Jodi’s Stage 4 Epithelial Metastatic Ovarian Cancer Story
Jodi shares her stage 4 ovarian cancer story, from first symptoms to undergoing chemo and a hysterectomy, and also highlights how she navigated life with cancer.
In particular, Jodi describes losing her hair, including eyebrows and eyelashes, how important it was to have caregivers and support, and how she managed a cancer diagnosis and treatment as a parent. Thank you for sharing your story, Jodi!

- Name: Jodi S.
- Diagnosis:
- Ovarian cancer
- Epithelial
- Stage 4 (metastatic)
- Age at Diagnosis: 42
- 1st Symptoms:
- Extreme bloating
- Extremely tight skin
- Changes in digestive tract
- Significant pelvic pain
- Sharp, shooting pains down inner thighs
- Extreme fatigue
- How diagnosis happened:
- Felt body wasn’t right after birth of sixth child, insisted on testing
- Treatment:
- Chemotherapy, 4 cycles
- Hysterectomy
- Additional chemotherapy, 3 cycles
- Diagnosis
- Treatment Decisions
- How did you decide where to get treatment?
- Did you get a second opinion?
- How did you like your medical team?
- You've been to both a small and big hospital. Which was better?
- Did you understand the different players on the medical team?
- Describe each test and biopsy
- What were the results of the biopsy?
- How long did it take to get results?
- Describe the wait between appointments, tests, and results
- Did you undergo genetic testing?
- Treatment and Side Effects
- What chemotherapy treatment regimen did you undergo?
- Describe each cycle of chemotherapy
- How many bags of chemotherapy for each cycle?
- How were you feeling physically after each infusion?
- Did you experience any chemotherapy side effects?
- What medications and methods did you find most effective with the side effects?
- Did the cycles of chemotherapy get better or worse?
- Did you get a port or a PICC line?
- Describe the plan for surgery (hysterectomy)
- Describe the actual surgery
- How long did the surgery last?
- Any side effects after surgery?
- How was your second round of chemotherapy after surgery?
- Did you have the same side effects?
- What was the toughest part about treatment?
- How was your PET-CT scan after you finished treatment?
- How often do you have to undergo scans moving forward?
- Life Outside Treatment
- Describe the hair loss
- You also lost your eyebrows and eyelashes
- Were you surprised by your reaction to losing your hair?
- What helped you feel better about the hair loss emotionally?
- What helped you with the hair loss physically?
- You had to experience hair loss again after the second round of chemotherapy
- What helped you manage your thoughts and emotions?
- How did you manage your energy levels?
- Were there any big surprises during treatment?
- "Let yourself feel”
- You and your spouse had to work out a system in who would do the research
- How was the financial part of the process?
- Did you use alternative or holistic medicine?
- Support and Parenting
- What's your advice to people undergoing treatment for ovarian cancer?
- How important is it to have caregivers?
- Advice to cancer patients on how to ask for help?
- How many children do you have, and how old were they when you were diagnosed?
- How did you manage your emotions around the children?
- What are the extra considerations for a parent undergoing treatment?
- Any advice to other parents who are dealing with cancer?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You can do this. It will be hard, and there will be good days and bad days. I think it’ll be harder than the doctors portray it to be, but you can do it. Your body can do it.
Let people help you, let people love you, and really take care of yourself and stay on in a good, positive mental mindset. You can go to the dark places, but bring yourself back to the positive places.
I think you will be surprised at what your body can do. I have been.
Jodi S.
Diagnosis
How did you get diagnosed?
After I had my last baby, my belly just never went down. It just felt like it never got back to normal, even in exercising, I could lose some weight, but as soon as I got it off, I would just balloon back up. That was a concern, so I was talking to my doctors about that.
It felt, as time went on, it was getting tighter and a little more uncomfortable. Then probably about three months before I was diagnosed, it really started getting big and uncomfortable and tight.
I’ve been pregnant six times, but I never felt like my skin was going to open like that. When you’re pregnant, you just feel like you’re going to pop. I really hadn’t experienced that kind of feeling of explosion.
When that started occurring, I started having a lot of pain down in the pelvic region. When I would eat, I would have some sharp, shooting pains down my inner thighs. I had a very raspy voice. I wasn’t sick, but I sounded like I was sick. I sounded terrible.
You had to fight for the first doctor to listen to you
I think that was just me demanding, “This isn’t right. I don’t feel like this is a weight loss problem.” I think all the doctors wanted to help me lose weight, to get the tummy down. Just saying that I could feel something in my lower abdomen.
It’s going and saying I want all these tests. Test me. I think with ovarian cancer, a lot of patients are misdiagnosed with weight problems or digestive problems or things like that.
I just knew that I was really starting to lose my energy and having a hard time walking, so I knew something wasn’t normal. I just went in and cried until they did it.
»MORE: How to be a self-advocate as a patient
Describe your first symptoms
- Extreme bloating
- Abdominal pain
- Fatigue
- Changes in the digestive tract
- Difficult to walk
- Extreme loss of energy
I would really only notice [the abdominal pain] when I was laying down, usually after I ate a meal. I would think, “Oh, my ovaries hurt, or something’s going on.”
At first I thought I was starting to have menopausal symptoms, but when I would look that up online, my symptoms didn’t align with the menopausal symptoms at all. I just kept looking, and ovarian cancer was coming up a lot with my symptoms.
I started feeling like, “I think I have this. I think I should be tested, or at least my insides should be looked at.”
How did you convince the doctor to order the first CT scan?
Instead of saying, “I’ve got this big bloated belly,” I finally went into the doctor and said, “I don’t think this is weight related. There’s something wrong. I feel like there’s something in my lower abdomen. I want a pelvic exam; I want scans. I want anything. This big belly’s not normal, and it’s not due to weight loss.”
I had seen the nurse practitioner to my family practice doctor. I had never seen her before. She really was listening to what I was saying. She gave me the pelvic exam. During that exam, I could feel the tumors, and I told her, “I can feel those.”
She said, “They may be uterine fibroids.” I said, “I don’t think I feel good enough for this to be uterine fibroids.” She originally scheduled me to get an ultrasound and later that day just decided, based on that exam, to skip the ultrasound and head straight to the CT.
I think she knew I wasn’t going to leave without some sort of exam or some sort of test set up, but she was very sympathetic, really listened to what I was saying, and didn’t brush it off as a weight problem.
I felt so relieved she listened to me. It was just more relief and a little bit of fear that someone was finally agreeing with me. Her words were, ‘All of my little alarms are going off for you.’
I did have that little sense of fear, but I think I already knew that it was cancer, so I braced myself for it.
