Donna’s Stage 1-2 PMBCL Non-Hodgkin’s Lymphoma Story
Donna was diagnosed with stage 1 to 2 primary mediastinal B-cell lymphoma, a subtype of non-Hodgkin’s lymphoma.
She describes undergoing 6 rounds of chemo, how she dealt with hair loss, parenting with cancer and advocating for herself as a patient. Thank you for sharing your story, Donna!

- Name: Donna S.
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Primary mediastinal B-cell lymphoma
- Stage 1-2
- 1st Symptoms:
- Visible lump in center of throat
- Itchy legs
- Occasional trouble swallowing
- Treatment:
- Chemotherapy: R-EPOCH (Dose-Adjusted)
- 6 cycles, each cycle = 3 weeks
- Diagnosis
- Chemotherapy and Side Effects
- Describe your chemotherapy regimen
- What was Week 1 of chemo like?
- How about Weeks 2 and 3?
- What were the side effects?
- Describe the side effect cycle
- Were you prepared for the side effects of treatment?
- What helped you the most in dealing with side effects?
- How did you deal with chemo?
- How was the port?
- What was the worst part of treatment?
- What got you through that worst part?
- How were the scans?
- Describe the waiting periods after tests and scans
- Losing Hair from Chemotherapy
- Support and Reflections
- What helped when you lost all your energy?
- What was the biggest surprise?
- How did you manage your thoughts and emotions?
- Giving yourself space
- What gave you the best mental and emotional relief?
- What do you wish you had known before you began chemo?
- Be your own advocate
- How important is it to have caregivers?
- Can you work during treatment?
- Advice for others going through what you went through
- Parenting with Cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Remember that no matter how bad things may seem at first, you really don’t know the outcome until you get there. Going through chemo to fight cancer was not nearly as bad as I made myself believe it would be. None of my original fears came true, and I have come out on the other side better than before.
Most importantly, no matter how bad this ordeal was in the midst of it, I understand why it happened. The person I am today as a result of this experience is the person I needed to be. For that, I am grateful.
Donna S.
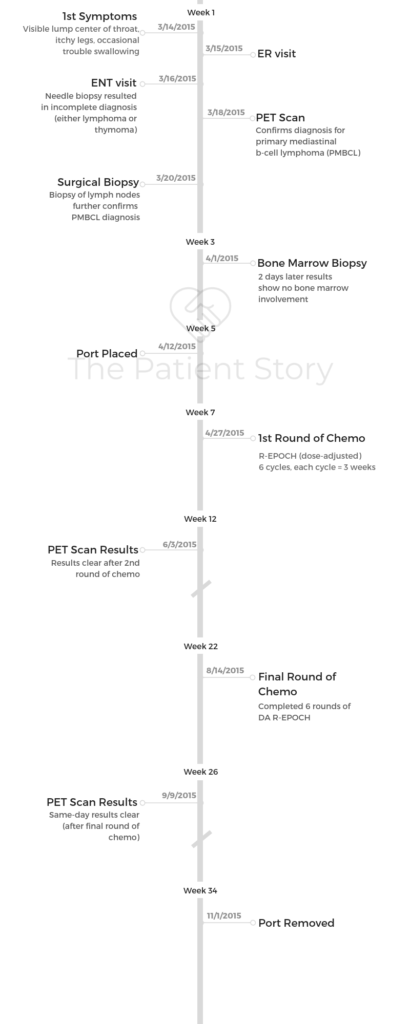
Diagnosis
How did you get diagnosed?
When I got out of the shower in the evening, I noticed a lump in my throat that I did not see the day before. I pushed on it, and it felt pretty hard, but it did not hurt.
My heart sank a bit because I instinctively felt that something was very wrong. My first thought was thyroid cancer. I didn’t know what it was, but I knew it was not good.
I went to the ER the next day in hopes of getting a quick answer, as well as a benign answer. They did an ultrasound and told me to see an ENT (Ear, Nose, Throat) specialist. My blood work came back normal except for slightly elevated LDH (in the 300s).
They told me that was nothing and not to worry. They did not give me any information about my lump, which I thought was odd.
When I got home, it felt like the longest night of my life waiting to see the ENT. I did not get much sleep that night. At that time, I had no other symptoms other than the lump.

