Keyla’s Stage 1 PMBCL Non-Hodgkin’s Lymphoma Story
Keyla was diagnosed with stage 1 primary mediastinal B-cell lymphoma, a subtype of non-Hodgkin’s lymphoma.
In her story, she details undergoing chemo, how she managed hair loss, parenting with cancer, and how to ask for help during treatment. Thanks for sharing your story, Keyla!

- Name: Keyla S.
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Primary mediastinal large B-cell
- Stage 1
- 1st Symptoms:
- Bad cough
- Slight trouble breathing
- Treatment:
- Chemotherapy: R-EPOCH (Dose-Adjusted)
- 6 cycles, each cycle = 3 weeks
- Week 1: continuous infusion through PICC line (arm) or port (chest) for 24 hours lasting 5-6 days
- Week 2: side effects tend to kick in, ranging from nausea to mouth sores
- Week 3: typically the healing week when blood cell counts recover
- Note: If your white blood cell count (WBC) doesn’t rebound back into the standard range, your next chemo cycle may be delayed.
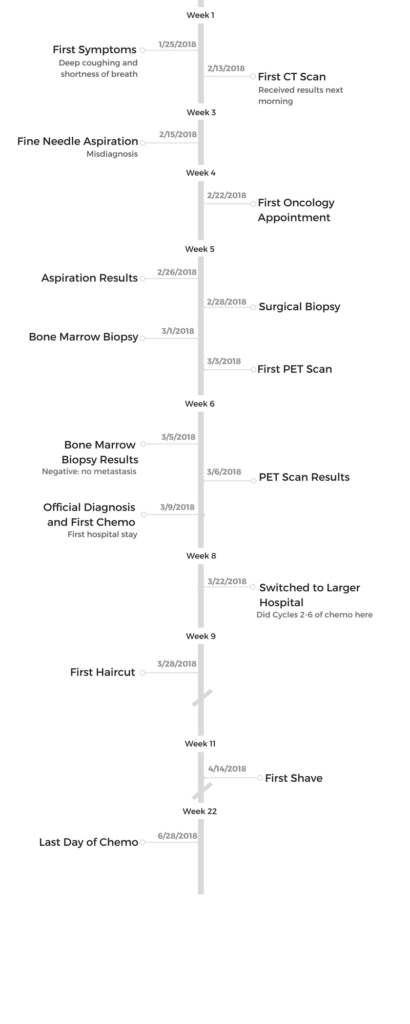
- Diagnosis and Treatment
- How did you get diagnosed?
- What tests and scans did you undergo?
- How did you choose hospitals?
- What was Week 1 of chemo like?
- Describe Weeks 2 and 3
- Sensitive scalp issues
- How did you deal with chemo?
- How was the port?
- What was the worst part of treatment?
- What got you through that worst part?
- Describe the scans you've undergone
- Describe the waiting periods after tests and scans
- What was the biggest surprise?
- Symptoms and Support
- What were the side effects?
- Describe the side effect cycle
- Were you prepared for the side effects of treatment?
- What helped you the most in dealing with side effects?
- Describe the hair loss
- What helped with the hair loss?
- What helped when you lost all your energy?
- How did you manage your thoughts and emotions?
- What do you wish you had known before you began chemo?
- Be your own advocate
- How important is it to have caregivers?
- Can you work during treatment?
- Parenting with Cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Remember, just because you have cancer, it does not mean that you should let it define who you are or what you do.
Make the most of the time you have and enjoy it to the fullest. I can truly look back on my spring and summer and say I had a great time, in spite of what I went through.
Keyla S.
Diagnosis and Treatment
How did you get diagnosed?
I found out Valentine’s Day morning, just 3 days after giving birth to my first baby girl. My husband and I were woken up at about 7:00 a.m. in the hospital to a thoracic surgeon we had never met before, telling us they found a 20-centimeter mass in my chest that was most likely malignant.
This doctor thought we knew about the mass and that he was just informing us that he did not think is was benign. That was not the case.

We were completely caught off guard. In fact, I remember my husband looking at me and back at the doctor over and over again with the most shocked looked on his face, which had gone completely white, and repeatedly saying, “You said it’s not cancer, right?”
Wrong. I started showing “signs” about 2 weeks prior to giving birth with just a bad cough and a little trouble breathing that I thought was caused by being pregnant.
Scans and tests
Once I gave birth, the doctors did an X-ray of my chest and originally thought I had a pneumonia, so they ordered a blood culture. It turned up a false positive for staph in my blood, which they treated me for through a PICC line in my arm for 2 weeks.
