Non-Hodgkin Lymphoma Overview
Below we feature some of the basic background of non-Hodgkin lymphoma, including common symptoms, diagnostic and staging tests, as well as treatment.
Diagnosis
What is non-Hodgkin lymphoma?
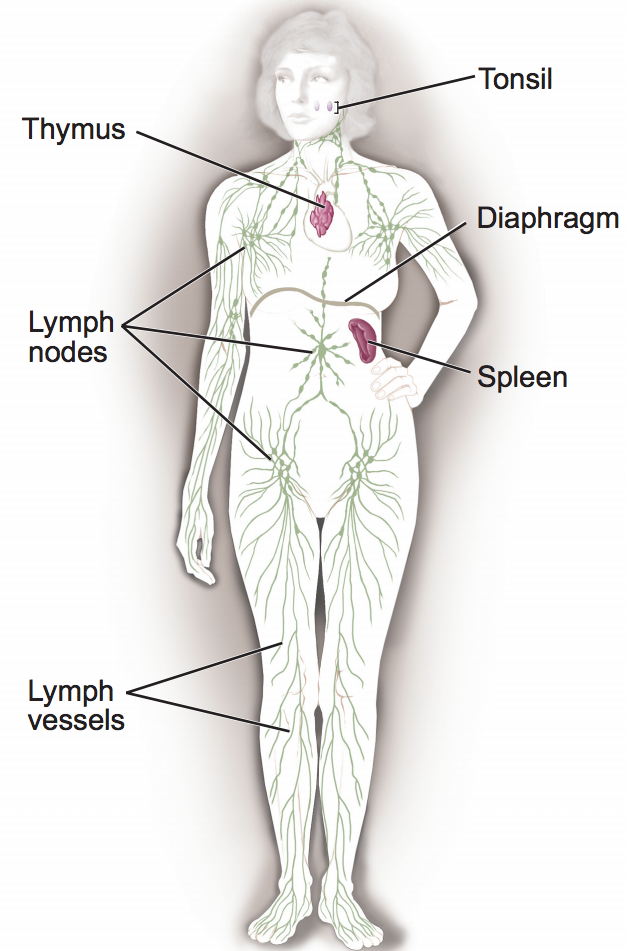
Non-Hodgkin’s Lymphoma is a cancer that develops in the body’s lymphatic system, which is part of our immune system. It’s one of two main types of lymphoma (the other is Hodgkin’s lymphoma).
- Lymphatic system: network of lymph vessels (also covers thymus, tonsils, spleen, stomach, small intestine, skin)
- Lymph: clear fluid that carries white blood cells, particularly lymphocytes like your B-cells and T-cells
- Lymph vessels: these cover all tissues of our body
- Lymph nodes: store white blood cells; filter out and remove foreign cells and organisms, get rid of waste products and fluids from the body (usually in neck, chest, underarms, chest, and groin)
- Lymphocytes: one type of white blood cell geared toward fighting infections started by viruses, bacteria, or fungi
Lymphoma happens when the lymphocytes start to multiply out-of-control. This usually means that lymphoma can start essentially anywhere but typically is found first in a lymph node (swollen). That indicates that your lymphatic system is fighting an infection.