As time went by after diagnosis, I started to feel a little out of breath or winded. Sometimes I had trouble breathing, and sometimes I felt a burning sensation in my chest. I am not sure if it was related or not, but I do recall trouble swallowing certain foods as well. However, this had been going on for 2 years prior to the lump.
I had a needle biopsy procedure done in the visible lymph node protruding just below my thyroid gland.
How did you choose hospitals?
Both hospitals were in the city (about an hour drive). However, one hospital had satellite offices near my home, where I could get my blood work without having to drive back to the city every couple days. It would have been very difficult in between my in-patient chemo treatments to drive that much.
Also, the hospital I chose had a free reiki service, which was really helpful during infusions. Lastly, they allowed my husband to stay in the room with me during each chemo infusion, which took 5 days.
What were your treatment options?
I had 3 choices:
- DA-R-EPOCH: Inpatient and the possibility to avoid radiation
- R-CHOP and radiation: One day of chemo instead of 5 days of inpatient, but radiation at the end would be necessary
- A research study that was similar to R-CHOP, also needing radiation.
I really didn’t want to do the inpatient chemo, but avoiding radiation was important to me. I did not want to do a research study when there was already an option available that provided a 92% cure rate.
It took me 5 weeks after my diagnosis to research all of my options, including natural options with no chemo, before making my decision. In the end, DA-R-EPOCH gave me the best chance of a cure while also avoiding radiation.
Chemotherapy and Side Effects
Describe your chemotherapy regimen
I had 6 rounds. Each round was every 3 weeks. I had 1 week in hospital and 2 weeks at home. The first week was the infusion. I did end up with side effects during the infusion, but once I got home from the hospital, the second week was the worst part of it.
The third week was easier, and I was almost normal after rounds 1 and 2, but I still suffered effects in the third week during rounds 3 through 6. The effects were less severe than Week 2, but still hard nonetheless.
- Treatment:
- Chemotherapy: R-EPOCH (Dose-Adjusted)
- 6 cycles, each cycle = 3 weeks
- Week 1: Continuous infusion through PICC line (arm) or port (chest) for 24 hours, lasting 5-6 days
- Week 2: Side effects tend to kick in, ranging from nausea to mouth sores
- Week 3: typically the healing week when blood cell counts recover
- Note: If your white blood cell count (WBC) doesn’t rebound back into the standard range, your next chemo cycle may be delayed.
What was Week 1 of chemo like?
There was a large fear of the unknown. My biggest concern at that time was not knowing what side effect was coming up next or when the side effects that came would go away (if ever). The worst part was waiting in the room for the chemo to arrive.
I remember wanting to run away, get on a plane and escape! Once the poison was hooked up, I remember thinking that there is no going back now. I named my chemo pole “the tower of terror.”
What helped during my first infusion (which is the most scary) were the nurses. They talked me through my fears and assured me that everything would be fine.
How about Weeks 2 and 3?
By the time I was ready to go in for my second week of chemo, I felt about 99% the same as before I even started. I remember thinking, “Chemo is almost easy!”
However, chemo has a cumulative effect, and by later rounds of chemo, I was not back to my normal self again before the next round. The later rounds are harder than the earlier ones, but there was a trade-off. The fear of the unknown was replaced by the more intense side effects.
What were the side effects?
- heartburn
- sore throat
- lightheadedness
- vision changes
- mood swings
- temporary neuropathy (improved after they lowered vincristine chemo drug dosage
- bone pain (Neulasta shot)
- nausea (by Day 3 of chemo)
- fatigue
- slow heart rate (occasional)
- low white blood cells/neutrophils
- runny nose
- puffy face/eyes (from the steroids)
- bladder pain (irritated by drugs)
- when hair fell out, scalp felt a little pain
Describe the side effect cycle
The side effects were predictable each cycle, with a little more intensity during the later rounds of chemo. I actually named the different phases because they were so reliable.
Phase 1 started the day after chemo. For me it was after my 5-day hospital stay. I named Phase 1 the “meat grinder” phase. It felt like I went through a meat grinder. Basically, everything hurt.
The second week after chemo, Phase 2 began. I called Phase 2 “the stratosphere.” This was when my hemoglobin would tank, and I would feel dizzy and weak as if I did not have enough oxygen. I was stubborn, though, and refused blood transfusions.
