the RPLND. They cut open your whole chest and abdomen, kinda reach behind your organs, and pull things out.
There’s a less invasive version that’s like laparoscopic, but also apparently there’s some controversy around it. I don’t know a ton about that.
But there’s a surgery, there’s the radiation, there’s the chemo, and then there’s just surveillance where for the next five years you just do surveillance and you get scans every couple of months at first, eventually down to every six months, and you do scans and blood work and just check to see if anything comes up.
He recommended surveillance, and the reasoning for that was that he said that based on my results I have about a seven- or eight-percent chance of the cancer coming back. He said that radiation was the only treatment that I would do and if I were to do that that would bring it down to like three-percent or something.
Those numbers didn’t really seem worth it to do radiation considering that radiation has side effects where it can introduce mutations that could become other cancers later, you also can get some organ damage, you can damage the bowels, stuff like that. So you can have like bowel problems. So he wouldn’t recommend the radiation.
The problem that I had was I had dug into the literature a bit and read some of the studies. His numbers didn’t match the numbers that I had.
From what I had read, patients like me based on my results have about a 30-percent chance of the cancer coming back, and then you have to do the VEP chemo. The great thing is that it’s very effective.
If you get it, it’s like 98-plus-percent survival rate. It’s just crazy good. The downside is that it has a lot of these acute and long term toxic effects. The individual drugs that they use are fairly toxic.
I’ve talked to people who have gone through this particular flavor of chemo and consistently they’ve said if there’s any way for me to avoid it, I should. It does things where it messes up your lungs, you can’t breath, you’re gonna have like respiratory issues for the rest of your life, you never can scuba dive again, and like all these other things.
It may have fertility issues, so you may want to try and avoid that. I was asking a lot of questions of the urological oncologist and he said “Well you know if you’re curious to learn more I can refer you to a radiation oncologist if you’re interested.” I said “Yeah, I’d like that.” So he scheduled the appointment and I had a call.
The radiation oncologist was great. He was very informed. He started off by citing studies and literature. He says, “Well there is one study done in like 2004 where they had this many patients, and they looked at this and they found that based on your risk factors,” which for me is the tumor size and the lymphovascular invasion, those two risk factors, make my risk a higher level than other patients of it coming back.
He said based on that, he also saw around a 30-percent chance. He was referencing a different paper than the one I had found.
Describe the recommendation of undergoing “chemo-lite”
He said I would be a good candidate to do what I would call “chemo-lite.” Instead of doing three drugs, it’s one drug. Instead of doing four cycles or so you do like one to two cycles.
The one drug, individually, is supposed to be less toxic than the other three individually. That drug’s Carboplatin.
Apparently a relatively new thing that people are doing within this type of cancer is doing Carboplatin treatment. He told me it’s pretty effective. It could take my 30-percent risk down to around five-percent or less, and it also doesn’t have as many of like the long term side effects.
Why did the radiation oncologist know more about treatment options?
The thing that was interesting was he said that he’s a radiation oncologist but he’s telling me about chemo to do, and that’s usually what the medical oncologist would do.
He said the ironic thing we’ll find is a lot of times you’ll find a radiation oncologist will know more about the treatment options and chemo than even the medical oncologist who administered chemo.
He said part of the reason for that is just historically radiation oncologists were the ones who managed testicular cancer patients.
Basically by default, anyone who got surgery or the orchiectomy, the first thing they would do afterwards would be radiation, as well. So they were immediately given a radiation oncologist who was managing their care.
Because of that, radiation oncologists were seeing the majority of patients because for many of the patients after radiation they don’t need anything else, and if they do their radiation oncologist would be the ones to identify that and then refer you down the line.
Was there discussion about whether to remove the other testicle?
The question was: Should you do the surgery or not so you can prevent something from happening? I think oftentimes the recommendation is much more nuanced. I’d say anybody who’s giving you like a very easy answer on that, you would probably want to reference your doctor.
But there is a problem for example with testicular cancer. They used to just treat everybody with radiation. But what happens is there are seven out of ten of those people they’re treating, or maybe even nine out of ten depending on what the risk factors were, who don’t need it at all.