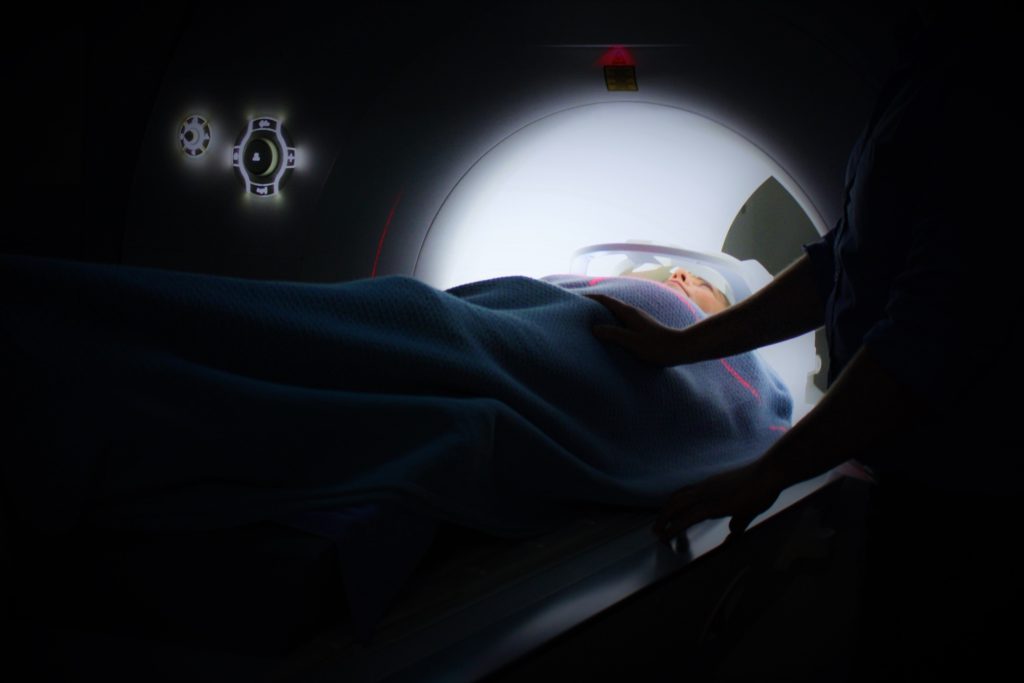
What was the CT scan like?
I just went in, drank some water. They put in an IV, put in the iodine, which is a really weird sensation. They tell you everything that’s going to happen. You’re not in the machine very long; you just kind of go in, breathe, and come out.
I didn’t have any side effects from the iodine. I felt pretty good, but a couple days after, I just felt yucky. I wouldn’t even say I was sick. I just didn’t feel right. I wasn’t hungry.
The bloating in my tummy was off the charts, but after a couple days, everything settled down. Every time I get a CT scan, for a couple days after I just feel a little off, but not really sick. Just not well.
How did you process the news of your diagnosis?
I was driving in my car by myself, and I saw my doctor’s office pop up, so I pulled over. I actually said to myself, “He’s calling to tell me I have cancer.”
I got myself to a good place where I could talk, and he was kind of beating around the bush, like, “This looked good on your CT,” and I said, “Just tell me the bad stuff.”
He said, ‘You’ve got some big tumors on your ovaries, and it’s looking like ovarian cancer.’
I was like, ‘I knew it!’
He said, ‘What?’
I said, ‘I just knew it!’
I felt almost a little excited. I was actually glad I was by myself when I hung up the phone. I was by myself, and I just had some time to collect my thoughts. Within the minute, I knew how I was going to approach it.
I had confidence in myself. I had this little plan for myself that I was going to listen to my doctors, I was not going to react, I was not going to Google anything, and I was going to listen to my gut.
»MORE: Processing a cancer diagnosis
How did you break the news to family?
I believed I was strong enough and could do this. That made it easier to go back and tell my husband and six kids later. I told my husband, and he was bawling. I was very composed and ready to move forward. He was bawling. Then I told my kids, and they were bawling, but I was okay.
It was when everybody went to bed — and I had never seen my kids that scared — that night when everyone went to bed, I got my turn to cry.
But I wasn’t crying because I had cancer, and I wasn’t crying for myself. I was crying because it was so heartbreaking to see my family like that.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to get treatment?
I just got the scan at the local hospital near my home, just a small hospital. When the results came back and I went for a follow-up with that nurse practitioner, she had already scheduled me an appointment with the gynecological oncology department down at UCSF.
She was very excited to have gotten me in with that group and just real excited that she was able to get an appointment at all. I didn’t have to go and search. She set all that up for me. It felt like she was giving me the best.
Did you get a second opinion?
I didn’t because I loved my doctor at UCSF, and I just felt great about her from the first second. My husband really wanted a second opinion, so we went down to Stanford and had a great doctor down there.
She pretty much said they would do exactly what the doctors at UCSF were doing. It’s about an extra hour drive to Stanford from my house, so she didn’t think it was practical to come to Stanford. She knew my doctor at UCSF and said if I had that doctor, I would keep that doctor.
But I will say the thing about the second opinion is after meeting with the first oncologist the first time, we had some questions. Leaving and going home and really thinking about it, we had some other questions.
This doctor knew we were there for a second opinion. She was like, “Ask questions. Ask me questions, all the questions you can, and when you go back to your other doctor, you can compare and see.”
She was really good to answer a bunch of our questions directly knowing she wasn’t going to be caring for me. I think that helped my husband a lot.
I didn’t want to know a lot of the details, so I was out of the room for a while.
How did you like your medical team?
What we ended up doing with my treatment was I had a regular oncologist at UCSF. They’re part of an oncology group, so the group reviews everybody’s cases.
Doesn’t matter who your doctor is. They meet together. They go over your case file and all make decisions together on how they’re going to proceed. So I felt really good.
Even though I loved my doctor and I would have trusted anything she said, I felt really good knowing she wasn’t just going to be making decisions off the fly, that everybody sat down.
Maybe people with more experience, less experience — they were going to talk about my case, and they were going to come to a decision together. I always felt very confident that I knew my case was getting looked at very strongly.
For my chemotherapy, UCSF is quite a drive from my house, so they referred me to the Marin Cancer Center. I had a separate oncologist there who just took care of my chemo. My UCSF doctor was the one in charge, and she would tell him what she wanted done.
They would coordinate together. I liked that there were two doctors because they would tell me different things, and then they’d come to an agreement together.
I will say my chemo doctor was a little more willing to talk to me more straightforwardly, like, “If this doesn’t happen, then this,” or, “This is really not good.”
I would get a little bit worked up, but then when I talked to my regular oncologist, she would calm me right down. She just knew. She would say, ‘This is something that we don’t need to worry about right now. If it happens, we’ll address it.’
Back to that, just don’t tell me more than I need to know because there can be a lot of anxiety involved in worrying about the what if’s.
You’ve been to both a small and big hospital. Which was better?
I actually found that I liked UCSF much better, mostly because I was really in an oncology department. They were very sensitive to that. I think they’ve got several different locations where they’re doing the radiology stuff, so the radiology technicians do a lot of it. They’re very friendly, skilled, with good bedside manner.
When I went to the small hospital, they had actually told me the wrong appointment time. When I came in, they said, “You missed your CT scan.” I said, “I’ve got my little card right here.” They had scheduled it wrong.
The nurse practitioner was like, “Whoa, look at that size of that belly! We’ve got to get you in today. Let me call and get you worked in!” I remember feeling a little nervous when she said that.
I was so grateful that she was squeezing me in and she was being sweet, but those kind of things set off little alarms in you.
I remember feeling nervous, and I never felt like that at UCSF. I just think at the department down at UCSF, they’ve been trained to be more non-reactive to the different things.
