Crystal’s Stage 2 PMBCL Non-Hodgkin’s Lymphoma Story
Crystal was diagnosed with stage 2 primary mediastinal B-cell lymphoma (PMBCL), a non-Hodgkin’s lymphoma subtype, and underwent R-CHOP chemo.
Explore her story below, where she also highlights the issues of hair loss, cancer’s impact on her relationships, and how it inspired her to become a nurse. Thank you for sharing your story and for your work, Crystal!

- Name: Crystal Z.
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Primary mediastinal B-cell lymphoma
- Staging: 2
- 1st Symptoms: Chest pain
- Treatment:
- Chemotherapy
- 6 cycles of R-CHOP (Rituxan, Cytoxan, doxorubicin, vincristine & prednisone)
- Infusions for 5 days every 3 weeks
- 6 cycles of R-CHOP (Rituxan, Cytoxan, doxorubicin, vincristine & prednisone)
- Chemotherapy
I don’t see my life as a regular timeline now. I see it as before, during and after cancer. For me, I have a different outlook.
I try not to take anything for granted because I know life can change in an instant.
Crystal Z.
- PMBCL Diagnosis
- Chemotherapy Treatment
- Reflections
- Cancer inspired you to be a nurse!
- Who were your primary caregivers?
- How did cancer affect your relationship with your husband?
- What are some ways family and friends can help out?
- What was hardest for you mentally and emotionally?
- Cancer and fertility
- What’s your “new normal”?
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
PMBCL Diagnosis
What were your first symptoms?
I had started having chest pain. It was early in the fall of the year before my diagnosis the next January. I went to get it checked out, and they told me I had a pulled muscle.
I still had the chest pain, so I went back in December. They said I had walking pneumonia. They didn’t really think anything of it. In January, it hurt to eat or drink anything, so I went to the ER. That’s when they found a mass.
How did you get the diagnosis?
They did an X-ray. They didn’t see anything. The doctor had a funny feeling, so he did a chest CT, and that’s when he saw it. Then he transferred me to a hospital about 30 minutes away, which is the hospital I work at now.
I got the results of the CT scan, but they didn’t know it was cancer yet. They just knew it was a mass, so they transferred me. I didn’t get the biopsy until the next Monday because I went on a Friday. I got the results that Thursday.

We did a full body CT after the results came back and then did a bone marrow biopsy to make sure it hadn’t spread.
»MORE: Read different experiences of a cancer diagnosis and treatment
Describe fine needle aspiration (biopsy)
I had a needle biopsy for the mass and a bone marrow biopsy to make sure it hadn’t spread to my bones. My mass was in the sac around my heart, but it hadn’t infiltrated my heart yet, so for the needle biopsyI was laying on a table.
I was awake for it, but I had some medication to make me loopy. I wasn’t supposed to remember the biopsy, but I did. You get a scan, they mark you, and then they put you through the CT scan again just to make sure they’ve got you marked right. Then they take a huge needle, stick it in, and pull some of the mass out into a syringe.
Describe the bone marrow biopsy
For the bone marrow, you lay on your stomach. It’s done through the back of your hip. They drill into your bone and take a sample of bone marrow.
The needle biopsy isn’t painful, but it’s scary because you can hear the popping sound. The bone marrow biopsy hurt afterwards. Sitting down hurt for about 2 weeks.
How did you process the PMBCL diagnosis?
I didn’t think cancer until they told me. They took me for a bone scan, and I was sitting down waiting. They took my glasses off, so I couldn’t see anything because I’m almost legally blind. I was sitting there for transport waiting for someone to take me back to the room, and I hear someone say, “I chose you for this.” I didn’t see anyone.
The next day, they diagnosed with me cancer, so I just felt like that was something I heard from God because I never saw anyone.
I was a teacher at that point, so my first response was, ‘When am I going to be able to go back to work?’
I’m known for that. The doctor said I wasn’t going back to work, and I was like, ‘Oh, yes, I am.’
