Ashley’s Desmoid Tumor Soft Tissue Sarcoma Story
Ashley shares her desmoid tumor soft tissue sarcoma story and undergoing extensive chemotherapy, both IV and oral pills, for treatment.
Explore her in-depth story below, where Ashley also highlights how she handled stress management, how she approached work during treatment, and navigating the issue of fertility preservation. Thanks for sharing your story, Ashley!

- Name: Ashley W.
- Diagnosis:
- Soft tissue sarcoma
- Desmoid tumor
- Aggressive but no metastasis
- Age at Diagnosis: 28
- 1st Symptoms:
- Unable to walk after car accident
- Leg tightness growing worse
- Increased swelling in leg
- Misdiagnosis:
- Baker’s cyst
- How diagnosis happened:
- After car accident, leg wasn’t healing right. Pushed for an MRI after an ultrasound showed mass and was misdiagnosed as a Baker’s cyst.
- Treatment:
- 24 cycles of chemo infusion
- Methotrexate
- Navelbine
- Vinblastine
- Oral chemo (pills)
- Nexavar (sorafenib)
- 24 cycles of chemo infusion
To anybody who has also been going through a sarcoma diagnosis or any type of cancer diagnosis, I just want to encourage you that even though this is gonna be hard, you have the ability to get through the difficulty.
I think that the most important thing is to do your research, whether it’s you doing the research or somebody else is doing it for you, to find which doctors know about the type of cancer that you have and the best ways to treat it, and to surround yourself with a group of people who love and support you through the process.
Ashley W.

- Diagnosis
- What was the specific diagnosis?
- How did you get diagnosed?
- Pushing for a scan
- Did you advocate for yourself as a patient?
- Describe the ultrasound
- Describe the MRI
- Differences between the ultrasound and MRI
- How long did it take to get the scan results?
- Waiting for the results
- Describe the biopsy on your leg (origin of tumor)
- What was the news after the biopsy results returned?
- Where did you go for treatment?
- A different approach to treatment
- Treatment Decisions
- First Chemo (Infusions) & Side Effects
- Getting a port for chemo infusions
- Port surgery healing
- Did you like the port?
- Describe the chemo (24 infusions)
- How long did the infusions last?
- Describe the chemo side effects after the first infusion
- List all the side effects
- What helped you alleviate the side effects?
- Some hair loss (thinning)
- Did you get neutropenic (low white blood cell counts)?
- How was the Neupogen shot?
- What was the follow-up protocol after your first 24 infusions?
- What were the scan results?
- Second Chemo (Oral/Pills)
- Life Outside Treatment
- How did you manage the mental, physical, emotional stress?
- Giving yourself some grace
- How did you approach people for help in general?
- Advice to people who want to help patients & caregivers
- Were you able to work during treatment?
- You regret not taking more time off work
- How did you approach insurance and paying for cancer treatment?
- Anything else you wish you had known or done differently?
- Getting pregnant after chemo
- Ashley’s message to others
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What was the specific diagnosis?
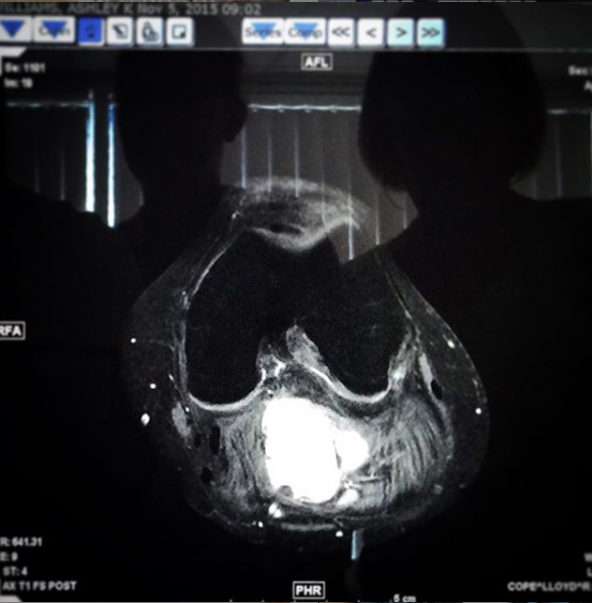
It is very aggressive locally, so the actual name of what I have is aggressive fibromatosis. It’s located in the popliteal fossa (knee pit) of my left leg, and so that’s the cavity behind my left knee.
It extends down back of my thigh and down back of my calf. There’s no staging with my tumor.