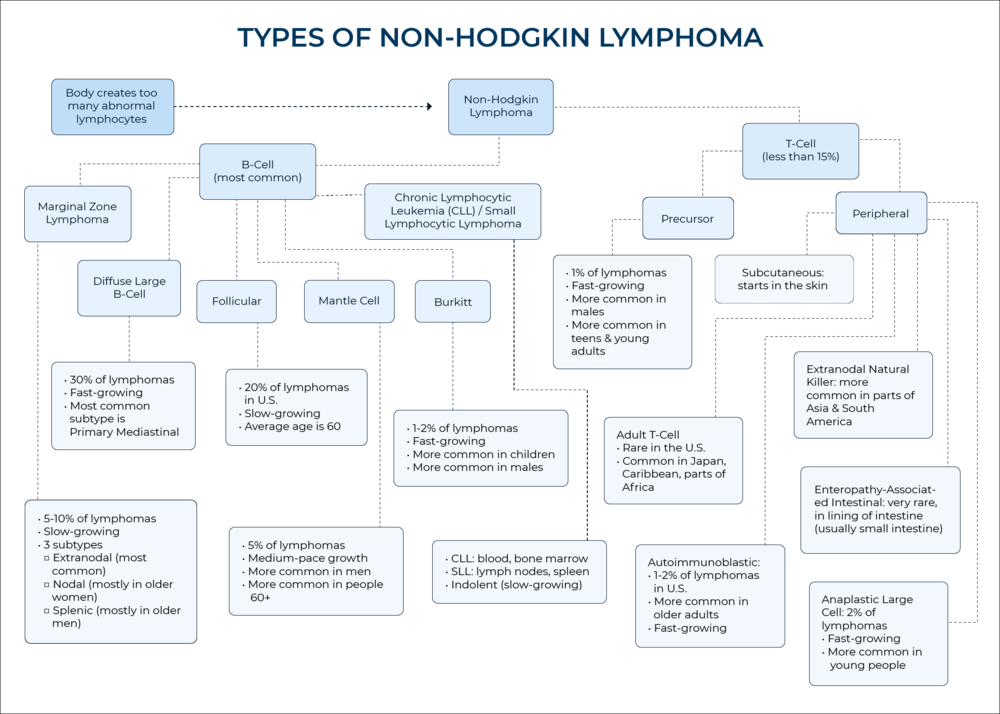
Non-Hodgkin’s lymphoma types & subtypes
Here is a chart to give a general picture of the different types of non-Hodgkin lymphoma and subtypes.
Of these, the largest subtype of non-Hodgkin lymphoma is diffuse large B-cell lymphoma (DLBCL) which tends to grow quickly.
What are the most common symptoms?
Note: these are the most common symptoms of Non-Hodgkin Lymphoma, but there will be differences person to person. These may also be caused by many other reasons other than cancer, especially if they’re short-lived.
- Swollen, painless lymph nodes (neck, armpits, or groin)
- Unexplained weight loss
- Fever
- Soaking night sweats
- Coughing
- Trouble breathing
- Chest pain
- Weakness and tiredness that don’t go away
- Pain, swelling, or a feeling of fullness in the abdomen
*Source: National Institutes of Health
What tests do I have to undergo pre-diagnosis?
This can also range depending on where you are and/or what doctor you go to. Here are some general guidelines.
- Physical Exam: The first step is usually having a doctor check for swollen lymph nodes in your neck, underarms, and groin. The doctor will usually also feel around for a swollen spleen or liver.
- Blood tests: If the doctor suspects swollen lymph nodes or wants to be extremely thorough even without them, s/he may order blood tests in the lab. Unless your doctor’s office has a lab on-site, this will mean going to another location to draw and test the blood. The lab is checking for the number of white blood cells, an indicator of lymphoma. It would also check for other substances like lactate dehydrogenase (LDH) which tends to be high when lymphoma is present.
- Chest x-rays: A doctor will order this to see whether there are swollen lymph nodes and/or other signs of disesase.
- Biopsy: This usually requires surgery and is the most surefire way of diagnosing lymphoma. There are different kinds.
- Excisional: removing the entire lymph node; usually involves general anesthesia (going under), performed by Ear Nose Throat surgeon
- Incisional: removing part of a lymph node; usually involves general anesthesia (going under), performed by Ear Nose Throat surgeon
- Fine Needle Aspiration: getting a small sample of the lymph node; usually involves local anesthesia, performed by doctor
What tests do I have to undergo for staging?
Your doctor needs to know the extent (stage) of nonHodgkin lymphoma to plan the best treatment. Staging is a careful attempt to find out what parts of the body are affected by the disease. Lymphoma usually starts in a lymph node. It can spread to nearly any other part of the body. For example, it can spread to the liver, lungs, bone, and bone marrow.
Staging may involve some of these tests:
- Bone marrow biopsy: The doctor uses a thick needle to remove a small sample of bone and bone marrow from your hipbone or another large bone. Local anesthesia can help control pain. A pathologist looks for lymphoma cells in the sample.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your head, neck, chest, abdomen, or pelvis. You may receive an injection of contrast material. Also, you may be asked to drink another type of contrast material. The contrast material makes it easier for the doctor to see swollen lymph nodes and other abnormal areas on the x-ray.
What are the different types?
There are main ways of categorizing types of Non-Hodgkin Lymphoma:
- Origin of the cancer
- B-Cell is most common, making up around 85% of all Non-Hodgkin Lymphoma cases in the U.S.
- T-Cell makes up less than 15% of the rest of cases in the U.S.
- Pace of growth
- Indolent (low-grade) lymphomas grow slowly. They tend to cause few symptoms.
- Aggressive (also called intermediate-grade and high-grade) lymphomas grow and spread more quickly. They tend to cause severe symptoms. Over time, many indolent lymphomas become aggressive lymphomas.
(Check chart at top of page for complete visual.)
How common is non-Hodgkin lymphoma?
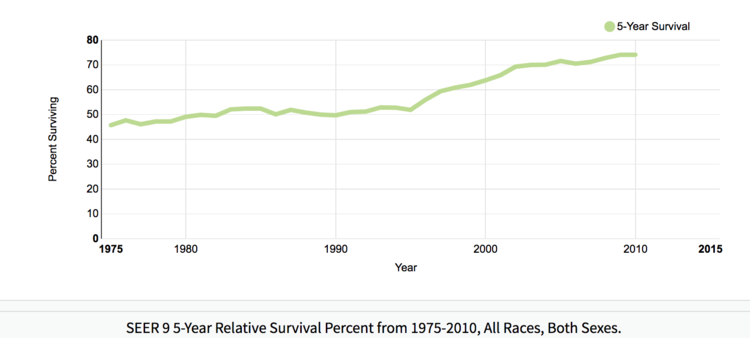
Non-Hodgkin lymphoma makes up an estimated 4.3% of all new cancer cases in the U.S. According to the same data, the number of people dying from NHL is going down while the five-year survival rate has been on the rise since 1975.
YEAR 5-YEAR SURVIVAL RATE (%)
1975 45.7
1980 49.1
1985 52.4
1990 49.7
1995 51.9
2000 63.8
2005 71.6
2010 74.1
*National Cancer Institute
Treatment
What is the standard treatment?
According to the National Cancer Institute, there are nine different kinds of standard treatment used for non-Hodgkin’s lymphoma, including:
- Radiation therapy
- Chemotherapy
- Immunotherapy
- Targeted therapy
- Plasmapheresis
- Watchful waiting
- Antibiotic therapy
- Surgery
- Stem cell transplant
There are also promising new developments in clinical trials and CAR T-cell therapies, especially for refractory/relapsed non-Hodgkin’s lymphoma.
What is a PICC line?