I think I was in denial a little bit. I understood what he was saying, but I thought I would be able to get treatment and just get right back to work. I understood that I had to do chemo, but I was determined to get back to work.

Chemotherapy Treatment
What was your treatment plan?
Because of the location of my cancer, they could never do surgery. The plan was to do chemo, and if chemo didn’t work, we would move on to radiation and go from there.
I started treatment quickly. I had the port put in, and about a week later or so, I started chemo. I had to go to the cancer center and get set up as a patient.
They give you a lot of information about your chemo, the diet you need to follow and the potential side effects.
They said, “We don’t know how this will affect your ability to have kids. You can try to save eggs, but it can take months. You’re taking a large risk to wait.” There was no time, so we went ahead and started chemo.
What was your chemo regimen?
I had R-CHOP. It’s Rituxan, Cytoxan, doxorubicin, vincristine and prednisone. I had 6 chemo cycles. I went 5 days in a row, and I would do that every 21 days. I got Rituxan on a Monday. That took about 8.5 hours. Normally, it doesn’t take that long, but I had a bad reaction, so they had to do my infusion very slowly.
I went home with a chemo pump at the end of day one. Tuesday through Thursday, I would go back to get a 30-minute infusion. Each of those days, I’d go home with a pump again. I was constantly getting infused. Friday, I had to get the last infusion, and that lasted about 5 hours.
Then I was finally unhooked. A day after I finished a round, I had to get the Neulasta shot, which boosts your white blood cell count.
Then I had 2 weeks off in between each cycle, but 2 days during that time, I had to go get blood work. I was always at the cancer center.

What side effects did you experience from chemo?
Summary: Fatigue, weakness, bone pain (from Neulasta shot), taste changes, hair loss
Fatigue was the very first one. That showed up the day after I finished the first chemo. I would fall asleep randomly anywhere. I carried a Pillow Pet everywhere. I was very weak. I don’t know if that was from the cancer itself or the chemo, but I was always weak.
The week after chemo, I would have to get help walking. Neulasta hurts every bone in your body, so I was extra weak from that. My mom and husband would have to help me to the bathroom. I had a dog who would help me. She would stand beside me as well.
My taste buds changed immediately. My mouth got really hot. My hair started falling out about 2 weeks in. As soon as it started falling out, we shaved it.
The worst was probably the fatigue. I was 23, an athlete, a coach and used to being very independent. Needing somebody’s help to do pretty much everything was really hard. The hair loss was bad, too. Then I got used to it, but that one kind of messed me up.
»MORE: Cancer patients share their treatment side effects

Losing hair from chemotherapy
They told me it was going to be about 2 or 3 weeks. I knew it was coming. I was trying to decide what I wanted to do. I wanted to be in control of one thing, so I decided to shave it off.
I took a shower, and I noticed a lot of it was coming out. My mom dried my hair for me and told me not to look. She pulled out what was falling, and she got a trash can full.
The next day, my best friend shaved my head at her house. My husband shaved his head with me.
A mutual friend came to my head shave, and she told me about an idea she had when she had cancer. She told me about a hat and scarf party.
It’s like a baby shower but for your bald head. Everyone brought hats and scarves and saw your bald head for the first time.
We took that idea and did a crazy hat and scarf party. Everyone still brought hats and scarves for me, but they came wearing crazy hats and scarves. It really made me feel at ease and more comfortable.
»MORE: Dealing with hair loss during cancer treatment
Describe the scans through treatment
I had scans after my third treatment and another at the end. My mass was 13 cm. After the third treatment, it had shrunk to 5cm. My doctor saw an immediate impact before the scan because my heart rate was better.