From there, they decided to do a CT scan, which showed the tumor. I was in shock. The only thing I said was, “Okay.”
I was ready to fight it, and I really didn’t even know what ‘it’ was at the time.
I went into surgery the next morning because I had a baseball-sized lump under my right armpit. My surgeon thought it might have something to do with the tumor.
I had brought this lump up to my OB/GYN during my visits, and she assumed it had to do with my milk supply coming in. We found out immediately after surgery that she was correct. That was our first win against cancer.
What tests and scans did you undergo?
In the following 3 weeks I had a needle biopsy, bone marrow biopsy, a port placed, a surgical biopsy because the cells from needle biopsy had dried up by the time they reached the Mayo Clinic, and a PET scan.
I’ll be honest, the bone marrow biopsy hurt, but that was probably because she couldn’t get enough fluid, so she had to do it 4 times. I don’t think that normally happens, but the surgical biopsy was probably the worst. It hurt for weeks after, and I’m now left with a decent-sized dent on the right side of my chest where the scar is.
‘Battle wounds,’ we call them. I’ve learned to accept these. They’re part of a story I’m grateful I get to tell.

How did you choose hospitals?
I didn’t at first. I didn’t even choose my oncologist at first. She was chosen for me by my surgeon. As soon as my port was placed, I was given a day and time for an appointment with an oncologist who worked out of the same medical network as my surgeon. I’m assuming his team set that up for me.
I did whatever they told me to do. I really just went through the motions and didn’t question anything. Whatever I needed to do to beat this and put it behind me, I was willing to do.
After hearing that the cancer I had was curable, after thinking for a little over a week that it wasn’t, I honestly didn’t care what I went through. I knew it was going to be a temporary bump in a long road ahead, and I didn’t care how bad it was as long as I was able to get to the other side.
After the first round of chemo, I was really able to assess the situation better and sit down with my husband to discuss if we really wanted to continue at the hospital where I did my first treatment, with the oncologist we had, or if we wanted to get a second opinion.
Always get a second opinion if you feel anything off at all with who is treating you. That was my moment of speaking up. Once I switched hospitals and doctors, I didn’t have to speak up. Everything just clicked.
What was Week 1 of chemo like?
At the time, I didn’t know what to expect from chemo. We were given a diagnosis and checked into the hospital later that day. I didn’t have time to look anything up or ask anyone. I was in a hospital that, quite honestly, probably shouldn’t be treating chemo patients, in my opinion.
My port was accessed just days after being placed, which was a little rough to begin with. But looking back, it was the very least of my problems for that first round.
The hospital I was staying at over those 5 days had all us chemo patients shoved into one hallway on a floor not designated for cancer patients, with nurses and nurse aides taking care of us who knew basically nothing about chemo.
There had to be 2 chemo-certified nurses on the floor at all times, but it would take hours before I saw one if I had a question or needed anything that had to do with my chemo — the entire reason for my visit.
Week 1 side effects
I had a bad reaction to the Rituxan the first night, including a 103-degree fever and cold chills that uncontrollably shook my entire body for 20 to 30 minutes.
That was really the only bad reaction my body had during the first round. And swelling, but that would have been better if they would have let me leave my room and walk.
At the hospital I’m at now, I’m encouraged to get as much exercise as possible. I usually ride the exercise bike they have here for about 40 to 45 minutes each day I’m there and take 5 to 10 laps around the floor.

I was also put in a room with a shared bathroom with another chemo patient during my first hospital stay. I ended up walking into [the bathroom] during one of my days there and finding a dirty bed pan left on the seat of the toilet, probably not the best thing for someone going through chemo — or anyone for that matter.
I also had chemo poured on me twice by one of the nurses changing my bags. Yeah, I definitely recommend finding a hospital you trust that has a good reputation for exactly what you’re going through.
I was all smiles during my stay. I always focused on the positives. It really wasn’t that bad as far as side effects go, or maybe I was just so thankful to have my life and know there would be an ending to everything I had to go through that it didn’t seem as bad. Nothing this entire time has been even close to unbearable. It’s not nearly as awful as I anticipated.
Describe Weeks 2 and 3
Weeks 2 and 3 I just focused on taking things day by day. I didn’t know what to expect, so everything was a little scary. Any time I started having symptoms, my husband and I looked it up on our stack of papers we were given from the hospital with every medication and side effect.
My mind was put to ease knowing it was something normal.