After that came Phase 3: “bio warfare.” That was when I became neutropenic and had no immune system, so contracting any germs would have been extremely dangerous. I would take Neulasta shots to increase my white cells.
Those shots lead me into my last phase: “snot city.” This was when my eyes and nose would drip for over a week due to my allergy to the shots.
The chemo cycle was as predictable as Old Faithful! Once in a while, I would get something new like a mouth sore, but for the most part, I could count on those 4 main events.
»MORE: Cancer patients share their treatment side effects
Were you prepared for the side effects of treatment?
I was not sure what to expect until the first round was over and I was beginning the second round. I felt more calm going into Round 2 because I knew what to expect, and my side effects were very predictable. Once I knew what to expect, I felt more prepared.
What helped you the most in dealing with side effects?
Summary:
- Anti-nausea: Ativan (through an IV)
- Bladder irritation: oxycodone
- Mouth sores: lidocaine, magic mouthwash, Colgate Orabase, canker sore patches, gargling baking soda and warm saltwater
- Neulasta bone pain: oxycodone

I was given some medication for discomfort. When my anti-nausea medication stopped working (usually by Day 3 of chemo), I was given Ativan through an IV. Ativan helped with the nausea, but it made me not remember anything after I received the dose.
It was fun watching videos that my husband taped of me talking to him and having no recollection of it!
My bladder was very irritated from the chemo drugs, so I was given oxycodone to help. I didn’t take much of this, only a couple while in the hospital and once after I got home.
For mouth sores, I tried everything from lidocaine to magic mouthwash. The only thing that helped was Colgate Orabase for canker sores. It helped me to eat. Gargling with baking soda and warm salt water expedited the healing process.
I did not opt for blood transfusions, even though my hemoglobin was very low. I waited out the discomfort (extreme weakness and fatigue), which usually lasted a few days.
I had bone pain from my Neulasta shot after the first round of chemo and needed to take an oxycodone for it. I did not try the Claritin, but I heard that helps prevent the bone pain. I did not experience bone pain with any of my subsequent shots. I rested most of the time, but on days that I felt good, I tried to be more active.
How did you deal with chemo?
Since each round of chemo was very similar, I kept a journal of my side effects. It explained the time point that they would show up and when they resolved.
It was great to refer back to the journal in my next round so that I could anticipate how long I will be dealing with a certain side effect. It gave me comfort because it reminded me that it would soon pass.
I kept my job since it was a work-from-home job. Working helped me maintain a sense of normalcy in my life. I brought my computer to the hospital, and it helped me pass the time.
I also had a coloring book. My husband stayed with me the entire time, which was also extremely helpful. I prefer to say, “We dealt with chemo.” Everyone should have at least one person to help them through this process. Having him there kept me calm and prevented the loneliness that would have made my thoughts wander down a destructive thought process.
»MORE: Patients talk about working during cancer treatment
How was the port?
Since I declined antivirals, antibiotics and anti-fungal medication, I opted for a port because there was a smaller risk of infection. Also, due to the countless amounts of blood work needed, it spared my veins and made access very easy. I have no regrets opting for the port.
What was the worst part of treatment?
Once I got a handle on the side effects and the fear of the unknown diminished, it soon became a fear of not surviving cancer or treatment failure.
Aside from the emotional aspect, the worst part was temporarily being physically unable to do the things I used to do. Whether it be eating (mouth sores), fatigue, dizziness or nausea, there was always a challenge.
I became too weak to stand in the shower, so I had to sit. I could not lift plates from the dishwasher into the cabinet because they were too heavy. It would take me several minutes to climb the steps.
Losing the ability to use your body in the way you were used to was the hardest, followed by the fear of not knowing when or if you will ever get back to normal again.
What got you through that worst part?
Talking to people who have been through the same chemo regimen saved me. Hearing everyone tell me that it is temporary and that I will get back to normal once chemo is done was really what got me through chemo.
Seeing people years past chemo living normal lives with no problems calmed my fears. It made me fight just a little harder and hang on just one more day when I wanted to quit.
How were the scans?
Scan day is the worst. You are filled with such anxiety wondering if the cancer is gone, if it came back or if it spread.
My first scan was after my second round of chemo. It was a miracle; the scan was clean, and there was no evidence of lymphoma! I was overwhelmed with joy and happiness, and then I thought “Wait, that was it?”
It was almost like beating cancer was too easy. I realized I was very fortunate to have a complete response that early on in treatment. It meant my prognosis was very good.
My next scan was after my last round of chemo, and believe it or not, I was terrified. However, that scan came back clean as well. So did the 6-month scan after that, the 1-year scan after that and final 2-year scan. All were equally hard in their own way.
Describe the waiting periods after tests and scans
My hospital tried to get the results in the same day, but the waiting period was extremely hard. At any moment, your life could go on happily, or it could turn upside down again at the drop of a hat.
Wondering which path your life was going to go was incredibly hard. Since your chances of relapse is next to nothing after 2 years, my 2-year scan left me with a very surprising side effect.
Once I got the clean scan, I felt fatigued, depressed and almost angry. It was almost as if I had been happily running on adrenaline during my 2 years post chemo and once I reached the 2-year mark and everything was likely to remain good, the adrenaline left my body and
I was feeling terrible. I couldn’t understand why I wasn’t over the moon upon hearing my results and good news. It took me a few days to snap out of it.
»MORE: Dealing with scanxiety and waiting for results
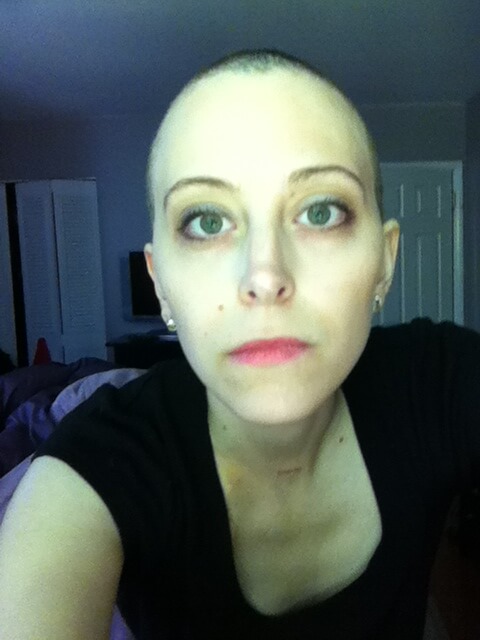
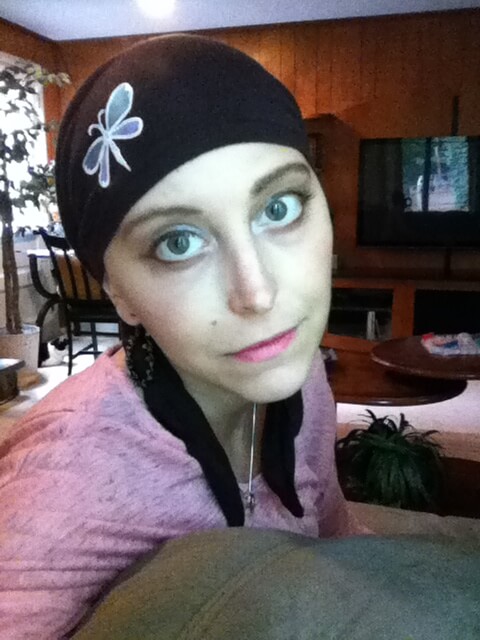
Losing Hair from Chemotherapy
Describe the hair loss
I had very long, beautiful, brown hair, and I was really upset about losing my hair at diagnosis. However, after my hair was gone, I was surprised that I did not wear my wig very much.
Though my wig was made from my own hair, it was more comfortable to wear little cotton hats instead. I never anticipated I would go without my wig, and I only wore it a handful of times after chemo was done.

Were you surprised by your reaction to losing hair?
Yes! When the time came, I had already been anticipating it. Right after my second round of chemo, I noticed my bangs coming out in clumps.
That was it. Without a second though, I went upstairs and just shaved my head. I felt like that was one thing I had control over: not watching my hair fall out piece by piece each day.
I didn’t realize how ready I was to lose my hair, but I did have a lot of time to prepare and get used to the idea. It was harder to lose my eyelashes and eyebrows. That was the difference between looking sick and not looking sick for me.