How did you get diagnosed?
I was in a car accident a couple months earlier, and I hit my knees against a dashboard. I went to physical therapy after that, and I was doing fine. I had my car accident at the beginning of June.
On October 31, I was unable to walk anymore. In between that time, I remember telling the physical therapy people I feel like someone is cranking my leg tighter and tighter.
Where your Achilles tendon is, I felt it was being cranked tighter and tighter. I kept mentioning to my physical therapist that I was very swollen and the swelling in my leg wasn’t going away. They kept saying, “It’ll be fine, it’ll be fine.”
Pushing for a scan
I decided to go to my orthopedic one more time. I asked him on multiple occasions if I could have an MRI done because I thought that I had a tear in my meniscus because I had pain around my knee. He was convinced that I had a Baker’s cyst.
He actually dismissed me. “This isn’t that big of a deal. You really need to stop coming in. It will work itself out.”
But he said, “Since you’re so freaked out about it, I’ll send you for an ultrasound.” So he sent me for an ultrasound and saw the mass and diagnosed me with a Baker’s cyst.
A couple of weeks passed before I wasn’t able to walk again. The day I wasn’t able to walk, I called my doctor. He said, ‘Ashley, something would be seriously wrong with you if you actually can’t walk. Are you sure you’re not just being dramatic?’
I said I didn’t think I was, so he finally sent me to an MRI and called me and told me about a week later that I had a tumor.
He says that he’s never seen anything like this in his career, so he didn’t know what to do with it.
Did you advocate for yourself as a patient?
The doctor was very dismissive, unfortunately. One of the things that I normally tell people is that prior to really any type of doctor’s appointment, I would recommend writing down a list of questions that you want answered before you get into the room with the doctor and you start to read their body language, their tone of voice, and the fact that they’re always in a hurry.
In my first several appointments, I would just be very accommodating to their schedules and the fact that they were so busy. I would forget everything that I wanted to ask.
I now write down all of my questions and make sure I go through with them with the doctor before to not minimize my own thoughts. I would often minimize my feelings based off their reaction.
»MORE: How to be a self-advocate as a patient
Describe the ultrasound
It all happened very, very fast. I was diagnosed and started chemo within a month of each other. Including the MRI and the ultrasound, it was probably a six-week process total.
I had an ultrasound, and the thing that they were most concerned about was the ultrasound tech noticed that I had a pretty large mass in the back of my legs.
Honestly for me, I didn’t realize how large it was because I have had issues with my left leg since I was a kid, and my left leg has always been larger than my right leg. But I had multiple tests done when I was a kid, and nothing showed up as being abnormal. The fact that my left leg is bigger than my right wasn’t alarming to me.
But when I went in for my ultrasound, it was obviously very alarming to the ultrasound tech. She actually started crying while she was doing my ultrasound, and she would just touch my leg in certain spots and be like, ‘Honey, does this hurt?’
It didn’t hurt. She just started crying and said, ‘You have something wrong with you.’
That was terrifying to me also. But the main thing that they wanted to check with the ultrasound as well is to make sure that the major artery in my leg wasn’t compromised or being strangled by the mass. It was a long process because they didn’t do an ultrasound on just the site locally.
They had to do it on my entire leg and check the artery basically from like the top of my hip area all the way down to my ankle. It was an hour to an hour and a half.
Just based on what I shared, that was alarming for me. That was of the beginning of like, “Okay, I have some things. There’s something wrong here.”
Describe the MRI
The next test that I did was the MRI, actually, because the ultrasound came back and showed a mass, but it doesn’t show contrast. He saw the mass and originally diagnosed it as a Baker’s cyst and said that there’s the potential that I might need to get it drained in the future, but it should be fine.
When I couldn’t walk and he sent me for the MRI, I had to have an MRI with and without contrast, which was the first time that I had had that done.
With the contrast is how it showed that it was a tumor.
The MRIs, for me, I still dread them because they’re very painful. My tumor is in the back of my leg, so when they put me in the MRI, all of my weight sits on top of my tumor because you’re lying flat. That first MRI was difficult because of that.
I had never really been in a position before where I had to not move and put weight on the tumor site. Again, that was a pretty alarming test, knowing that there was something that was off.
You have to lie down, and then they put you into — I don’t know any other way to really call it other than a tube. It sounds like a jackhammer for two hours. It’s just very loud banging noises for two hours while they run the machine.
It’s a long time to lie still. Especially when you’re in pain and also when there’s anxiety about, “Oh my goodness, one, when is this going to end? Two, what is wrong with me? What is happening?”
Differences between the ultrasound and MRI
For the ultrasound I had to lie down, but I could move and my legs were not straight out in front of me with all my weight resting on my calves. So my left leg I could kind of turn it so that the weight was on the side of my leg, and I could move if I needed to.
With the MRI they just stick you in a position, and you can’t move. I don’t recall that specific one, but I know the MRI that I have to do can take as short as 45 minutes, but I’ve had them take up to 2.5 hours before because I am naturally moving from the pain in my leg, which makes them have to redo it.
I vividly remember that one just because I had an MRI before, but you lay down, and you go into the tube. It wasn’t a standing one. They have to maneuver your leg and put cushions around it to make sure that it doesn’t move, but once you’re set and you go into the MRI, then they can’t touch it at all.
That specific one, I don’t remember how long it was, but every one of them has been probably an 1.5 to 2 hours to get them done.
How long did it take to get the scan results?
The ultrasound was a day or two. He may have called me later that day or the next day, but it wasn’t long.
The MRI, I’m pretty sure it was a week. The MRI showed that it was a tumor. That’s when I was referred to my orthopedic oncologist. I went there for an appointment on, I believe, November 12th. Then then he did a biopsy on my leg.
Waiting for the results
We all have our own ways of coping. For me, I had already determined that the worst-case scenario would be that I’d need surgery.
I was preparing myself the whole time, worst-case scenario, ‘Ashley, don’t worry. Surgery, you can do that; people do that every day.’ And I didn’t worry.
The last thing I expected was to have a tumor that came up in my life. I had just had the car accident, and so I was thinking more it was some injury associated with that, like a torn meniscus or something in my knee.
I did not expect the mass in my leg to be a tumor. I thought, “Of course, if my doctor knows what he’s talking about, it’s a Baker’s cyst, but it’s obviously being caused by something else that they’re going to uncover.” So I was 100% blindsided by the diagnosis.
»MORE: Processing a cancer diagnosis
It was maybe a little bit different for me, that waiting process, because I was on a completely different lane than, “Could this be cancer”?
I was hopeful during the waiting process because I had been in pain, I couldn’t walk, and the car accident had been three to four months prior.
I was thinking, “Okay, this is it; this is all I’m going to have to do. They’re finally going to tell me what’s wrong, what I need to do, get me walking, and I’ll be good.”
The waiting for me I would probably say was more aggravating just because you want to find out immediately, but it was probably very different than what most people experience.
»MORE: Patients describe dealing with scanxiety and waiting for results
Describe the biopsy on your leg (origin of tumor)
I think the orthopedic oncologist took eight samples. Basically I was in the doctor’s room, and I had to lie on the doctor’s table on my stomach. My family was with me at this appointment, and they had asked everybody to exit the room, so I was doing the biopsy by myself.
They position you, they sterilize you with the iodine, and they tell you that it’s going to feel like a pinch. They give you a shot first. They had to take a while to strategize where to do the biopsy because my tumor is entangled in the nerves, and it’s wrapped around the major artery in my leg.
They had to do an ultrasound there first prior to doing the biopsy in order to locate a spot where they could go in with the needle without hitting a nerve.