I get very tired immediately following each treatment as I come down from the steroids, and typically just stay in bed for the majority of the day that first day I’m home. I have swollen knees, legs and feet for the first few days once I leave the hospital, which makes it difficult to walk.
My face gets very swollen each time from the steroids and fluids, but that usually only takes about 2 weeks to go down. The tingling in my fingers was a weird feeling those first couple of weeks after my first round, but I’m used to it now.
Sensitive scalp issues
I think the worst thing during those first few weeks was how sensitive my head got. It actually started burning, and at one point I had taken a shower, gotten out, and my hair just stayed in one lump from shampooing it. I wasn’t even able to brush it.
I called my friends, turned on some fun music and cut it off, then had one of them shave it. I didn’t mind losing my hair. I knew losing it was coming eventually. Why get upset about it? It was all temporary, and it felt good at that point, physically and mentally. I shaved it short but not all the way down. I didn’t shave it completely bald until after the second treatment. It was too sensitive before then.
»MORE: Patients describe dealing with hair loss during cancer treatment
How did you deal with chemo?
Chemo really is this scary thing we hear about, but going through it myself, it’s really not nearly as bad as I had anticipated.
That feels weird saying, because I definitely don’t look forward to it or enjoy how I feel during this time. I hear some of these stories of people who have to go through so much worse, and I feel like what I go through is almost next to nothing comparatively.
For a couple of days after leaving the hospital, I’m weak and tired and have nausea and stomach pains, but it only lasts a few days for the first couple of rounds and lengthens a little each time.
I really don’t think that it’s awful to go through. The mouth sores are annoying and do hurt a little, but nothing intolerable, and they didn’t start till after my third round.
The bone soreness from the Neulasta shot is a little difficult to deal with. I have been stopped in my tracks a lot from the pulses it sends throughout my body, but it’s nothing too horribly bad.
Honestly, chemo and the 2-a-week lab appointments in between each cycle to check my levels is more of an annoyance for me, because it takes me away from my family and my newborn baby, but it has become my new norm. I just keep telling myself that it’s all temporary and that it’ll be over soon. I have so much to be thankful for, and my focus on that has been a key in staying positive throughout this process.
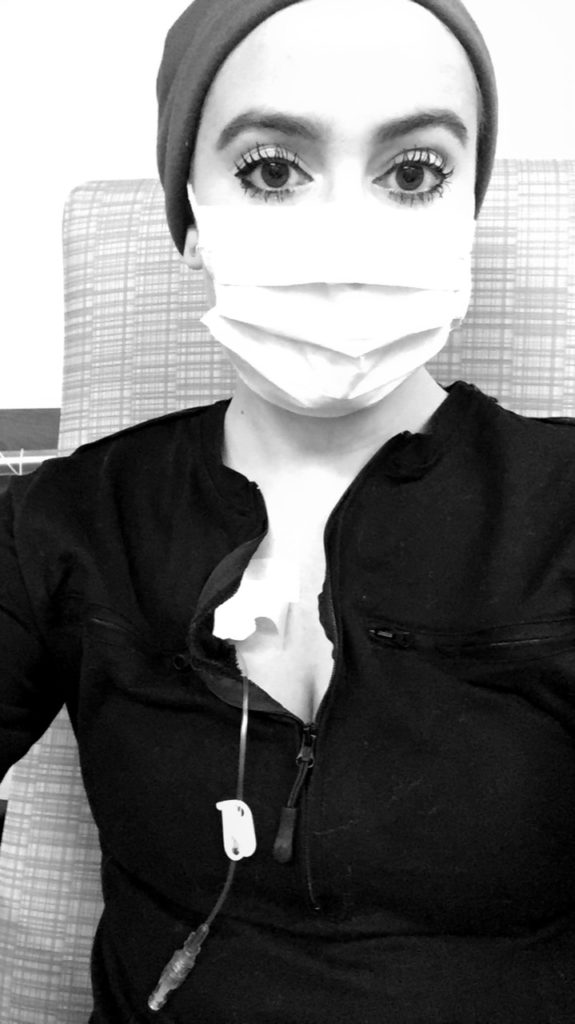
How was the port?
I was so nervous about this port. I had no idea what it even was, but it has truly made this experience so much easier for me. My veins are tiny and do not react well to needles, so getting a port has simplified dealing with needles.
It had a little issue getting blood return from it after my first round, but the nurses at the new hospital I went to used a Cathflo (helps restore catheter function) to flush it out, and it has worked perfectly since.
