Bruce’s Gleason Score 8/9, Stage 4A Prostate Cancer Story
Bruce shares his stage 4A prostate cancer story, Gleason score 8/9, which began with a diagnosis at just 51 years old. He details going through a radical prostatectomy (surgery), salvage radiation, and hormone therapy.
Explore Bruce’s in-depth story below, where he highlights many important quality of life topics, including the impact of hormone therapy on sexual function, the importance of self-advocacy and awareness, why it’s important for men to share their stories and ask questions, and the transition to survivorship.
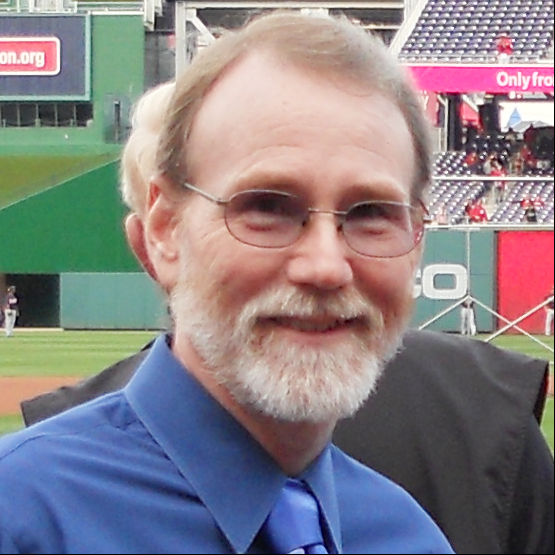
- Name: Bruce M.
- Diagnosis (DX):
- Prostate Cancer
- Gleason Score 8/9
- Stage 4A
- DX age: 51
- 1st Symptoms:
- Velocity change of urination
- Discovered cancer after brother was diagnosed with aggressive form of prostate cancer
- Treatment
- Radical prostatectomy: surgery to remove entire prostate and surrounding tissue
- Salvage radiation
- 6-weeks
- Every Monday-Friday
- Hormone therapy
- Casodex
- Lupron shot (three years)
The phrase that I hear people say is that it’s living with cancer. That’s really appropriate. I’m living with that knowledge that it could come back. It might get me in the end, I have no intention of it doing so, but it’s something I just realize is part of my life now.
I’ve accepted it as okay, that’s just what it is, I’m just going to move on and keep living my life. I think it’s really just not letting it rule your life, just knowing it’s a part of your life, and you want to rule it as opposed to it ruling you.
Bruce M.
- Meet Bruce
- Video: Bruce on Getting Diagnosed
- First Symptoms and Test
- What were the first symptoms
- What happened at the first doctor visit
- Your brother’s prostate cancer diagnosis pushed you to get tested
- Was your brother going through prostate cancer treatment at the time
- When did you realize you may have prostate cancer
- What is the PSA test
- How long did it take to get the PSA level results
- Getting Diagnosed with Prostate Cancer
- Describe the urologist meeting
- Results of the second PSA test
- Describe the digital exam
- Describe the biopsy
- Recovering from the biopsy
- Issues of infection post-biopsy
- When did you get the results from the biopsy
- What was your layman’s understanding of the Gleason score
- How did you process learning about prostate cancer
- How was your conversation with your urologist about prognosis and treatment
- How did you and your wife process the diagnosis
- Treatment Decisions
- Video: Bruce Talks About Treatment
- Prostate Surgery (Prostatectomy)
- What was important to know heading into surgery
- Changing diet and exercise pre-surgery
- How was the prep before surgery
- How were you mentally prepared for the surgery
- Describe the CT scan
- Describe the bone scan
- Results of the scans
- Describe the prostate MRI (with rectal probe)
- The value of the prostate MRI
- Undergoing a pre-op physical
- How were you feeling going into the operating room
- What do you remember of waking up from surgery
- The surgery was quick in part due to your weight loss
- You had undergone a robotic surgery
- Recovering from Prostate Surgery (Radical Prostatectomy)
- Planning for More Treatment
- Salvage Radiation
- Hormone Therapy: Casodex & Lupron
- Video: Bruce on Quality of Life and Reflections
- Reflections After Treatment
- Keeping up with good diet and exercise
- Concerns about sexual function after surgery (prostatectomy)
- Keeping a sense of humor
- Survivorship
- What’s your message to other men on the importance of sharing, expressing, asking
- What does self-help mean (self-advocacy)
- The power of sharing your story
- Taking care of yourself after treatment
- Your "different" normal
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Meet Bruce
Tell us about yourself outside of cancer
Passionate about scuba diving though I don’t get to do it often now. I’ve been diving since I was a little kid. My older sister scuba dove and got us into that. Used to live in California and did that as a youngster.
I became a scuba instructor in 1983. The first (PADI) instructor class held in Egypt is where I got my instructor certification.
I was there for a couple of years with my then-girlfriend now-wife, Lisa, whom I met in college in California (see picture).
I love diving into the water. It’s very comfortable!
Video: Bruce on Getting Diagnosed
First Symptoms and Test
What were the first symptoms
I noticed that I couldn’t really control the velocity of my urination. Whether that was due to the prostate cancer or not, I’m not positive specifically, but at the time it was a bit concerning. But I was also getting older.
What happened at the first doctor visit
The doctor looked at it and did a digital exam. The conclusion given back to me was it probably was just me getting older. There was a blood test I could do but it wasn’t really reliable, it was controversial,
Besides, I was ‘too young’ to think about those things, anyway. I was 48 at the time, so they didn’t think it could be an issue of prostate cancer.
I had never even heard of prostate cancer and it was never mentioned in the discussion with the doctors. So at that point, I didn’t think much of it anymore, just chalked it up to me getting older.
Your brother’s prostate cancer diagnosis pushed you to get tested
It wasn’t until later in 2012 when my older brother contacted his male siblings and said he’d been diagnosed with a very aggressive prostate cancer. He recommended we get tested.
I planned to do that but I couldn’t recall what kind of cancer he mentioned. That’s the problem with the lack of advocacy. It just wasn’t in the normal, daily lexicon.
We just don’t know about it as younger men. Older men are much more versed in it because it’s known as an older disease, in general.
So when it came time to make the appointment, the medical staff asked what kind of cancer my brother had. I was thinking it was colon cancer. So I went and got my colonoscopy, which came out with flying colors.
I hadn’t heard of prostate cancer, so it wasn’t in my mind. That could have been a fatal mistake, and nearly was so.
It wasn’t until later in the fall that my brother followed up and asked if I had gotten my test. I said yes, that I had gotten my colon test and it was perfect. He said no, it’s a prostate test you need to take, the PSA, not colonoscopy.
So I called my doctor again and made an appointment to get tested for the PSA.
Was your brother going through prostate cancer treatment at the time
My brother was scheduled for surgery. It had escaped his prostate into other organs, so he had a much more dramatic surgery than I did.
When did you realize you may have prostate cancer
When I got the results from my physician on the first PSA test, she called me up and said she’d schedule an appointment with me with the urologist right away.
That’s not usual. They usually send you an email and you look it up online. That was when I first started really thinking that this would be really serious for me, as opposed to just my brother.
What is the PSA test
It’s a simple blood test. They draw a little bit of blood. There’s no fasting, there’s no extraordinary requirements.
One thing you can’t do is any sexual activity, so a lot of men will gripe about it. I believe it’s three days ahead of the PSA test you can’t have sexual activity or it will skew the results.
Men will brag and say that’s really annoying, in reality I don’t think any men are having sex that much at my age that they can’t withstand three days of waiting for the blood test.
It’s very simple, very easy. The PSA test, itself, when I was first talking to my original doctor, there was a lot of controversy on its efficacy. There were some studies done on the harms of the PSA test versus the actual deaths involved. So there’s recommendations to get away from doing the PSA test some years back. That was around the time I was getting it.
People equated the harms equally of getting and not gettin the PSA test, equating getting an infection from a biopsy or false-positive PSA to death.
To me, they’re not equal! One’s a lot worse than the other.
For the simple blood test, it’s an easy thing to do. The thing you have to think about for men looking at this for the first time, is you have to have some fortitude when you get the results.
The PSA level might be higher or elevated but it’s the doubling time, how rapidly it’s growing, that’s the issue.
So listen to your doctor, but you don’t want treatment without taking the PSA test later or following up with some other evidence, like a biopsy or digital exam. It might be when you take the second PSA test doubling time might be 100 or 25 or 30 years. By then you’ll die of something else other than prostate cancer!
It wasn’t my case, but in most cases, it can be a long time. At that time you do active surveillance, wait and see if it changes at all.
But don’t panic after your first PSA test, even if it’s elevated. It might be elevated but would take a long time for it to get somewhere problematic.

How long did it take to get the PSA level results
I got the results the next day. It was fairly quick. Normally with the doctor it took a couple of days, but this time was within a day.
Getting Diagnosed with Prostate Cancer
Describe the urologist meeting
My first question was wait, if this is cancer, why am I seeing a urologist? Prostate cancer is unique in that way in that it’s the urologist who takes the lead, generally, at first.
The urologist did a digital exam and said he felt some nodules but not to panic yet, that they would check another PSA test in three weeks to see if it changed at all, and if so, how much.
Results of the second PSA test
The PSA level had risen at least three points which in PSA terms, is a lot during three weeks. So it was appearing aggressive. At that point, the doctor recommended a biopsy.
Describe the digital exam
That’s where they probe with their finger, their digit up your backside. They are feeling the prostate to see if there are any lumps or forms they can feel that aren’t normal. That’s what they’re looking for.
It’s really just something you have to do, and I don’t want to say you feel violated, it’s just not that big of a deal. It’s very quick. They feel around, and then you’re done.
Considering the consequences of not doing it, it’s a pretty small price to pay in the small amount of discomfort. I feel way more pain when I’m trying to do my taxes.
Describe the biopsy
The biopsy sounds scarier than it feels. When they describe it to you, it can be terrifying. Going through it, it’s not that bad. You lie on your side and to reach the prostate, they take the needle and go through your rectum, take some tissue samples of your prostate.
Just the idea of a needle going up there sounds terrifying but they numb you up. You do feel a little pinching here and there as they collect the samples, but it wasn’t nearly as bad as I feared.
Recovering from the biopsy
There was a little pain for about a day or so. But the fact that it doesn’t stick in my head as being terrible means that it wasn’t that bad.
Again, someone has stuck a needle in you so it is sore there for a little while. But I was more afraid of infection than anything else, so again, I did everything the doctor said.
They mentioned there could be bleeding. I didn’t encounter much of that. You just take antibiotics and do some cleaning down there.
Issues of infection post-biopsy
There are issues of potential infection after so you have to be very mindful. Through this whole journey, do what the doctor says. That’s really key.
The doctor said do x, y, z, it works when you do what they say. If you do the oftentimes difficult or “male” thing, thinking I can do it myself, just do what the doctor says.
I don’t recall exactly what all the post-biopsy care was but they give you some antibiotics to make sure there are no infections. It has to stay clean.
It took just a few minutes once they got started. You feel some pinching but it’s no worse than someone pinching your skin, it’s a pin-prick type of sensation. When it’s all done, you have a lot more concrete answers.
When did you get the results from the biopsy
Gleason score is probably one of the most confusing aspects of the prostate cancer journey. I was at work at the time, and the doctor had the nurse give me a call.
The nurse called and said she was calling on behalf of the doctor. It was a very busy day for me and she asked if it was okay to give me my results over the phone. I was thinking sure, I had so many things to do, so fire away.
She gave my Gleason score and said the biopsy was positive for cancer. All the cores were positive for prostate cancer and I had a Gleason score of three plus three, and three plus four, measured as a 6/7 score.
That was kind of it. She said they’d be back in touch with me and the doctor would schedule a follow-up appointment. I left it there because she didn’t sound alarmed, so I wasn’t too alarmed.
But when I got home and started doing research, I didn’t really understand what she told me. Then I realized okay, this sounds moderately bad in terms of Gleason scores.
What was your layman’s understanding of the Gleason score
There are two numbers there and they have to do with the aggressiveness of the cancer. What they view in the microscope of how disorganized the cancer seems to be.
So the first number is the most prevalent amount and the second number is the lesser prevalent amount of aggressiveness and disorganization of the cancer cells. That’s my layman’s understanding of it. Then there’s a left side and right side, so you generally get two sets of numbers.
How did you process learning about prostate cancer
I knew it was concerning for my brother, but again, since I didn’t know much about prostate cancer and hadn’t heard much about it, I didn’t think it was a big deal in terms of risk.
Then as I started reading about it, once I was diagnosed, I realized just as many men died a year of prostate cancer as women do of breast cancer. That was really the stunning statistic that hit me.
The other thing is when you look at it, there are two different sides of the story that are equally true, but give different pictures.
On one hand, you hear a lot about prostate cancer not often being fatal and that usually, it’s mild, and most men don’t really have a problem with it. That’s true. It may be for some men.
But the other half of that coin is how many men have it. And when you have that many men have it, it’s very ubiquitous as you get older, the absolute numbers of deaths are very high.
So while on one hand the percentage of men who have serious problems are small, but the sheer number of men who have it drives that number of those with serious problems in real time very high.
It wasn’t until I started reading about that when it really struck me that this could be bad.

How was your conversation with your urologist about prognosis and treatment
That appointment was grim. I had already done some reading. The “seven” score was the part that resonated with me as not a good number to have since it was out of scale of ten. Your six, seven score is moderately aggressive, and your eight, nine, ten scores are bad.
So my wife and I went into the appointment and it was very sobering, if not downright scary. They started showing me these charts. We had this conversation that they’d have to take action on this because it wasn’t good, it was very aggressive, looking at the Gleason score and how fast the PSA was rising.
The urologist said my life depended on this. Those charts showed the survival rate which was very grim and scary. That was a very unsettling meeting. It took about 45 minutes to an hour as we muddled our way through it.
Most of the time, he was speaking to convince me and my wife that we needed to take action, and fast action. He was also trying to explain the range of options available.
At that time, I was still trying to get my head around the first things he was saying, like it was not a good Gleason score number to have.
As frightening as it was, you have to stand back and look at as we contemplate those survival curves, they’re normal bell curves, which means most people are in the middle and you get a few on the extreme ends on the higher and lower ends.
Our strategy was to look at this like there’s a reason some people are falling on one end or the other of the bell curve. It’s a random sampling of the general population.
So we needed to focus on what we could do, what we had control over, that could put us on one part of that curve of another.
That’s where our mental attitude had to be: what is in our power to change that we could have control over?

How did you and your wife process the diagnosis
Coming out of the meeting, we were shell-shocked. I honestly don’t know if the intent was to make sure that we did the treatment, that we didn’t blow it off.
One of the problems they have with the recommendations with the PSA test is the concern of men going out and getting radical treatment, like getting surgery after one test.
That was apparently very prevalent then. Then getting prostates removed that didn’t need to be.
I think part of the motivation behind the PSA recommendations, and they said this much in the study, was to drive that down. But we were on the opposite end. The urologist was trying to make sure that we took action and didn’t take it lightly. He succeeded in convincing us.
It was scary, very scary. Moving from that, it’s about trying to get information. As you try to cram for any test or learn anything, there’s so much information out there. But then I did get a second or third opinion in seeking other advice based on the tests.
»MORE: Patients share how they processed a cancer diagnosis
Treatment Decisions
Tip: get help and support from others from the start
For people who get a high Gleason score and an outcome where the doctor feels it’s very concerning, you don’t necessarily want to do all the research yourself. That’s really a bad idea because as we know, the internet is full of exaggeration one way or the other.
It’s hard to find definitive, scientifically-based information, and so it’s helpful to have a family member, in my case my sister, who did a lot of research for us and helped us out.
She could look at it from a more neutral eye, rather than trying to terrify ourselves by what we were reading and then fundamentally discard the information.
Learning from others who’d been through treatment
One thing I wish I had done earlier was go to a prostate support group of some sort. I didn’t do that until my treatment was well along the way.
I learned things there, hearing things being said, that would have been very helpful before going into surgery and before deciding treatment. The hardest part was trying to decide what treatment to go for.
What were the top tips you wish you had known earlier
The tough part was knowing what to expect. I just wanted to hear other people talk.
I don’t know if this is universal but I went to two different support groups. One was a general cancer support group and one was a prostate cancer support group.
I went to the general one first and there was a lot of emotion, which isn’t bad, but a lot of people going through some rough times. The session I attended, I was the only one with active cancer.
Most of them were people who had survived the cancer and were terrified about it coming back. A lot of talk was the emotional part of it, which has its benefits.
But when I went to the prostate support group, it’s largely a bunch of older men who have time on their hands because most of them are retired. They know a lot about the X-ray machines, the procedures, the topics.
I sat there and they’re bragging about whose is better. I realized I didn’t know enough, sitting in this group. These guys knew their stuff! There was no or little coddling, at first. There was a lot more bravado.
As it moved on, I realized there was a lot to know. One of the things, from my own research and family research, is the outcomes are kind of the same statistically, regardless of treatment. So you’re looking at the extra features to make the decision.
It’s like a car. All the cars on the lot drive and have the same basic, core features. So what are the luxury items or the features you want to live with later? That’s the same way with prostate cancer.
For example. In radiation treatment, it was far less invasive and a lot easier as an initial treatment. But there’s still a chance you have some residue PSA there that you have to keep an eye on.
Certainly some of the radiation treatments now are very focused on the area so there’s less tissue damage around it.
Surgery is more radical in that you’re taking the whole thing out. But I opted for that choice because I knew once it was out, it’s not coming back, if everything worked well.
I was wrong for my own situation, but at least at that point, if there’s PSA, it’s due to cancer and not to anything else.

Weighing pros and cons of surgery vs. radiation
With radiation, a lot of guys I knew opted for that because it was easier for their routine. They didn’t like the idea of someone cutting into them or going in and removing something.
On the other hand, for some men, removing the prostate is not needed necessarily, so a lot of people will say it’s cancer, let’s get rid of it, and be done. So you have both lines of thought.
Most people I knew who opted for radiation was out of convenience for doing it that way. It didn’t really impact their lifestyle very much.
Video: Bruce Talks About Treatment
- Radical prostatectomy (surgery to remove entire prostate) and recovery
- Getting restaged to 4A and Gleason score 8/9 (instead of 6/7)
- Salvage radiation
- Hormone therapy (Casodex and Lupron)
Prostate Surgery (Prostatectomy)
What was important to know heading into surgery
One of the best things, something I didn’t know at that time, wouldn’t impact the surgery too much. But rewinding a little, my PSA had been rising very rapidly. I looked at things I was in control of, what I could mitigate to help save my own life.
After talking to doctors at Johns Hopkins, and looking at materials from Mayo Clinic and the NIH, diet and exercise were things I could control.
There was a study relating to a low incident of prostate cancer in China versus the United States. They tracked immigrants to the U.S. Those men soon had the same rates of prostate cancer as the other people in the U.S.
That takes the genetic part out of the equation, so there’s definitely some environmental part in this. At the time, it was mostly looked at as red meat in the diet.
Changing diet and exercise pre-surgery
I shifted to a complete vegetarian diet and then exercised like a madman. I also dropped out of the workforce.
I took time off of work because after that meeting with my doctor where he gave me the grim results, I was talking to my staff and said I just didn’t feel like coming in.
One of my senior colleagues said then don’t come, we’ve got this, we’ll take care of this. Don’t worry about this. So I researched the options for me on treatment and decided on the surgery, but I exercised every day. I was riding about ten miles a day on the bike.
It flattened my PSA. It didn’t rise anymore after that. In that short period of time, I can say it slowed things down, but as a consequence, I had also lost a fair amount of weight, about ten pounds during that time. My surgery was very quick.
The doctor came out and said the surgery was normally a lot harder to do because of the amount of fat. But with me reducing the amount of fat I had, it made it a lot easier for the surgeons.
I just looked at it and said hey, if you’re coming into my house, it makes sense that I should clean up!
So it’s a benefit, not only do you slow down the cancer, but you make it easier for the surgeon.
So to the extent you can, maintain a healthy lifestyle until the surgery’s done. Do the best you can to be in good shape when you go in.
I visited my office the week before surgery and they were all stunned. They said wow, you look great, not like you’re dying from cancer! I said well, I look great now but we’ll see how it goes.
How was the prep before surgery
That was the main thing – trying to stay as healthy before the surgery. The prep, itself, for the surgery wasn’t too bad. They did do some scans, like the bone scan, and the CT scans. Those were somewhat arduous. I also did an MRI, which was probably the toughest one.
How were you mentally prepared for the surgery
It never occurred to me that I would not succeed. I felt this was something I could win, I had every intention of winning. Were we scared? Of course we were scared.
But I felt there were things I could do, like the diet, exercise, and doing what the doctor said. I was not about to let cancer ruin my life without a fight. Oddly, a lot of that fight is trying to be as normal as you can.
Describe the CT scan
In terms of the pre-op process, they did a CT scan to see if they could find any of the cancerous tissues, which is not a high-fidelity test, but if you can see it on that scan, things are probably pretty bad.
Describe the bone scan
They do a bone scan, which is when they inject an isotope into your blood, which felt kind of warm. It was a weird sensation going through. It didn’t hurt or anything. It just was a strange sensation.
Then they did a sort of X-ray. It was a CT scan-type machine. With that, they were looking for any infection of the bones, because that would mean the cancer progressed a lot further. That’s a whole nother stage of cancer that’s likely fatal.
Results of the scans
The CT and bone scans both came back clear.
Describe the prostate MRI (with rectal probe)
Then they did some imaging where they put a probe into the rectum and did another type of CT scan that gives them more fidelity for the surgery, to guide them on what to do.
My wife looked at me and said I came out of that and said, “I’ve been violated.” That one I wasn’t ready for. They said they had to put a probe up, but I didn’t know anything about that probe.
Fortunately, they didn’t tell me too much about it so maybe I shouldn’t mention it here, but it was very quick. Probe was in. But it wasn’t very comfortable. I was sitting there for about 20 minutes while they did it.
Throughout the course of my entire treatment, they did this type of imaging twice. For the second one, at least I knew what was coming. I was able to relax and say okay, this is it. It didn’t make it any less uncomfortable, but at least I didn’t have the same shock.
I could mentally prepare for it a bit, whereas the first time, I had no clue. I lied down, guy said roll over, and he just shoved the probe in, and I was done! That was not a fun experience. The biopsy was more pleasant than that, in a sense.
The value of the prostate MRI
The fidelity they got out of that MRI scan, they showed me some of the pictures, was quite remarkable.
It was a new treatment tactic they were using at the time to see if it increased their ability to find the cancer in the margins or in the outside tissues.
So even though it was really uncomfortable, it was really valuable.
This was something the NIH was doing for research that gives them more fidelity for the surgery, to guide them on what to do. When people want to study you for your cancer, that means you’ve hit a brass ring you didn’t want to reach for!
Undergoing a pre-op physical
Right before surgery, they did a complete physical and all the blood tests. They checked my heart, as well. I did that with my regular doctor. Most of the tests were done by my regular doctor even though the surgery was done at NIH.
How were you feeling going into the operating room
When I went into surgery, it was kind of calming. I realized something was finally going to get done. I didn’t worry about some things that give people anxiety, like what would happen when I woke up. I wasn’t too concerned about that.
That said, we did the will thing, filling out my will. I made sure all of our finances were in order and made sure my oldest son knew how to access my files and records if my wife wasn’t able to. Just common sense things like that that you do before any (major) surgery.
What do you remember of waking up from surgery
It was a quick in and out.
They wheeled me into the operating room and told me and my wife it’d take about three hours for surgery. When I came out of surgery, I had only been in the operating room for about 30 minutes! So my wife wasn’t around, nobody was around. They had expected a bit of a wait.
To be honest, that wasn’t the first thing on my mind. It was like, I’m here, at the moment I feel comfortable even with the IVs everywhere. I really wasn’t alarmed that my wife wasn’t there when I woke up.
The surgery was quick in part due to your weight loss
Yes, they said it was very clean in there. They didn’t have to spend time moving things out of the way so much.
You had undergone a robotic surgery
To be honest, I’m an engineer and a geek. There was a geeky aspect to this.
When I found out the surgery was going to be robotic, I was like oh my goodness, I’d do this even if I didn’t have cancer, this is cool! I was really into getting the robotic surgery just because it was cool (laughs).

Recovering from Prostate Surgery (Radical Prostatectomy)
When you woke up were you in pain, how was recovery
We stayed a couple of days in the hospital, maybe even one extra day just because at home there were a lot of stairs and other things, plus a dog who’s very rambunctious at times. With a catheter in, I really didn’t want the dog jumping on me too much.
They’re very proactive in getting you walking literally the first day after surgery. I think it was the very first evening when I did my first getting out of my bed, at least going a few feet.
Overall, I was pretty comfortable, as they were giving me a lot of medication. The one challenge they had was my catheter got a little blocked at one point.
So I stayed an extra day to take care of that. That was very uncomfortable. Then they got that blockage released and then it was okay, and I filled up a lot of that bag.
That was my only real tough part coming out of surgery, that isn’t necessarily normal for everybody. That was something that happened for me.
The first night they gave me some Ambien. I had never in my life taken a sleeping pill. I’ve always been a sort of insomniac and burn the candle at both ends all the time.
Traditionally in my life, I’d do four, five, maybe six hours of sleep a night. That pill was wonderful! They gave that to me and I went out like a light.
I had some anxiety about falling asleep and the doctor said don’t worry, we’ll give you something. The next morning, whenever they woke me up to change something, that was wonderful.
Managing the catheter and getting it taken out
The catheter was probably what I had the most anxiety about. In hindsight, you can’t wait to get it out, but it’s not painful. I was worried about every little movement I made, but it wasn’t that bad, at the end of the day. It was actually quite livable.
Removing the catheter
Even more than that, my biggest fear was removing the catheter. I couldn’t think any way in my head that they could remove that thing and it wouldn’t hurt like crazy.
I know I’m being a wimp, women give birth and have kids all the time. I told my wife at her bedside labor, if there was some way I could take all her pain off her instead of her going through this, that we would be childless!
The fear was unfounded. After about a week, they took the catheter out and put in some cold fluid, and I hardly realized that it was out. It was a flash and it was out, no pain. That was one of my biggest anxieties, removing the catheter, and it was unfounded.
The cleaning of the catheter was challenging, the cleaning of the area. There’s a lot of maintenance to do with it (at home). That was arduous.
Great care at the hospital
At NIH, and I haven’t gone through many surgeries in my life for comparison, but the staff there really cared and really took care of me. They were passionate about the care of their patients.

Any last guidance on recovering from the prostate surgery
I needed patience to walk farther and farther everyday. It is tough feeling weaker or more vulnerable. You’re just taking little baby steps at first and going very slowly.
So we started off just slowly walking my way down the sidewalk. One day I’d go a few feet, then the next day maybe a few feet farther. That became my goal post everyday. I was trying to make it to the next driveway. It took patience. It probably went by more quickly than I remember.
You really are up and around pretty quickly after. Once the catheter comes out, you’re free to do a lot after that.
Did you need a lot of physical assistance after the surgery
The initial walks, I needed a little bit more help, though I wanted it more than maybe I actually needed it. There’s someone right there with your arm in case you don’t make it. As you test the waters, you realize you can go pretty well.
My brother had a much more invasive surgery. It took him a lot longer to recover from that. With my robotic surgery, and I also didn’t have nearly as much invasion as he had of the cancer, that I recovered much quicker. I was sitting up within a few days and moving around the house much more quickly.
Planning for More Treatment
You were re-staged with a higher Gleason score post-surgery
The pathology report on the actual cancer once they got the whole thing out to look at. My pathology from the biopsy showed a 6/7 Gleason score.
My pathology report with the surgery came out as an 8/9, which was a lot scarier. It was 8/9 on one side and 7/8 on the other side.
But the real signal that was that the cancer had invaded the lymph nodes. As a precaution they removed all of the lymph nodes around there, about 20 lymph nodes.
At that point, once I knew it had made it to the lymph nodes, that took away my comfort of knowing that the cancer was gone forever. I knew, mentally, that now it had gone outside the prostate, who knew where else it had gone.
You had been staged 4A
You don’t hear the 4A too much. It’s what the pathologists and doctors use a lot, and the cancer groups use that, but with prostate cancer it’s more about the Gleason score and PSA scores.
That’s what is most talked about. You look back and read the details of what those other numbers actually mean.
New treatment plan
Once I heard that, my elation over the surgery was tempered. I remember walking with a friend saying now you’re done, you’re cancer free. I said maybe, maybe not. They thought that was a negative attitude but I was just trying to be practical.
It did invade lymph nodes so I knew I may not be out of the woods. I was proven to be correct in that they did a PSA test a few weeks after the surgery and it was miniscule, but it was still there at a .17 if I recall.
The doctors explained that wasn’t abnormal, sometimes there’s residual PSA after surgery. So they waited another six weeks or so and then it had risen to over 0.2. At that point they said it was an indication that the cancer was still there somewhere. The surgery wasn’t a complete success.
The biggest success was that it bought me a lot of time. Had I not discovered my error in taking the wrong cancer test from my brother, I wouldn’t have survived. It was very aggressive.
The whole prostate was engulfed, it had gone into the lymph nodes. It was an 8/9, so my odds of survival were not good had I not had the surgery right away. Even then, the word doctor used was this is a very lethal cancer. That resonated a bit more after that.
By then, my family and I had done a lot of homework. We knew what the next step would be, which would be the salvage radiation going forward. So I mentally prepared for that. Just hearing the PSA numbers that low means you have some time.
Salvage Radiation
Describe the salvage radiation process
I was at the NIH, so they were trying things that they weren’t doing at other places. Beforehand, they gave me some medication, Casodex and Lupron before the radiation. Those were started about six to eight weeks ahead of time.
The idea was to get my testosterone production down before the radiation.
They had said it would help with the outcomes of the radiation. The salvage radiation, even though you don’t know exactly where the cancer is, they’re aiming in the pelvic region still.
That’s an unknown when you first start with the radiation – is it even there? There’s a chance it’s not and it’s somewhere else. Odds are, if you’re a betting person, which at that point you have no choice but to gamble, it’s probably there in the pelvic area.
How was the actual salvage radiation process
It was daily radiation for six weeks, Monday through Friday, so no weekends.
The NIH did a process of having you drink water before the radiation and to help move your organs out of position, out of the way of the radiation beam, as well as to make it a more clean shot.
The theory was the radiation would have a lot more effectiveness and less collateral damage to other tissue. It seemed to have worked.
That was hard to do because you’re drinking water and the idea is to fill up your bladder quickly, and then you have to hold it during the treatment.
You’re hoping they get it right the first time because it’s hard to hold that bladder. That was a little uncomfortable.

How long was each radiation session
The session itself was very short, 15 or 20 minutes. The prep work was drinking the water and waiting till your bladder’s full. Then you go in there so they can do a preliminary radiation (test) shot to make sure everything’s organized and how they want it. Then they do the actual radiation treatment.
The quick scan takes a minute or two, then they look at the results, adjust you maybe, then do the actual radiation treatment. So it was a good hour-and-a-half altogether.
Were there any immediate radiation side effects
No, never felt a thing. Had to pee a lot! But other than that, I didn’t feel a thing.
Radiation side effect (later): blood in the urine & incontinence
That was unrelated to the cancer but was caused by the radiation treatments. You don’t feel it, it’s painless so you don’t notice it. But I did have a small mass start to bleed inside the bladder.
They just cauterized it. They went in and did a local procedure, doing it very quickly, cauterizing it so it didn’t bleed anymore.
It was disconcerting because you’re awake when they’re looking into your bladder with a little scope. They’re talking about what they’re looking at. Then they went, “Hmm.”
I looked at the monitor and echoed, “Hmm?” I don’t like hearing that! What do you mean, “Hmm!”
He answered it was a small mass and that was where the bleeding was coming from, adding they’d cauterize it and do a biopsy, which came out negative. He explained it was likely caused by damage from the radiation, but that made me a bit nervous.
In terms of incontinence, the key message is do your Kegel exercises religiously, both before and after treatment.
I’ve found that I have minimal incontinence issues when I regularly do the exercises but when I slack off, it becomes more impactful (more leaking, especially when lifting objects). Fortunately, when I get back on track with the exercises it improves again (at least so far).
The fatigue study at NIH
The NIH knew that exercise helped reduce fatigue from radiation treatment. What they didn’t know at the time was how much exercise, how much or how little, to make that work well. I don’t know the results because last time I checked, they were still ongoing.
They said exercise helped reduce the fatigue from the radiation treatment.
During the radiation treatment, I got tired. It took a lot out of me because they were killing tissue inside of me, so my body was doing a lot of work to try and cope with that. The NIH found that if you do exercise, it reduces the amount of fatigue you feel.
What they didn’t know and what they have been trying to figure out is how much exercise is needed to make it relevant.
Our study was broken into two groups. One was more strenuous exercise versus slow ones. So for walking you’d do on a treadmill, and one was at a higher speed and one was at a lower speed.
I was in the higher speed group. It was easy for me in the sense that I was competing with 80-year-olds while I was 52. It was a lot easier for me, as I got my cancer at a much earlier age than what was normal.
That’s something to do – exercise during your radiation treatment. It will reduce the amount of fatigue you have.

Hormone Therapy: Casodex & Lupron
Describe the Casodex and Lupron
The Casodex was to reduce the ability of my adrenal glands of being receptors of testosterone and the Lupron was an injection to help reduce the production of testosterone. It was shooting at it from both angles.
Testosterone is basically what the prostate cancer feeds on and prostate cancer is really a diabolical creature in that even without the testosterone, it could take some estrogen or it can start producing its own testosterone. So it can mutate in that manner, which is kind of scary.
The process ahead of time before the radiation was to drive down my testosterone levels, starving out any bit of cancer that was there. The cancer was miniscule at this point, very small according to the PSA numbers.
How many doses of Lupron did you have to take
It varies. I started off with quarterly shots. I was getting different dosage amounts. Then I went every six months, so that was a bigger dose, but I wouldn’t have to get the Lupron as often.
It was a shot in the backside. The shot wasn’t that bad. From what my wife says, the needle was really big, so she said she was glad I didn’t see it. She told the nurse not to show me the needle.
So the needle might be big but it wasn’t any worse than any other shot you get in the hind end.
How did the Lupron affect you
The Lupron was probably the most impactful thing on my life. It takes away all your testosterone, so it’s a lot of changes to your body.
One of the things I had a problem with was hot flashes, which is typically a woman’s menopause issue. When I described some of these side effects, my wife said oh, you can go through menopause with me!
I was literally dripping sweat in meetings. I was still at work, would go and be just dripping on the paper in front of me. I talked to the NIH to ask if there was something we could do about these hot flashes because they were miserable.
They first recommended some drugs, but I didn’t want any more hormone medications. I asked what else there was. They mentioned that acupuncture might be effective.
I had never give it a whole lot of thought, but I was never a big believer necessarily in acupuncture. I didn’t not-believe it. I was skeptical but decided to give it a shot.

Acupuncture helped relieve the hot flashes
I went and did the acupuncture. It was remarkable. I did acupuncture once a week.
Within the first four weeks, most of my side effects had gone away, in particular the hot flashes.
I did an eight-week treatment (eight treatments total). I did one more treatment a year later and that pretty much solved all my hot flash problems throughout my Lupron treatment. I’d get mild warmth and a little bit here and there, but nothing severe.
It was a miracle.
I became a believer after that because sitting there when the acupuncturist was sticking me with needles, I thought this isn’t going to work.
By the end I wanted to be done with the acupuncture, but it wasn’t really painful. I’m just not one who can sit still very well, sitting still for a half-hour or so.
I went in very much a skeptic, and after the fourth week, I was doing daily radiation, I was part of a fatigue study, so I was used to going where they told me. So it was just one more appointment. I wasn’t really thinking about it.
Then my doctor asked me about my hot flashes. Then I realized wow, I hadn’t had any. Just halfway through the treatment, the acupuncture reduced the hot flashes significantly.
What were the other side effects of Lupron
The other side effects were feeling more emotion, more tired, I didn’t have the assertiveness at work that I normally had, which in some cases was tough on the job a bit.
That time period, through the three years of 2013, 2014, 2015 into 2016, was really tough. I exercised as much as I could.
In terms of the physical things, the Lupron also reduces your bone mass. While you don’t feel that, it is a concern, so I took a lot of calcium during this time.
I was doing load-bearing exercises, walking, lifting weights, and doing what I could to try and mitigate the loss of bone mass.
I also learned more and appreciated more what women go through! There was one night when my wife and I were in bed. I was kind of emotional and sad.
My wife asked me what was wrong and I said I didn’t know, just that I was feeling sad and didn’t know why.
She reached into her bedside table and pulled out a piece of chocolate and told me to eat it. So I ate that and thought wow, I felt a lot better.
So men, when women say they want some chocolate, don’t deny them. They deserve it and it will help.

Undergoing DEXA scans for bone mass
I was getting DEXA scans, which I had never heard of, though women are more familiar with it. They use them to measure your bone density with a scan.
It was a bit alarming to go into the place to get my DEXA scan. I walked in and it was all women, who were probably alarmed by the man who went in. I was like sorry, ladies, I’m one of you now (laughs), here to join the party.
How has the follow-up been
Once I was off the Lupron, initially I would take a PSA test and meeting with the urologist every quarter. Then after a year or so of continued negative results off the Lupron, it dropped to every six months with quarterly PSA tests.
Now, three years out, I don’t see the urologist regularly any more, but still get a quarterly PSA test.
NIH checks up on me once a year to see how I’m doing, track and record my progress, check for additional indicators (e.g. explained pain), and answer any questions.
I still get a DEXA scan (bone density check) every couple years resulting from the hormone therapy (Lupron). If I continue a trajectory of restoring my bone density, I would guess that I would get the DEXA scan less often, but I haven’t had that conversation yet with my primary doctor.
Video: Bruce on Quality of Life and Reflections
Reflections After Treatment
Keeping up with good diet and exercise
I do have a lingering concern that as life has returned to a normalcy of sorts, I’ll become too complacent with my diet and exercise. As you know, it’s a balance between guilt and getting on with life. That’s why it’s important to form good habits, so it’s not an issue when we decide to indulge.
I’ve been relatively diligent about doing load-bearing exercises and walking a lot, though not as much during the COVID pandemic. Instead of walking around the office building, I’m walking around the house and outside, some.
As a consequence, I’ve been able to restore a good amount of my bone mass that I had lost. I wasn’t sure if it was reversible or not.
The other consequence is I still don’t eat red meat. I still eat chicken, poultry, and fish. I’m grateful for the substitute red meat products that allow us to have something.
Concerns about sexual function after surgery (prostatectomy)
It’s time for that talk about the birds and the bees, but with a focus on just the bees. Erectile disfunction is a very real possibility with some prostate cancer treatments.
And for a bee, a limp stinger can be a humiliating and highly frustrating experience. A bee can still have all the chemically-induced urges that drive it to seek honey, but without the ability to satisfy it.
A lot of men would rather face an uncertain death (even a certain one) than consider life with a dysfunctional stinger.
So my message for them is to just man up (I can say that with prostate cancer) and get tested. The earlier it is diagnosed, the less chance of having issues with erectile disfunction.
If the prostate is removed, a man will be unable to produce ejaculate, but all the important sensations can still be intact. Surgeons and doctors take care to preserve as much nerve tissue as possible during surgery, often with good results.
Surgical and radiation technology is also improving all the time. There are also a lot of treatment options for ED such as Sildenafil (think Viagra) to get your pal standing at attention again.
However, testosterone supplements are not one of them! Prostate cancer feeds off testosterone, so not a good idea.
In fact that’s the purpose of hormone therapies for prostate cancer, to eliminate and block testosterone to starve the cancer. Though there are some bright sides to hormone therapy aside from saving your life. During treatment you and your female companion will finally have sexual compatibility. You’ll both “have a headache.”

Keeping a sense of humor
My kids on the right there, and my spouse, Lisa, in front of me at the National Mall in Washington, D.C.
That beanie seemed fitting. I mentioned the cancer support group and the first one I went to, they asked me as a newcomer if I had any thoughts on the cancer support group.
I said actually I did, I thought the cancer support group wasn’t a great idea. The cancer is doing just fine without any help. It’s me who needs the support, not cancer!
Not a chuckle. Not a smile. I thought man, there needs to be a lot more humor than this. I’ll talk about that later in this conversation – the importance of humor and of keeping up a positive attitude.
One thing my wife and I found that was useful was trying to keep the moment light. In particular, when you’re in the waiting room with all the other men waiting to get treated, to not be a downer. Not to be doom and gloom.
»MORE: Read more from a prostate cancer caregiver perspective
Survivorship
There’s always the concern it could come back. You’re never fully out of the woods, but it doesn’t rule my life. For a short period of time, it kind of did, for two reasons.
One, I quickly became a vocal advocate at work and around my friends who decided not to get a PSA test, or put it off.
I tell my story because I was shocked to learn about it, too late. I feel very strongly that people should be talking about this more. It’s something men don’t really like to talk about, at least in public.
When I spoke at my office after my surgery and before the radiation, I described some of my journey and asked if people had questions. But I had a lot of men come into my office privately to ask me the questions.
They didn’t want to ask anything right there in front of the group and in front of everybody, but they were very curious. This is how I’ve pretty much found them to be.
If I’m around colleagues and I talk about it, they want to hear and want to talk about it, but one on one. They don’t want to talk about it in a group.
What’s your message to other men on the importance of sharing, expressing, asking
What I’ve learned from this is that men want to know and they should know. It’s something that’s just not talked about a lot, so they don’t hear it much. It’s not on TV. You don’t have a lot of commercials.
I have seen some commercials lately and things with sporting events, baseball, football, talking about prostate cancer awareness days. Particularly for people of color, they’re higher risk than the rest of us.
And it’s happening at an earlier age, just like a lot of cancers. I think we find that there’s less talk of cancer in terms of organs and more about cancers having more in common than we knew before.
But the fact that it doesn’t kill so many men every year, that’s one message that you get. You also hear the message that most men don’t die of prostate cancer and for most men, it’s mild, which is true.
But it affects so many people that there are a lot of people who do die. And it’s so preventable these days, unlike some cancers like pancreatic, which are very difficult to try and detect or thwart once you get it.
Prostate cancer is immensely treatable if you catch it early. There are also a lot of options to treat it these days.
If you’re going to get cancer, now’s a great time to get it because there are a lot of advancements in the treatment.
The PSA test is something that is so easy to do and you should be doing it at age 40 and, in my opinion, every year for men. Don’t disregard it. There’s no fasting before the PSA test. It’s such a simple thing to do. It can save your life.

What does self-help mean (self-advocacy)
The self-help is being aware of what the science is, being aware of trying to separate what’s out there on the internet versus what’s real, what’s truth. There’s a lot of resources for that.
The internet isn’t the best place to look for medical information. Your cancer support groups and organizations, there are a lot of non-profit prostate cancer advocacy groups that will weed through all of that for you and largely give you the information you need.
Take your time, try to sort it out. There are so many options now for treatment. There’s not just a clearcut path of what you should do.
To use a different analogy, if you use a hammer, every problem looks like a nail.
Surgeons are more likely to recommend surgery, a radiologist more likely to recommend radiation, so you have to go through and weed through them. Take your time to find out the pros and cons out of each.
I did think that most of the radiologists and surgeons I spoke with were open in giving me the other side of the coin, but it helps to talk to a range of experts, and go to these support groups. You are helping yourself decide on how to keep yourself healthy.
→ Re-read Bruce’s overview of what to consider
For me, the biggest life-saving measure I was in control of was my fitness and diet.
Those have such a huge impact and we’re finding out more and more on how much of an impact they have, not just for prostate cancer but for other diseases, as well. That is really the thing you have control over: your attitude, diet, and exercise.
The power of sharing your story
I had the advantage, in a way, because my condition and my Gleason scores were far worse than most men I ever came into contact with. So I could say, look, if they could see me being humorous still, it helped make them.
They’d think okay, he’s a lot worse off than I am, and he’s okay, so I can be okay.
I remember attending one support session where one book author came on and talked about surviving an aggressive cancer. As he talked, he gave his Gleason score, which was a six/seven, and I thought, wow, mine’s worse than that. So that’s not giving me a whole lot of comfort here (laughs).
But it’s survivable. 20 years ago, even ten years ago, it was not as survivable. If you seek the help, do the early warning, and get family members to do some of that research for you so it’s not too depressing to help sort it out, it’s something you need to be doing.
Taking care of yourself after treatment
It’s important to take care of yourself after treatment and find outlets. In my case, it was drawing, cartooning, and watching baseball to relax. Pursue some of the activities or ambitions that you’ve been putting off. For me, it was diving into the greeting card business on Etsy.
It’s okay to treat yourself well, attend to your own mental and physical needs, and recognize new personal limits.
I was a workaholic before, feeling fine with very little sleep. For a long time after initial treatment, I needed seven to eight hours of sleep to feel sharp and became tired after a normal day of work.
After my Lupron treatment ended, I’ve gravitated more to a six-hour sleep schedule. However, I still find myself needing more family and hobby time in the evenings.
I can now manage long hours of work for few weeks at a stretch, but I’ve learned to fence off my personal time a bit better to nourish my personal mental and physical health with less guilt.
Finding time for physical exercise remains the most challenging. Easier to do during these COVID telework times, but very difficult with long work commutes. Using a standing desk at work I think helps provide some load-bearing activity to counter the loss of bone density during the hormone treatments. Still, renewing my exercise regimen is something I still need to work on.
Your “different” normal
The phrase that I hear people say is that it’s living with cancer. That’s really appropriate.
I’m living with that knowledge that it could come back. It might get me in the end, I have no intention of it doing so, but it’s something I just realize is part of my life now.
I’ve accepted it as okay, that’s just what it is, I’m just going to move on and keep living my life. Sure, I have a hard time adjusting to temperatures in rooms, sometimes.

You don’t want cancer to rule your life, though it’s a part of your life.
I feel I’ve lived a pretty rich life in terms of adventure and doing the things I’ve wanted to do. I can’t say cancer suddenly made me appreciate life more, I always appreciated life from way back in college when I read a book about a newlywed couple.
The man had written it and his wife had just fallen through the ice, and they had just been married. That really hit home for me as wow, life can change so quickly.
I’ve always embraced doing lots of things I’ve wanted to do and tried to enjoy life the best I could, but it’s just another piece of that. It’s another part of yourself. A part of what you have to go through. When I knew how severe my cancer was, I had to rethink my retirement plan a bit, investment strategies.
We have our contingency plan if it comes back in an aggressive way, we know what things we want to do that we haven’t gotten to on our bucket list yet.
I think it’s really just not letting it rule your life, just knowing it’s a part of your life, and you want to rule it as opposed to it ruling you.
Inspired by Bruce's story?
Share your story, too!
Prostate Cancer Stories
Paul G., Prostate Cancer
Symptoms: None; elevated PSA levels
Treatment: Prostatectomy (surgery), radiation, hormone therapy
Mark K., Prostate Cancer, Stage 4
1st Symptoms: Inability to walk
Treatment: Chemotherapy, monthly injection for lungs
Mical R., Prostate Cancer, Stage 2
Symptoms: No symptoms, caught at routine physical with PSA test
Treatments: Radical prostatectomy (surgery)
Jeffrey P., Prostate Cancer, Gleason 7
Cancer Details: Diagnosed at 59, biopsy had not detected it
1st Symptoms:None, routine PSA test, then IsoPSA test
Treatment:Laparoscopic prostatectomy
Theo W., Prostate Cancer, Low-End High-Risk
Cancer details:
Low-end high-risk prostate cancer, early kidney cancer
1st Symptoms: PSA level of 72
Treatment: Surgery, radiation
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Cancer Details: Staged Gleason score 9
1st Symptoms: Urinating more frequently middle of night, slower urine flow
Treatment: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Gleason 8/9, Stage 4A
Cancer Details: Staged Gleason 6/7 pre-surgery, post-surgery changed to 8/9, PSA level at 27
1st Symptoms: Urination changes, brother's prostate cancer diagnosis
Treatment: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Al Roker, Prostate Cancer, Gleason 7+, Aggressive
Cancer Details: Aggressive but caught early
1st Symptoms: No symptoms, caught at routine physical with PSA test
Treatment: Radical prostatectomy (surgery)
Steve R., Prostate Cancer, Gleason 6, Stage 2-4
Cancer Details: Started at stage 2 and gradually progressed to stage 3, and then to stage 4 with metastasis to lymph nodes
1st Symptoms: Rising PSA score
Treatment: IMRT (radiation therapy), brachytherapy, surgery, and lutetium-177
Clarence S., Prostate Cancer, Low Gleason Score
Cancer Details: PSA levels fluctuated but were never extremely elevated, cancer contained to prostate
1st Symptoms: No symptoms, caught at routine physical with PSA test
Treatment:Radical prostatectomy (surgery)








3 replies on “Bruce’s Gleason Score 8/9, Stage 4A Prostate Cancer Story”
Thank you Bruce. My husband age 58 was diagnosed with prostate cancer (stage 4a) gleason 8/9 psa over 200 and in the pelvic lymph nodes. The doctor feels he is in the ‘curable group.’ He is now getting started with fitness and has been watching his diet. God bless you for sharing your story!
Thank you for sharing. My experience was/is very similar.
Great story and thank you – Been there with a Gleason 9