That took a little bit of time, I’d probably say 15 to 20 minutes to locate it. It doesn’t seem long, but at the time it seems like forever. Then they pinpoint the spot; they put a sharpie on the spot where they were going to go in. They do topical numbing. Then they did a shot in my leg, went in, and took I believe it was eight samples of my tumor.
I don’t want to be negative because I always want to encourage people that they can make it through whatever difficult thing they’re facing, but the biopsy was extremely painful.
My tumor was deeper than the shot of anesthesia could go, and the force of taking the samples caused me to get a Charley horse in my leg, but I couldn’t move my legs because they had taken so long to locate the spot.
I had a nurse literally holding down one hand on my calf, one hand on my thigh, and holding me down so that the cramping wouldn’t actually move my leg so they could still get to the spot, but it was painful.
After they took the sample, fortunately, this doctor’s office had the ability on site to test it. So about 45 minutes later, I got the official diagnosis. I just had to wait in the office while they sent the biopsy samples to test.
What was the news after the biopsy results returned?
I remember him coming back in after the biopsy and saying, “I have really good news for you. You’re not going to need surgery. You’re just going to need 24 rounds of chemo over the next six months.”
I was like, “What?” It wasn’t even an option in my mind that that’s something I would need. I was so confused by the way he presented it because he was like, “This is such good news.” I was like, “This is terrible news. What are you talking about?”
It all happened very, very fast. I was told I had a tumor on October 31. I was officially diagnosed November 13, then I started my treatment on December 10.
»MORE: Read different experiences of a cancer diagnosis and treatment
Where did you go for treatment?
When I was diagnosed, I went to an orthopedic oncologist, Dr. Temple. He referred me then to an oncologist hematologist, Dr. Cohen, who worked for the University of Miami.
Dr. Temple was located in Mercy Hospital in Miami, but they worked together on a work group of local doctors in the area who were trying to do research on what to do to treat desmoid tumors because there is very little research on them. There’s no verified treatment method. It’s all kind of trial and error.
I had to go every single week for treatment. I had to go to the University of Miami Hospital first to see my oncologist and get blood work done. He would approve me for treatment, then I would drive over to Mercy hospital, which is about 15 minutes away.
I’d get the infusion, and then I’d come home. That was for the first 18 treatments. Then the last six treatments I was able to get my infusion in my blood work transferred to a hospital that’s much closer to me.
A different approach to treatment
My doctors had done research and published a research article that used low-dose chemo to treat the tumor. I was told whenever I originally got the diagnosis that had I been diagnosed 10 years earlier, my only treatment option would probably be amputation. For the past several years, people who have desmoid tumors, it has been [the option].
Now this is coming from my doctor, and I trust my doctor. I say that as a disclaimer because surgery is still a treatment option, but my doctors told me that since it is so rare and it appears like a local tumors, the typical oncologist or doctor who is picking a course of treatment would typically send their patients for surgery to have it removed.
But their research has shown that those who have surgery have an extremely high likelihood of the tumor coming back and growing more aggressively and also growing resistance to treatment.

They actually say it’s more dangerous to get surgery than to treat it with other methods. They had done research on the combination of methotrexate and Navelbine, which is also known as vinorelbine, and doing that in low doses over the course of a year. That had shown to be very responsive.
But my oncologist told me at the very beginning that I was something like the 60th patient that he had treated in his career with this. It’s something that’s not common. Most people who are diagnosed with it in my area were sent to this team of doctors or one other doctor down here.
Treatment Decisions
What was your prescribed chemo regimen?
I received my official diagnosis and treatment option on November 13. They wanted to start chemo immediately because with my tumor type, it doesn’t shrink, so the chemo doesn’t make it disappear.
The way that they describe it is if your tumor is like a light, the chemo will cause it to turn the lights off. I basically refer to it as being like an active tumor versus an inactive tumor, but I’ve been prepared that I will always have the mass of the tumor.
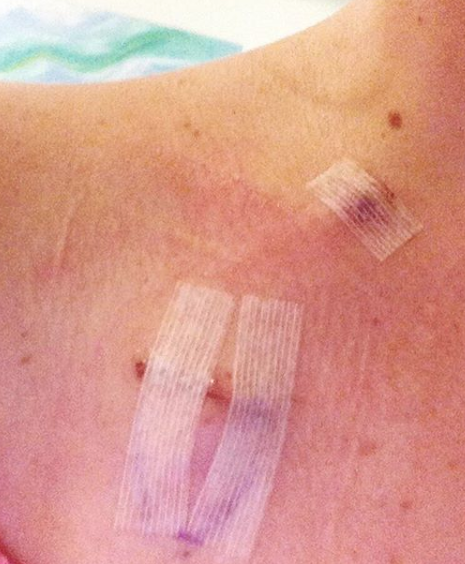
Because of this, they wanted me to start treatment immediately so that it wouldn’t grow any larger. It was the holidays, so it took some time to do some scheduling. I went in to get my port put in on December 2 at the University of Miami Hospital, and then had my first infusion on December 10 at Mercy Hospital.
Prescribed medicine with chemo
I am someone who does not love taking medication. I very rarely take Tylenol or anything, and so I was prescribed quite a few medications to take with the chemo.
Primarily Zofran, which is the anti-nausea, and then Bactrim, which is an antibiotic that they wanted me to take. I don’t remember how often. I feel like it was every day. The antibiotic was to ward off any infections that could come.
I chose the first time not to take the anti-nausea meds because I wanted to see how I would do on the treatment and if I really needed to take that much medicine, which was a terrible mistake.