Those nine out of ten people are just getting like sometimes pretty significant organ damage and side effects for no reason. They don’t have a very sensitive way to differentiate it. They can’t segment that population well, and so that’s why right now they don’t do that anymore.
For testicular cancer, if you have one testicle, then in general for almost everybody, you still have the exact same testosterone production, you have generally the same level of sperm production and quality and all of that.
Your quality of life shouldn’t really change very much if you have one. There shouldn’t be any change to your lifestyle. You’re still able to be like sexually active and all of that stuff.
But if you lose two, then you’re effectively castrated. If you lose two, that has a very significant quality of life effect because once you have that, then you are no longer able to produce any sperm.
You’re no longer producing testosterone. Your body would go through hormonal changes. You would start to have mood shifts and your personality might completely change as a result of that. You would be unable to have sexual intercourse basically. Your libido would go down.
All of these things would happen if you lose that. So they would never recommend doing a double orchiectomy unless there was real reason to.

There’s a small percentage chance of cases where somebody will get cancer in one testicle and then also get it in the other later in life. But it’s better to just wait till that happens.
Even if I went into some follow up like 10 years from now and they did an ultrasound and they saw a little bit of cancer in there or something, I probably still would not do an orchiectomy. You never know, it could be a slow growing cancer, it could take decades for anything to happen.
And so in that case, I’d rather wait and then when it does become a problem, I know that there’s effective chemotherapies that can be used. So I’d rather wait until they need to be used.
When were you able to work again?
Even a day after the surgery, I could work. I live three floors up. I was able to go up those stairs. I just moved slower and there’s pain when you move, so that’s it.
Your ability to function at work would probably depend on what types of medication you’re taking for pain, so you probably wouldn’t be able to operate any heavy machinery afterwards or do anything that requires really critical deep thought.
I had the surgery on a Friday evening. I had my co-founder over on Monday and we were working, but I was basically working from bed.
»MORE: Working during cancer treatment
How did your diagnosis impact your life perspective?
It makes you think about things in life and what you want to focus on and all of that. It makes you have one of these feelings like that. I think any time you have something that feels like a near-death experience, or something that makes you confront your own mortality, it makes you think in that perspective.
I had all these things flash through my head. It’s hard to emulate that kind of experience because it just has to feel that kind of real, I guess. For me it was a strong feeling of I wanted to spend more time with friends and family. I wanted to write.
Also, I felt like there’s things I’m working on, just on my professional side of life, there’s things I’m building that I hope will make an impact on the world. I’m like, “Oh, shit, I’m not going to be able to finish that.” So, yeah, I kind of had a lot of those thoughts.
Fertility
When did you first think of fertility preservation?
I thought about it as soon as I heard that there was a tumor. After the ultrasound results. I didn’t really know very much so I started Googling, looking around, and you can find pretty quickly that in general the male physiology, like everything works the same with one testicle versus two.
One is able to do the job of both, so that’s kind of like, if you’re gonna get cancer, at least it’s one that you have two of the organs for so you can have a backup.

Why did you decide on freezing your sperm (sperm banking)?
There’s still risks because there are things that can go wrong in the surgery. There’s things that could happen. The other thing is I’ve never done a fertility test in my life.
I didn’t know that apparently, if you have testicular cancer, you’re at risk for having low fertility to begin with.
I wanted to baseline things. I wanted to be like before I do the surgery, before I do anything else, I want to know if things were okay and then they got worse or whatever, even though it wouldn’t be clinically relevant probably in terms of prescribing treatment.
It just was something I wanted to know. I wanted to do a testosterone test because if two months after the surgery I’m feeling weird things or something strange, it would be helpful to be able to say, “Oh, well since the surgery, my testosterone has changed.”
I asked my doctor that and when I looked in the European documentations, they do recommend looking at testosterone and other levels before the surgery.
So I asked for that and he’s like, “Oh, sure.” I messaged, referred to a paper with the link and said, “So, I think I should probably look at this and this.” And he just responded, “Sure.”
Fortunately, the surgery didn’t seem to cause any fertility issues so I haven’t been through anything yet that would necessarily cause fertility issues. I think the thing that can lead to that is chemotherapy.
If you do the standard chemotherapy for this, it generally makes you infertile for some period of time and that could be a year, it could be like five years, it could be the rest of your life. That’s something that’s very hazy and they don’t really know how to segment people right now to be able to tell what effect it’s gonna have on which people.
They just kind of say that there’s a chance that you’ll be infertile for the rest of your life, but there’s chances that you won’t and so that’s one of those long term side effects that’s not great. The fortunate thing is you can sperm bank and that’s an option.
The doctors weren’t encouraging, “Oh, you should sperm bank before the surgery,” because, even though you probably should just in case something goes wrong, it’s very unlikely for something to go wrong during the surgery.
But before you do chemo, they 100-percent would recommend that you sperm bank if you plan to have children. It’s important in the future.
»MORE: Fertility preservation and cancer treatment
Describe the process of freezing your sperm (sperm banking)
[Depends on location of services.]
To put things in perspective, it’s a lot cheaper and easier than freezing eggs. You might even enjoy it. It’s a much easier process.
The first place I went to was on the order of $1200 or $1300 to do the initial banking, and then they charge $250 per year for storage for one sample. A sample would be one tube collected.
Generally in a visit, you’d give one tube, and you’re supposed to abstain from any sexual intercourse for four days roughly before you give the sample. So you can give one sample about every four days. If you have more than one sample, then they increase it to $450 per year.
That was the only place I could find that had any availability. I think way more of the people who are there are there for sperm donation at that place. It’s next to a college campus. I think just a lot of people are using that as a source of income.
In that case that I was able to get that appointment and find it was kind of expensive. But UCSF is where I ended up going. They have reproductive health services and so there it was on the order of $900, maybe $950 or so, and that gets you the sample and five years of storage.
Every time you do another sample, I want to say it’s something like $100 to $200 just to add another sample in there, something like that. But it worked out that it was cheaper, much cheaper long term than doing the other one.
When you give a sample, they separate that into vials and they generally say you want five vials to ensure pregnancy, to have the best chances. From one sample, you can get roughly five vials, so I think had five or six vials.
So you probably want to take into account that you’re going to need four days between any sample you’re giving, and I would think you might want to give something like three to four samples if you really want to be sure that things are going to be okay.
Any changes in the sperm tested before and after your surgery?
It was the same.
Advice to others on preserving fertility
I wish I had just banked sperm earlier on. So I recommend to friends now that there’s no reason not to bank it earlier on. But the fertility thing, I haven’t reached that hump yet.
That’ll happen when I get to the point of chemo, so that’s what I’m trying to [decide] right now: whether or not I do carboplatin.
If [the cancer] comes back, then I’ll have to make that decision. The only decision you can make in this whole process is whether or not you bank sperm. That’s all you have.

Inspired by Rick's story?
Share your story, too!
Testicular Cancer (Seminoma) Stories
Rick H., Seminoma, Stage 1
Age at Diagnosis: 34
1st Symptoms: Noticed one testicle larger than the other, dull pain
Treatment: Orchiectomy (surgical removal of one testicle), neoadjuvant chemo (1 infusion of Carboplatin)
Testicular Cancer (Non-Seminoma) Stories
Mikael H., Non-Seminoma, Stage 1
Age at Diagnosis: 32
1st Symptoms: Fatigue, one swollen testicle
Treatment: Surgery (removal and reconstruction), radiation, hormone therapy
Steve L., Non-Seminoma, Stage 4
Age at Diagnosis: 25
1st Symptoms: Grape-sized tumor on neck; hip and pelvis pain; ultrasound revealed tumor on right testicle
Treatment: Chemotherapy (BEP), removal of right testicle, lymph node resection (RPLND), and tumor dissection in the neck
Hugo T., Non-Seminoma, Stage 2B
Age at Diagnosis: 21
1st Symptoms: Pea-sized lump on right testicle
Treatment: Surgical removal of right testicle, lymph node resection, chemotherapy
Matthew O., Non-Seminoma, Stage 3C
Age Diagnosed: 24
1st Symptoms: Fatigue, one swollen testicle
Treatment: BEP chemotherapy, surgeries (including complications)