What was the worst part of treatment?
Losing my eyebrows and eyelashes, along with the face swelling from the steroids, completely changed how I look. I have always had very thick lashes and brows, so to me, this was much worse than losing my long hair.
Even this didn’t really affect me too much until after Round 4. I just took less pictures of myself and didn’t look in the mirror as much. Maybe it was a blessing!
I have definitely learned that what I experience in life is so much more important than how I look doing it.
With that being said, I do feel like I was deprived of that “new mom” experience because of having cancer. I’d spend 4 to 5 days every 21 days in the hospital, followed by 8 hours of Rituxan as an outpatient on the eighth day, then feeling sick for a week or so after, and getting labs done twice a week, then starting to feel better only to go right back in the hospital.
I’d say I have been at a disadvantage when it comes to being able to spend quality time with my little girl. That’s probably the worst part for me.

What got you through that worst part?
I found that not looking in the mirror as much as possible — especially when I am in the hospital, and my face swells and gets very red from the chemo — and just focusing outward on what’s going on around me versus dwelling on how I see myself currently has really helped me when it comes to being concerned about my looks.
Lots of FaceTiming helped me cope with not seeing my kids while I do my hospital stays.
Describe the scans you’ve undergone
I’ve had 2 PET scans. I had one before my first round of chemo and one after my second round. After my second round, my PET scan showed that on the SUV scale (a scale that determines how active my tumor is by how much sugar it absorbs), my tumor went from over 10 (very active) to a 2.35, which was great. It had also shrunk from 20 cm to 12.5 cm.
The scans were easy and painless.
The first one was a little uncomfortable because I wasn’t able to lie on my back for very long without coughing because of where the tumor was and how large it was, but by the second scan, my cough was completely gone, and I was able to lie on my back without any issues at all.
Describe the waiting periods after tests and scans
The unknown was a bit scary. I think the worst one was the week in between hearing that I had an incurable type of cancer with a 10 to 12 year life expectancy to having the surgical biopsy, which determined that I did in fact have a curable cancer.
During the other periods of time between scans/tests and the results from them, I really just focused on my family and friends and spending as much time with them as possible.
I wanted to feel normal before the crazy started, so that’s what I chose to do. I didn’t dwell on what could be, but instead enjoyed what I had in front of me.
»MORE: Dealing with scanxiety and waiting for results
What was the biggest surprise?
Definitely finding out that my cancer was incurable and then getting that surgical biopsy done and determining it was in fact curable. I would say that was the biggest, best surprise I’ve ever experienced in my life.

Symptoms and Support
What were the side effects?
Quick note: the list looks long, but it really hasn’t been horrible for me so far. These are just some of the things I noticed.
- menopause
- hot flashes
- confusion
- neuropathy in fingers
- low white blood cell counts (neutropenia)
- low potassium
- swelling in legs, feet, face, stomach (from steroids and fluids)
- sensitivity to sun
- lightheadedness
- hair loss (everywhere)
- muscle weakness
- mouth sores
- sore throat
- joint pain
- fatigue
- nausea
- stomach pains
- loss of appetite (after third cycle)
Describe the side effect cycle
The only side effects I had while in the hospital for my 4-day rounds was swelling of the face, knees, legs, feet, hands and stomach. I actually felt pretty great during my stays otherwise. The day I leave the hospital, I still have a lot of swelling, but the steroids keep me energized. They start wearing off through the day, and I get a little tired.
By the second day, I have all-over body soreness, and it’s a little painful for people to touch me. I have a slight cough, and my throat usually has a tickle for a few days. The tingling in my fingers starts my second day home as well, along with a little nausea and stomach problems.
My legs and rest of my muscles are also pretty weak during this time, and it’s more difficult to get up and down on my own. The side effects are pretty much the same every time. They just get a little worse each cycle.
Were you prepared for the side effects of treatment?
I don’t think you can really prepare yourself for the side effects. I honestly just dealt with them as they happened, and after a couple of cycles I knew what to expect.
It seems like a long list, but it really isn’t horrible. It hasn’t been for me, at least.
What helped you the most in dealing with side effects?
Take Zofran before you eat by at least 30 minutes. Don’t wait for symptoms to start; be proactive. Also, I started getting the Magic Mouthwash while I got my Rituxan during outpatient on Friday’s following my cycle and using it before I got sores, which helped prevent them from getting bad.

Describe the hair loss
Hair loss on my head wasn’t a big deal for me when it happened. It was actually a relief when I shaved it off because my head started to be very tender and burn a little as my hair was falling out.
The hair loss on my face was more difficult because I have always had very thick eyelashes and eyebrows, so I didn’t enjoy that by any means. They start to grow back between each cycle, so I know they’ll come back quickly. It’s definitely nice not having to shave my legs though!
What helped with the hair loss?
I purchased a wig and also had someone give me one, but I mostly just rock a light beanie or go bald and proud. I’ve learned that I care much more about how I look than anyone else, and I can’t even see myself on a regular basis. So why dwell on something I can’t control?
What helped when you lost all your energy?
I can’t say I really lost all my energy. Sure, I’m tired after each round for 4 to 5 days or so, but I get some sleep while my mom and husband take care of the kids for a day-and-a-half after treatment. Then I suck it up and realize I have a household to take care of, and life goes on whether I have cancer or not.
I just focus on my kids and my family and friends and don’t mope around with a “woe is me” attitude. Sorry, I’m blunt, but that’s what has worked for me!
How did you manage your thoughts and emotions?
Talking to my family and friends about how bad I was feeling, physically and mentally, seemed like a burden. I never wanted to be a victim or have people think of me this way, so I write.
I started writing letters to my kids through this process, and that’s helped get my feelings and thoughts out. I plan on continuing these letters and giving them to all 3 kids by the time they’re 18.
I will say that I have enjoyed my summer so far and encourage anyone who has to go through this to try and enjoy as much time as you can with people you love, doing things you love. I got out and lived in spite of what I was enduring physically and mentally. That was the best decision I could have made.
What do you wish you had known before you began chemo?
At the time, before I started my first round, the unknown was a little scary, but I’m glad I didn’t really know what to expect. Ignorance was bliss, looking back.
Be your own advocate
I pretty much just went with whatever my doctor told me. When I didn’t feel like something was clicking, I took the necessary steps to change it, like I did with my doctor and hospital.
» More: How to Be Your Own Advocate
How important is it to have caregivers?
For me, it has been very important, especially having caregivers for my kids when I’m either not there or not at 100% physically.
There are times when I think I’m superwoman, and I can fight through any side effect and just tell myself it’ll be okay, but I have learned that I need someone there with me for about a week after leaving the hospital each time.
I put myself in a scary situation once where I had the baby by myself at home 3 days after my third round, husband at work, and I got very lightheaded and had to do everything I could not to pass out for about an hour straight.
I had to call friends of ours who lived nearby to come over immediately and make sure the baby was taken care of, and I pumped myself full of fluids, laid down and had my father-in-law come stay with me for the rest of the day.
I’ve learned to be okay with help from others and that sometimes I can’t do it all all by myself.
Can you work during treatment?
I was very fortunate in the sense that I had my baby and found out about my cancer 3 days later, because I was able to be on maternity leave from work during the same time as the majority of my treatments.
I have heard of people working a little during the same chemo I am receiving, but I personally didn’t want to risk getting sick and delaying my treatment process, so I chose to stay home the whole time.
I plan on taking a little over a month off once my sixth and final cycle is over before I return to work. It gives me more time with my baby as well, without interruption from hospital stays and labs, so I’m looking forward to that.

Parenting with Cancer
How old were your kids when you were diagnosed?
I have the youngest, our baby girl who was 3 days old when I was diagnosed; our oldest boy, who is 8; and our youngest boy, who is 7.
Did you tell your children about the diagnosis?
Yes, we did. We involved the mother of our oldest when we told him (both are my stepsons), which made it much easier. He had experienced his grandma going through breast cancer just a few years prior, so he had an idea of what to expect.
He was emotional, but I smiled, made light of the situation and told him, ‘I’m superwoman and can get through anything.’