Describe your first visit to the hospital
I was terrified, and I went to a hospital that had a lot of people having chemo at one time. There would often be 10 to 15 people in the room, and there would be only one chemo nurse.
For my first time, they were very attentive and put me in a room by myself, but there was only one private room, and there was one very large room where everybody sat together.
I remember being terrified because I was still healing from the port. I had only had it in a week before. It was uncomfortable, and they were going to access my port. That’s the one thing that I had looked up: the type of needles that they use for that.
Heparin solution
The first thing that they put in is the Heparin, which is like a cleaning solution for your port. When they put it in, the first thing that they asked me is if I could taste it, and that’s how they knew whether or not the medication was getting into my system.
I don’t know if you ever had Heparin. That stuff is the worst, and to this day I cannot even be anywhere near anything that smells like rubbing alcohol. It makes me nauseous. I wasn’t expecting to taste it.
I thought that that was very weird, and so that was the initial nauseating thing for me, the ability to taste it. I don’t even know how I would begin to describe to someone the sensation of having the medicine pump into your port. That was a very odd sensation.
You went to two hospitals. What were the differences?
This could make me emotional because it’s one of those things that you don’t realize — the [importance of] care that you’re receiving until you receive care from multiple places and you have something to compare it to.
At the first place, everyone spoke Spanish My nurses spoke Spanish, and I don’t speak Spanish, so I could barely talk to my nurses. There were 15 people in a room, one nurse. They didn’t wipe down the chairs in between people. But I just assumed that that’s what chemo infusions were.
Then when I came up here to Holy Cross Hospital, there was one nurse for a station, and a station had two to four chemo chairs. They would fill up the station, so there’d be one person you’d put at each station, and then they’d start filling them in cyclically.
There were times where there was one chemo nurse dedicated to me. I think there was only time where that nurse had two people, me and somebody else.
I had my own like little area that was set up with magazines and a TV. They had a little kitchen with snacks, which I would never eat anyway, but there was also water and stuff like that.
The previous place there wasn’t a TV. I’d bring stuff to do myself. But at the second place at Holy Cross, they could hook the line up to the port and take my blood, test it, come back, administer the chemo. I’d only have to get stuck once. Everybody was super kind, so I could communicate with everybody. It was a night and day experience.
In the first location, I was having an IV drip for both of my medications. In the second location for the chemo, they gave it to me in a syringe, and the nurse sat with me for 30 to 45 minutes as she slowly pushed the medicine into my port through a syringe. I asked her, “That’s interesting that you’re doing it that way because at the previous place, they put it in an IV, in a bag.”
She said, “We have to do it in a syringe because if anything were to happen and your line were to back up and the medicine were to leak onto your skin, you would have a third-degree burn from a drop of this stuff on your skin. So there has to be somebody here checking to make sure that there’s no backflow of the medication; it’s the safe thing to do with the patient.”
So I just felt very, very comfortable at Holy Cross. I felt taken care of, and at the previous location I’m thankful that I didn’t realize how bad it was until I left. But now that I’ve been somewhere else, the first place was not a great experience.
Obviously a very important level is just your safety. It sounds like that was compromised. And then on another level is just people don’t understand how important it is to have these little things go well. The quality of life stuff.

Any advice to others looking for a place for treatment
I think people have a tendency to minimize things because going through something like chemo is seemingly so dramatic and affects so many people that the little things, at least for me, I didn’t want to make a big deal out of it. At least I was getting the treatment I needed. At least I knew I’d get the infusion by the end of the day.
But it is the little things that make the world of difference. From a mental health standpoint, it’s a very traumatic experience.
And all of those little things, there are a lot of things that happened at that center in Miami that I still mentally go back to sometimes. It just was so horrific in addition to what you’re already going through.
Something as simple as sanitary and clean, like wiping down a chair, makes the world of difference. And that I’m not just another number of somebody who is getting chemo administered today. There’s someone coming around bringing me a water bottle or says, “You know, it looks like you’re uncomfortable in the way that the needle is positioned. Here, let’s try this and make sure that you’re comfortable.”
Rather than just I’m part of a chemo mill, you know? That’s how I felt at the first place, that I was just a part of their normal process. At Holy Cross I felt like a person.
First Chemo (Infusions) & Side Effects

Getting a port for chemo infusions
I think that that’s the thing that my brain decided to focus on as the most scary part for me.
I had probably given blood like three times in my life prior to that, so I was afraid of needles and didn’t know what to expect because I knew that they wouldn’t be putting me to sleep. That terrified me, too.
I was literally in the waiting area, and even when they brought me back to my little bed to prep me, I was uncontrollably shaking. The nurses could not find a vein in me either, and they said that was either because I was dehydrated or anxious. They had to put [the IV] on the inside of my left wrist, like a little vein right there.
As soon they gave me the medicine, they wheeled [me] into the operating room. It’s super intense because there’s tools everywhere, people everywhere with their masks, their shoes covered, and their stuff on their head. I don’t know if it’s an X-ray, but they project your chest cavity on a TV screen that you can see.
As soon as they gave me the medicine, it was like I knew everything that was happening. I knew that they were doing surgery. I could feel the pressure in places even though I didn’t feel the pain. I knew exactly what was going on, but now I just didn’t care at all.
I tried talking to the doctors. They would say things, and I would try responding to them. Words would come out, but I have no idea what they were. I remember them saying to me, “Don’t worry, Ashley. You don’t have to talk to us.”
It was a lot of buildup for me because I was terrified, but it was probably the experience that needed the least amount of buildup because it was not painful. Once they give you this medicine, it wasn’t scary. It was pretty quick.
It’s just a very strange feeling when they put it in. I got it put in, stitched up, and they covered it with one of those Band-Aids that can’t get wet for like a week. I didn’t uncover it until the following week, whenever they accessed it for chemo.
Port surgery healing
It was sore, but it wasn’t painful. I think they gave me ibuprofen for the soreness. I remember it being sore and weird, because you learn your body, and now you have this little golf ball sticking out of your chest.
I remember hitting it on things, and I’m confused as to how I would hit something on that so often. It’s in such a weird spot that you’d constantly hit something on it. But it was fine.
Did you like the port?
It went well. At the first location that I had treatment, they had the numbing spray that they sprayed on it, so I didn’t feel anything. Again, I remember being terrified because I didn’t often have to deal with needles at that point. Everything went well, all things considered.
I think for me my port has always been symbolic, and I’ve always thought, “Okay, this will truly be over once the port comes out.” My doctor prepared me that after my four-month checkup, if all was well, the port would come out. So I was expecting it to come out four months after my treatment ended, and it didn’t. Just because my tumor had kept growing. I kind of had to accept it as a part of me that may be here for an extended period of time.
Yes, I’m proud of it. I’m not interested in hiding it; it’s not an experience that I’m ashamed of. But I think it still also represented that I [was] in the middle of a battle that I [had] yet to overcome.
Describe the chemo (24 infusions)
Methotrexate, vinblastine, navelbine
They were every Thursday. The entire process included me driving an hour to get to the hospital, going to one hospital to get my blood work, going to another hospital to get the infusion, and driving home.
That entire process probably took about 10 hours every Thursday, but the actual infusions themselves I would say took on average two hours. I was in a very, very high traffic office where I was getting my chemo, where administering chemo was not the only thing that they did.
How long did the infusions last?
I never really knew what to expect for my first 18 rounds of treatment. I would say that the first one was an 1.5 to 2 hours, but then from there it varied anywhere between 45 minutes and my entire day.
I had two separate chemos, the methotrexate and the vinorelbine, and at the first location, they were both administered by a chemo bag, like a drip. They didn’t do any saline.
At my second place they did it completely differently, so I had two very, very different experiences of how they administered the medication, too.
Describe the chemo side effects after the first infusion
With the first time, I remember feeling very strange when I left, but I wasn’t nauseous, and I wasn’t feeling bad. I remember leaving, and I felt a little spacey, but I was like, “Hey, maybe I can do this. This isn’t too bad.”
It was the middle of the night, so maybe eight hours later, that I just was very, very sick. I have always described it to people as a mixture of being very, very drunk and having food poisoning at the same time.
It’s a terrible way to explain it, and it’s a terrible thing to put my name on, but I just said that. It was like food poisoning, but it was also that feeling of like, “If I close my eyes, the entire world around me is spinning, and I just would rather not close my eyes.” I slept on the bathroom floor that night.

List all the side effects
- Nausea: often vomited a few hours after infusions
- Frequent headaches, migraines: never had any before treatment
- Intense fatigue: so bad I chose not to eat because the kitchen was too far away
- Loss of appetite/extreme hunger: these would come and go in waves
- Eyes sensitive to light
- Low ringing in ears
- Bad taste in mouth
- Hair thinning
- Major brain fog
I had vinblastine mixed with methotrexate. At one point they also switched it to a combo between methotrexate and Navelbine (vinorelbine). It’s nearly impossible for me to distinguish what was specific to vinblastine.
What helped you alleviate the side effects?
- For nausea: Zofran
- For headaches: thieves oil (essential oils of clove, lemon, cinnamon, eucalyptus, rosemary)
- For bad taste in mouth: eating pickles
- For all side effects: hydrating frequently
Zofran was amazing for that first round of treatment (chemo infusions). This round of treatment (oral pills), it does nothing for me, which I think is the strangest thing. But the first round, Zofran was amazing.
I had a lot of side effects to the Bactrim, that antibiotic, so I was only on that for a couple of weeks. That’s also something that my doctor says. Had I been on the Bactrim, I might not have gotten so sick that one round. But Zofran was really the only additional thing I was taking at this time.
This sounds really strange, but the taste in my mouth was so terrible all the time, and the taste, a lot of times, is what would make me nauseous.
I also had a post-nasal drip with the chemo. I ate pickles all the time. It was the only thing that alleviated some of the taste in my mouth. I ate pickles all the time.
After my treatment, I would just use thieves oil. I don’t know if you’re familiar with that, but it’s a mixture of five different essential oils that are said to be antiseptic and clean the air.
I would just use that after every treatment, and that would help me. It has lemon, cinnamon, eucalyptus, cloves, and rosemary in it. So those five things. That would help me with my headaches. I very rarely got headaches when I was just using that.
I very seriously can tell you that there was a major difference the week that I did make it a priority to drink lots of water, that my side effects were much less.
I just would get nauseous with the thought of drinking water, too. So I wasn’t quite about it. But the weeks that I was intentional, it was a different period.
»MORE: Cancer patients share their treatment side effects
Some hair loss (thinning)
I never lost my hair completely, but my hair thinned dramatically. I ended up going to a dermatologist because after one week when I got sick and my hair started coming out, I also started developing like an allergic reaction, and so I was getting patches of hives.
I went to a dermatologist, who also checked my head, and she told me that I had lost about 70% of my hair, so I never lost it completely.
I have very, very thin and very, very fine hair, and so for my hair to be thin, it didn’t faze me. My oncologist did tell me that it was much more likely that it would thin than fall out in clumps, but it was always on the table as a potential.
»MORE: Dealing with hair loss during cancer treatment
Did you get neutropenic (low white blood cell counts)?
I was, once, toward the end of my treatment. It was in April, so it was about four to five months in. I got viral laryngitis, so I had a virus of my vocal cords.
That’s when I had to go in and had to get Neupogen shots to increase my white blood cell counts.
How was the Neupogen shot?
I know that they say that you’ll probably have a lot of bone pain on the Neupogen, but I didn’t notice a ton of bone pain. So the Neupogen shot didn’t seem to negatively affect me.
What was the follow-up protocol after your first 24 infusions?
They did a scan every three months. They did it twice while I was getting the IV chemo.
Originally, I was prescribed a full year of weekly treatments, so 52, but my tumor had responded to that mix of chemo. So at 24 they decided to put chemo on hold.
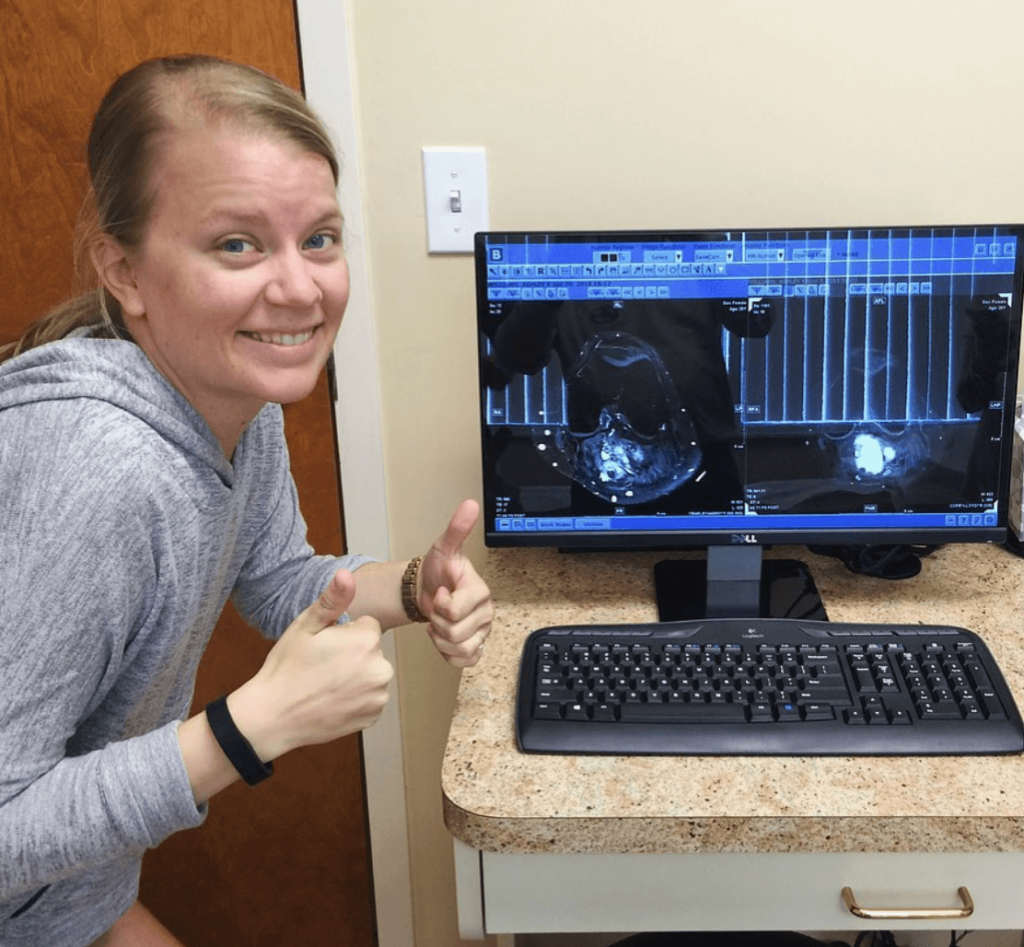
They showed me pictures of the scans. The active cancer lights up, and the inactive cancer doesn’t. The difference between my scans were extremely noticeable.
Throughout that time I had been working with the therapist, so by the end of my treatment I was walking, too, which was great. There were so many different things that were encouraging along the way to show me that it was working.
After that they wanted me to continue to get scans (MRIs with contrast) every three months and to continue every three months to come see him for a checkup. I don’t remember if it was three or four months, my three- or four-month checkup after I finished. Chemo ended on June 9.
I ended not knowing that it was the last one either, so I didn’t necessarily celebrate or do anything like that because I thought that the scan would show whether or not I needed to go on to 52. I knew that it could have, but I wasn’t sure.
At my next checkup, they weren’t comfortable with the reaction my tumor had. They did tell me that once the chemo infusions were over that the chemo would still be working on the tumor for up to a year.
That’s why they put me on hold. They wanted to keep checking me to see if there was a continued response. They weren’t comfortable with the next scan, which is why they did not approve for my port to be removed.

What were the scan results?
I had an MRI with contrast in September or October, and then I had another one in December or January. It wasn’t that it was bad; it was just progressively not giving them the level of response that they wanted to see.
In June 2017 for that checkup that I went to, they prepared me that I would probably start chemo again in the new year. They gave me a prescription of a very high dosage of naproxen that I took every day.
After about two months, I could tell that naproxen wasn’t really working. My leg felt swollen all the time. I called them, and they changed me from naproxen to another medicine called diclofenac.
That was very helpful in my mobility, all of the soreness, and the stiffness in my leg. It is not used to treat the tumor, but it’s used essentially to help keep you off of chemo for a longer period of time. It makes it not reactivate as quickly.

Second Chemo (Oral/Pills)
When did you learn you needed additional treatment?
When I went back in November 2017, I was told that I would need more chemo. I don’t have a percentage per se of how much it decreased with the infusion, but it had decreased to the point where the doctor felt fairly confident enough to take me off of the chemo, give it the year after to still be working.
When I was told that I needed to prepare to go back on chemo, they explained it like my tumor is almost like a knob of ginger or something. It has those little knobs that come out of it. The heart of the tumor is still inactive, but there’s little spindles that are coming off active and growing pieces to it.
I grew a golf ball size [mass] coming out of the back of my calf. When I was originally diagnosed with this, I did not have that. It just looked like my leg was swollen.
About four months after my chemo infusion, I noticed this lump starting to develop. The golf ball coming out of the back of my leg was a spindle that shot off of the core of the tumor [before] attacking those pieces of it, if that makes sense.
There were complications finding a specialist
I went to my oncologist, and he told me that he could no longer carry my case. He had an office at the University of Miami Hospital. but he actually worked independently for something called The Orthopedic Association, which at the time was the name of it.
Dr. Temple and Dr. Cohen were both involved in that association, which is how they were connected to each other and referred to me to each other.
In November 2017, Dr. Cohen told me that he was no longer going to be working independently but that he would begin working for the University of Miami as an oncologist for specific types of cancer that wasn’t what I had. He switched my doctor to a Dr. Wilkie. He then scheduled an appointment for me to see her in December of that year.
The waiting that had to happen between my appointment with Dr. Cohen where he told me that he wouldn’t be able to be my doctor anymore and that meeting with Dr. Wilkie was probably the most anxiety-provoking waiting period ever.
I think when you go through something like chemo, I honestly believe that there is PTSD attached to it. I’m a therapist; that’s my job. I could not wrap my head around having to go back to the treatment, and I just really struggled with that.
I didn’t know what this other doctor was going to prescribe me. I had been told so many times that there were no other doctors in the area that treated this. I really struggled.
Treatment options
The specialist told me that I had two options for treatment this time. One was an infusion that would happen once a month of something called doxorubicin, or I could take the oral chemo.
They both have been shown to have pretty positive outcomes for people, but the doxorubicin, the major side effect is an allergic reaction. I had had a pretty severe allergic reaction to the previous chemo, so they wanted me to try the oral chemo first, which was great for me to hear obviously.
Describe the second chemo (oral/pills)
January I started the oral chemo. It is the first time I’ve ever had to work with a specialty pharmacy for medication and that process was really easy. The whole insurance process and everything with the oral chemo has been very easy, which I’m grateful for.
I started it on the 12th. I take 400 mg a day, which is two pills. I take one in the morning; I take one at night. After about 10 days of taking it, the first time I broke out in hives over every single surface of my body. It was everywhere. I had to stop. I had to go on a steroid pack, and then I started again.

What were the side effects?
When I started again, I got very sick. I got the flu essentially, and I got another round of the same viral laryngitis that I had before. I had to stop, and I restarted for a third time in March.
They were nervous about the rash, an allergic reaction, because most people who start having an allergic reaction with this medicine never adjust to it, but my doctor had me take Claritin and had me do a step-up approach.
She had me on one pill a day for a week, and then the next week it was one pill one day, two pills the next, one pill the next, two the next, and we’d go back and forth for a week.
After two weeks I was up to the full dosage, and with that and with the Claritin, my body was able to handle it. I haven’t had an allergic reaction, so that’s great.
»MORE: Cancer patients share their treatment side effects

Follow-up protocol
I had a MRI done in June. I would get blood work done every two months and get a MRI with and without contrast done every six months. In June, it was obvious that my tumor was responding. She said it’s responding very slowly, but it’s responding.
I was originally prepared for six months to a year. December will be almost a year; at that checkup I will either be told I’m done or there’s a potential to be told I have another year because you can be on it for up to two years at a time.
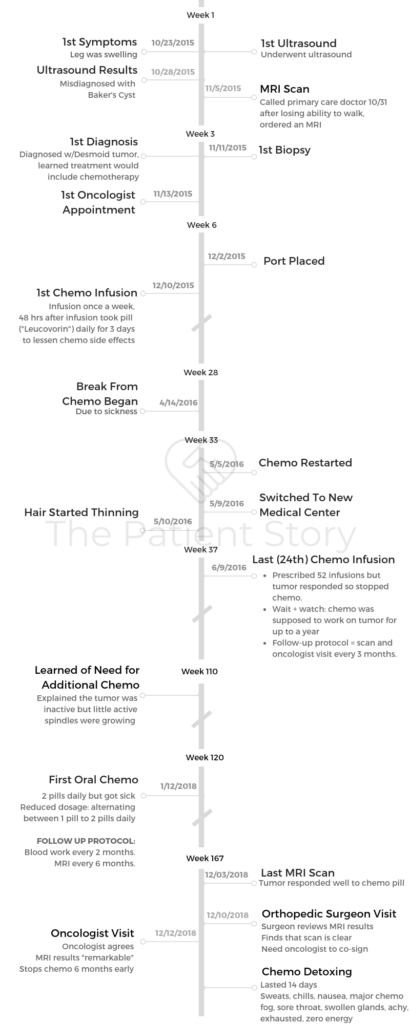
Editor’s Note: In December 2018, after Ashley’s initial interview with The Patient Story, she underwent another MRI. The results were the best any of us could hope for. Here was her update on social media:
After reviewing my MRI, the oncologist said my results were ‘remarkable.’ Remember my ‘white glowing mass’?
Well, this MRI had ‘almost no’ white, which means ‘almost no’ active cells. Here’s to the end of a chapter, and the beginning of a new one!
The world is my oyster.
Life Outside Treatment
How did you manage the mental, physical, emotional stress?
I think one of the most important things for me is realizing that life doesn’t stop with the diagnosis, and life doesn’t have to stop with the diagnosis.
I made a very intentional effort to try new things, to do things that I love, and to be around people who are positive and who are supportive. For me, church is a good thing to you and that group of people who are supportive, but those are the main things I would say.
Understanding that life is not over; there is life after cancer, and there is life after treatment.
There are people who are supportive and who love you and to allow yourself the time, the space, and the forgiveness to process. Then walk through what your experience is. I think a lot of times we’re hard on ourselves, but [it’s] how we handle our experience and the difficulties that we experience. How some days we want to complain and some days we just don’t want to do it anymore. I can’t tell you how many times I’ve said that: “I just don’t want to do this anymore.”
Giving yourself some grace
I think forgiveness for ourselves is a really important piece of that, too, and just being kind to yourself. Cancer and chemo is a lot, and it is hard, and it is traumatic, and to expect that.
Accept[ing] that it has been painful and hurtful, and difficult is okay, and a necessary part of overcoming it.
How did you approach people for help in general?
My parents and my sister live here, so my initial reaction was, “How can I manage this in a way that is the least intrusive on everybody else?” 24 treatments down in Miami is a lot.
I can’t walk. I have a dog. I live in a townhouse on the third floor. He’s going to need to go out, and I can’t get out of bed. How do I do that? I have a kitchen that’s not on the same level as my bedroom, and I can’t make it downstairs to get water or food.

It was a lot to ask of people. My job was very good to me and my parents were there, but I would say that I didn’t have much additional support. I didn’t have people bringing me meals or anything like that. That kind of thing would have been really nice.
I think people don’t know what to do, and they don’t know what to say. They don’t want to intrude, and then if you have the type of personality where you don’t want to be intrusive, then it can cause it to be a pretty isolating experience.
My encouragement on both ends of that would be if you are going through treatment to speak up.
This is the time to ask people for help and to receive help, and that something as small as my roommate or my neighbor taking my dog out for me in the middle of the day was something that would make me cry, because I felt like they were doing so much for me.
Advice to people who want to help patients & caregivers
I would say kind persistence is appreciated because there are things that you can do, but I just think that the common thought is, “I don’t want to be even more of a burden than I already am.”
I can give it from a therapeutic angle of ensuring words go a long way and ensuring people that they’re not a burden or that they’re worthy of having help. That you want to help, that it’s not a burden to help. All of those things, I think, are really important to hear.
When I think you’re looking at someone who’s going through something like chemo, someone’s reaction would be, “Well, of course. My heart breaks for what they’re going through. I genuinely want to help.” So to communicate that genuineness is really important.
»MORE: What kind of support cancer patients say helped the most

Were you able to work during treatment?
Yes, I have worked at the same place for several years, and they have been very, very good to me. That’s one thing that I have to say I have not had any issues with work going through this process. I worked full-time through both of my treatments.
For the first one, I had an arrangement with my job where I could be out on Thursday and Friday, and I worked my 40 hours Monday through Wednesday.
The entire six to seven months that I was on that round of treatment, I think I took eleven vacation hours. If I could do it differently now, I would definitely take the time off, but I think it was just such a welcome distraction at the time.
They were great. If I started feeling sick at work or something like that, I could work from home. That was huge for me.
I needed my job; I needed the insurance obviously. That year when I had the infusions, I had like over 100 doctors appointments that I went to in that year period. It was crazy.
»MORE: Read more on how others dealt with work after a cancer diagnosis
You regret not taking more time off work
When you’re going through the treatment, I think your goal, honestly, is survival. You think, ‘I just have to get through this, and then I’ll be okay.’
I wasn’t prepared for after chemo. After chemo was probably harder on me just mentally and emotionally, because I hadn’t allowed the time during treatment for me to do any type of emotional processing for it.
I felt I needed to get all of these things done. I just needed to get through it. I just needed to persevere.
Now looking back, I wish I would have taken the opportunity to build in some space to be able to grieve everything that was happening, to be able to process everything that was happening, but I didn’t. I did that afterwards.
It’s been almost 2.5 years since I ended my first round of IV chemo, and I’d probably say I’m still working through things associated with this diagnosis and treatment that I wish I would have just taken the opportunity to do that.
»MORE: Read more on how others dealt with work after a cancer diagnosis
How did you approach insurance and paying for cancer treatment?
I was on FMLA (Family and Medical Leave Act) because we didn’t know how treatments would go. I was 27 when I was in the car accident, and I was 28 when I was diagnosed.
My insurance renewal is in April, and everything happened between June and December. I was young and didn’t opt in to short-term disability, didn’t opt in to accident insurance or anything like that.
I opted in for the cheapest base-level insurance, just thinking that I am young and healthy, and I’ll be fine. But I did have FMLA. My job would have allowed me to take the time off.
I had the hours and the ability to do so. I was encouraged to do so on several occasions, but I didn’t because mentally I just think it was better for me to keep working.

Anything else you wish you had known or done differently?
That’s a tough one because there’s a lot of things I wished that I could have done that realistically I would not have been able to do.
For example, I was diagnosed mid-November and started treatment. Because I started treatment at the end of the year, I met my full deductible by the end of December, and then I met my full deductible for the next year by the end of January.
So I had two deductibles that I had to meet [and] had to pay within two months.
But in reality, when you get a diagnosis like this, you don’t have the time to plan out, “Oh, let me start that at the beginning of the year so I only have one deductible.”
I wish. But I’m surprised that it was as smooth for me financially as it has been, just with my insurance helping.
The one thing that I did opt into at work several years prior to this was a health savings account (HSA), and I have been putting in the maximum amount that you can put in annually. I probably started doing that two years prior to my diagnosis.
Financially, that is probably the thing that kept me afloat when I had to meet those two deductibles. I had at least one of my deductibles in my HSA account.
If I could recommend anything, it would be that. That is literally what made it possible for me.
Getting pregnant after chemo
There are a couple of support groups online that I’m a part of, whether it’s people with my type of tumor who have been pregnant and who have been fine.
There are other people who have gotten pregnant and it’s triggered their tumor to start growing. My tumor is very large in the back of my leg, and so there’s not much room for it to grow without it compromising my leg.
While pregnancy in the future is definitely something that I have been told is an option for me, I have also been told that the likelihood of it triggering my tumor to grow is very high.
Since my tumor is so large, there’s a possibility that I would not be able to wait till after the delivery to start chemo at that time.
I have pretty much been prepared that if I were to get pregnant, I would either be on chemo for a while pregnant, or I will be on chemo immediately after. Those are really daunting things to hear.
There is hope in becoming pregnant one day. I’m not in a position right now where that would be a life choice for me, but I am sure it will be something that will be very difficult for me.
It’s difficult for me now, even thinking of the options that I have, but I’m sure that when that time comes, when I’m married and talking about starting a family, there will be a lot of pros and cons to it.
My natural inclination is I would never want to put a child through chemo, so my natural inclination is accepting that that’s not the future that I have. It’s not a no, but that’s where I’m at now.
»MORE: Fertility preservation and cancer treatment
Ashley’s message to others
I was diagnosed with aggressive fibromatosis, a type of desmoid tumor, which is a type of sarcoma, at the age of 28. To anybody who has also been going through a sarcoma diagnosis or any type of cancer diagnosis, I just want to encourage you that even though this is gonna be hard, you have the ability to get through the difficulty.
I think that the most important thing is to do your research, whether it’s you doing the research or somebody else is doing it for you, to find which doctors know about the type of cancer that you have and the best ways to treat it.
And to surround yourself with a group of people who love and support you through the process. I think that that is the most important part to this process.


Inspired by Ashley's story?
Share your story, too!
Desmoid Tumor Stories
Ashley W., Desmoid Tumor
Cancer details: Rare, <3% of all soft tissue tumors, more common in women
1st Symptoms: leg tightness, increased swelling in leg
Treatment: Chemo infusion (Methotrexate, Navelbene), oral chemo (Nexovar)
...
Demi D., Desmoid Tumor
Cancer details: Rare, <3% of all soft tissue tumors, more common in women
1st Symptoms: fatigue, lump in hip
Treatment: Surgery, radiation, chemo
...
Alicia B., Desmoid Tumor, Stage 4
Cancer details: Rare, <3% of all soft tissue tumors, more common in women
1st Symptoms: lump found in right armpit
Treatment: Chemo, radiation, targeted therapy, clinical trials, surgery, including forequarter amputation
...


