Kimberly’s MZL Non-Hodgkin’s Lymphoma Story
Kimberly shares her marginal zone lymphoma diagnosis, a subtype of non-Hodgkin’s lymphoma, and undergoing chemotherapy into remission.
She also shares how she navigated life after a cancer diagnosis, including the support that helped her most and dealing with survivorship. Kimberly shares the best part of her story in depth in our last segment of her story: her successful fertility journey!
Thank you, Kimberly, for sharing your story so openly.

- Name: Kimberly O.
- Diagnosis (DX)
- Marginal zone lymphoma (MZL)
- Non-Hodgkin’s lymphoma subtype
- Early stage
- Age at DX: 35 years old
- 1st Symptoms
- None obvious, routine blood test during physical showed abnormal results
- Later, longer nosebleeds
- Treatment
- Chemotherapy
- Rituximab & bendamustine
- 2 days every month for 6 months
- IV infusions
- Chemotherapy
- Fertility Preservation
- Egg harvesting
- Egg retrieval
- Embryo freezing
- Implantation
- Videos: Kimberly's Story
- Introduction
- First Symptoms & Tests
- Marginal Zone Lymphoma Diagnosis
- You got the diagnosis (bone marrow biopsy results) a week later
- How did you break the news to loved ones?
- How did you decide to get a second opinion?
- When did you get the full second opinion?
- How did the marginal zone lymphoma impact your overall treatment plan?
- Describe the PET scan with contrast dye
- What were the PET scan results?
- Chemotherapy & Side Effects
- How did you get the chemo infusions?
- Describe the chemotherapy regimen (rituximab, bendamustine)
- How were the chemotherapy infusion sessions?
- What were the side effects of the rituximab and bendamustine?
- You were able to keep working throughout chemotherapy
- What was the scan and blood work schedule through treatment?
- How were the midway PET scan results?
- Any thoughts about getting chemo infusions through the IV?
- Describe how you processed hearing about remission
- What’s the follow-up schedule?
- Navigating Life After Diagnosis
- Fertility Journey
- Whose idea it was to go see a fertility doctor, and why that was so important to you?
- What were the first decisions you had to make?
- What was the egg harvesting and retrieval schedule?
- Describe the egg harvesting process
- Describe the egg retrieval process
- Any guidance on dealing with so many needles?
- Describe the paperwork that has to be done before IVF
- How did you pay for the procedure?
- The surprise of frozen egg storage fees
- What were the different costs of the egg retrieval and storage?
- How many eggs were you able to freeze?
- Transitioning from eggs to embryos
- Mosaic embryos becoming “normal”
- Describe the implantation day
- Did you feel anything during the implantation?
- Describe what you saw on the monitor/screen
- When did you learn the results of the procedure?
- COVID-19 visitor restrictions
- Any plans for your 3 other frozen embryos?
- Any guidance for others on the fertility journey?
- Marginal Zone Lymphoma Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Videos: Kimberly’s Story
How I Got Diagnosed
Chemotherapy & Navigating Life After Cancer Diagnosis
Kimberly’s Full Fertility Journey
Introduction
I’m 32 weeks pregnant as of right now. Due date is April 25th, so it’s getting closer and closer. First kid, a boy.
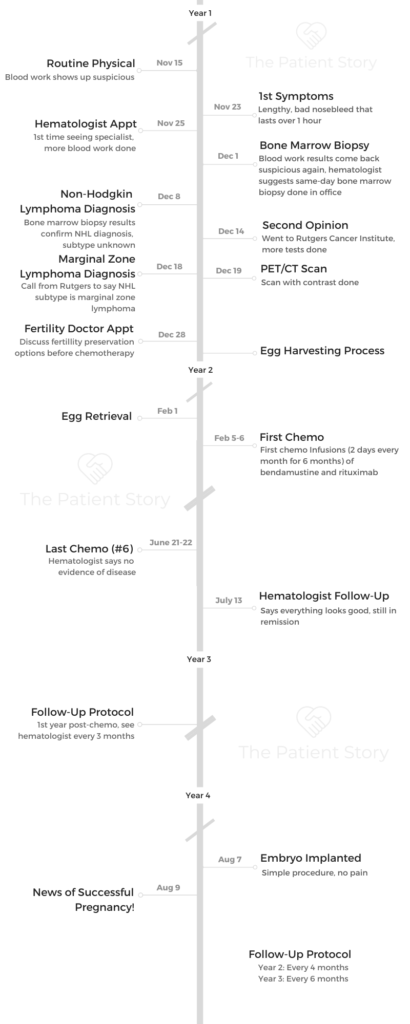
Other than that, I come from a great family. Filipino by heritage. By my last name, my husband is Irish. That’s pretty much it.
I’m a pretty easy-going person. We come from huge families. I’m a big soccer fan. We are season ticket holders of New York Red Bulls. We watch them, and then we watch the USL, which is the minor league team over at Montclair State.
We’re huge fans, and now we’re also fans of Sky Blue FC, which also play at the same arena. We’re just big sports fans!
First Symptoms & Tests
What were the first symptoms?
Nothing, really, and that was the weird part. I had my yearly physical, and my doctor was asking me, “Oh, is everything all right? Anything weird?”
Everything was fine. She drew the blood like she normally does. She gave me my flu shot like she normally does.
Then a week or 2 later, I had a really bad nosebleed. I used to get them a lot when I was a kid. I thought I grew out of it because I didn’t really have them anymore, but then this one was pretty bad.
It lasted about 45 minutes to an hour. It was bad. That was before I got the word from my doctor to see a hematologist. I had my blood results, but I didn’t really know how to read them.
Describe the visit to the hematologist
When you look up whom to see, there’s also ‘slash oncologist’ next to their name. I was just like, ‘This isn’t good.’
I went to see the hematologist, who was not far from our house. He just did the same thing. He goes, “The blood results do look a little weird. I want to dig a little deeper, so let’s just order more blood tests.” I’m like, “All right, fine.”
Came back probably a week after that. He said that it still looked weird, and he didn’t like the way it looked. I was like, “This is getting better and better.”
Then he said pretty much that he wants to order a bone marrow biopsy. You hear it, and you automatically think of cancer. That’s what I thought.
You had the bone marrow biopsy on the spot
It was the same day as my hematologist appointment. I came in that morning, and then he goes, “If you have time today, I can check my schedule, and we can get it done today.”
I’m like, “Oh, okay. I might as well.”
I worked a half hour away from the office, so I didn’t want to go to the office, go back to the doctor, go back to the office again. I was just like, “Yes, I’ll just hang out and get it done.”
My husband, he was working about an hour away south at the time. I called him up and he booked it an hour north to the office.

Describe the bone marrow biopsy
It was weird. I was awake for the whole thing, which I wasn’t expecting. To be honest, I don’t know what I was expecting. All I knew was that it was invasive. Kind of invasive, you could say.
They laid me on my stomach, and they numbed my hip bone from the back. They numbed the skin first, numbed the bone and then they numbed the inside of the bone.
Then they extracted the marrow from my hip bone. It was just a weird sensation. All I felt was tapping, and I knew things were moving. I just felt pressure and tapping. My husband, all the while, was watching this whole thing next to me.
When we were done, they just let me lie down on my back so the pressure would stop the bleeding on my hip. When the doctor left, my husband and I were left in the room.
I was like, “Was it gross?” I go, “Did it look gross?” He goes, “Yes, it was pretty gross. All I saw was just him screwing something and digging and the extraction.”
How bad was the pain?
There was some pain, but once I did say there was pain, it went away right away. My doctor, he was even asking during that time. He goes, “Okay, now I’m taking the marrow sample. Let me know how it feels.” I was like, “It just feels weird. There’s nothing to describe it other than weird.”
Marginal Zone Lymphoma Diagnosis
You got the diagnosis (bone marrow biopsy results) a week later
We made the appointment for us to come back. Not only was it me and my husband, it was my parents, my mother-in-law and my aunt, who is a retired nurse in Jersey City.
She was familiar with the cancer, too, because my father-in-law passed away from cancer. The 6 of us were in this room with my hematologist and his nurse giving us the news that I had cancer.
The night before, my husband and I prepped ourselves for the worst-case scenario. When he gave us the news that I had cancer, that it would take about 6 months of chemo, and that a normal life is possible after that, we were pretty much okay.
Not everyone else in the room was ready, but we had prepared ourselves for the worst. Then when it wasn’t the worst, we were actually relieved.
Even though it was cancer and it sucked, it wasn’t the worst-case scenario, which is good.
We knew it was non-Hodgkin’s lymphoma from the start. I think my hematologist thought it was one type, but then when the second opinion came back, they really found out it was marginal zone lymphoma.
How did you break the news to loved ones?
We just basically told people it was non-Hodgkin’s lymphoma. We just didn’t really know what type yet. We told my family first because they were further. I couldn’t get to them fast enough. It was easier to call them and tell them on the phone.
That was tough. When it came to my husband’s side of the family, my aunt who was there, she was the one on the horn basically telling everybody, which is fine. I didn’t really want to be the bearer of bad news at that time either.
It was helpful because then I didn’t have to repeat myself thousands of times and say it over and over again, because you already knew what’s happening. It’s just a matter of fact — the more you say it, the more real it is. But it’s real already.
»MORE: Breaking the news of a diagnosis to loved ones
How did you decide to get a second opinion?
My hematologist recommended that we get a second opinion. He recommended either Memorial Sloan Kettering or Rutgers Cancer Institute. Both were fine, so we didn’t really have a preference.
I asked my primary doctor her opinion on it, and she said Rutgers would probably be the best bet. Even though Sloan Kettering is cancer-focused, so is Rutgers Institute just because they just have this huge building and everything’s taken care of right then and there.
We ended up going to Rutgers, and that pretty much took all day. Thankfully, the only thing I had to go through were more blood tests. That was fine. Other than that, it was just a consultation with their doctor at the time with their oncologist.
When did you get the full second opinion?
It was either a week or less than a week. I remember getting a call from my hematologist. I was out the door heading to work, and then he called me with the official subtype.
I was half paying attention until he told me, “Okay, what are you going to tell your husband that I told you?” I was like, “Oh.” I was like, “Let me head back into the house, and let me write this down.”

How did the marginal zone lymphoma impact your overall treatment plan?
It wasn’t any different as to what treatment was going to be. That didn’t change. The only thing that changed was just the name that they called it.
I remember when we first talked about the results, the full name of it was something with an abbreviation of LPL (lymphoplasmacytic lymphoma). Then we got the official marginal zone lymphoma subtype diagnosis.
He said treatment was pretty much going to be the same: 6 months of chemo, once a month for 6 months.
The only thing that was really different was just the classification of it, so nothing really on my end needed to be done. Just how they classified it is all.
Describe the PET scan with contrast dye
The only scan I had was my PET scan. You had to drink the stuff beforehand and sit still. I was just like, “Sitting still is not great with me,” especially when I know I have to sit still. That was the only thing that I had to go through.
I did get the contrast dye. The first scan was with the contrast. An old coworker of mine said she went through this PET scan also for a different reason. She saw the contrast that I had to drink, and she’s like, “If you could drink it cold, drink it cold. It’ll go down easier.”
I saw on the label that I wasn’t allowed to drink it cold, so I was like, “I’m just going to have to tough it out,” which I did. Thankfully, I only had to drink 1 and not 2 that the doctor’s office gave me. That was good.
Just sitting still for the whole thing was tougher. When I know I have to sit still, it’s not that great. Of course, everything starts to itch. You’re trying to think of other things, but then you want to wiggle your toe or something like that or raise your eyebrow, and you know you’re not allowed to.
Other than that, you think it’s longer than it’s supposed to be, but it’s really faster than you think it is. It just feels super long. I didn’t know what to expect from that because I’d never had a PET scan before.
What were the PET scan results?
When my doctor showed me the results, he was just like, “Yes, it’s just looking for hot spots in your body.” I was just like, “Oh, okay.” He went through the results with me, and he went pretty much from my head to my feet. He goes, “Yes, that’s your brain. That’ll show up. That’s your heart. Of course, that’ll show up.”
He said, “We’re looking for things that are out of the ordinary. Your major organs, they’re normal. They’re supposed to show up.”
They caught it so early that it didn’t really show anywhere. It just showed up in my blood tests. We were really thankful for that.
When we asked what stage I was in, he said, “Well, there really isn’t one where you’re at. You’re practically at zero, so we caught it. You’re one of the rare ones. Marginal zone lymphoma is rare to begin with, considering it affects elderly men more than anybody.”
Chemotherapy & Side Effects
How did you get the chemo infusions?
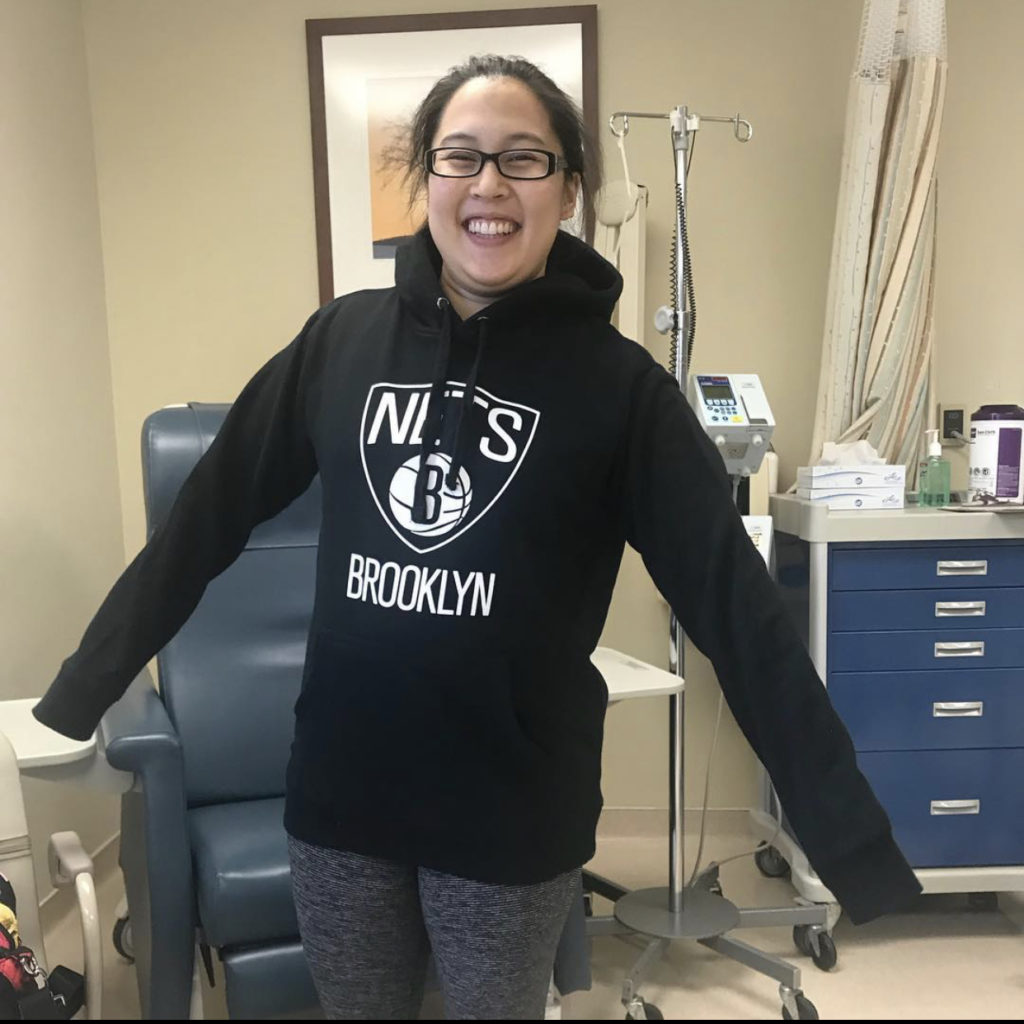
It was all IV. I was really hoping it would be all IV just because I was going in once a month for 2 days. I was really hoping that I wouldn’t have a port, and thankfully it was all IV.
Granted, later, towards the end, it started to get difficult for them to find a vein, which started to suck more and more because they just had to poke more and more.

Describe the chemotherapy regimen (rituximab, bendamustine)
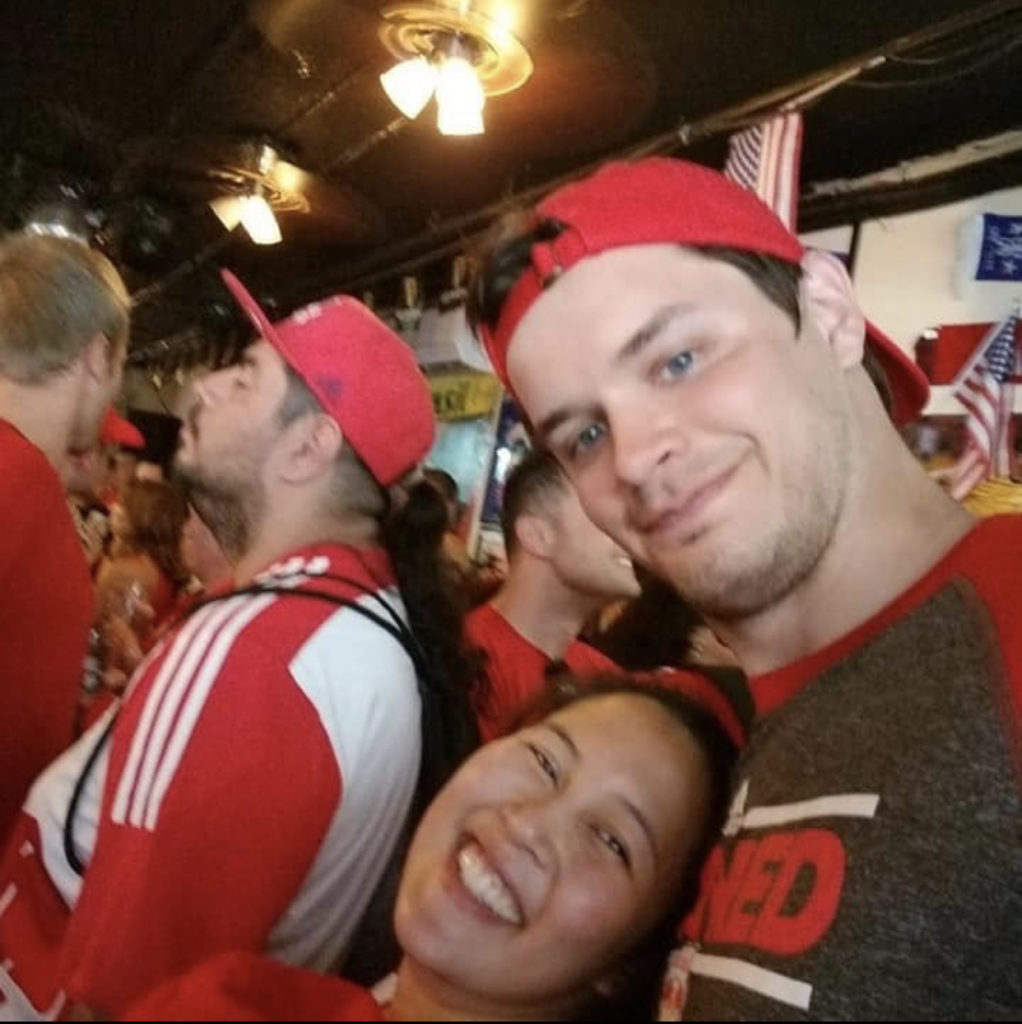
The first treatment was in late February, early March. That’s a picture of my first treatment. We came home that day, and I just took a picture of my ID bracelet that I had treatment done in my hand because that was the first one, so the first day. That was a longer day, so I was pretty much in the infusion room all day.
Little did I know, or maybe I just didn’t hear it from my doctor, that treatment was 2 days every month, the second day being shorter than the first. My husband had the great idea of [switching] it and making the longer day the second day so that he could take the day off from work and be with me all day.
Then the first day, I would just have either my dad or someone from our family just sit with me for an hour. The first day, the short day, was about an hour or 2, and then the long day was all day, about 8 hours.
How were the chemotherapy infusion sessions?
The first, the short day of chemo, it was fine. I sat in the chair, and they hooked me up. There was a portable TV. Each chair had a portable TV so you were able to watch TV. You were able to bring your headphones, just listen to music, do whatever.
For the most part, whoever was with me just chatted throughout treatment to make time go a little faster, because every time, it was always someone different. Whether it’d be my dad, my mother-in-law, a cousin or even my husband at some points, we just chatted away.
The second day of chemo, which was the longer day, was not so much tougher, just longer.
Before they started the infusion, they gave me Benadryl, which always makes me sleepy. Once Benadryl kicked in, I was either ready to pass out or passed out already and only woken up by the blood pressure cuff taking a reading every 30 minutes or so.
Other than that, if I wasn’t sleeping, I was watching TV or whatever was downloaded onto my laptop. This picture was taken right when they unhooked me from everything.
I was ready to go home, and I think it was snowing that day. We looked out the window of this infusion center in Berkeley Heights, so it’s kind of up in the mountains. We were just like, “Oh, I hope we can get home!”
What were the side effects of the rituximab and bendamustine?
I don’t think I had many. All I do remember is one weekend. I forget which session number it was, but it seemed that after every long day session, I was starving. Even though they served me lunch during the middle of the day, I didn’t really eat during treatment.
When I got out of treatment, I was starving. We would always go somewhere to hit up some fast food for me to just get something in my stomach because I was really hungry.
I was fine the day of treatment — the weekend of, because we always planned it out to be a Thursday, Friday treatment. Always on the weekend, I was hungry, and also I wasn’t hungry. It was just annoying because I’d want something, but I didn’t know what I wanted.
Water was just not good enough, and nothing in the kitchen was good enough. I do remember one weekend where I just wanted ice cream, some dairy, and my husband had a family party to go to. I couldn’t go because I just had a treatment, so he went and represented for us.
My parents were away that weekend, so no one was in the house with me. I just couldn’t figure out what to eat, so I ended up making myself pancakes with whipped cream on it. For some reason, it just hit the spot, and I was content for a good few hours until I got hungry again. I made enough for myself that it lasted throughout the day!
I had no nausea, thankfully. No nausea. I was just very tired the weekend after infusions. I just spent my Saturday watching TV and falling asleep, watching TV, and then the same thing on Sunday and would go back into work Monday.
You were able to keep working throughout chemotherapy
Yes, I got really lucky. My doctor just said to keep a normal schedule as possible. If I feel good, then do it. He said because my routine was basically going to the gym three times a week and going to work five days a week and last I had chemo which was, I was off Thursday, Friday and going to work Monday, Tuesday, and Wednesday.
My oncologist definitely encouraged me to be as active as I could be. I would go to the gym Tuesdays and Thursdays. Obviously, when I had treatment, I would just go Tuesdays.
Thursdays and Saturdays, I would just hang out at home, and everyone would just be checking in on me and seeing how I was. I got lucky. I was very lucky.
What was the scan and blood work schedule through treatment?
There was one scan midway through treatment, I remember. Before every treatment, I would get blood work done, or at least before I saw my doctor.
A week after treatment, I would get blood work done just to see where all the levels were. The one level that my doctor kept looking at was my IgM, because apparently when that first started, that was abnormally high.
Then as treatment went on, it started to get lower and lower and lower, even to the point where it was really low. That was our indicator whether chemo was working or not, and it was.
How were the midway PET scan results?
From what I saw, there was nothing that was jumping out. When he went through it with me, he goes, “It’s working. What we’re doing is working, because nothing’s really jumping out. We’re just going to keep doing what we’re doing until we get to the end, and then we’ll just run another blood panel on you and see where everything is.”
Everything was good at the end!
Any thoughts about getting chemo infusions through the IV?
In hindsight, a port probably would have helped me even if it was only once a month because getting blood work done now is a task-and-a-half.
In this picture, that’s my left arm that I’m getting infused in. The only vein that they can find now is my right arm, and it’s in one spot.
With me being pregnant now, blood work is a pretty constant thing. Thankfully, there’s enough time in-between that they can get the same vein all the time. In that aspect, I guess I’m lucky, but yes, we had to keep switching arms.
At one point, on my shorter chemo days, we would go through my hand just because it was easier, and my longer days would be in my arm.
Towards the end, the maybe last 3 sessions of chemo, they had to use a vein finder, which was almost like an infrared overhead projector, to find a vein. It was pretty cool, but it sucked they had to use it, but they did find a vein using that.
All the nurses were really patient with me towards the end of treatment, because it was getting very difficult. I remember chemo just ended, and they were having trouble finding a vein.
Now I just have to have a disclaimer to whoever the technician is, “I had chemo done 2 years ago. If you can find it in this arm, great. If not, it’s usually the other arm that’ll work.”
Usually, when I tell them that and they see how young I am, they’re just like, “All right, we’ll be a little bit more careful not to poke around as much.”
Water definitely helps. If not water, Gatorade, as long as they’re not checking your sugar.
Describe how you processed hearing about remission
That was my last chemo session. Oddly enough, it was the day before my cousin’s birthday. I remember seeing my doctor a week after that.
He said, “Your blood work is looking great.” I knew it was my last session, but I didn’t get to ring a bell or anything like that, which is fine because it was almost like a factory that I was in, but with people in and out all the time.
My next appointment with my doctor for the follow-up, he goes, “Your blood work looks amazing. There’s no sign of anything that was there before. Your blood levels are normal. I can’t officially put you in remission because we’d have to do another bone marrow biopsy. I don’t want to put you through that again, so officially, unofficially, you’re in remission.”
That was good. We are really happy about that. Other than that, unfortunately, I didn’t get to ring a bell, but that was fine. Just taking a picture with that, the culmination of everything was the best.

What’s the follow-up schedule?
It’s every 6 months, so I next see him in June. I just get blood work done the week that I see him. Usually, it gets done a couple of days before I see him.
Then by the time I see him, he has the results of my blood work, and we just talk about it. That’s pretty much it. We just touch base personally, and I let him know what’s happening in my life. He asks how my family’s doing, how my husband’s doing. That’s pretty much it. Then he’s like, “All right, see you in 6 months.”
Navigating Life After Diagnosis
How did you mentally get through treatment?
It was just basically a countdown for treatment. The first infusion came, and it’s just like, “Okay, only 5 more, and then only 4 more, only 3 more.”
When the last one happened, it was just like, “This is great. I don’t have to be here anymore. I don’t want to be here anymore.”
It was really nice knowing that there was only X amount of treatment time left. When my doctor said, “Okay, we’re done. You don’t have to go through chemo anymore. Everything worked.” It’s just like, “Really? Are you sure?”
Because you don’t hear that story all the time. You hear, ‘Oh, we have to check you again,’ and, ‘Oh, it’s back,’ but it wasn’t like that for me.
So I was just like, ‘Okay, okay, we’re taking this as a win. A huge win.’
What support was most helpful from your loved ones?
It wasn’t so much advice that my family was giving me. It was more words of encouragement. They would check in on me every now and again.
Even when I wasn’t having treatment, they would just check in on me, send me a text, “Hey, how you doing?” Or, “How you feeling?”
Other than that, it was fine. Or they’d just be like, “Are you out of work? I just want to check in on you and see if you’re all right.”
There’d be times where I’d just be like, “Oh, yes, I just got out of the gym.” They were surprised. They’re like, “You’re going through treatment, you’re going through chemo and you still have time to go to the gym?”
I’m like, “Yes, I feel fine.” I was like, “Other than the 2 days of chemo on that weekend, I feel like crap sometimes, but other than that, I feel good.” They’re like, “You’re amazing.”
How has survivorship been?
We know I’m not going to be 100% cured of this thing. It’s always going to be inside of me, and it’s just a matter of when it decides to wake up again.
I remember telling my niece and nephew when I was in remission, and they asked, “What does that mean?” I was like, “Well, it means that the cancer is still inside. It’s just sleeping.” Then they’re like, “But you’re all right though, right?” I was like, “Yes, I’m good.” They’re like, “Okay.”
I described it to my husband, because he wasn’t at home at the time when I told them. He goes, “Yes, that’s a good way to put it. We know it’s there. We know it’s always going to be there. It’s just a matter of when it decides to do its thing again, if it’ll ever do its thing again.”
Yes, I’m cancer-free, but at the same time, I’m like, “Is it ever going to come back? Will it come back?” We don’t dwell on it. Everything’s good, check-ups are good, and blood work is good. Just keep chugging on.
That’s all you can do. You can’t be afraid of what might happen later down the line, because it’ll just drag you down.

Fertility Journey
Whose idea it was to go see a fertility doctor, and why that was so important to you?
When I first got diagnosed, I didn’t even think about us having a family. It was my aunt who was in the room with us and asked, “Is this going to impact her fertility?” We had just gotten married in March. It was December!
My doctor was able to refer us to a couple of fertility doctors, just to be safe, to go through fertility preservation.
»MORE: Fertility preservation and cancer treatment
What were the first decisions you had to make?
We went to our fertility doctor at RMA of New Jersey in Morristown. She was able to present us with either freezing eggs or freezing embryos.
At that point, the chances of thawing an embryo was a lot better than thawing a frozen egg going through IVF. At least at this point with that frozen embryo already, we are already halfway there. All it needed was just to be thawed out and then implanted back in me.
What was the egg harvesting and retrieval schedule?
That was done. Everything was done really fast. I got my diagnosis in December, egg retrieval was done in February, and a couple of weeks later was my first chemo treatment.
Everything had to be done fast just because we wanted chemo to start right away and not prolong it any longer.
With the whole fertility medicine, the shots and the monitoring, chemo was pushed back probably about a month, which wasn’t so bad. It didn’t affect me. They obviously had to ask permission from my doctor, but that didn’t really impact anything.
Describe the egg harvesting process
It was a lot of blood work for me and my husband, but mostly for me. It was probably just a couple of vials from him, but for me, it was different.
I had to go through morning monitoring, which is going to the clinic every other day so they could check my hormone levels. They would draw blood, just a small amount, but enough for it to be annoying, to check my hormone levels and to see where everything was and to see what stage I was at.
That was pretty much it. Then I let them know when I got my period and then would basically start over from there, see where everything was. It was about a month of monitoring.
Describe the egg retrieval process
When it was time for getting ready for egg retrieval, there were shots and making sure the timing was right every night. It was about 2 or 3 different types of shots in one night.
Then at one point, my husband was helping me because my hands would start to get sweaty, and the meds wouldn’t work. Then ice packs were involved because the abdomen area started to swell after the shots. It was a lot. The shots for me were more stressful than the chemo itself.
»MORE: Read a patient’s detailed egg retrieval journal
Any guidance on dealing with so many needles?
I am not a fan of needles either. I still can’t watch blood work being done on me. When the needle enters the skin, I can’t watch, but seeing them change up the tubes, I can watch fine. It’s just the whole initial entry that I do not like.
Knowing that I had to do that myself, it was basically taking a couple of deep breaths before, reminding myself, “You’re doing this for yourself, for your future family. It’s good that you’re doing this.”
It also helped that my husband would say, “Thank you.” He was like, “This is for us.”
Describe the paperwork that has to be done before IVF
That was like an eye-opener for us because the paperwork asked, “Okay, what happens if…” There were a lot of “if” questions.
If one dies or if both of you die or if you guys are no longer married, if you guys divorce, what happens? If you become pregnant and you guys separate, what happens? There were just so many different scenarios that it was just like, how do you even come up with these things, seriously?
We have both been brought up Catholic, but the paperwork options that they were giving us weren’t the ones that we wanted. The only options were either donate to science or discard. Really? No, I don’t want to either. That’s terrible.
My husband was not very happy after we got through that whole contract consent form thing and at one point he goes, “I just don’t want to answer these questions anymore. Just put the same answer there for everything.”
I said okay and I was checking them off . Then I said, “Okay, now you need to sign.” He’s like, “Seriously?” I’m like, “Yes, we both need to sign this.”
How did you pay for the procedure?
We actually took out my 401(k) for it because we knew we wanted a family eventually. We just didn’t know when it was going to happen. At this point, I had a lot of money saved in my 401([k) from my previous job. We took that out.
We basically paid for fertility treatments for it, as well as the other bills that needed to be paid along with it. That was a huge chunk of change. That was a big check to write!
The surprise of frozen egg storage fees
We were fine once everything was said and done and they’re frozen. Everything was good, and then we hit the bills for the yearly storage fee, and we’re like, “What?”
I thought it was okay. I thought we didn’t have to pay a storage fee. They’re just like, “No, you just pay for the year,” and it’s just like, “Oh, okay,” so we paid the storage fee for the year.
That’s when the discussion happened of, instead of them giving us a bill for next year, if we wanted to implant, just try one and see if it’s going to work or not.
What happened was Christmastime rolls around, and at that point, we’re like, “We’re going to get a bill in January for the embryos that are frozen. Do you think it’s time to start having a family?”
He goes, “Yes, let’s try.” I was like, “Okay, I guess I’ll just call our fertility doctor in December and see if we can get an appointment for January.” That was how our conversation went.

What were the different costs of the egg retrieval and storage?
The whole process itself, because it wasn’t covered under insurance, was about $7,000. Storage for the year was about $1,000 to $1,500 a year.
Then we went through the implant. Thankfully, it wasn’t a lot because insurance did cover some of that part. It was a lot less than what we were thinking of. That was more considered as IVF at that point. Everything else beforehand wasn’t covered under insurance.
How many eggs were you able to freeze?
While I was taking the hormone shots, they would do the ultrasound and the blood work every other day in the morning. They were looking at 12. They would see on the ultrasound 12 eggs. I’m like, “Okay, that’s a good chance. That’s a good shot.”
The egg retrieval came, and the nurse was like, “We were able to get 7.” I’m just like, “7? There were 12 the other day. I don’t know what’s going on.” They were like, “Yes, the other ones weren’t viable,” and we’re like, “Okay.”
Transitioning from eggs to embryos
They combined my eggs and his sperm together, and then it came down to 4. We were just like, “All right, we could do with 4.” They’re like, “Not just regular 4.” We’re like, “What do you mean?”
They’re said 2 of the embryos were normal and 2 were what they call mosaic. It either means that they’re missing something or there’s an addition of something. They were not sure.
Because the part that they took for genetic testing didn’t really come back definitive, so we ended up having 2 normal embryos and 2 mosaic embryos.
Mosaic embryos becoming “normal”
That was 2 years ago when this happened. When I called in January about getting one implanted, one of the normal ones, because they wouldn’t let you do the mosaic ones first. You have to go through the normal ones first.
They said that because it’s been 2 years since everything has happened, the people who have used their mosaic embryos are just as viable as the normal ones. They do end up becoming normal. Basically, they end up being a normal embryo at some point during the pregnancy.
Granted, a lot of invasive testing would need to be done, like an amniocentesis, which I found out has a 5% chance of a miscarriage. I’m just like, “Oh, boy.”
We used one normal embryo, we have another normal embryo that’s frozen, and we have 2 mosaic ones. We had to go through serious counseling before using the mosaic ones.
Now, 2 years later, I think they just treat it like a normal embryo, because the research has been found that they do end up becoming normal and that whatever was missing or added ends up working out somehow on its own.
Describe the implantation day
August 7th was when the implant took place. It was weird because it happened on a Friday, and then that following day, one of our cousins was getting married, and so everything was off-limits.
Then I went in on Sunday morning to get a pregnancy test done, and a couple of hours later they called to say that we were pregnant!
I don’t think I had to fast. I remember it happened in the morning, and about a half-hour before I went in, I had to drink about 16 ounces of fluid. It could be water, juice, coffee. They didn’t really care as long as it was 16 ounces of something.
I didn’t know why, but then they said it was so they could see better because my bladder would be full, and it would expand everything in my uterus.
The best way to describe it was almost just like a yearly exam, almost, where there’s just a lot more people in the room other than you and your doctor. There’s a person with the ultrasound, making sure the doctor’s in the right place in your uterus, implanting it in the spot where it’s supposed to be.
That was pretty much it. It was just like a tiny, tiny little thing. It was pretty cool to see. You could just see everything happening on a monitor next to you, and that was pretty much it.
Did you feel anything during the implantation?
No, it was like a normal GYN exam, but actually more comfortable in a way because they’re not comfortable normally. I didn’t feel a prick. I barely felt anything at all. I just saw it happening, and I was just like, “All right. That’s it? Okay!”
Describe what you saw on the monitor/screen
I saw my uterus, where they wanted to implant the embryo, and then you would see a little catheter come into the screen. That’s where the embryo was.
She would just lay it down or inject it into my uterine wall, and that was pretty much it. It was so simple and yet so complicated at the same time.

When did you learn the results of the procedure?
2 days later. We were nervous because we didn’t know if we would get the news right away or if we would wait for it.
We didn’t know if we’d hang around the office until they let us know or they’d call us to let us know. The nurse was just like, “Okay, we’ll call you in a few hours when it’s done.”
We finally got the call, and we just told our immediate family and our closest friends, and then we didn’t really tell everyone in the world.
We didn’t put it up on our social media until I was after the 3-month mark, but hearing his heartbeat was amazing for the first time. Seeing him grow throughout the ultrasound, it was awesome.
COVID-19 visitor restrictions
The only thing that sucks is that this happened during COVID, so my husband couldn’t see much of it. He was only able to come for one appointment, and that was the first-trimester screening.
He was able to see this picture live, so that was good, but everything else after that, he wasn’t allowed to come anymore.
I’d bring home the sonogram (ultrasound pictures), and I tell him what the doctor says, and he’s just as happy and excited about it as everyone else is in the family.
Any plans for your 3 other frozen embryos?
By the time I give birth to this first baby, I’ll be 39. Time was not on my side, definitely. We’ll have this baby boy, and then probably a year after he turns 1, we’ll assess the situation and try to use the other ones.
As long as I’m healthy and I’m able to carry, we’re going to do our best to carry all 4 of them if we can.

Any guidance for others on the fertility journey?
It’s rough. It’s not easy, but it’s still worth it in the end. The reward is definitely higher than the risk, and it’s so much better.
Knowing that you can have a family, even after cancer, it’s the light at the end of the tunnel.

Inspired by Kimberly's story?
Share your story, too!
Marginal Zone Lymphoma Stories
The Importance of Positive Role Models
The example that Nick's father set for him as he was growing up taught him how to prioritize and advocate for his health.
Nick M., Nodal Marginal Zone Lymphoma
1st Symptoms: Daily hives, GI issues, weight loss, heart issues, night sweats
Treatment: Rituxan (rituximab) and high-dose steroids
Kimberly O., Marginal Zone Lymphoma
1st Symptoms: None at first, routine blood work showed suspicious results, bad nosebleed
Treatment: Chemotherapy (bendamustine & rituximab)
Rachel P., Marginal Zone Lymphoma, Gastric MALT
1st Symptoms: Fatigue, bloating, stomach pain
Treatment: Chemotherapy, targeted therapy, surgery