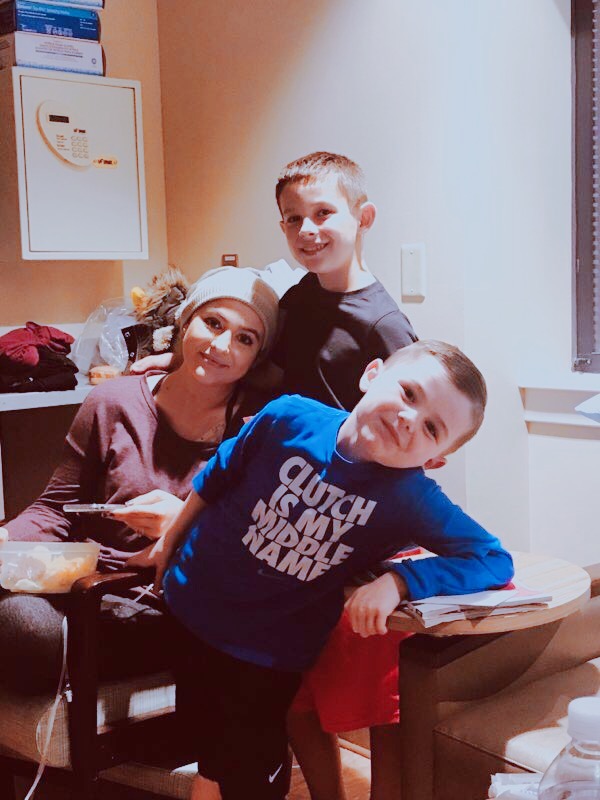
The conversation with our youngest son was very similar, but the relationship with his mom is not the greatest. We have full custody of him, so my husband and I explained everything to him one on one.
He was more confused, but again, I made it as light as possible and talked about how strong I am and assured him that I was going to give cancer the biggest fight possible and that it didn’t know who it was messing with.
We laughed and hugged, and then I went in my room and cried a little on my own, and that was that. He often asks how I got “my cancer,” and I explain that it wasn’t anything specific, just the something my body produced on its own. He’s still a little confused, but we are very open and honest without saying anything that would scare him.
How has it been raising a young child as a patient?
It’s been challenging, but I’m really not the one doing the majority of the “raising” right now, and that’s been the most difficult part of it because I’m a very hands-on parent and person with everything I do.
I can’t go to nearly as many school functions, baseball games, basketball games, play dates with other kids, plays they’re in, fun activities like going to the movies or to laser tag, birthday parties of other kids, doctor visits, etc.
My husband is the ultimate dad, and I’m so thankful for him and for my loving and caring mother, who has basically moved in with us during my treatments and for about a week following.
I have been blessed with awesome, awesome people in my life, with whom I trust getting my day-to-day tasks done while I cannot.
What are extra considerations when you have to parent while undergoing treatment?
Allowing help from others is okay to do. All the help I can get. Like I said, my husband and my mother — and also my mother-in-law and father-in-law — have been so key in making our lives as stress free as it can be during this time. I am so appreciative for each and every one of them.
Also, it’s been difficult to accept, but I’m going to have to miss out on things involving the kids. It’s been tough having to miss things and not being as involved as I’d like to be and once was, but it’s all temporary. I am missing out now so that I can have so much more time with them later.
»MORE: Parents describe how they handled cancer with their kids
Any advice for how to ask for that help?
Swallow your pride. Tell people that you’re not too proud to admit you need help running your household.
People, family, friends, strangers even — not weird strangers, but classmate’s parents whom you hadn’t met until now — want to help you. You just have to be open to it.
Thankfully my mom is a retired teacher, so we have lots of help there. She has really been a godsend. But I’ve also been okay with asking my friends to watch the baby while I go get my labs done twice a week.
Or if Zack and I need a date night, or whatever the case may be. Remember, just because you have cancer, it does not mean that you should let it define who you are or what you do.
Make the most of the time you have and enjoy it to the fullest. I can truly look back on my spring/summer and say I had a great time, in spite of what I went through.

Inspired by Keyla's story?
Share your story, too!
Primary Mediastinal B-Cell Lymphoma Stories
Arielle R., Primary Mediastinal (PMBCL)
1st Symptoms: Swollen neck lymph nodes, fever, appetite loss, weight loss, fatigue, night sweats, coughing, itchy skin, trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Keyla S., Primary Mediastinal (PMBCL), Stage 1
1st Symptoms: Bad cough, slight trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Donna S., Primary Mediastinal (PMBCL), Stage 1-2
1st Symptoms: Visible lump in center of throat, itchy legs, trouble swallowing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Patrick M., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Bump pushing up into sternum
Treatment: 6 cycles of DA-EPOCH-R (dose-adjusted) chemotherapy at 100+ hours each
Crystal Z., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Chest pain
Treatment: 6 cycles of R-CHOP chemotherapy
Stephanie C., Primary Mediastinal (PMBCL), Stage 3
1st Symptoms: Visible swelling around the jaw and neck area, major fatigue
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
Mags B., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment:(1st Line) R-CHOP chemotherapy, 6 cycles
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatment: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy









