Bobby’s Stage 4 MCL Non-Hodgkin’s Lymphoma Story
Bobby was diagnosed with stage 4 mantle cell lymphoma at 56 years old. Explore his story as he outlines going through a clinical trial to reach remission.
He also talks about breaking the news to his loved ones, taking health issues seriously and taking care of mental health.

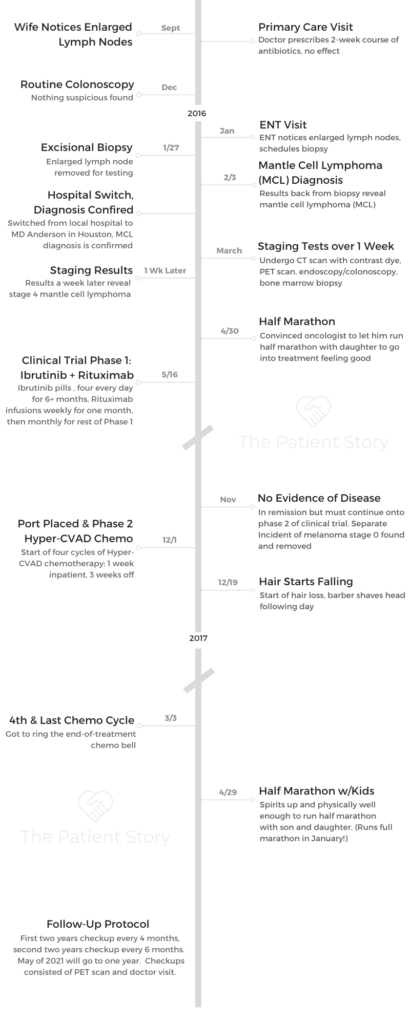
- Name: Bobby J.
- Diagnosis (DX):
- Mantle cell lymphoma (MCL)
- Subtype of non-Hodgkin’s lymphoma (NHL)
- Stage 4
- Age at DX: 56
- 1st Symptoms:
- Fatigue (only in hindsight)
- Enlarged lymph nodes (noticed by spouse)
- Treatment:
- Clinical Trial
- Phase 1: Ibrutinib + Rituximab
- Ibrutinib: Oral pills
- 4 pills/day for 6+ months
- Rituximab: Infusions
- Weekly for 4 weeks
- Moved to monthly
- Ibrutinib: Oral pills
- Phase 2: Consolidated Chemo
- Hyper-CVAD
- 4 cycles (traditionally 6 cycles)
- Inpatient for 1 week
- Off for 3 weeks
- Video: Getting Diagnosed & Staging
- Getting Diagnosed
- Tell us about yourself outside of cancer
- What were your 1st symptoms?
- Describe the ultrasound tests
- What happened at the ENT visit?
- Describe the excisional biopsy
- Had the doctors ever mentioned cancer being a possibility?
- How did you learn the cancer diagnosis?
- How did you decide where to get treatment?
- How did you tell your friends and family about the diagnosis?
- It’s important to delegate responsibilities to others if you can
- Staging (Tests & Scans)
- Treatment Decisions
- Getting Diagnosed
- Video: Bobby on Treatment and Side Effects (Clinical Trial)
- Treatment and Side Effects
- What was your treatment regimen (clinical trial)?
- Issue with low heart rate
- How did you pass the time for the rituximab infusions?
- Did you need a caregiver at the infusions?
- What were the ibrutinib and rituximab side effects?
- How did you learn there was no evidence of disease (NED)?
- Describe getting the port placed
- You started the chemo (Phase 2) right after the port placement
- Describe the prep before the Hyper CVAD chemo
- Self-motivation to move around as much as possible
- How many days did you get off between the 1-week cycles inpatient?
- The anti-nausea cocktail caused depression
- Also couldn’t drive after first nausea medication dose
- You asked to stop taking the anti-nausea cocktail
- Any side effects from the hyper-CVAD chemo?
- Describe the hair loss
- How did you end the chemo treatment?
- Treatment and Side Effects
- Video: Bobby Being Part of a Clinical Trial
- Being Part of a Clinical Trial
- Describe the clinical trial
- How did you discover the clinical trial?
- Describe your impression of your oncologist
- What was the prep like getting into the clinical trial?
- You couldn’t take other medications during the trial
- What would have happened if your fever had passed 100?
- What made you and your wife so sure about the clinical trial?
- Describe meeting the first person to go through the clinical trial
- If you had been Patient #1, would you have still done the clinical trial?
- Was the monitoring any different in the trial?
- What did you have to include in the journal?
- Donating your tissue and blood samples to research
- What’s the follow-up?
- Did you have to deal with insurance for the clinical trial?
- Being Part of a Clinical Trial
- Video: Bobby's Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I can’t tell you the blessings that I’ve received that I would not have received had I never been diagnosed with cancer.
I know that’s probably the weirdest, oddest thing that anybody would say, but from my shoes, I don’t think I would change anything in terms of what happened.
It has brought me and my family closer together, it has helped me from a faith perspective, and there are so many people I’ve met whom I would have never met.
Bobby J.
Video: Getting Diagnosed & Staging
Getting Diagnosed
Tell us about yourself outside of cancer
I played golf in high school and college. I ran just to keep my legs in shape. It was really odd that right before I got diagnosed, I wanted to run a race with my son in Colorado, and I’d gotten pretty bad out of shape. I fluke-ishly found this race in Colorado, and he agreed to go with me. This was about 2 years before my diagnosis.
I got in somewhat decent shape to run the race. I ran it again the following year. The year after that was when I was diagnosed. Part of that, physically — the doctor said the reason why it helped me get through my treatments was that I was in such good shape.
I was getting in shape for a race I wasn’t aware of.

What were your 1st symptoms?
The first symptom I had — and didn’t realize — was fatigue. I was running. I live in Louisiana; it gets very hot here.
My son and I were getting ready to go back to Colorado to climb, so I was running to get in shape for that. I noticed after I’d run about 5 miles, I got tired. Usually I could go about 6 miles without any trouble, and I noticed that at 5 miles, I started getting really tired.
Once that happened, the next thing was my wife noticed an enlarged lymph node on my neck. I also had one on the back of my neck.
When I went to the doctor’s, he said, “When you come back, we’ll start dealing with it from there.” Fatigue really was probably the first sign. I would not have known that.
Describe the ultrasound tests
The next thing — after the antibiotics I took for 2 weeks that didn’t work — was I had 2 ultrasounds done. One was on the lymph nodes on my neck. I had another small lymph node on my ribcage. It was almost like a calcium deposit.
They did the ultrasound on my neck. Then they did one on my ribcage. Both of those tests came back inconclusive.
What happened at the ENT visit?
My general physician suggested after the colonoscopy that I go to the ENT since the colonoscopy did not show any cancer. We made an appointment with the ENT.
Of all the things I’ve been through, probably the most invasive thing I felt was when he had to check my throat and went through my nose.
I feel so bad for people who have to take the swabs for COVID because I know how uncomfortable it is. It didn’t hurt. It’s just strange.
The ENT looked and really couldn’t tell anything. The only thing he felt like he could do to make sure was to biopsy and remove one of the lymph nodes.
Describe the excisional biopsy
I went in, and the anesthesiologist came in. He said I’d be in his hands for the next hour, however long it’d take. I got drugged up pretty good! My memory was of speaking to the anesthesiologist. The doctor came in. My wife took some funny videos.
I was pretty drugged up. The next thing I know, I woke up, and they said they’d let me know the results in about 1 week. That was on a Wednesday. My next appointment was about a week later.
Had the doctors ever mentioned cancer being a possibility?
I don’t remember them ever mentioning cancer. It was that I could have cat scratch fever, I had a cat, because he used to scratch and bite.
Never to my knowledge did they say anything about cancer.
How did you learn the cancer diagnosis?
It was a very emotional day. I had an appointment for 3 o’clock. My wife and I went down. The doctor came in and said they’d just got the results back. He said I had mantle cell lymphoma.
He began to go through some of the items, like, “This used to be very bad. Now there’s a better survival rate.” I felt really bad for the doctor. I actually went back and saw him last year. I didn’t have an appointment, just went by his office and asked his nurse to see him. I said I didn’t know how he’s able to do this, giving people this kind of news.
It was a very emotional time. My wife, who was there with me, and I were only in for about 15 minutes.
How did you decide where to get treatment?
My doctor discussed some treatment options here locally. We opted not to stay here in town.
We had decided years ago that if anything like this ever happened, we would seek medical attention at MD Anderson in Houston. It’s close enough for us, and the reputation there is wonderful.
How did you tell your friends and family about the diagnosis?
I remember I went back to work. I did not want to call my employees and let them know this is what happened. When we got back to the parking lot and we got my children on the phone, I couldn’t tell them. My wife had to.
We just got them both on the phone. Neither of them lived here. Next, we had to go to my office. I pulled my employees together, and I couldn’t tell them either. My wife had to tell them as well.
It was pretty devastating from that perspective. I’ve heard other people who’ve been diagnosed. Never would have dreamed that it would be me one day.
There were a couple of days it was very emotional because the one thing that I struggled with more than anything was they didn’t know how bad it was.
They just knew that I had mantle cell lymphoma. It was bad enough being told, but not knowing what stage I was made it worse. They didn’t know.
It’s important to delegate responsibilities to others if you can
One of the things my wife and I agreed on, or I insisted on, was that I didn’t need to think about anything other than getting well. I said I needed her to be in charge of appointments, telling me where I was supposed to be and when.
I’ve always been a very loyal worker. I put in the hours. I do what I’m supposed to do. During this time, I told my wife that whenever, whatever, this cancer was priority 1, and everything else would go to the backburner.
My wife took over that role and would let me know where I’d have to be and when. She kept everything organized and moving forward.

»MORE: Breaking the news of a diagnosis to loved ones
Staging (Tests & Scans)
Describe the CT scan
My veins are not great. I don’t drink enough water, so needles are not really nice to me. I have not had a lot of success with the CT scan, although I just got back from Houston last week for my check-up. It was all clear, and I only got stuck one time for my CT scan, which was unusual.
That one I dreaded the most. I really dreaded going down there — not worried about the check-up but for the stick for the contrast dye. I really didn’t like that one too much.
Describe the colonoscopy/endoscopy
The colonoscopy prep, for anyone who’s ever had one, there’s no fun there, especially when you’re not at home. The actual test itself was really not difficult. They put you to sleep, and you cruise through it.
Describe the PET scan
The PET scan was similar, but you have to be patient with it. They inject you with “nuclear sugar” — that’s my layman’s term for it. You have to wait about an hour before they actually put you in the tube. There’s nothing constricting, so it’s open-ended.
There really weren’t bad issues, other than the fact that I had to hold my arms up over my head during the test. For somebody who’s not really limber, 15 minutes in one spot is not really fun.
Describe the bone marrow biopsy
There was a local shot [of anesthesia], similar to the colonoscopy, so I really didn’t feel anything. I didn’t feel the incision and the actual biopsy itself.
I was pretty knocked out. I didn’t know other than I lay down, and the next thing I knew, I was in a wheelchair. It was not bad.
How long did it take to get the staging results?
I had all the tests done over about a week’s time. Their terminology for the stage 4 cancer for me was above and below the diaphragm, and the bone marrow was also involved.
Treatment Decisions
How did your doctor describe the “watch and wait” method?
My doctor said the mantle cell lymphoma was very slow-growing (indolent). One of the things I learned, or my interpretation of it, was that whatever they give you, any time frame of “how many years you have left,” it’s after you go in remission.
For me, I thought if I could not have any treatment, the longer I could hold the treatments off, the timeline for remission wouldn’t start. Even though the cancer was there and diagnosed stage 4, the doctor seemed to think that it could be years before they would treat me.
When he explained that to me, I thought that was cool with me because as long as my timeline didn’t start until after treatment and remission, it’s years I’d be adding onto my life.
He did a great job of explaining that. I had no issues with the watch and wait method and delaying actual treatment.
You ended up starting treatment soon after
Later, H. pylori (bacteria) was discovered in my stomach from the endoscopy, which caused an ulcer. My oncologist determined the ulcer was caused by the cancer and decided to start treatments.
The local doctor did not discover cancer in the colon from the colonoscopy because no polyps were discovered, and most colonoscopies do not biopsy the colon during this procedure. Cancer was found in the colon from the test in Houston because they did a biopsy.
This was the only time that my doctors actually disagreed.
The gentleman who did the endoscopy felt the ulcer was caused by the H. pylori. That was good because I didn’t have to start treatments.
But my main oncologist was the one who decided he thought the cancer caused the ulcer, so they’d go ahead with treatment. In his mind, we’d just wipe the cancer out. We started the treatments shortly after that.
Message about getting a second opinion and self advocacy
I think it’s very much about people being at peace with their decisions.
Like it or not, you’re dealing with life-and-death decisions. I’m not saying that had I gone somewhere else my outcome would have been different. It could’ve been the same.
I do know that we were very much at peace about making the call to go to MD Anderson. My doctor wrote the protocol for my treatment. To me, it’s different if you go someplace like that compared to a doctor maybe in a smaller city who doesn’t see mantle cell lymphoma patients. They may open a book and say this is what the book says your treatment is.
We also considered another place. I have a friend who lives in Baltimore, so we considered Johns Hopkins and maybe the Mayo Clinic, but that was a bit of a stretch for us. My wife and I were very much at peace going to MD Anderson, and it’s just a first-class place.
»MORE: How to be a self-advocate as a patient

Deciding to run a marathon before chemotherapy
It was another emotional time. I’d actually signed up for this marathon the year before. I ran it in 2015, and it was in Nashville. My daughter lives about 20 miles away from there.
After I got diagnosed, the doctor actually told me he didn’t want me to run. My point for my oncologist, when he finally acquiesced, was that I wasn’t running it for my own self-satisfaction or gratification.
I was running to show that you can be sick and still run. You can be sick and still be active.
He finally relented. My daughter said since my oncologist didn’t want me to overdo it, she’d run with me. She doesn’t run at all.
It was probably a bigger achievement for her than it was for me because she finished. It took me about 30 minutes longer the year she ran it with me than the year before. I kept telling her she just slowed me down.
It was a great experience to do that, knowing that of all the things we were getting ready to be in front of.
My point was, ‘Hey, we’re going to do this, and we’re going to show this cancer who’s in charge here.’
Video: Bobby on Treatment and Side Effects (Clinical Trial)
Treatment and Side Effects
What was your treatment regimen (clinical trial)?
Summary: Ibrutinib (oral pills, 4 a day for 6+ months) + rituximab (infusions, weekly for 4 weeks, then monthly) + Consolidated Chemo (4 cycles of hyper-CVAD, 1 week in hospital, 3 weeks off)
The protocol for the first part of treatment was the ibrutinib pills. I took 4 of those every day. It is a blood thinner. Then I took the rituximab. I had my first infusion on a Monday. I had them 4 consecutive Mondays.
Issue with low heart rate
Because I started running, my heart rate had gotten fairly low. It was averaging somewhere between 47 to 48 beats per minute, which was a side effect from the running.
The protocol for the treatment was that if your heart rate was in the 40s, you couldn’t take it.
Since I’d get those results from exercise, the doctor felt it wasn’t going to be an issue. But everytime we would visit the doctor, they would have to call him before the treatment started because they would not mix it until he gave me approval with my heart rate under 50.
That was a little bit of a drag because usually we wouldn’t get there till 4 p.m. or 4:30 p.m. to take the treatment. It lasted anywhere between 4 and 6 hours. Then we’d have a 6-hour drive back home.
How did you pass the time for the rituximab infusions?
Fortunately, for me, they would inject Benadryl into the IV before they gave me the treatment, and it’d just knock me out. I’d go right to sleep. As soon as I took it, lights were out.
I actually slept for about 4 to 5 hours, which was about the length of time of the treatment. When the nurse came in to take the needle out, she goes, “You’re free to go home!” I was ready to go.
Did you need a caregiver at the infusions?
I drove myself, but my wife went with me every time. The first treatment I had, they gave me the rituximab really slowly because they didn’t know how I’d react to it.
After about 4 hours, I woke up and got a little restless, so I started walking the floor. When I came back, my wife was in my bed.
Then I had to sit in the chair the rest of the time. You move, you lose!
What were the ibrutinib and rituximab side effects?
The only side effect that I had didn’t happen until my July treatment. I broke out in a pretty serious rash that lasted for about 2 days, and then it went away and never came back after the other treatments.
I did not have any side effects from anything. It was strange that I did continue to run all summer, and I ran my fastest 10k, 5k. Times I’ve never run before!
All the time I was taking the pills and going through treatments, so basically, they did not affect me at all.
»MORE: Read more about ibrutinib and other patient experiences
How did you learn there was no evidence of disease (NED)?
During 2016, I had 4 colonoscopies because even though my colonoscopy in December 2015 was clear, it was clear because they were polyps. When I had my colonoscopy done in Houston, they took biopsies, and the cancer was prevalent in my colon.
Unfortunately for me, because of the prep you have to go through for the colonoscopies, it was the last place that the cancer showed up. I had a colonoscopy in November 2016, and it was clear. It had already been clear everywhere else, so the colon was the last place where they found the cancer. It was now gone.
The doctor then said it was time to go to the next stage of the clinical trial, so I went from Phase 1 to Phase 2.
Describe getting the port placed
I had 2 options: the PICC line or the port. I didn’t want the PICC line. We’d visited a gentleman who had a PICC line during his third treatment.
Having to go through all the maintenance of keeping it flushed, and it was always there, even if you could tape it and put it under your shirt… I decided I didn’t want any part of that.
We opted for the port. For the procedure, they put me to sleep, although I do believe I woke up during the procedure. I didn’t feel anything, but because it was on December 1st, the doctor was singing Christmas carols.
I asked one of the nurses, and she said, “Yes, he was singing carols.” I was sort of coming out of it as he was finishing up, but there was not a lot to it.
You started the chemo (Phase 2) right after the port placement
They went ahead and accessed the port while I was there. I had it put in my left side because they said it would be better for me as a right-handed person.
I stayed in the hospital for a full week. I was taking the treatment the whole time, every day. They told me how many bags that I would get from each of the medications. It was a different drug each day.
Describe the prep before the Hyper CVAD chemo
The first day we went to the medical center and had the port placed, then we had to go to the actual hospital and wait there. We went to the room, and the nurse came in and explained what I was getting ready to take.
The nurse explained the medications they’d give me for nausea. They started the treatment. I’d taken my laptop with me. This was on a Friday, and I was answering emails.
I was on the phone, probably more so to get my mind off it than I was trying to be a hero and say I was working through my treatments.
Friday, after close of business around 4 o’clock, they indicated to me that I needed to make sure to walk every day. They were going to give me a shot in my stomach to make sure the blood flow remained adequate.
My wife and I walked the first day about 3 miles all around the complex. The next day, we walked about 2 miles.
Sunday, we got up and went to the chapel. The alarm for my pump went off because one of my lines got kinked, so we returned to the room to get the alarm silenced.
It just hit me all at one time. It was like somebody flipped the switch. I went from being fairly active, walking around, to just basically being dead.
Self-motivation to move around as much as possible
On the hospital floor, for every time you lapped, you could stop at the nurse’s station, and they’d give you a sticker. I figured out how many stickers it would take to make a Christmas tree for my door, and I made all the laps I needed.

How many days did you get off between the 1-week cycles inpatient?
21 days. We would go September 1st, and the next time I went into the hospital was September 28th. Then it was a week in the hospital, and then 21 days at home.
I did have a small window where it didn’t have to be exactly 21 days. I think my last treatment I was outside that cycle by maybe a day or 2.
The anti-nausea cocktail caused depression
The worst side effect from the nausea medicines was it basically put me in a depression. I lay in bed, did not want to get up. There were 3 different medications they gave me. I’m not sure what the 3 were, but it caused me to go into depression.
I never understood why people ‘give up,’ why they don’t want to take any more treatments or want to check out. I understand that now.
Even though I’m not a depressed person, the medication said, “I really don’t care anymore.” I didn’t care to get up, I didn’t care to get out of bed, and I didn’t care to walk. I was just like, “Leave me alone.”
We have a friend who came in who wanted to come up and see me. I had to tell my wife that I didn’t want to see anybody. I asked her to tell them sorry. I didn’t talk to my children on the phone. Nothing. I was very depressed.

Also couldn’t drive after first nausea medication dose
After my first treatment was over, it was the only time I did not drive there. When we got in the car, I was still pretty much comatose from the nausea medicine. They had to pretty much carry me out. I got in the car, put the seat back and told my wife to take me home.
She didn’t know how to drive home because she had never driven home from there before. I had to get us out of the city, and from there I went to sleep.
By the time we got home, the medicine had actually started to wear off, and I was pretty much back to normal the next day.
You asked to stop taking the anti-nausea cocktail
They just called it a cocktail, and it was 3 different anti-nausea medicines. In Cycles 2, 3 and 4, I did not take the anti-nausea cocktail. I believe I took some Ativan.
The main thing is that I got physically sicker, but I took that sickness over the depression.
Only in the first cycle of the chemo treatments did I ever get to that point. The rest of the time, I just said, “Okay, I’ll get sick.”
I got sick, then slept, got sick, then slept. But for me, it was better. I was more active. I was walking more. Even though the treatments were supposedly hitting harder, it helped me not have to take the anti-nausea cocktail.
Even though it was supposed to help me, mentally it was something I didn’t want. I drove home after the last 3 treatments as well. That was a difference for me.
Any side effects from the hyper-CVAD chemo?
There were the normal things you get taking this type of chemotherapy, like losing your appetite. The whole time they were telling me to eat something, I was like, “What’s the point?” I would eat it and then get sick.
And the food was great! The first two days I was actually able to eat something, I got to order off of a menu that was different for patients. Starting Sunday into Monday and Tuesday, there was no appetite at all. I didn’t want anything. Food was the furthest thing on my mind.
Describe the hair loss
I have a pretty full head of hair for being 61 years old. I was in the shower. The doctors said if my hair was going to fall out, it was going to take about 2 weeks from when I got home to start.
I was washing my hair every day, and nothing was changing. I was going along and thought since I had gone through Phase 1 with no issues, I would go through Phase 2 with no issues as well.
About the 14th day from when we got home, I was in the shower washing my hair. After rinsing it out, when I opened my eyes, I noticed there was quite a bit of hair in the tub. Not only was it there, it was everywhere.
Don’t mean to get too graphic, but it took me about 30 minutes to clean up the shower. After I thought I had beaten it, the fact that it happened, I was just disappointed.
I really wasn’t traumatized by it. I didn’t know what I was going to look like with no hair.
»MORE: Dealing with hair loss during cancer treatment
How did you end the chemo treatment?
I asked the doctor when I was told I was in remission why I had to go through this maintenance ordeal with all the harsh chemotherapy. He said, “A cell is very small.”
He said he could not guarantee, even though the PET scan was clear and the colonoscopy was clear, that there was not a cell or 2 floating around.
He said the chemotherapy would take care of it, so I said okay.
Video: Bobby Being Part of a Clinical Trial
Being Part of a Clinical Trial
Describe the clinical trial
The combination of the rituximab and ibrutinib pills was the first phase. The trial I was in, there were about 150 people altogether. I got a chance to meet the first person to be in the trial. That treatment regimen was a clinical trial also because of the second phase.
My normal treatment for the hyper-CVAD chemotherapy would be 6 weeks. I only had to do 4.
How did you discover the clinical trial?
I’m leaning very much on my wife in this situation. She actually heard about the clinical trial before we went down to MD Anderson. She was very much an advocate for me to get in the trial.
We thought we were going to be on the outside because they had only taken so many patients. By the time we got there, they actually expanded the trial, so I was in the expansion part of the clinical trial. I think they had limited it to about 100 patients at first. I was like number 140 or so.
They added 50 more spots, so I barely got in. It was something we wanted to do. I felt very positive about it.
Describe your impression of your oncologist
When I got there, the doctor I got assigned to was Dr. Wang, who is a superb doctor.
The first day we ever met him, he walked in and said however long it would take for us to be there, we should ask any questions we have, and that he’d be there until we were ready to go.
Just a super human being. Orlando was my first nurse, and the physician’s assistant — they were a wonderful team.
What was the prep like getting into the clinical trial?
Because of the way the trial was set up, the ibrutinib tablets that I took during the trial were at no cost. The pharmaceutical company supplied those as part of the clinical trial.
We would have to go to the pharmacy there at the hospital to get the pills. We had to keep a log of when I took the pills, my temperature and some other things.
When we went back to the clinic, they would take the bottle of pills, count all the pills I had left, and make sure that everything was accounted for in terms of the number of days I took them and how many pills were left over.
You couldn’t take other medications during the trial
There was a part of the trial where I got a sinus infection during the trial part, which I’m very susceptible to getting. I could take no medication for that. If my fever got above 100 degrees, I would have to go to the hospital. It got to 99.9. Just barely got under the wire there.
I couldn’t take anything for the infection because any medications I took during the trial period may have affected it. There were some medicines I would normally take that I couldn’t take during the trial.
Everything was very regimented.

What would have happened if your fever had passed 100?
They would have just gone in and made me stay there if my temperature had gone above 100. It would have been something they would have just watched.
It wasn’t life-threatening or anything like that. I just couldn’t take anything for it, so it would have had to run its cycle without medication.
What made you and your wife so sure about the clinical trial?
Knowing I wouldn’t have to take as many rounds of chemotherapy, and the trial had a very good success rate. We were told that chemotherapy, in and of itself, may cause cancers later in life.
One of the reasons they wanted to back off the 6 treatments to 4 treatments was to make sure the side effects years from now wouldn’t lead to another cancer from the chemo.
We felt very strongly going the route of clinical trial was the way to go. The success rates of the people who’d already been in it were really high, so we felt very positive about it.
Describe meeting the first person to go through the clinical trial
We were there for a check-up, and he was there for his check-up. My wife had created a Facebook page just for mantle cell lymphoma patients at that hospital. He had joined that group.
Every time we’d ever go to the hospital, we’d let the group know we’d be down there in case they wanted to meet. Today with COVID-19, it’s more difficult.
He was in the waiting room to go in, and it was pretty unique to see the first guy in the trial. He had probably started the trial about 6 months before me.
He looked fine, and it’s always encouraging to see somebody who’s gone through the entire process. There was a gentleman who actually called me and wanted to talk to me about my experience. When I finished talking to him, he said that if I did it, he could do it.
It’s always encouraging to see somebody who’s gone through it. You can survive. It’s just a matter of knowing that it’s a brief part of your life.
If you had been Patient #1, would you have still done the clinical trial?
If I would have been the first patient, I would have done the same thing. Just the fact that you’re with people who are very smart, you just have to trust your doctors.
Was the monitoring any different in the trial?
I think only because we were going back so frequently. We had to go back every month to get the pills refilled. We did have a journal. Every day we had to write down pills were taken. We didn’t skip any pills.
Ibrutinib is a blood thinner, so I had to skip every time I had a colonoscopy. They would not be able to take the biopsy if I was on the ibrutinib, so I stopped taking the pills 3 to 4 days prior to the colonoscopy and 3 to 4 days after.
It was all part of the protocol, so it was built into the trial, and the medical teams always knew that. It scared me, because the pills are very expensive, that I would drop or lose one. We kept up with the pills and with the journal.
What did you have to include in the journal?
There was not really any feeling documented, but I wrote down any side effects I had.
Going through the trial, I think I was the only patient I know of who didn’t have to take any platelets (get blood transfusions), never missed work other than the treatment days when I was in the hospital, actually ran during the end of the second phase of the trial, able to exercise, and pretty much normal during the whole trial.
Donating your tissue and blood samples to research
Going through the trial as a patient, I allowed the hospital to take extra blood samples and extra tissue samples from me, anything they needed from me that was “extra.”
I felt like there were people who’d gone through this before me who did that, and because I was at a research hospital, the more they had, the better it would be.
Hopefully, whatever I left for them to do their research on will help somebody behind me now. I’d encourage anyone going through this, if they’re asked, to also allow that. You’re already stuck in a lot of cases, so what’s one more vial of blood?
What’s the follow-up?
After I finished the trial, my last day of treatment was March 3, 2017. We went back to see Dr. Wang at the end of March, just as a follow-up visit. The check-ups are seeing the doctor and a PET scan.
He would check me and say, ‘Enjoy your life!’
My first 2 years of remission, we went every 4 months, and then my second 2 years, every 6 months.
My last 6-month treatment will be in May of 2021. I’ve already been told that if I’m clear, I’ll start going once a year.

Did you have to deal with insurance for the clinical trial?
At the clinic and the hospital, there’s an advocate there for you, as well as a dietitian. When we first went, the advocate we spoke with about insurance knew everything and had things squared away. My insurance company was fabulous. I have no complaints with my insurance carrier (Blue Cross and Blue Shield of Louisiana).
Never had a hiccup. Never got any denials. They were just absolutely wonderful. I appreciate all that they did during that time. It was a load that was taken off of me.
Video: Bobby’s Reflections
Quality of Life Reflections
Taking health issues more seriously
Going on a trip to Yellowstone was something I wanted to do, so we decided to go there as a family vacation after Phase 1.
When my wife was looking at pictures, she noticed some slightly gray areas where the skin had gotten a bit discolored. She said it didn’t look right, and so we asked our doctor about it. He sent me to a dermatologist.
They did a small biopsy, a little scrape, and it came back as melanoma. It was stage zero. I look at it as somebody my age, where the skin is supposed to change anyway.
Had I not been at the hospital and gone through this process, I would have never have known it. I would have just said, ‘I’m just getting old, and that’s just a spot that old people get.’ I wouldn’t have gone to the dermatologist.

What support got you through cancer treatment?
My family. I had a brother who’d gone through radiation and chemotherapy a few years before I did. He would offer me advice.
People from our church who’d gone through cancer. My family was incredible in the support they gave me.
My work, I can’t thank them enough, including my superintendent (of schools), who called me and said whatever they needed to do, they’d be there for me.
The support not only at home but at work, where I spend every day it seems like, was just incredible. I’m so blessed with that.
My wonderful wife, who stood by me the whole time. Made me take my pills. Made me get to my appointments on time. An incredible woman. I’m so blessed to have her.
How did the diagnosis impact your relationship with your adult children?
They’ve always known Dad to be a pretty strong guy, and I got that from my dad. He was a World War II veteran. He told me not to give up. He told me to always keep trying in life.
My adult children were used to seeing Dad strong. They were there for me. My daughter lives outside of Nashville and my son’s in Brooklyn, but they always knew the right time to call.
They checked on me, how I was doing, told me they loved me, and reminded me to keep going. They were there for me.
I finished my treatment March 3rd, and we returned to the race where it all began. This time, all 3 of us — my son, daughter, and I — ran.
We had a great day. I spent time with them. I have 2 grandchildren from my daughter, and so we got to spend some time with them there.

The importance of taking care of mental health
I am very much faith-based. I have a very strong belief. That peace that I got during this whole experience was through my faith and my beliefs. That part is really what got me through it.
It’s all well and good to have this huge support group around you, but you still have to do the work. It’s you who has to get through it. I don’t know what I would have done had I not had that to lean on.
I’ve always told people this: I have a blessing and a curse. I have a curse because I got cancer. I had a cancer that’s supposedly incurable. I do believe that I have been cured. I don’t believe it’s ever going to come back.

How has cancer changed your life perspective?
I can’t tell you the blessings that I’ve received that I would not have received had I never been diagnosed with cancer. I know that’s probably the weirdest, oddest thing that anybody would say, but from my shoes, I don’t think I would change anything in terms of what happened.
It has brought me and my family closer together, it has helped me from a faith perspective, and there are so many people I’ve met whom I would have never met.
I don’t think I would change anything. I know that’s probably an odd thing to say.
There are plenty of bad memories, like lying in the hospital bed and losing my hair. I had people tell me that I didn’t look bad bald-headed, and I would look in the mirror and think I was a strange-looking person!
I figured out one day why I’d looked so strange. My eyebrows had fallen out. Even though my head has a good shape to it and I probably didn’t look weird bald-headed, the weird person staring back at me from the mirror with no eyebrows looked alien.
Now I’m back to normal. I just have to give God praises for letting me be here on the anniversary of my first day of chemotherapy.

Inspired by Bobby's story?
Share your story, too!
Mantle Cell Lymphoma (MCL) Stories
Tim H., Mantle Cell Lymphoma (MCL), Stage 3/2
1st Symptoms: Lump on left-side of neck that grew bigger over a couple years, new lump on right side
Treatment: 6 cycles Nordic chemo protocol, alternating cycles of R-CHOP and rituximab + high-dose cytarabine, autologous stem cell transplant
Sheryl B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: (Over 15 years) Skin irritation from temperature changes, rising WBC levels, unexplained fatigue, retinal hemorrhage, hardened abdomen (from enlarged spleen)
Treatment: 6 cycles Hyper-CVAD chemotherapy
Shari B., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: None, lymphoma discovered at unrelated doctor appointment
Treatment: 6 cycles R-CHOP, 5 cycles Phase 3 trial of Velcade + Rituxan (normally for multiple myeloma), allogeneic bone marrow transplant (BMT)
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Fatigue, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Hives, inflamed arms
Treatment: Calabrutinib, Lenalidomide, Rituxan
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: Elevated white blood cell count
Treatment: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
1st Symptoms: No symptoms
Treatment: R-CHOP chemotherapy, rituximab