I felt they were all very professional. Since it was a teaching hospital, they were very informative, telling me what they’re doing and why. It was just great; I loved it down there.
As for my infusion center at a different, “smaller” place (Marin Cancer Center), I actually liked having the little smaller place for my actual infusions.
That was a much smaller community, and I think for my chemo, I loved that. Because it was a small infusion center, I knew all the nurses taking care of me, they knew me, [and] we knew about each other. It felt like family.
You would get to know the people around you in the room. I’m there on Fridays; I know all the Friday people. That had a real family and community feel to it. That was closer to home.
Did you understand the different players on the medical team?
Yes, I used the online portal a lot to communicate with the nurses or with the doctor. My doctor was very good and would communicate directly with me. She’s called me several times. She would always call me before she put something in the portal and talked to me about it.
I felt like I had great communication with her. I felt every time I went in for an appointment at UCSF or at Marin General, I always had to fill out mental health questionnaire, so I knew that there were resources available.
If I had said, “I’m struggling; I’m spiraling,” I knew that the doctors would be in there in a snap to get me set up with something. I always felt like there were resources available to me.
I didn’t really need any of them, but I felt like I would have easy access to them if I needed it. I would have felt very comfortable to call and say, “I’ve got to talk to somebody right now.”

Describe each test and biopsy
After the first CT scan, it was just of the abdomen, but they could see a little bit of fluid in my lungs. I went and had another CT scan done of the chest, where they did find a little growth on my sternum and a couple of enlarged nodes in my lungs.
After that, I had to have a biopsy in my lower abdomen. I think they were trying to get tissue right off the tumors on the ovaries.
It was a very simple procedure. They just numb you up. They go in with a needle and take a sample of the tissue and sent it off for testing to find out what exactly kind of cancer I had and to make sure it wasn’t colon cancer or another type of cancer showing up in the ovaries.
It was very similar to getting an ultrasound for a baby, actually, because when you go in, they put all the goop on your tummy and do an ultrasound to actually find good pockets of tissue.
When they go in, they know exactly where they’re going. I did not feel a thing. I can’t even remember feeling anything when they numbed the area, when they did the numbing injection.
It was very painless at that time. Since I was so bloated, they did drain a bunch of fluid at the time, and it made me feel so much better. There was really no recovery. I went and sat in a waiting, recovery room for about an hour and then got dressed, went home, and was fine. The whole thing was pretty easy.
I’d get my blood test the day before I had chemo. I’d go in and get my blood drawn just to make sure all the levels were okay and that I had recovered well enough and also to track the CA125.
It’s one of those tumor markers, which is a really good indicator for ovarian cancer. It was one of the things they did to diagnose me with ovarian cancer. A normal CA125 is between zero and 35.
Mine was at around 6,500, so it was a big indicator. Then every time I’ve had chemo, it’s been going down and down and down. It was high. I think you can use it to mark other cancers, but it’s a very good marker for ovarian cancer.
What were the results of the biopsy?
Originally, I was diagnosed with stage 3, but once they found the stuff up in the chest area, they bumped me up to stage 4.
It had crossed over into the lungs, but it really hadn’t metastasized. They still wouldn’t classify it as metastasizing out of the lower abdomen so much.
It wasn’t in any of my vital organs.
The lymph nodes in the lungs were very tiny, just barely enlarged, so it was the growth on the sternum that was the big concern for them.
How long did it take to get results?
For the biopsy, about a week. But I’m going to go back to when I was first diagnosed.
First, it took a long time to get the first CT scan and then a long time to get back into the doctor. When I got my first appointment with my oncologist, it was about three weeks out.
You know you have cancer, and you have to wait three weeks to see the oncologist. Then they’re scheduling another CT scan in two weeks, then a biopsy, and you have to wait.
The doctors didn’t have the sense of urgency that I did. Looking back, now that I’m on the other side of it, they were actually — in terms of medical scheduling — getting me in quite quickly. Things were moving the normal rate and the normal pace, but when I was actually in it, I felt like it was forever. I was very impatient.
Describe the wait between appointments, tests, and results
It felt like, ‘I have cancer! Let’s get going on this!’ But there was quite a bit of a wait, and that’s so normal. The doctors weren’t worried about it, but I was.
I’ve come to find out from everyone else I’ve talked to that just the waiting to get the treatment started is the worst part. I think that was just horrible waiting.
Waiting to get going because I knew there was stuff all over in me, and I just wanted to start working on getting it out of there.
»MORE: Dealing with scanxiety and waiting for results
Did you undergo genetic testing?
We did genetic testing. Ovarian cancer is highly linked to breast cancer, so I met with a genetic counselor. We talked about my family history, family tree going back, family kids who are younger, females that are younger.
There were several different types of genes they tested for. BRCA1 and BRCA2 and some other more unusual genes. They were thinking I’m quite young to have ovarian cancer, and I’ve had six babies.
Usually that will serve as a protection against ovarian cancer, so they were hoping there was something in my genetics, but everything came back normal.
I just talked to a counselor. We went back and filled out a family history tree, talked about health issues within the family, especially cancers and different types of cancers. Then I just had to fill a test tube up with spit, and I was on my way.
Those results took over a month to come back. They weren’t so urgent at the time because I had already started some treatments.
We haven’t talked about my big hysterectomy surgery yet, but after I had that, they did do genetic testing just on the ovarian tumors just to see if it was a rare kind of tumor.
Maybe I didn’t have it in my genetics, but maybe the tumors had something wrong with it or weird with it. It all just tested as a normal ovarian tumor.
Treatment and Side Effects
What chemotherapy treatment regimen did you undergo?
I had four rounds of chemotherapy, followed by a complete hysterectomy, and then three more rounds of chemotherapy.
Describe each cycle of chemotherapy
I had chemotherapy every three weeks. The infusions took about six hours.
The first cycle — I believe it was the Taxol — I had a bit of an allergic reaction to it, and they told me I might. It was really scary. They told me what would happen, but when it actually happened, it was really scary.
They started the infusion, and I was doing fine. They left, and all of a sudden I went from “I’m fine” to “I can’t breathe.” A cute lady in the room looked at me and said, “Do you need help?” I just nodded. She ran and got the nurses.
They were able to take care of that with some antihistamines quickly. They would do my Taxol infusions a little slower, so it would usually take well over six hours to get my infusions. There was a real chemical taste in my mouth and throat. I could tell I was being poisoned with something.
With the Benadryl, I usually just slept. I didn’t like people coming with me to get my infusions because I didn’t want to feel like I needed to entertain anyone.
I just needed to lay down and take my nap while they kept changing the bags, and so that’s worked well for me.
How many bags of chemotherapy for each cycle?
I think there were about four to five. There were two chemo bags, but then I would have saline solution, Benadryl, and some other antihistamines typically.
The first ones they injected quite quickly. I think two hours for one bag of the chemo and another three hours for the Taxol.
How were you feeling physically after each infusion?
The Benadryl would wear off within the six hours, and I would feel fine to drive back. I would always have someone on call just in case.
I would say, “I should be done around four this afternoon, so just in case I don’t feel well, can you come pick me up?” But I was always able to drive myself home.
Did you experience any chemotherapy side effects?
Day 1 was I would just be tired, but I would feel great. I would go home and rest, but I would feel great. In the middle of the night or the next day, I would just get so nauseated, be so sick.
Those first few treatments, especially prior to my surgery, I felt like my insides were being electrocuted. It felt like I was being shocked on the inside, especially on my abdomen, where my cancer was.
But I could feel it in my arms, legs, hands, feet, and it felt like a shocking pain that was vibrating. It didn’t let up for a while. That would only be for a few days.
They had told me about the numbness in the fingernails, the mouth sores, everything, but I remember calling them up and saying, “I need some pain pills because nobody told me I was going to be electrocuted! This hurts.” That starts to subside.
»MORE: Cancer patients share their treatment side effects
What medications and methods did you find most effective with the side effects?
I really feel like I could take the anti-nausea medication, and I learned after the first one, I’d just take it that night when I went to bed [and] take it when I wake up. [I] just keep on that regimen. It really kept the nausea down.
I only threw up a few times during the whole process. After the first time, I was in a lot of pain. I always just took the meds beforehand and just kept taking them until I felt noticeably better, because it was so much easier to stay on top of it than to get behind.
The pain pills would help me relax enough to sleep, so I would just sleep through it. Once that feeling of being shocked inside would go away, then the bone pain would set in. I could have shooting pains in my bones; I could just have dull, aching pains.
My mouth would get really raw. You have all the neuropathy in your fingers and your toes. I had restless leg syndrome really badly. I couldn’t hold still without some medicine.
The doctors prescribed a lot of anti-nausea medications, three different kinds, different variations I could take. It was just trial and error [to figure out] what worked best for me. They would just give me pain medicines.
I don’t like taking pain meds. I was like, “I don’t want to come out of this cancer addicted to pain meds,” and they said no.
You’re in pain, and you need to take them. When you feel better, you won’t want them. We don’t see a lot of chemo patients come out addicted to meds.
As soon as I felt like I didn’t need to take them anymore, I really don’t think about them or want them at all.

Did the cycles of chemotherapy get better or worse?
My first chemo treatment, I actually felt better after four or five days. I got up and I did a few more. The more chemo, I had the worse it was and the longer I was down.
By my last round of chemo, I was flat in bed for over two weeks before I could get up and start moving around again. The doctors would say, “Really?” Yes, really.
I was really frustrated because they said I wouldn’t feel good for a few days, and I would be able to do more. I took that as I would be yucky for a few days, and then I’d be able to get up and function. That was not the case.
I still didn’t have energy to do anything. I could get up and do a few more things like drive my kids to school, mostly just drive around, get in and out of the car. Other than that, I was pretty weak and on the couch all the time.
I went in and [jokingly] said, “You lied to me, you guys. You said I was going to be moving, and I’m on the couch all the time!” They said, “You’re doing great! That’s normal.”
I said, “You need to tell your next patients that they’ll feel yucky and probably start to feel better, but won’t be able to do much instead of implying that I would still be able to be a mom and take care of my kids.”
Did you get a port or a PICC line?
The one thing from getting my second opinion at Stanford is she said, “Be sure you get a port. Make them give you a port.” I didn’t. They just said my veins were great, and I just did everything using an IV.
Now as time has gone on, I’m getting my blood drawn so often, and I was getting IVs for surgery, IVs for scans, IVs for chemo that I feel my veins are really shot.
I wish I had listened to that advice and asked for a port or PICC line.
At the time, it was like, “Well, my veins are great. They’re just doing these IVs.” But now it’s a lot more difficult. A lot of my veins have scarred, and I do wish I had kind of pushed or at least asked about getting a port and a PICC line.
»MORE: Read more PICC line experiences
Describe the plan for surgery (hysterectomy)
The cancer was all over my lower abdomen. It was in my fallopian tubes, my uterus, and the omentum. I’d never heard of the omentum before, but now I know what it is, and I don’t have one (anymore).
Originally my surgery plan was they were going to cut me open, remove all of my reproductive organs, my omentum, some lymph nodes. The tumors had been pushing on my bowels, so they were going to perform bowel reconstructive surgery.
Having the chemotherapy, I had to have another CT scan before surgery. That one actually came back showing what looked like a spot on the breast.
I was supposed to have three cycles of chemo before surgery and three after. I had four cycles before surgery because I then had to go get a mammogram to rule out breast cancer.
That came back clean, but it postponed the surgery a couple weeks because, again, you’re waiting for those appointments and those results. We just kept me on the chemo regimen. Then they said I would have two chemo cycles after surgery, but they lied and gave me three.
After the mammogram, from the result of the CT scan, the chemo had killed so much of the cancer and shrunk so much that they thought they could go in laparoscopically instead of cutting me open. My oncologist said, “We’re going to start laparoscopically. If we can’t do it, we will cut you open.”
Describe the actual surgery
There was still a good chance for bowel reconstruction surgery, but thankfully they were able to do everything laparoscopically. They removed all the cancer in my lower abdomen.
The fallopian tube that was really swollen, enflamed, pushing on the bowels — the chemo had killed all of that, so it just lifted right off the bowel. I didn’t have to have bowel reconstruction.
What seemed like bad news, delaying the surgery and having an extra cycle of chemo first, led to me having a much easier time. They were saying, ‘You’re going to be in the hospital for a week.’ I was there overnight.
I just was in a recovery room. I never made it into a real room. They just released me. I just had four little incisions on my belly and through my bellybutton, and it was great. I didn’t have all the pain [and] everything that would have come with being cut open.
I didn’t look at anything, so after, when she was reading me the report, I remember looking at her and saying I was full of cancer. I remember saying, “I’m so glad I didn’t know. I would have been so discouraged had I known.”
How long did the surgery last?
We got there early in the morning, got prepped. I would say we got there 8 in the morning. I think surgery was supposed to start at noon; it didn’t start till one. I was in surgery five to six hours. Surgery was over at 6:30 at night. Stayed overnight.
My parents and my husband wanted to stay with me, and I was like, “Please go home,” because you don’t sleep that night. Someone was in the room checking me every 20 or 30 minutes. Taking my blood, checking my incisions. They were just doing a lot.
I was up most of the night, so I was glad I didn’t have people in there. I was glad my caregivers could go get a good night’s rest so when I came home from the hospital the next day, everybody was refreshed and ready to go.
I didn’t sleep at all. They get you up for everything to put things or to massage your calves, to get you to go take a few steps, to go to the bathroom, take the catheter out.
It was just nonstop people in and out of the room all night.

Any side effects after surgery?
I did get a urinary tract infection after the surgery. I just thought it was because I had surgery, and I really wasn’t feeling well. I waited too long to tell the doctor. I let it get out of control. I was like, “I’ve done chemo and surgery, and this urinary tract infection has leveled me.”
I did deal a little bit with that, but once I got on the antibiotics and got going, I recovered from that very well. I still think I had this false sense of, “After I have surgery, I’ll feel better.” Nope. I really didn’t.
I ended up getting really, really sick and throwing up a lot, and I didn’t eat for about a week. My dad is a physician, so I called him.
I’m like, “I don’t feel good,” and he was like, “I think you just have a urinary tract infection. Just ask your doctor to test, to leave a sample.” He’s like, “It’s such an easy fix.”
I wished when I first started feeling bad that I just called my doctor and said I don’t feel good.
Because I was already so wiped out from the chemo and the surgery, this little tiny infection just wreaked a lot of havoc. I wish I had spoken up a little more when something was just a little off.
Having the laparoscopic surgery instead of an entire reconstruction made a huge difference in the recovery. It was a much more gentle procedure.
Because I had the chemo, I didn’t have to have the bowel reconstruction. What was going to be this horrible, awful surgery turned out to be major surgery but not as bad as it could have been.
»MORE: Read more patient experiences with surgery
How was your second round of chemotherapy after surgery?
I had to wait a month after my fourth round of chemo to have surgery. Then I had the surgery and had to wait another month, more like five weeks, to start up the second round of chemo.
Did you have the same side effects?
Same drugs. I felt worse after the surgery. My doctors just say, “Really?” I say, “Yeah.” But I’ve had other doctors who are not oncologists say, “Well, you had so much cancer in you. It was fighting all those cancer cells. Now that it’s all out, it’s attacking more of your healthy tissue, so that’s probably why you’re feeling a little worse.”
I was just ready to get it over with at that point. I was sicker a lot longer, so well over a week the first time, about a week-and-a-half that second one, and with that last round I was down for about two weeks. I just felt a lot weaker than I used to. I didn’t have the energy to get up and do things. I just felt really rundown.
I think the side effects were a little more intensified. I was a little more nauseous. Very sensitive to foods. My mouth was a lot more tender. Got a lot more mouth sores.
I didn’t quite feel that same electricity feeling, but my bone pain was real. The restlessness. I’m still almost five weeks out of that last chemo. I still am really restless and uncomfortable, and then some pain in the evenings.
What was the toughest part about treatment?
The toughest part about treatment would be the pain and the fatigue. That inability to get off the couch and go do stuff. I felt really cooped up just not being able to go do what I want to go do.
How was your PET-CT scan after you finished treatment?
It came back all clean. The stuff up on my chest that they were worried about is completely gone. It was a PET scan because I had that growth on my sternum.
It can leave a mark. They couldn’t tell. They could tell it was different from the CT scans. I got that radioactive dye in there. Nothing lit up. Everything was clear down to my abdomen.
For right now, I’m all clear of cancer. I still don’t feel well. I don’t have a lot of energy. I feel a lot better than I did. I’m getting stronger every day. I should say I’m excited to live the next three months not worrying about the cancer.
I’m just going to live, and then when we get to the CT scan, then I can let myself be anxious for a day or two. But I don’t want to live my life worrying about my next CT scan.
How often do you have to undergo scans moving forward?
I think it’s every three months for the first year. I’m not sure about the second year. I do know the one statistic that they did tell me that I still wish I didn’t know was that there is a 50% chance that it will come back in the first two years after treatment.
I’m just going to gear my mind to be one of the 50% that doesn’t and just try to live happy until I hear otherwise.
Life Outside Treatment
Describe the hair loss
I think as soon as I found out I had cancer, I knew I was going to lose my hair. In fact, we told our kids, “Mom will be sick. She’ll be in bed. All of my hair will fall out.” I knew from the get-go that I would most likely be bald.
I think I had geared myself up for that. I just knew it. I’m going to lose my hair; it will grow back. I’ll be great. I had long hair, and I love having long hair. When it started falling out, I had to go to a wedding, so we cut it up to my shoulder and still at the wedding. There was just hair everywhere.
When I got back from the wedding, I said to my husband, “Okay, I’m ready. Let’s shave this; let’s just do this. It’s awful having all this hair all over me.”
We went into the bathroom. I sat on a stool on the bathroom. My husband got the clippers. My 15-year-old daughter sat on the toilet just to hold my hands. I didn’t ask her to be there. She just wanted to be. As soon as my husband started shaving, I lost it.
In that moment, I felt like I had no control over what was happening in my life. No control over my body. I don’t have any control over my hair. I have no control. I felt the complete loss of control, and I was sobbing hysterically.
My little 15-year-old daughter was just squeezing my hand, saying, “It’s going to be okay, Mom.” When I felt like I was losing control of everything, her little 15-year-old wisdom realized that it was about more than just the hair.
She was like, ‘It’s all going to come back, Mom. You are going to get better. You will be able to take care of us.’
I would say, “This is not about the hair,” and she’d say, “I know it’s not, but it will all come back, Mom. Your hair, your life, you taking care of us, the things you love to do — it will all come back.” She just kept holding my hands and telling me that over and over.
I didn’t realize it was going to be so traumatic. I thought I had prepared myself. I still get very emotional thinking back about that moment because it was traumatizing. That’s the only word I can think of.
It was traumatizing having to shave all my hair off. I hate not having hair. I hate everything about not having hair. I want my hair back. I’ll go anywhere bald, but I’m dying for my hair to grow back.
»MORE: Dealing with hair loss during cancer treatment
You also lost your eyebrows and eyelashes
Later when the eyebrows and the eyelashes fell out, I remember I had done a couple rounds of chemo. I’d been sick for months. I remember going in the bathroom and looking at myself in the mirror. You look weird without your eyebrows and your eyelashes.
I just had that gaunt, grey look, sunken-in eyes, and I was hunched over. I couldn’t stand up straight. I just remember looking in the mirror and saying out loud, “Oh my goodness, I have cancer! I am so sick! Look at me; I am so sick!” It really hit. I knew I had felt awful, but how sick I was really hit.
I went out of the bathroom, found my husband, and said, ‘I have cancer.’
He’s like, ‘I know.’
I said, ‘No, look at me. I have cancer. I am so sick!’
It was, again, that feeling of, “I don’t have control over this. I’m changing so much, and I don’t have control over it.” It wasn’t even about the hair or the eyelashes then. It was about all the other things of my life, like [how] I’m really not taking care of my family.
I’m really not getting outside. I’m not doing anything I enjoy to do. I think when you see that visual and you have that visual, it also resonates with your soul, with the emotional, the spiritual, the mental things that you’re unable to do as well.
Were you surprised by your reaction to losing your hair?
I thought I would feel better. I had hair all over me. I thought it would feel better to shave it, but no, as soon as it hit my head, I was not okay with it.
I wasn’t expecting to be so emotional about it. I really did just feel this huge loss of hair and of myself and of who I am. It wasn’t so much how I looked. It was the outward gesture of what I was losing on the inside.
I sobbed. I didn’t look in the mirror for two days. My three-year-old saw my husband and my daughter sweeping all of my hair into the dustpan and throwing it away. He came into me the next morning, and he said, “Mom, why did you throw all your hair away, ’cause you know you really don’t look good like that, don’t you?”
I just started laughing. Some of my kids were scared to look at me. It took me about two days, and I just really built myself up before I actually looked in the mirror.
Then I was fine. I was like, “It’s gone. I can’t do anything about it. Hallie is right. It will all come back, so I need to work on taking those steps to get everything back.”
What helped you feel better about the hair loss emotionally?
I think I finally accepted we’re moving forward. I was so scared for the side effects of chemo. I was a lot more anxious to get chemo than I thought I would be.
I thought I knew what was coming, but when I actually had to do it, it was a lot harder. Looking at that, the hair came off. We’re moving forward. Now it’s onto the second round of chemo.
Round 1 is done. Hair is gone. We’re moving onto second round of chemo. I really did, the whole time I was in treatment, focus on the next step.
Even when I was first diagnosed, the original plan was to have a hysterectomy, bowel reconstruction, and everything first, then six rounds of chemo.
When the CT came back showing stuff in the chest, they switched it to sandwich the surgery in between the chemo so we could get working on the stuff up in the chest as well.
What helped you with the hair loss physically?
When I first knew I was going to lose my hair, I went and got a wig that looked just like my hair. I had so many people sending me caps and hats and scarves.
I thought I would still just wear a wig and be cute. I soon realized that wigs are kind of a pain, and I didn’t have the energy. I didn’t feel good enough to care about what I looked like when I went out.
But my head was cold all the time. My neck was really cold, even with a beanie on. I found I liked the beanies because they kept my head warm when I was outside. When I was inside, I just went bald because I don’t really like stuff on my head.
Even with a beanie on outside, I was really bothered by the draft on my neck, so sometimes I would wear a hoodie. I’d have the beanie on, wear the hoodie, put the hood up just to keep my neck warm. I wore scarves more. I did not like that cold feeling coming on my neck as much as my head.
I looked ridiculous. I had my beanie, I’d have my hoodie, I’d be walking around in my slippers, and I didn’t care because if I was going outside, I wasn’t going to waste my energy to get ready. I was going to use that energy to go watch my boys’ basketball game or something.
By the time I would try to get ready, I’d be so exhausted I couldn’t go out, so I just gave up on looking cute at all. If I can go and be there, that’s good enough for me right now.

You had to experience hair loss again after the second round of chemotherapy
My hair did grow about an inch during those two months, and it was traumatic to lose it all over again. It didn’t matter that it wasn’t my long locks of hair.
It was hard to see, to wake up and have the pillow full of hair. To just feel like, “Ugh, I’m still in this. I still don’t have control.”
It’s just a reminder of what you’re missing. But I was ready. That was the next step, so I was just ready to do the next step.
I didn’t have the same traumatic and emotional response to losing it, but I did have those same feelings of, “This thing is running my life. I just want a little bit.” I kind of felt I was moving backwards again. It was hard to lose my hair again, just what little bit I had.
I wasn’t sobbing, but I did cry about it and have those same feelings of, “I have cancer, and I can’t do this, this, this, and this.” I just think for some reason the hair loss just brings that up for me.
What helped you manage your thoughts and emotions?
My husband and my mom. Everyone was planning the surgery and being gung ho. I stayed focused on that CT scan. They said they didn’t think it was going to show anything. Nobody thinks it’s going to show anything.
But all I thought about was when the CT scan is done, then I’ll make the next plan.
When it came back showing stuff in the chest, my mom and my husband were a little bit rocked because they had already moved forward. They had made plans for the surgery [and] had people come to stay with my kids, and I hadn’t.
I wasn’t rocked or felt like my plan had changed because I had just kept it going step to step. I think that really helped me. I didn’t have big surprises because I wouldn’t let myself think far enough in advance to get surprised.
I’m a very spiritual person, so my own thoughts and my meditation — ’cause when you’re just laying there on the couch for months on end, you have a lot of time to lay. Even with the kids around, I just always made sure I had some quiet time every day where I just laid there and got my brain right and got in good space.
I had this line or this path that I knew I wanted my thoughts to be on this path. I want to be positive, I want to fight, I want to keep going, I want to be a happy person, [and] I want to be a grateful person. But with those emotions, when I would get off and I would start feeling ungrateful or start feeling scared or sorry for myself, I would let myself go there for a minute a little bit.
Then I would say, “It’s okay. Cry. This is really hard, this is really painful, and this is really scary,” whatever the emotion is at the time. I would feel like I was getting off this little path. Then I’d say, “Okay, you had a little break. You’ve had your break; come get back on the path.”
I would remind myself that I was doing it, I was strong enough, I had my medications, [and] I had things to make me feel better.
That’s always how I visualized it. This little path, and maybe I’d get off the path a little bit. I always visualized myself bringing myself back onto that path.
It helped because I didn’t give myself the opportunity to mourn things or to be sad. But I always ended up by bringing myself back to where I wanted to be.
How did you manage your energy levels?
I had great friends. They would just come up. Where I lay on the couch in my house is so awkward. There’s not a great place to sit, but they’d just come sit on my fireplace and talk to me, bring me things.
If I was feeling good enough, I would have people say, “We’ve got to get you out of the house, even if we take you to Costco and you just ride around the little cart in Costco.” They knew my limits. They could tell when I didn’t feel good.
I didn’t waste my energy on things like cooking and cleaning. When I had people helping, my friend brought over dinner at the start. I said, “I feel so bad because you brought me dinner, and I’m going to go watch my boys’ basketball game.”
She said, “I brought you dinner so you could can go watch your boys’ basketball game.” She said, “That’s why we’re doing our little food train, because we want you to get out and go see your kids.”
I would try to get out, and as hard as it was, I’d go to their basketball games, I’d go to their baseball games, [and] I’d go to their little programs at school.
I didn’t worry about the laundry, cooking, cleaning. I just let other people do that for me. That was good because you make those connections with people instead of just laying on the couch feeling sorry for yourself.
I could get out and do some things here and there. I made sure I tried to do that almost every day. Some of those post-chemo days, it was not happening.
Were there any big surprises during treatment?
The biggest surprise was the amount of support I received. I think some of it is just because I let people help me, but I cannot believe the number of people that wanted to help my family that have helped my family.
That was the biggest surprise to me, just how good people are. How when they see you in crisis, they just jump in and take over. Doesn’t matter if you’ve had a hurricane and a huge flood, and you see those rescue work people out there, the helping hands down in Houston. That was kind of all going on.
I thought, “I have my own people who are here to rescue my family.” That was the biggest surprise.
I would say physically I was surprised at how hard it was to lose my hair. I knew it was going to be painful, and I was surprised at how much my body’s been able to endure.
Your human body can really withstand a lot.
I knew it was going to be painful. I just didn’t know it was going to be that painful, that emotional. All those things. Just how resilient my body’s been through it, how it was able to do it.
“Let yourself feel”
My husband was like, “Stay positive, stay positive!” I would maybe start to voice my concerns or worries, and he’d say, “You can’t think like that.” Everyone would try to pep talk me, so I started saying, “No, I have to feel this. This is scary, and I have to think about what if my kids don’t have a mom.”
I get to have that thought, and I get to work through it. I just found that those things were better if I did it by myself. Then I have a friend who’s a great listener, so I would tell her after. I would say, “I went to that dark place today, and this is what I was thinking. This is how I got myself back out.”
I would explain my process to her, but I wouldn’t really include them in the process because I felt like they want so much to help me. At one point, I did say to my husband, “You have to let me feel these things and work through these things, or I’m not going to be able to stay positive.”
You and your spouse had to work out a system in who would do the research
I’m usually the big researcher. I was thinking I had ovarian cancer from researching my symptoms so much, but as soon as I was diagnosed with cancer, I just had this feeling that I just didn’t want to know.
There’s so many opinions on how to treat cancer. I just needed something constant, so I didn’t want to Google life expectancies. I didn’t want to know life expectancy. I didn’t want to know the worst. I just wanted to know the next step.
My husband wanted to know the worst. He wanted to know what could happen. I think, in a way, he felt like if he knew what was happening, he could fix it. I just knew that I had zero control. I knew I had the most common type of ovarian cancer, but I still need to go and look up what the name of it is.
I didn’t even want to know that because I felt the more I was reading about it and people would tell me things about it, I felt I was worrying about things I didn’t need to be worrying about.
Just knowing about it was causing anxiety, so I’m like, ‘Whatever the next step is, whatever the doctors are saying the next step, I’m good with that. Just don’t make me worry about all these things that could happen. Until they’re happening, I don’t want to worry about it.’
The second I was diagnosed with cancer, I knew. I just had this feeling in my gut to not research this. I had a good friend that went out and researched a bunch. She came back and said, “Whatever you do, don’t Google ‘ovarian cancer.’ You’ll be really scared.”
I said, “I know. I’m not.” So I told my husband, “I don’t want to know these things because I’m already so sick and dealing with so much that I can’t worry about the what if’s. But if you need to know the what if’s, go for it.”
The doctors knew that, so he would come to my appointments with his little binder. They would give him all the information or write things down for him in the binder just because they knew I didn’t want to know.
I really think that made a huge difference in my emotional and mental dealings with the cancer, because I did not have any fear of what could happen.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How was the financial part of the process?
I was raising my six kids full-time, but my husband has insurance. I just was assuming it was going to be really expensive, and it is. We’ve done some fundraisers. Some of my friends and family have put together some fundraisers, and I just tucked that away in a separate account.
I just make monthly payments on my bills. At first I was making big huge chunks of payments, and I kind of realized that smaller payments over a longer amount of time were going to work a little bit better.
I’m feeling like I might have to get a job to pay off my cancer bills. Smaller chunks over a longer period of time will give me a little bit more time to get healthy to pay off our deductibles.
Did you use alternative or holistic medicine?
I’ve looked into a little bit. The one thing my doctor did say to me was, “Nothing you ate or drank caused your cancer. Nothing you eat or drink is going to take your cancer away.” She just said there are great, healthy things out there to try.
She asked me to please not be extreme and to keep eating. She didn’t want me juicing. She wanted me to keep my energy up and to feed my body. I really listened to my doctors with that, but I did try to eat healthy, exercise.
I’ve done acupuncture. I just recently started acupuncture when I was going through my treatment. I also have rheumatoid arthritis, and I haven’t been able to have any treatment for that while doing the cancer treatment, so that’s been very painful and difficult along with the cancer.
I’ve heard so many cancer patients say acupuncture has helped them and so many rheumatoid arthritis patients say acupuncture has helped them. Since I finished chemo, I have started acupuncture, and I love it.
It feels really good. I don’t think I’ve been enough to see the physical effects yet, but there’s something about it where you get in a very good mental place, where you’re just laying there with these pins all over you.
They just have you focus on your breathing and your meditation. I felt like I really have been able to get myself in a good place. I’ve been struggling since I finished chemo because I feel like I should be feeling better than I am.
But that is one part where I go, and I can really bring my thoughts back around to, “You’re doing good. Look, you’re at acupuncture. You’re not on the couch; you’re doing good!” I have tried that, and so far I’ve loved it.
»MORE: Read other patient experiences on yoga and meditation
Support and Parenting
What’s your advice to people undergoing treatment for ovarian cancer?
I’ve talked a lot about not Googling and not doing those things. I still kept myself very well educated. I asked my doctors a lot of questions, but I would not scare yourself. I just wouldn’t go searching for things to worry about.
I would really turn to the source, which is your doctor and your caregivers. I would base your decisions and stuff on that because you are not going to get all the clutter that you would get if you go out and Google, “What happens if you have ovarian cancer?”
A lot of different things can happen. You just want to know from your doctor what’s likely going to happen to you. They’re the ones that can tell you that.
The other thing I’d be really big about is to let people love you and help you through this. Just take care of yourself and let other people take care of the other things.
It will just give you so much freedom to work through things and to get healthier.
It gives the people who love you the opportunity to do something for you instead of feeling helpless. I think that strengthens the relationships all around. Instead of getting frustrated and mad at each other, you really come to love each other more.
How important is it to have caregivers?
When I was first diagnosed and going through it, my husband would call the moms and say, “We need you. Come out.” They would just jump on an airplane and come out. I would say, “Why did you do that? I’m fine.”
He’s like, “You might be fine, but we aren’t.” He would say, “I can’t take everyone everywhere they need to be and do my work and everything.”
Towards the end, after the surgery, when I started having chemo, it was me. I was on the phone saying, “I am so sick. I need you to come out and take care of the family. I can’t even drive the kids to school or pick them up anymore.”
I think it’s everything to have caregivers, just so you can work on getting better. So you can use that energy, the little energy that you do have, doing things that matter most, like things with your kids or with your husband or keeping up those relationships.
You use your energy maintaining your relationships instead of doing dishes. That was really important and a really hard thing to do.
The sicker you get, the less hard it is to just let someone else take care of things. I also talked to the caregivers. I said, “So glad you’re here. I’ve got to tell you, I feel a little worthless laying on the couch. I need to feel like a mom.”
At first my kids would come to talk to me, and they’d say, “Don’t bug your mom. She’s sick.” I’d say, “No, I want to talk to my kids. I want to know what’s going on. Let them come bug me.”
I told the caregivers that I needed to feel like a mom. I need to feel like a person, so if my friends come over, let them come in and talk to me.
If the kids ask to go to their friends, make them come and ask me. Just let me feel like a mom a little bit. Let me help with the homework if I can. Let me do the little things I can do so I can still feel like a person.
There’s no way I could have taken care of myself without a caregiver, let alone a whole family. I think even if you’re by yourself dealing with cancer, you have to let people take care of you. You just have to.
»MORE: Parents describe how they handled cancer with their kids
Advice to cancer patients on how to ask for help?
I would just ask. It took me a long time to get to that point.
Sometimes my mom and my mother-in-law would both be in Utah, and I would be there usually the week before chemo, when I was feeling the best.
I would be doing things by myself. I did have some bad days. I remember texting them and saying, “I can’t go get my kids from school today.” We’re doing three or four after-school pickups because they’re in so many schools. My friends would just do it.
I just got comfortable enough. I would only ask certain people that I felt really comfortable asking. Anytime somebody said, “What can I do for you?” or, “I want to do something for you; I just don’t know what. What can I do?”
I would say, “Hallie’s got this big project and needs to go to Michael’s and get some stuff. Could you run her down to Michael’s for me?” I would just say that. I just started thinking about what we had on our list. I probably could have taken her down, but I probably couldn’t have walked around the store with her.
There’s some sense of I’m doing it for my kids. They need this, and so I can’t let my stubbornness stay in the way.
»MORE: What kind of support cancer patients say helped the most
With my husband, I knew he was spread really thin. When some of our male friends, some of our couple friends, would say, “What can I do for you?” I’d say, “Can you please take my husband out golfing? Just get a tee time and invite him to go golfing. I would feel a lot better right now if I knew he was getting some down time, too.”
Just saying, “You just have to say yes.” Give people, if they don’t know, give them something. I really learned people are really asking because they really want to help you.
How many children do you have, and how old were they when you were diagnosed?
Six children. They were 15, 13, 11, nine, six, and three years old when I was diagnosed.

How did you manage your emotions around the children?
Every time we got a round of treatment or it was time to go in for another chemo, it would kind of be a celebration that we’re moving forward.
When I had my surgery and the news was great, of course we were happy, but I just never let myself get too excited or too ahead of myself. When I got the results of the PET-CT scan, I was thrilled because I desperately felt like I needed a break from treatment.
My husband still said, “…if you come off Cloud 9,” and I said I never really stepped on Cloud 9 because I don’t feel good enough to get to Cloud 9. Part of trying to keep that evenness is because I have six kids. I don’t want to put them through an emotional roller coaster, like things are great, and now I’m really sick, and things are great.
There would be times when I would really not feel well. Especially after some of those chemo treatments, I would cry and cry pretty hard. I just couldn’t control it. I just hurt, and my body just cried. It would kind of scare my kids a little bit.
My older kids, I really talked to them and said, “When I cry, I’m okay. I just hurt, and it feels better to cry. I’m okay.” My little kids — that was really scary for them.
I would get my husband or bigger kids and say, “Take the kids outside. Go upstairs; go somewhere else. I’m crying, and I don’t want the little kids to be scared.”
Part of that roller coaster was the thought of telling my kids I was cancer-free because they’d be so excited.
I said, “We’ve got about three months to have a lot of fun, and I’ll have another scan. Now that it’s gone, our job is to keep it away. There might still have to be stuff I have to do in the future, but for right now I’m great.”
Kids don’t understand the same way adults do, and I didn’t want to take them on that emotional roller coaster. When they were at school or I had some free time, that’s really when I would let myself process things or have those moments of, “I don’t want to do this anymore. I want this to be over. My body is exhausted. I just hurt; I don’t want to be in pain.”
You just have those moments. I would let myself have those moments, but I would always make my brain circle back into a positive space. I’m like, “Okay, I went there. Now I’m getting back.” I had to be there for my family.
What are the extra considerations for a parent undergoing treatment?
Just the day to day of taking care of a big family. My parents came out and stayed for a week. They live in Utah and I live in California, so my mom would come out and stay for weeks at a time and take care of the family. My mother-in-law lives in Utah. She would fly to California and stay for weeks at a time.
I think the biggest thing is when I was first diagnosed, so many people wanted to help me. My first reaction was, ‘No, we’re okay.’ I’m a very private person. I didn’t want everyone in my space.
But I just decided to say yes once, and then I promised myself anyone who offers to help, I won’t say no. No matter what it is, I’ll say yes. That was huge when I’m a control freak. I like to run my house. I like to take care of my kids. I like to be the one doing that.
I just let that go. I focused on myself, getting myself better, and what I needed. I didn’t have a lot of that extra stress. I just let my mother-in-law, my mom, my friends, [and] my neighbors take my kids, play with my kids, [and] bring in meals.
I didn’t cook for months and months. Friends and families brought in meals. I just let them and was so grateful because when you’re in the thick of it, you cannot make yourself do those extra things.
My husband was doing a lot with the kids. That’s one thing. I didn’t demand his attention a lot because I felt he was working and taking [care of the] kids. He had other things going on. I felt like he was already spread pretty thin, so just for him to come rub my feet at night or for us to have a short conversation was enough.
»MORE: Parenting with cancer
Any advice to other parents who are dealing with cancer?
I would definitely say to be honest with your kids. I think they are a lot more scared when they know something’s wrong, but they don’t know what it is.
Even though my kids were scared of the C-word, cancer, they would go to school, and they would come home after school and say, “Somebody said you can die from cancer. Can you die from cancer?”
I said, “Yes, you can die from cancer, but Mom is not there. I’m doing treatments, and it’s working. I’m getting better right now. If it ever got bad and I was going to die, I would talk to you about that. I would tell you.”
»MORE: Breaking the News to Family and Friends
That just brought so much relief. Especially my six-year-old. She’s old enough to know what cancer can do but still young enough she just doesn’t understand it like the older kids do.
When I would get chemo and I would be so sick, she would come crawl up on me by the couch and sob and sob that she wished I didn’t have cancer because she was so scared.
I would tell her, “This chemo is yucky. Mom really hurts, but this is what I have to do to get better, and I want to get better.” I have the little schedule for my sessions, so I knew I would be done with chemo in May.
I would keep telling her, “When you’re done with school, I’ll start to feel better.” But I’ve also been honest that we have to track it, it could come back, and if it comes back, I might have to do some more treatments.
The mortality has never come up. They’ve never discussed time frames or anything like that with me. My doctors have never given me anything like that, so I don’t give that to my kids.
But if they did, I would be honest and tell them because it’s a lot scarier wondering if your parent is going to die than to just know. If they know, they can talk to you about it and process it.
If not, then their little brains are all alone trying to figure out what’s going on, so I just think being direct and honest without too many details.
Just like I didn’t want to know all those details because I didn’t want to worry about the what if’s, I don’t want to give them any what if’s. I don’t want to say, “No, my cancer’s not going to kill me,” when I really don’t know what’s going to happen.
I want them to know it’s not going to kill me now, and things look great. I’m really excited about the way things are going. That’s what I say I’m really excited.
Every time I got a CT scan or even just my blood levels drawn, I’d come home and say to my kids, “My CA125’s dropped all the way down to 50. That’s such a good sign!”
They knew enough about that, so I would give them all the positives I could of it but answer their question honestly. Can cancer kill you? Yes, it can, and people have died from cancer.
But right now, my doctors aren’t talking to me about dying at all. We’re talking about living, so we’re focused on living. Just trying to keep it a positive spin like that, still being honest.

Inspired by Jodi's story?
Share your story, too!
Ovarian Cancer, Epithelial Stories
Heather M., Epithelial Ovarian Cancer, Stage 2
Symptoms: Extreme bloating, pinching pain in right side of abdomen, extreme fatigue
Treatments: Surgery (total hysterectomy), chemotherapy (Taxol once a week for 18 week, carboplatin every 3 weeks), concurrent clinical trial (Avastin) every 3 weeks
...
Jodi S., Epithelial Ovarian Cancer, Stage 4
Symptoms: Extreme bloating, extremely tight skin, changes in digestive tract, significant pelvic pain, sharp-shooting pains down inner thighs, extreme fatigue
Treatments: Chemotherapy (pre- & post-surgery), surgery (hysterectomy)
...


One reply on “Jodi’s Stage 4 Epithelial Metastatic Ovarian Cancer Story”
Just hearing Jodi talk about the electricity throughout her body felt validating. I just finished my hopefully last round of chemo for ovarian cancer, and after each treatment I would get that horrible electric shock feeling throughout my body. The Drs and nurses always acted surprised like they never heard of such a thing. The neuropathy following was nearly as bad. We are so much stronger than we realize!