What helped with the hair loss?
I loved wearing little cotton hats. They kept my head warm and were very comfortable. I even slept in them. I had a wig made of my own hair, but I only wore it a few times after I was done chemo.
You had a wig made from your own hair
I did a search online for places that make wigs out of your own hair. I provided my hair and a donor who had similar hair as me to create my wig. We had to send it through the mail, which made me nervous. However, when my wig arrived, I instantly burst into tears.
I can’t explain the feeling I had when I saw my hair come back to me in a form that I could use.
I hugged it for about 5 minutes!
Support and Reflections
What helped when you lost all your energy?
Resting and knowing it will pass soon.
What was the biggest surprise?
Everything was a surprise because I was drifting into a land of unknown.
The biggest surprise was my clean scan after 2 rounds. I did not expect that at all. Another surprise was actually seeing the good in my situation and appreciating the experience. It took until after my last round of chemo to almost be grateful for what had happened to me.
I became a new person, a stronger person, a person who was able to live in the moment more, enjoy life more, be full of gratitude and self respect. I love the new me!
How did you manage your thoughts and emotions?
I kept a journal. At first I was not going to document the experience because I wanted it over, and I never wanted to think about it again. However, when the time came, I picked up my pen and realized I had a lot to say.
Referring back to my chemo journal, I see there are more F-bombs than punctuation. When I got diagnosed, I think I went through all the stages of grief. I was in disbelief, and then I was angry. I even threw a wooden desk chair out of my second story office window.
One thing I still find interesting is that I had a greater fear of living with pain and disabilities from chemo than I did of dying. At times I thought I would rather just die than suffer the rest of my life.

Keeping a journal was a great way to vent my emotions without subjecting anyone to my anger or whatever I happened to be feeling that day. I am pretty sure I felt every emotion possible at some point during the journey.
Anger, fear, sadness, strength, weakness, loss, triumph, pain, loneliness, boredom, stress, fatigue, sociable, antisocial, happy, stir-crazy, peaceful, annoyed, determined, defeated, pathetic, delighted and close to God.
I documented symptoms and vented about how I felt. It was very therapeutic. I also limited who I spoke to. I could not handle speaking to every single one of my friends and family members about the same thing over and over again. I kept about 5 people super close, and they provided updates to the others for me.
Giving yourself space
I didn’t take any calls or answer too many texts. This was because my emotions were all over the place. I did not want to subject people to whatever might come out of my mouth, nor did I want to go over everything with everyone.
I preferred not talking to anyone about it, and I really did not like when someone asked me, ‘How are you?’
I know they meant well, but to me, it was opening a can of worms. It was overwhelming to rehash everything over and over.
My mom, my husband and 2 of my friends were the only people I cared to speak to. My mom provided updates to my dad, sister and anyone else who was checking in. I appreciated the outpouring of love in the form of cards, calls, texts, flowers, gifts, etc. I never felt so loved in my life. I was just physically and mentally unable to speak to everyone once treatment started.
What gave you the best mental and emotional relief?

The best relief for my fears and emotions was talking to people who had gone through it, gotten to the other side and are able to enjoy life with no issues.
I found the primary mediastinal large B-cell lymphoma board on Facebook and met many people who shared their experiences with me. I would post a question and have 80 answers within the hour. I really owe my life to them because if I hadn’t heard so many success stories, I probably would not have done the chemo.
When I finally accepted my situation and completed my research, I was ready to start chemo. I felt true acceptance when I chose my chemo regimen and my path forward was finally clear. My friends on the group also helped me during chemo by assuring me that the side effects would go away. They helped me decide between a port or a PICC line.
They shared my [sorrow], tears, triumphs, clean scans and every stage start to finish. They understood me and could actually provide helpful advice that calmed and comforted me. My family took care of me physically, and my friends on the Facebook page took care of me emotionally.
What do you wish you had known before you began chemo?
That none of my worst fears would come true (regarding side effects, etc.). That I would love the person I became after chemo was finished, that it changed my life for the better, that I am stronger than I thought, that there are people who love me more than I thought, and that there is a plan and a reason for everything, even if it doesn’t make sense at the time.