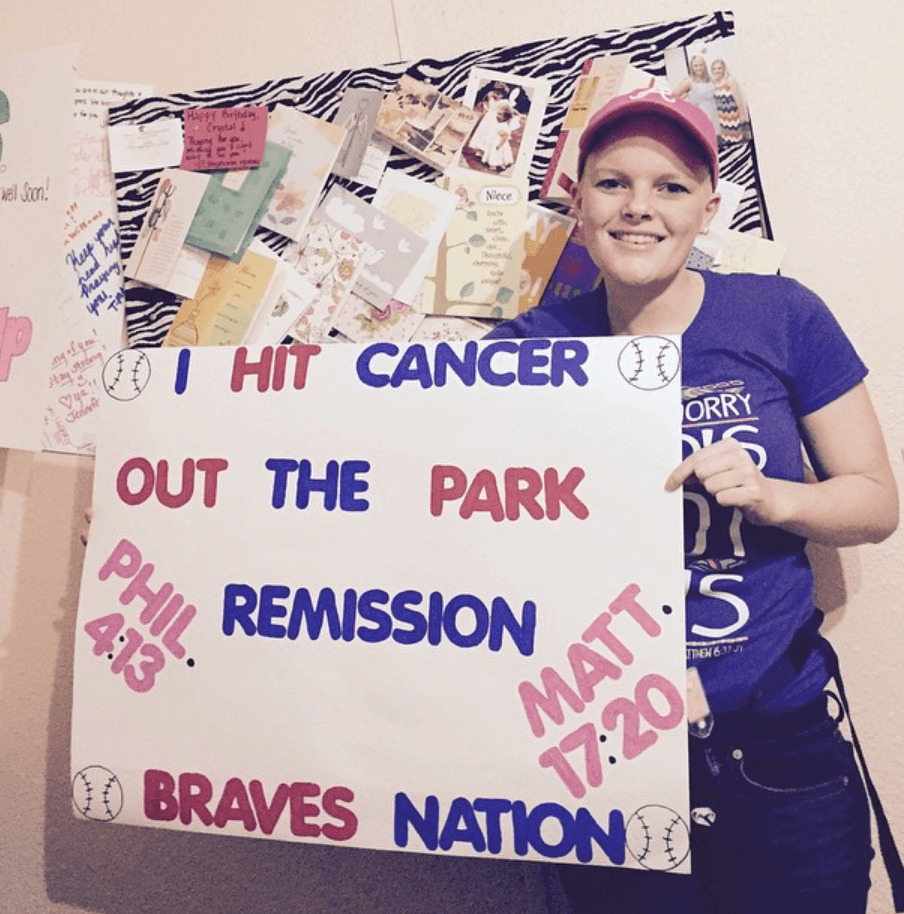
It shrank it to 1 cm by the end of chemo, and it wasn’t cancerous anymore. It’s still there, but now I just get scans to make sure it’s still not cancerous.
I’m technically in remission, but I’m not considered cancer-free. I’m almost at year 5, so I get scans every 2 years. I switched careers, and I work in the oncology field now.
I actually work in the same hospital as my doctor, so she felt comfortable pushing it back to scans once every 2 years. If I ever want a scan earlier than that, I can always ask.
»MORE: Dealing with scanxiety and waiting for results
Reflections
Cancer inspired you to be a nurse!
