Sheryl’s Stage 4 MCL Non-Hodgkin’s Lymphoma Story
Sheryl shares how she got diagnosed with stage 4 mantle cell lymphoma at 51 years old. She underwent multiple cycles of chemo to get into remission. Sheryl also talks about what support she needed the most, scanxiety and survivorship.

- Name: Sheryl B.
- Diagnosis:
- Mantle cell lymphoma
- Subtype of non-Hodgkin’s lymphoma
- Stage 4
- Age at DX: 51
- 1st Symptoms:
- Symptoms appeared over a period of more than a decade
- Skin reactions to temperature changes
- White blood cell count (WBC) started to climb every year
- Retinal hemorrhage
- Unexplained fatigue
- Abdomen “rock hard” (spleen enlarged 3x original size)
- Treatment:
- Chemotherapy
- Cycles A & B, alternating
- Cycle A: Hyper-CVAD
- Cyclophosphamide (Cytoxan)
- Vincristine sulfate
- Doxorubicin hydrochloride (Adriamycin)
- Dexamethasone
- Cycle B: High-dose cytarabine and methotrexate
- 6 cycles (3 A, 3 B)
- Rituxan infusion before each chemo infusion
- Rituxan done outpatient in clinic, chemo infusions done inpatient in hospital
- Chemotherapy
- Mantle Cell Lymphoma 1st Symptoms
- Mantle Cell Lymphoma Diagnosis
- Chemotherapy and Side Effects
- Did you get a port, PICC line or go through IV for infusions?
- Describe the mini-surgery for the PICC line and caring for it
- What was your MCL chemotherapy regimen?
- Rituxan was given outpatient starting Cycle 2
- Describe the inpatient cycle schedules
- Describe the hair loss
- What were the other chemo side effects?
- Any guidance on what helped with the side effects?
- Tips on how to get through repeated hospital stays
- In Remission
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

You are an individual, a bio-individual. No one else is like you. You will respond to the treatment in the way that you will respond, not the next person, not the person with the horror story. You can’t go down that road.
At the same time, be educated and knowledgeable about what you’re about to go through. Make your own decisions. If something doesn’t feel right, get another opinion. If it still doesn’t feel right, maybe you don’t do it.
Sheryl B.

Mantle Cell Lymphoma 1st Symptoms
First, how are you doing now?
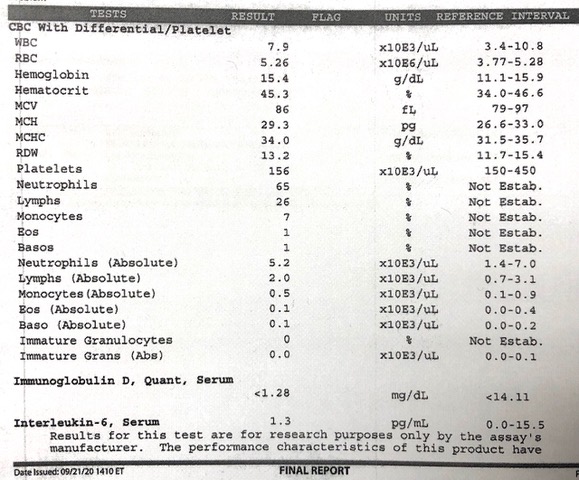
I’m doing pretty great. I’ve been in remission from mantle cell lymphoma since May 28, 2015. I just had some basic blood work done a few weeks ago, and it’s perfect.
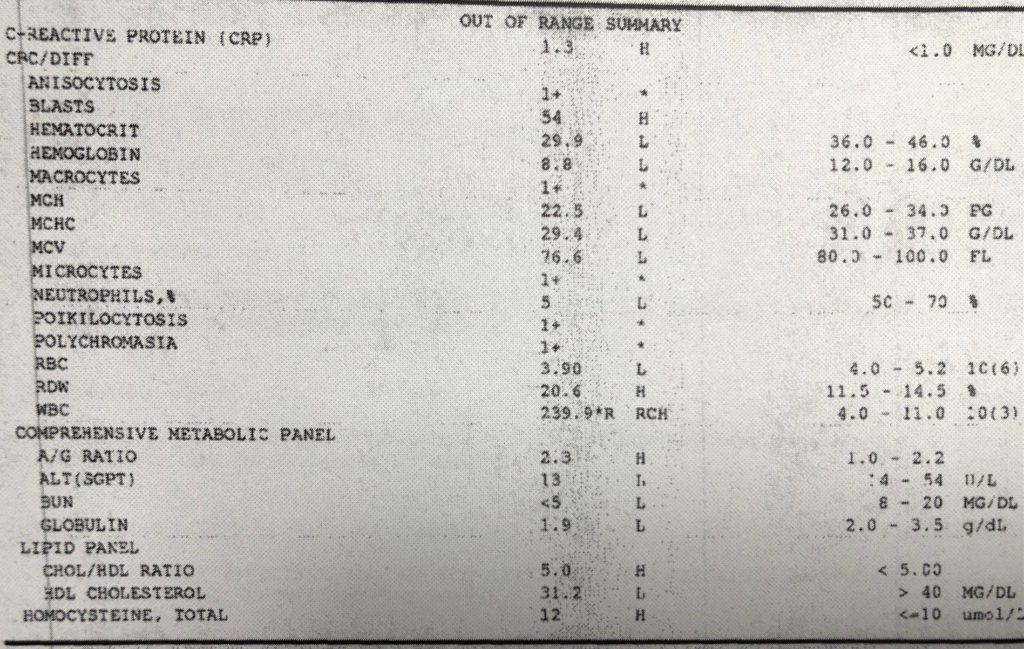
It’s down the line perfect, which to me, is an award or a diploma. It’s an achievement to see something like that because when I was diagnosed, it was a mess.
Today I’m really in some of the best health of my life at 57 years old.
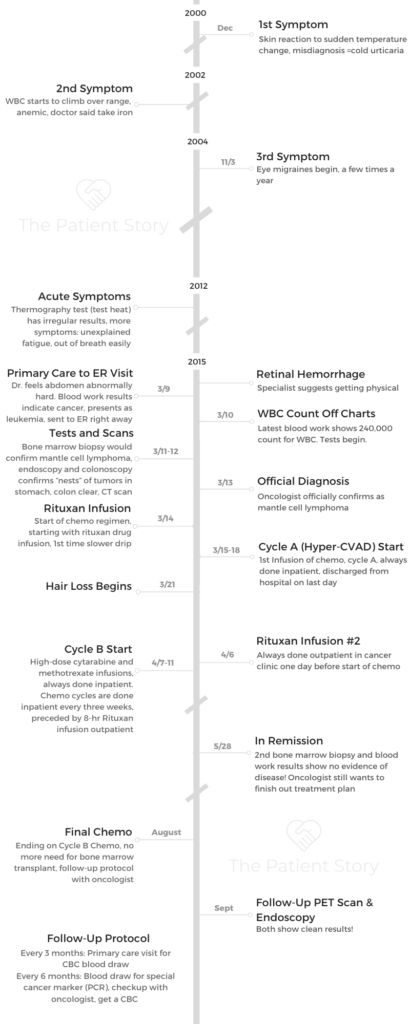
How did it take 15 years from first symptoms to get diagnosed?
One day I was outside walking through town. It was a windy, cool and wet day. I got back into my car, and all of a sudden, my face got really red, itchy and hot. It was really strange and scary to look at myself.
I drove myself home, and it took about 10 minutes to dissipate. I thought that wasn’t normal. There was something wrong here. I called my primary care doctor’s office, and the doctor I usually see wasn’t there, but another person was in his practice. This was Friday.
On Monday, I went to see him, and I told him about what happened. He said it was called cold urticaria — when your skin is cold and it warms up, you develop hives or a burning rash. He said he had that, too. It wasn’t a big deal. If I wanted, I could take an over-the-counter antihistamine.
It happened again and again. It was actually really scary. You never knew when it would happen. It would happen when my skin would get cold and then warm up somehow.
It was happening in the summer because I was outside, where it was great and warm outside, but then air-conditioned on the inside, so it was the change in temperature.
I wasn’t satisfied with that response, so I went to an allergist. She ran a whole bunch of tests on me and said it was idiopathic, meaning I had it but she didn’t know why I had it. She gave me an EpiPen in case I went into anaphylactic shock and a prescription for Allegra, which was prescription-only at the time.
I took that, and I thought it just wasn’t right. There was something still wrong about my biochemistry that there wasn’t before. Why was this happening? Just because they couldn’t figure it out didn’t mean there wasn’t something wrong behind it.
I lived with this for a while. Then I would go for my annual physical in 2004. My white blood cell (WBC) count started to climb higher. Then I started to become anemic. [The questions] became, “Did you have a cold recently? That would drive up the number. Oh, you’re a woman, it’s every month you’re becoming anemic from that. Here, take some iron.”
Every year I would go back, and it would be the same thing, but my WBC would climb up a little bit more and then a little bit more. I would become more anemic and a little more anemic. It would be the same thing, going on and on.
You started feeling acute symptoms in 2012
Things started to really seem to take a turn in 2012. I went through something very stressful, and I wasn’t feeling well. Then I did something called a thermography (test detecting blood flow and heat patterns), and my results came back very, very significant compared to the previous years when I had done the test.
I chalked it up to the stress of what I was going through. Since 2012, I really started to feel just exhausted from doing nothing. I just didn’t feel right.
I thought maybe I was going through menopause. Again, with the female issues, chalking it up to those changes. Then I got a retinal hemorrhage in my eye. That was early in 2015.
I don’t mess with my eyes, so I went to my eye doctor, who took a look at me and had a look of horror on her face. She sent me in that moment to a retinal specialist.
He looked at me, and he asked when my last physical was. I said it had been a couple of years. He wanted me to get diagnosed for hypertension, diabetes and a cardiovascular disorder. I still carry around the prescription in my wallet to this day.
I went right out, got a full physical. When I went that day, the doctor felt my abdomen and said it was rock hard. “Something’s going on.” He wanted to send me for an abdominal ultrasound for the next morning, and he’d set it up.
The next day — it’s March 10 — he calls. He said he wanted me and my husband to go into his office and that he had canceled the ultrasound. Jim, my husband and I went. He sits us down in the office and showed me my blood work that came back right away. The lab couldn’t get it back fast enough to him.
He said, ‘You have leukemia.’ When he showed me the results, my WBC, driven by my lymphocytes, was 240,000. The range is normally 4,000 to 11,000.
They did further analysis overnight, and there were all these crazy cells: cancer cells, misshapen cells, immature cells. You name it, I had it.
He said he had already called the emergency room and wanted me to go there right away, not stopping anywhere, not even home. He said they were waiting for me. His friend was the head of the leukemia department there.
When did you know something was seriously wrong?
I actually thought something was really wrong for a while. It just made sense. It was like, “Okay, now I know what I have.”
At first, I thought I had some autoimmune issue like lupus, and then the eye issue happened, the retinal hemorrhage. When the doctor said my eyes were fine — except for the hemorrhage — but asked about my last physical, it was then that I knew I was in for something. I actually said to a close friend that I thought I had lymphoma. I just came out and said it.
When the doctor examined me and mentioned my rock-hard abdomen, I thought ovarian cancer, pancreatic cancer, colon cancer. I thought of a cancer in that area.
What it really was was that my spleen was enlarged to 3 times its size from catching all those 240,000 times millions of white blood cells. It was like the repository for everything.
Basically, I had cancer throughout my entire body, including my eye. That’s what blocked my capillaries.
I didn’t get the connection with some of my symptoms previously, until I was in the hospital and I was thinking about it, because you have a lot of time to lie there and think.
Then I put it all together. Since I’ve been treated for lymphoma, I haven’t had the cold urticaria. I was just outside just now. It’s a cold, blustery day, and nothing. Now I understand the mechanisms behind why that happens. It pieced all of this together.
I go back to saying, back in 2000, something was wrong that wasn’t wrong before because this is happening now but didn’t happen then. What is it?
I won’t say nobody cared. Of course they cared, but nobody thought as deeply about it as I did. I thought deeply about it, but no professionals had thought deeply about it.
Mantle Cell Lymphoma Diagnosis
What tests did you undergo in the hospital?
Honestly, you start to feel like a thing, like a project. You lose your humanity a little bit, I have to say, going through it. You’re now a thing to be figured out.
I had heard horror stories about the bone marrow biopsy. The first time I had it done in the hospital to diagnose me, my primary care doctor’s friend, the head of leukemia, he did it. And it was fine! I thought, “This isn’t so bad.” It was pretty good.
Then going for the scans, I’m somebody who likes to avoid radiation therapy whenever possible. Now, I’m like, “My whole body’s being irradiated. Let them do it. We have to figure this out.”
I had to have a colonoscopy and an endoscopy to see if there were any lymphoma cells there. That was scary because that was under anesthesia, and the prep was miserable. I was in the hospital doing the prep, and it was already miserable in the hospital.
I did it, had a great doctor. They found a few little nests, groupings of cells, in my stomach. My colon was great, so it was like, “Great, I don’t have to get another colonoscopy for a while. They just did it. Awesome.”
I was getting blood work done every few hours. I was a pin cushion. They were poking and prodding me. It’s amazing how different each person’s technique was. Some you could hardly feel it, and some I would literally scream in pain.

But I was okay with all of this because it was going to help them help me and get to the bottom of what was really going on. It’s otherworldly.
You go to a place in my mind I never thought I could go. Somehow, I just did it. You just do it. You’re in a crisis situation.
Something switches on. You’re like, “Okay, I have to get through this. I have to do this and this, the next things, and then it’s all for good. It’s going to help everyone help me, and that’s it. Just got to do it.”
Those were really the tests they used to diagnose me. The CT scan, colonoscopy, endoscopy, bone marrow biopsy and a million different blood tests.
Describe the bone marrow biopsy
I was on my stomach, and they numbed the lower part of my back with a local anesthetic. They drilled into my spine. They literally drill, and I could feel the vibration of it. They went into a few different places to get different samples. That was it.
I felt more of the grinding of the apparatus than pain. The pain was when they gave me the shot of the anesthetic, but even that wasn’t bad.
He was a doctor and so gentle with me. The bone marrow biopsy was really nothing at all that time.
It took him 7 minutes, not quite 10 minutes to do the whole thing and get the samples. As a result of doing the biopsy, we realized I didn’t have leukemia. I had mantle cell lymphoma (MCL), which was a much more serious diagnosis. It gave good information.
How long did pathology results take?
That was that evening I was admitted that day, March 10. It was that evening I had it done. It came back the next day. It was in the hospital, where they expedite things.
Then they said they had to transfer me to the lymphoma floor with different people.

How did you process the mantle cell lymphoma (MCL) diagnosis?
I happen to have a very good friend who’s a retired physician. He was my advocate and my sounding board. He was able to deconstruct some things for me and let me know a little bit more — but not too much more.
I didn’t want to know too much more. I feel like that helped me get through things, just knowing what I needed to at that time, but I knew someone else was looking out for my best interests as well.
I knew it was more serious, and I knew what they had told me. When my primary care doctor first told me the news, the first thing I did was I looked him in the face and asked, “Am I going to die?”
He said, “No, you’re not going to die, but you need attention now. You need to get this dealt with now.” That’s when he said not to go home, go straight to the ER, don’t make a stop.
Once again, I asked the doctors [at the hospital], “Am I going to die from this?” One of the doctors said no, I wouldn’t die. They wouldn’t let me die, but I would have to go through 6 rounds of inpatient chemotherapy, alternating A and B cycles.
When I was done, they would do a bone marrow transplant. That’s how I was going to be okay. They don’t use the word “cure.” I understand that, but that’s how I wasn’t going to die.
Describe the colonoscopy and endoscopy
The colonoscopy and endoscopy were done by a doctor in the hospital, who then became my subsequent GI doctor. We had to do the fabulous prep that everybody talks about.
I had to drink this really hideous-tasting stuff and clean myself out the night before. Then I was up all night anyway, so the good thing is you’re so tired. The next morning, you’re so out of it because you’re so tired.
They wheeled me down to the procedure area. It wasn’t an operating room. They do a lot of these. Then I talked to the doctor for a few minutes. I got a good feeling about him. They put me in this twilight sleep.
I was glad to get them both done. I thought if everything is okay, I wouldn’t have to get another colonoscopy for 10 years.
I had been fearing it. I was 51, just turning 52, so I was supposed to do the colonoscopy anyway. When I woke up and they told me my results were good, I felt relieved.
Immediately, I felt good like, “Okay, that’s over with. I was out of the anesthesia. Now what could I eat?” That’s a good sign, by the way.
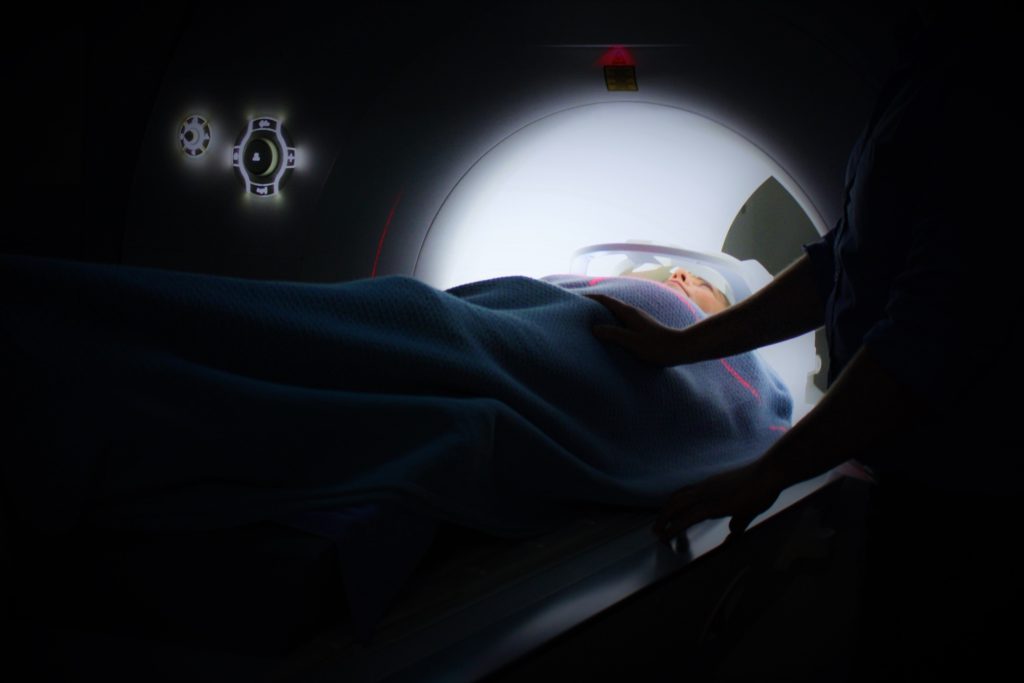
Describe the CT scan
They wheeled me down and gave me this injection of contrast dye. They told me some people reacted badly to it, so they wanted to see if I did. I didn’t.
I went into this machine, which could be a little claustrophobic, but my head was out, so that was okay.
Then I heard these click-click sounds and just felt in my head the radiation from it. I knew what they were doing and just wanted it over with.
The thing I kept hoping was I wouldn’t have a reaction to the injection, the contrast. That was almost occupying my mind. “Am I having a reaction? Is this one? No, I’m okay.” That kept me occupied.
You underwent genetic testing
One of the things about the blood tests is it was important for them to see whether or not this was genetic or acquired. It was not genetic. If it was genetic, they would have to treat me differently.
This was something at some point in my life, there was damage to my DNA and some of my cells, and they replicated out of control over time. That was important information they needed to get.
I had gene mutations, but they were only in the cells that were cancerous.
Chemotherapy and Side Effects
Did you get a port, PICC line or go through IV for infusions?
The first 3 times or so, we just did IV. Then the fourth cycle, we decided to go with a PICC line because it was getting too much — jabbing me, the veins started collapsing.
I ended up getting a PICC line installed and using that for the subsequent visits. It was in my arm, and I have a teeny, tiny little scar from it.

Describe the mini-surgery for the PICC line and caring for it
They wheeled me down and did a scan of the moment (and area), to see what was going on and guide them to put the line in my arm.
One of the things you have to be careful about is infection. They really worry about this thing getting infected.
It has to be flushed out [with saline regularly]. You take that home with you, and you go home with the PICC line in your arm. Now you have to learn how to flush that out yourself.
For the first bunch of times, we had a nurse come to the house with all the equipment and show us how to do it. Then you have to do it. The last thing that can happen is that it gets infected.
Now you have this thing in your arm. You can’t get it wet. You have to prep it when you take a shower.
You have to saran wrap around it. Then it’s there. It’s another reminder of things.
It did make life a lot easier when they had to give me all of the infusions and take blood.
What was your MCL chemotherapy regimen?
The first thing in the hospital was the Rituxan, a biologic, a drug I got. Technically, it wasn’t chemotherapy. They do it the day before, and then you get the chemotherapy.
It was March 14 when I got that. I happened to be alone. Everyone had gone home. It was late afternoon. They started to give me the infusion of the Rituxan.
What happened very quickly was I started to get chills. I was shaking uncontrollably and felt like I had a fever after about 10 to 15 minutes of getting the Rituxan infusion.
I called them for help because it felt like something was wrong. They stopped the infusion and said I was having a reaction, that sometimes people had a reaction.
What that reaction really was was I was so loaded with cancer cells throughout my body, this was literally the cancer cells being killed off. That was what I was feeling.
Because I had so much cancer in me to be killed, the reaction was just way too much. They had to scale it back and give it to me differently: a lot less over a much longer period of time.
That became what we ended up doing for all 6 cycles, even though by Cycle 3 or 4, I probably didn’t need it. But I said, “I’ll stay here longer, and you give it to me slower.”
I thought, “Geez, if this is how it’s starting out, this isn’t good.” There were several low points. That was definitely one of them.
I got through it, and the next day they started the chemo. There were 4 different drugs for Cycle A. It was A, B, A, B, A, B. A is better than B.
Cycle B is 2 drugs plus Rituxan. Cycle A is 4 drugs plus Rituxan, but it’s still better [than Cycle B].
You have to be inpatient because you’re getting the chemo over many hours in the infusions, and they have to constantly check your blood counts. The chemo will make certain blood cells plummet and will also affect kidney function.
They had to constantly test me to make sure things were okay, and if they weren’t okay, they’d have to give me treatment.
Rituxan was given outpatient starting Cycle 2
After this first hospital stay, I’d go into the cancer center and get the Rituxan infusion in the outpatient room with a bunch of other people. Then I’d go home. On those days, I’d be there 6 or 8 hours getting that slow Rituxan infusion.
Then I got to go home to prepare for the next day, being admitted to the hospital for the next 4o 5 days to get the other infusions.
Describe the inpatient cycle schedules
The cycles lasted 4 days. I’d get one infusion, then we’d stop for a while. Then I’d get another infusion. The weirdest one was on Cycle A, maybe the vancomycin (antibiotic), they’d inject that into me just a couple of hours before I was scheduled to leave the hospital. Then they rushed me out.
It was kind of weird but good. Get me out of here! There’s no feeling like being released from the hospital. You feel like you’re in custody.
You’re hooked up to those IVs for days. They go everywhere with you! I have to go to the bathroom, okay, I have to take this with me. I think I gave it a name at some point.
You are walking around the hallway to get that exercise and get out of bed, and you’re dragging it along with you. You’re hooked up to this thing.
The freedom of getting that off of you and being out in the fresh air was fabulous. It was the best thing ever in the world, like being released from prison.

Describe the hair loss
The obvious first side effect is your hair starts to fall out. It started about a week after I got home. Clumps of hair would be on the wall of the shower. That’s just a freaky thing to see.
My hair was even a lot bigger and longer then. To see that, it’s like a part of my body is now on the shower wall. “My body’s coming apart,” is how I felt. Then a friend of mine is a hairdresser. I went to her, and I had her shave me.
It was a lot less traumatic. Her sister is a wigmaker, so she then took my measurements and made me a custom wig of human hair similar to what I had.
Honestly, I wore the wig about 3 times because it was spring going into summer. It was hot. Where am I going? I’m going to doctor’s offices and to the hospital. Where am I going that I care?
I still have this beautiful wig, custom-made for me. Hopefully I never need it again. Maybe someone else will want it, and I can give it to them. That was hard. Honestly, after the initial shock of it coming off of me, I got over it.
Everybody told me what a great-shaped head I had, and I actually did. I really don’t look bad without hair. That was an obvious side effect.
»MORE: Dealing with hair loss during cancer treatment

What were the other chemo side effects?
Summary: rashes on hands and legs, low blood counts, high fevers, mouth sores
For Cycle B, one of the side effects was these horrible rashes, these scabby rashes all over my legs that were just hideous. Cycle B, my blood counts, my platelets plummeted, so the littlest thing that would make me bleed would be a horror show.
There were a couple of times I had to go to the cancer center and get blood transfusions because I was bleeding, and my blood counts were too low.
When I was getting treated, they analyzed me, and I also had to get transfusions. Between platelets and blood, I probably got 50 units.
That was the worst side effect because that’s scary. The littlest cut and now I’m uncontrollably bleeding and couldn’t stop it. That was horrific.
There was another horrible side effect. Beginning of June, I went back to get a check-up, and I had a fever. I wasn’t feeling right, so I knew something was wrong. It turned out I had a high fever of about 103 degrees.
They admitted me to the hospital, thinking I had some crazy infection. I told them I didn’t feel like I had an infection. It felt like something else.
They ran every test on me, including a bronchoscopy when they put you under, put in a scope and look in your lungs. My lungs were great.
I didn’t have any blood work that indicated an infection. They did another CT scan to see if I had anything and couldn’t find anything.
They called in an infectious diseases specialist. I kept having these fevers of 103 and 104. Then I would take Tylenol and get the fevers back down.
In another 6 hours, I’d start to get the chills again, and the fever would go up again. This went on for 11 days. I was in the hospital, not having chemo but having these fevers they couldn’t figure out.
At the end, they admitted it’s an effect of the chemo. I was like, ‘Okay, I thought that,’ but they had to do their due diligence and figure it out. I knew I didn’t have an infection.
Because of this, I was on all kinds of IV antibiotics just in case. Those do other things to you, which then you have to correct. That was another really, really bad side effect.
The mouth sores were much worse with Cycle B than Cycle A. I would be having a chemo infusion and started to feel nauseous in the hospital. Then I’d go home, and then the mouth sores would start. They gave me some prophylactic rinses for it, but it still happened.
What was happening was the nausea was subsiding, but I couldn’t eat because the mouth sores hurt so much. I would be starving but couldn’t eat or swallow because it hurt too much. So I lost a lot of weight.
By the third week of the cycle, the mouth sores would dissipate. I’d feel stronger, and that’s when I would load up with food. I would load up as much as I could eat then to prepare for the next time.
When I say load up, I mean good, healthy food, not junk food, to build my body up as strong as it could be for the next series.
»MORE: Cancer patients share their treatment side effects
Any guidance on what helped with the side effects?
For the mouth sores, they gave me a salt wash. That does help. I was drinking a lot of cooling things with ice; that helped. Other than that, there wasn’t a lot I could do for that.
For the rashes, they gave me some cream to put on. I did that, and it helped. I don’t have any scars from the experience, so that’s good.
In terms of the nausea, by the time I got home, it had gone away. I threw up only one time, and that was in the hospital during the sixth cycle. They’d given me some Tylenol and pre-meds, and that came up. But that was the only time I threw up.
Tips on how to get through repeated hospital stays
If you can have somebody bring in your food, have them bring in good, healthy food. Some of the hospital food was okay, but not the most health-promoting nutrition. It gets something into you if you can eat it.
I had my husband and a family friend bring in homemade soups. They also brought in green juices, but the team made them take them out because they were raw, and they thought it could be a disease risk with the raw juices.
Honestly, when I was home, I did juices, smoothies. Sometimes the cold smoothies were all I could get down, and I would pack my supplements into them, to get it down past my mouth sores.
The problem is, the hospital is the worst place to get any rest. Especially with what I had, they were testing my blood every few hours.
2 in the morning, the lights come on, a phlebotomist comes in. I was getting an hour or 2 of sleep at a time. I don’t even know what to say about that because it is what it is. Just know that’s going to be a thing.
The other thing is if you can get up and move around safely — if you feel like you’re going to fall, don’t do it — get out of the bed and get a little bit of activity. They’d have a lap counter, and you’d make laps around the floor. See who did what, almost like a contest.
If you can do that, don’t do it by yourself, have somebody there. Me and my little IV pole and husband or friend would go and do the laps.
It was important to try and move around as much as I could. But understand your limitations. If you feel you’re going to fall, the last thing you want to do is fall, trust me. Don’t fall. Even getting up and going to the bathroom, if you feel the least bit unsteady or dizzy, have somebody help you.

In Remission
How did they track the progress of treatment?
That was my second bone marrow biopsy. The bone marrow biopsy was one thing that helped diagnose my remission. The other thing was the PCR test, which tests for minimal residual disease. It’s just a blood test, not a complicated one, but also not a run-of-the-mill blood test. The results take a while.
That came back at that time as no evidence of disease. The biopsy also got back, but we didn’t get these results until after my fourth treatment.
The good news was the bone marrow transplant they were planning for me, interviewing and trying to find donors, was put on hold.
I looked at them when I got this result and said, “I guess we don’t have to do that anymore, or do we?”
They looked and were like, “No, I guess we don’t. But if it comes back, you’re getting that transplant.”
I said, “It’s not coming back.” Reading about what that entailed sounded brutal and difficult.
Processing news of being in remission
It was crazy because 2.5 months earlier, my whole body was loaded with these cancerous white blood cells from top to bottom, stage 4. And 2.5 months later, there’s no evidence of any disease in me. How is that possible? It was miraculous.
I feel I was spared for a reason. I think being able to tell my story and give encouragement to people is part of that. I think that’s the reason.

What is the follow-up protocol
I went for a PET scan that September to make sure there was nothing there. I went for a follow-up endoscopy, because at the time, they had found those little nests of some lymphoma cells. They wanted to check it out.
There was nothing there. Clean and beautiful!
At first, the first year, my follow-up was every 3 months. That would consist of going to the lab first in the cancer center and having a CBC (complete blood count). They’d test some of my vitals. Then I’d go upstairs and see my doctor. We’d go over the results, and that was it.
Because I was doing so well, it became every 6 months. I won’t go for any more scans if I don’t need any more scans. If I don’t need radiation, I don’t want to have more. Because what I had in mantle cell lymphoma can be detected through blood, I’m lucky.
I can do these PCR tests. Now, a month before my visit with my oncologist, I go to the lab, they draw my blood for the PCR test, they send it to a lab out West, it takes about a month to get the results back, and then I see my oncologist.
That day, when I go, I still get the CBC and then go upstairs. They have the results of the PCR and CBC tests.
Dealing with anxiety waiting for results
Those are the most nerve-wracking visits. About a couple weeks beforehand, I get really cranky and crabby. Sometimes I’ll go to my primary care doctor to do a CBC just so I can see, “Okay, this is good. No surprises.” It makes me feel better, and he’s more than happy to do it.
That’s the worst part of this thing, those visits, because you’re successful, but what if one day I’m not? Then what? That voice of, “Well you’re going for that stem cell transplant,” comes to my head.
It can’t happen. Not a possibility. I don’t want to even put that out there.
»MORE: Dealing with scanxiety and waiting for results
Reflections
How has survivorship been?
I feel like my best insurance policy against something going wrong is taking as good of care of myself, both body and mind, as I can. That’s the part I’m doing. The doctors do their part, but I have a part in this, too.
If I take care of myself — and I have to take care of myself better than the average person now that I’ve gone through all of this — if I can do the right things, I’m insuring myself against a recurrence and also mitigating effects of that really harsh treatment they give you in hazmat suits with skull and crossbones on it.
I have to do really well in terms of nutrition, eat a whole food plant-based diet, limit processed foods, take a whole bunch of supplements that protect cells and the immune system.
I do the fasting-mimicking diet every few months, which helps rejuvenate and get rid of dead cells that don’t belong in the body and regrow stem cells. I try to exercise.
My oncologist was huge on that. He would say that every time. I have to admit, during the pandemic, I’ve slacked off a bit on that. It’s something I have to do better at, but I’m not going to punish myself.
I know what I have to do. I’m going to get back, and I’m going to do it. Exercise is a big part of the healing process and mitigating problems down the road.

Wellness is a core focus for you in your recovery
Mindfulness, being present in the moment, just telling yourself, “At this moment, I am safe. At this moment, I am safe.” Also learning how to breathe properly, relax your mind, relax your body. It lowers blood pressure and heart rate. It’s something that I’ve been doing more and more of.
I own a wellness center. Before COVID-19, we were doing things live here. We can do them virtually. My practitioners are doing virtual sessions. My husband and I do it on our own. It really helps.
Your physical health helped you through treatment
My healthy lifestyle before, during (as best as I could) and after treatment up until today is part of why I was so successful with getting through treatment and mitigating the side effects as best as I could, and also recovering and rebuilding.
One of my doctors said another woman my age with my same diagnosis would not have fared as well.
People can sometimes have some control over their situations. I want people to feel like they they have some control over their lives, even if they face a serious diagnosis.
The importance of taking care of mental health
I’ll also admit, I’m seeing a psychologist, because you need that objective viewpoint of validating how you’re feeling and also course correcting. If your thoughts start to go in a not-great place, helping to course correct that back. I feel it’s maintenance.
Of course, during COVID-19, everything is amplified. Not only are you worried about your cancer issue, but your compromised immune system and what the implications are of that. I have to be more careful than most.
Your mental health is connected literally to your physical health. You can’t take care of one and not the other. We are one body with many different components; we’re not one part. We are not one heart, one spleen, a lymphatic system. We’re the whole thing.

What was the support you needed the most through treatment?
You definitely need support, but I honestly didn’t want too much support. What I mean by that is I had a few people who were closest to me, but I didn’t want a lot of people coming to the hospital.
I didn’t want a lot of people visiting. Number 1, it could have been an infection risk, but number 2, I didn’t want people seeing me like that.
More than that, I didn’t have the strength and the stamina to entertain people. Plus, if I had to get up and go to the bathroom, I’d have to drag this IV pole in my nightgown, and now I have an audience in front of me.
I only wanted very few of the people closest to me around, but I knew there were lots of people pulling for me. They were praying for me, sending me healing energy and light and goodness. I know they were.
I can’t tell you how much that helps. I ask for it every time when I’m going to my oncology visit. I ask for that again. It really gets me through everything.
The support I needed was more logistical, like making sure I had what I needed. That I had the food I needed, could get to the cancer center. My friend, who’s a retired doctor, would help me interpret things and give me advice on stuff. I don’t have much family. I don’t have any family within thousands of miles of where I live except my husband.
I remember lying there in the bed in the hospital thinking, ‘I wish I had a parent to be here and tell me everything was going to be okay.’
That was really hard. I remember wishing I had a parent to hold me and tell me everything was going to be okay. That support I don’t have because they don’t exist.
But I have a wonderful husband. It was very hard for him because he’s not trained for this, but he loves me. I’m his world. He’s in IT, so he has that kind of brain. Whatever he could do for me, he would do, no question.
He would visit every day and bring my food, however he could support me. He wanted to know, “How can I help you?” Thank goodness I had him and some close friends.
I had people operating my center while I was gone and able to keep my business open. I was very fortunate to have them and very grateful. The classes still went on, and things got done. That was a load off my mind.
People tried to take whatever burdens off of me that I could in whatever way that I could. That’s what a good caregiver does. They try to ease my burdens.
Message to other patients and caregivers
Get your support team together. Get those few people in your circle who can help you, who can be there in whatever way you need them. Figure out who they are, whether they’re family, friends or professionals in what they do. Get that support group.
Don’t read too much about your illness online. Only get the information you need to know. Know enough that you’re making the right decisions for you. I’m not saying hide from it either, but you could get lost in what happened to this person and that person.
I would hear these stories from other people when I’d be in the infusion room. They’d be telling their stories about how this didn’t work, and they got this problem from that treatment. It was like, “I can’t hear all of this. I need to stay in my lane and focus on my own situation, which is different from theirs.”
You are an individual, a bio-individual. No one else is like you. You will respond to the treatment in the way that you will respond, not the next person, not the person with the horror story. You can’t go down that road.
At the same time, be educated and knowledgeable about what you’re about to go through. Make your own decisions. If something doesn’t feel right, get another opinion. If it still doesn’t feel right, maybe you don’t do that thing.
You’re not forced to do anything, actually. You have free will. If something really doesn’t feel right or maybe you don’t connect with that doctor for whatever reason, you’re the client. Find another doctor. Sometimes the difference is the bedside manner. Makes all the difference in the world.
The other thing is, in looking at statistics, mantle cell lymphoma has a really, really poor 10-year survival rate. There are several reasons for that.
I just kept telling myself, “It’s going to be me. If 10% survive, it’s going to be me.”
My advice to you is that statistically somebody survives their illness. You be in that group.
Someone is, so you be that whatever percent that is. People make it — why not you?

I think I was meant to survive for a reason: to show people it was possible to have a stage 4 cancer diagnosis with a poor prognosis and come out of it better than before.
If I can help and inspire someone else, then this is what I am meant to do, and I am grateful for the chance to do it!

Inspired by Sheryl's story?
Share your story, too!
Mantle Cell Lymphoma (MCL) Stories
Tim H., Mantle Cell Lymphoma (MCL), Stage 3/2
1st Symptoms: Lump on left-side of neck that grew bigger over a couple years, new lump on right side
Treatment: 6 cycles Nordic chemo protocol, alternating cycles of R-CHOP and rituximab + high-dose cytarabine, autologous stem cell transplant
Sheryl B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: (Over 15 years) Skin irritation from temperature changes, rising WBC levels, unexplained fatigue, retinal hemorrhage, hardened abdomen (from enlarged spleen)
Treatment: 6 cycles Hyper-CVAD chemotherapy
Shari B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: None, lymphoma discovered at unrelated doctor appointment
Treatment: 6 cycles R-CHOP, 5 cycles Phase 3 trial of Velcade + Rituxan (normally for multiple myeloma), allogeneic bone marrow transplant (BMT)
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Fatigue, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Hives, inflamed arms
Treatment: Calabrutinib, Lenalidomide, Rituxan
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Elevated white blood cell count
Treatment: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: No symptoms
Treatment: R-CHOP chemotherapy, rituximab