Be your own advocate
I needed a plan, and I needed to be aligned with my treatment. Therefore, I took 5 weeks after my diagnosis before starting chemo to educate myself 24/7 on all of my options. I was able to customize a routine with the help of many different cancer experts, facilities, survivors, books and videos.
I combined a range of holistic and functional medicine with the chemo to stay as healthy as possible. The combination of 2 very different medical approaches, I believe, allowed me to get through a very dangerous and difficult chemo regimen (600 hours of chemo infusion) with little to no complications.
The chemo that I was on can cause your body to go into neutropenia and contract infections, which would delay chemo or even could cause death. It also would require blood transfusions regularly.
However, I was able to avoid transfusions, infections and many other side effects, such as infertility, as a result of blending many wonderful resources with my chemo treatment.
Both chemo and holistic body support in conjunction were necessary and essential to my success. I feel back to my normal self most days, and some days even better than before. Recovery was a sawtooth pattern always trending up. I am 3 years out now and have no real complaints.
» MORE: How to Be Your Own Advocate
How important is it to have caregivers?
It is absolutely essential.
Can you work during treatment?
The only reason I was able to work was because I had a work-from-home position with my company. It became more difficult to work during later rounds of chemo, but I still did not miss a day. I would not recommend working outside of the house.
There are too many germs, and the immune system is nonexistent at times. I also was unable to operate a car during treatment and worked from my bed.
»MORE: Working during cancer treatment
Advice for others going through what you went through
A quote from my chemo journal:
Remember that no matter how bad things may seem at first, you really don’t know the outcome until you get there. Going through chemo to fight cancer was not nearly as bad as I made myself believe it would be. None of my original fears came true, and I have come out on the other side better than before.
Most importantly, no matter how bad this ordeal was in the midst of it, I understand why it happened. The person I am today as a result of this experience is the person I needed to be. For that, I am grateful.
Parenting with Cancer
How old was your kid when you were diagnosed?
My son was 4 years old and turned 5 during treatment.
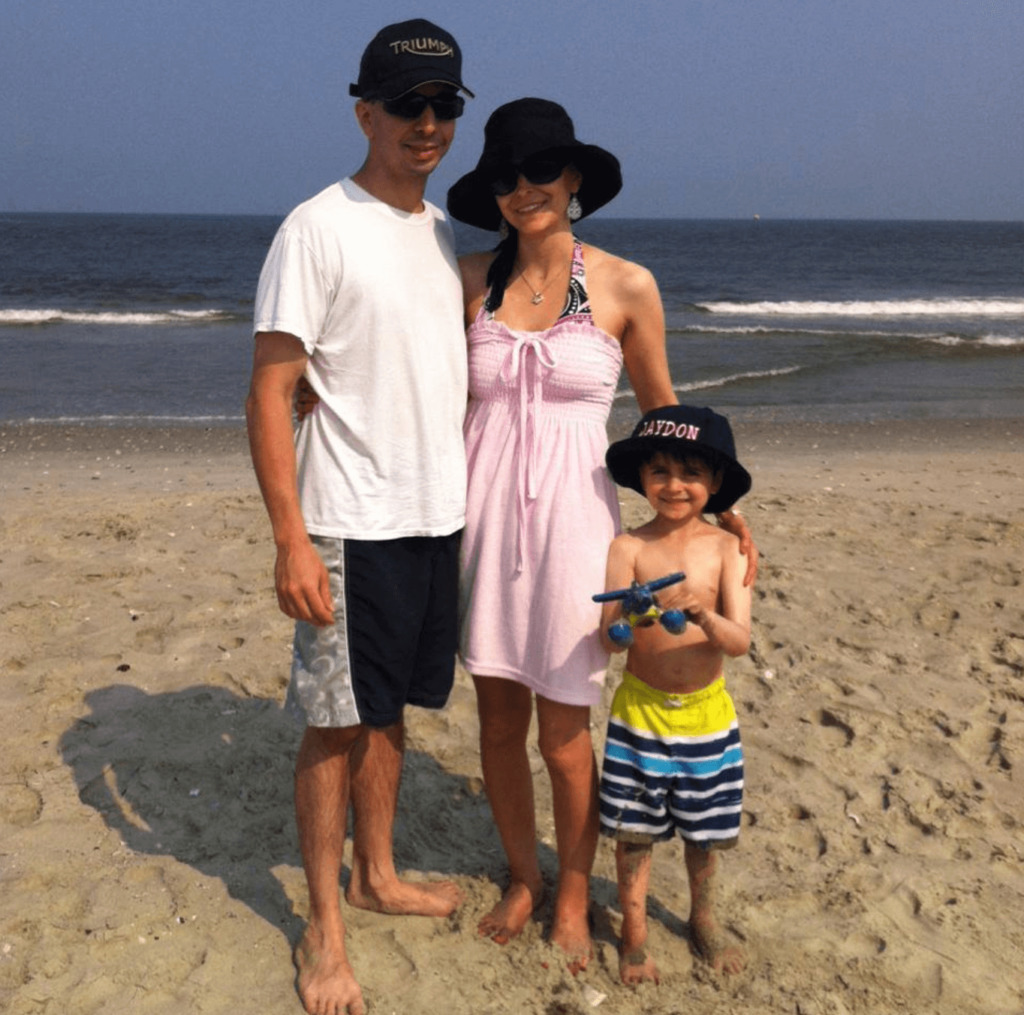
Did you tell your child about the diagnosis?
He clearly knew I was sick but did not know what cancer was or that it could kill you. He did become fluent in oncology terms, such as chemo, neutropenia and PET/CAT scans. He even asked, “Is there a Dog Scan?” A few years after, he learned a little more about what cancer is and how serious it can be.
How has it been raising a young child as a patient?
My mom stayed with my son while my husband and I were in the hospital for my chemo treatments. At home, my husband held down the fort, and I did what I could.
We tried our best to make things as normal as possible for our son. Though visiting me in the hospital on his birthday was not exactly normal, we did have a cake for him, and my mom and grandmom came to celebrate as well.
What are extra considerations when you have to parent while undergoing treatment?
Trying to keep germs away. It is important to stay isolated if your child comes home with a cold. We were lucky that my treatments were over the summer, so we could minimize contact with people as needed. It would be more difficult with school-aged children.
»MORE: Parents describe how they handled cancer with their kids
Any advice for how to ask for help?
I would not hesitate to ask for help. You are fighting for your life, and that is all you should be focusing on. If friends or family live nearby, I would suggest taking any help you can get.
Before I started chemo, we had all the days in the calendar marked for both sides of the family, so everyone knew in advance what to do and when. I would suggest planning ahead because things get tough during treatment, so it is good to be prepared ahead of time.
Take care of yourself first
It is inevitable that you will feel guilty for not being able to spend as much time with your children during chemo as you would like, however try not to beat yourself up too much.
Your job is to beat cancer so you can stay alive for your children.
Chemo goes very fast, even though it seems slow while you are in the middle of it. Take care of yourself before anything else. It doesn’t feel natural, but it is what you must do.
Update: Congrats, Donna!
This beautiful wife and mom has since become a mom of 3! Donna and husband, Jason, welcomed twins Alexander and Matteo. Big brother Jaydon has had a great time with his new baby brothers.

Want some cool children’s books? You can see Donna’s own creations on Amazon. Check them out here!
Inspired by Donna's story?
Share your story, too!
Primary Mediastinal B-Cell Lymphoma Stories
Arielle R., Primary Mediastinal (PMBCL)
1st Symptoms: Swollen neck lymph nodes, fever, appetite loss, weight loss, fatigue, night sweats, coughing, itchy skin, trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Keyla S., Primary Mediastinal (PMBCL), Stage 1
1st Symptoms: Bad cough, slight trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Donna S., Primary Mediastinal (PMBCL), Stage 1-2
1st Symptoms: Visible lump in center of throat, itchy legs, trouble swallowing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Patrick M., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Bump pushing up into sternum
Treatment: 6 cycles of DA-EPOCH-R (dose-adjusted) chemotherapy at 100+ hours each
Crystal Z., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Chest pain
Treatment: 6 cycles of R-CHOP chemotherapy
Stephanie C., Primary Mediastinal (PMBCL), Stage 3
1st Symptoms: Visible swelling around the jaw and neck area, major fatigue
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
Mags B., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment:(1st Line) R-CHOP chemotherapy, 6 cycles
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatment: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy