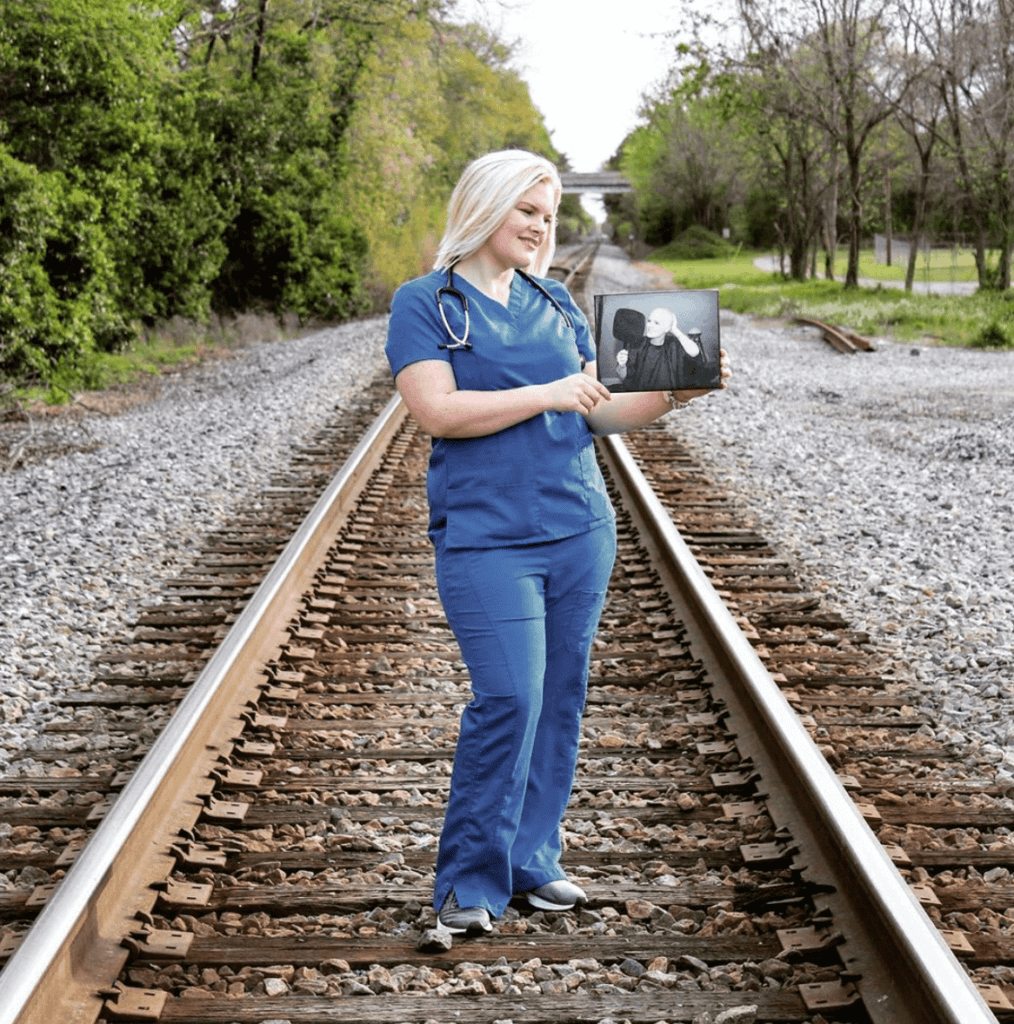
I left teaching and went to school to be a nurse. I had a bachelor’s degree already, so it only took me a year and a half to finish school.
I want to work at an inpatient center administering chemo. Right now, I work on an oncology floor. We do chemo, surgery, and we have palliative care.
After the chemo, I went back to teaching. I loved what I did, but I wanted to do something with my experience. I knew I had been through cancer for a reason. I tried to do some motivational speaking, but I could never get into that realm.
I went to a follow-up appointment, and there was a man who was in a wheelchair at the front door. His wife dropped him off at the door, and I said, “Don’t worry, I’ll go ahead and take him up. You can just meet us in the chemo room.” I took him up, and I waited on my appointment.
I had to come back the next day. When my nurses came to get me, they said, “Hey that man is looking for you. He’s asking for the nurse that brought him up yesterday.” They had to tell him I wasn’t a nurse.
I was joking with my oncologist about it, and she said, “You would make a great nurse.” Eventually, I thought about it more and more, and I went to school.
Who were your primary caregivers?
My husband, who was my boyfriend at the time, and I had only been dating for a month and a half. As soon as I was diagnosed, he and my mom moved in with me.
My husband works nights and my mom works days, so they rotated shifts. They would switch off taking me to chemo and just taking care of me.

How did cancer affect your relationship with your husband?
We went to high school together and had been friends for about 10 years. It was definitely amazing that he stuck around, but it’s very weird when you’ve been dating someone a month and a half, and they have to hold you up to go to the bathroom all of the sudden.
Whenever I was in the hospital, I overheard him talking to my mom, and he said he was going to propose to me.
I made him promise he wouldn’t propose until I got my hair back because I didn’t want people to think he was just doing it because I had cancer. Obviously, my hair came back, and we got married.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
What are some ways family and friends can help out?
For me, my coworkers and students would write me cards, and that meant so much. I was actually on the local news because they set up fundraisers for me, so I had strangers sending me cards from all over.
I had a board I would put them on, and I looked at it when I was feeling upset. People forget how simple and thoughtful a card is.

You can bring food. It’s so easy to bring a meal by, but it’s so helpful. Always bring food for the caregiver, too, because that’s one thing you can take off of them.
It sounds silly, but just bring a movie over and spend time with them. You can’t really get out much when you’re going through treatment, so having company over when you feel up for it is so nice.
What was hardest for you mentally and emotionally?
There were times that my counts were so low that I wasn’t allowed to leave the house. I was home, and I felt comfortable there, but when I was stuck there it kinda felt like a prison.
Being isolated and not being able to do things takes a toll on you emotionally. That was hard.
Cancer and fertility
We still don’t know if I can have kids. We’ve been trying, but we don’t know. I did some lab work. My ovaries are functioning, but they don’t know if I’ll be able to get pregnant. I’ll go see a fertility specialist soon.
It’s hard. Sometimes I try not to think about it. I feel like I want to get further in my career before we have kids anyway, so it’s okay.
Other times, it’s rough because people around me are getting pregnant, and I feel like, ‘Why can’t that be me?’ It’s rough, so I just try not to think about it.
»MORE: Fertility preservation and cancer treatment
What’s your “new normal”?
I don’t see my life as a regular timeline now. I see it as before, during and after cancer. For me, I have a different outlook. I try not to take anything for granted because I know life can change in an instant.
I always try to do things that make me happy, whether that’s sitting at home watching a movie with my dogs or going out with my camera. I just try to do things I enjoy.
Advice for someone who has just been diagnosed
It’s okay to feel every feeling. Don’t feel bad about feeling something. Make sure you talk to someone. Just because someone is there for you doesn’t mean they know what’s going on in your head.
You need to speak up if you need to talk about something.
Don’t expect people to read your mind or push you to talk. Learn to talk about those feelings.

Primary Mediastinal B-Cell Lymphoma (PMBCL) Stories
Arielle R., Primary Mediastinal (PMBCL)
1st Symptoms: Swollen neck lymph nodes, fever, appetite loss, weight loss, fatigue, night sweats, coughing, itchy skin, trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Keyla S., Primary Mediastinal (PMBCL), Stage 1
1st Symptoms: Bad cough, slight trouble breathing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Donna S., Primary Mediastinal (PMBCL), Stage 1-2
1st Symptoms: Visible lump in center of throat, itchy legs, trouble swallowing
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Patrick M., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Bump pushing up into sternum
Treatment: 6 cycles of DA-EPOCH-R (dose-adjusted) chemotherapy at 100+ hours each
Crystal Z., Primary Mediastinal (PMBCL), Stage 2
1st Symptoms: Chest pain
Treatment: 6 cycles of R-CHOP chemotherapy
Stephanie C., Primary Mediastinal (PMBCL), Stage 3
1st Symptoms: Visible swelling around the jaw and neck area, major fatigue
Treatment: R-EPOCH (dose-adjusted) chemotherapy, 6 cycles
Sonia S., Primary Mediastinal (PMBCL), Relapse, CAR T-Cell Therapy
1st Symptoms: Chest pain, superior vena cava syndrome (SVCS); persistent, dry coughs, headaches
Treatment: (1st Line) R-CHOP chemotherapy, 6 cycles (2nd Line) R-ICE Chemotherapy (3rd Line) CAR T-cell therapy
Mags B., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment:(1st Line) R-CHOP chemotherapy, 6 cycles
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
1st Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatment: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough, low-grade fever, night sweats
Treatment: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy