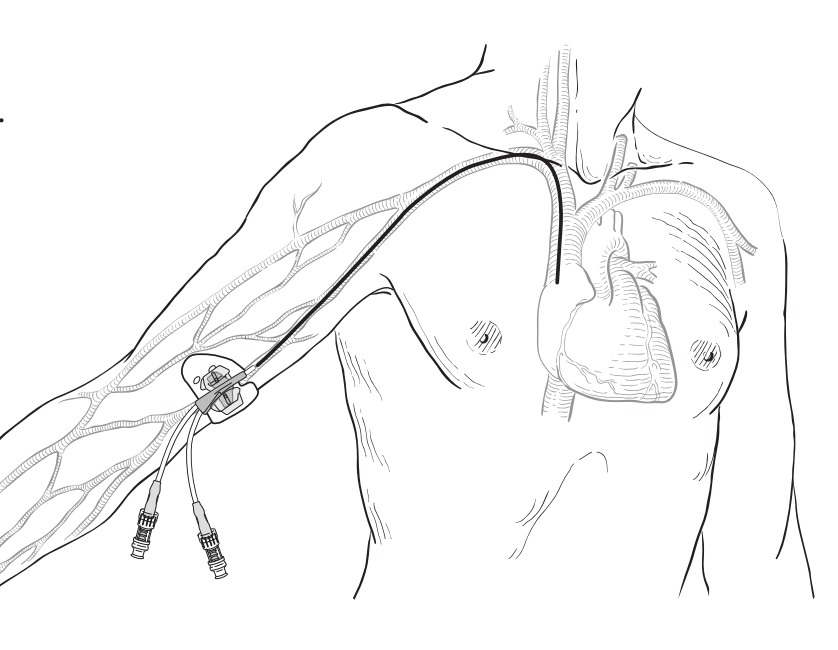
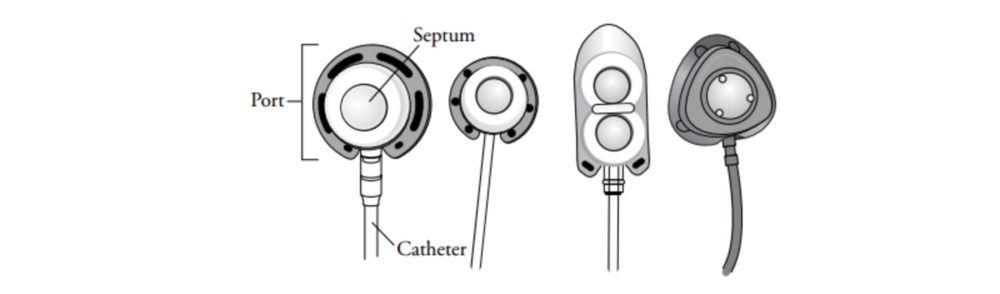
What is a port?
- A port is like an artificial vein that will allow your healthcare team to give you continuous chemo for multiple days. It can also:
- draw blood for tests
- give you intravenous (IV) medication
- give you IV fluids
- It’s about the size of a quarter with varying shapes. It is most commonly called a Port-A-Cath®, PowerPort®, BardPort®, or a Mediport®.
- This can be done outpatient in a hospital’s interventional radiology department
- Usually requires more anesthesia so you can sleep through the procedure.
- Total surgery time: under 1 hour
“The port is usually placed about an inch below the center of your right collarbone (see Figure 2). If you wear a bra, the port will usually be about 1 inch from where your bra strap lies.” – Memorial Sloan Kettering Cancer Center

“Your port may raise your skin about ½ inch above normal. You will most likely be able to feel it through your skin. It will probably not be seen when you wear a V-neck sweater. Most people will not know that you have a port. Implanted ports can stay in place for years. Once you no longer need the port, it will be removed.” -Memorial Sloan Kettering Cancer Center
Patient Events
DLBCL Patient Events
Non-Hodgkin Lymphoma Patient Stories
B-Cell Stories
Burkitt Lymphoma
Ashlee K., Burkitt Lymphoma, Stage 4
Symptoms: Abdominal pain, night sweats, visible mass in the abdomen
Treatments: Surgery (partial colectomy to removed 14 inches of intestine), chemotherapy
Emily S., Burkitt Non-Hodgkin Lymphoma, Stage 4
Symptoms: Constant fatigue, tongue deviated to the left, abscess in right breast, petechiae on legs, night sweats, nausea and vomiting, persistent cough
Treatments: Chemotherapy, stem cell transplant, immunotherapy
Erin R., Diffuse Large B-Cell Lymphoma (DLBCL) & Burkitt Lymphoma, Stage 4
Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatments: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
Diffuse Large b-cell lymphoma (dlbcl)
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy
Nolan W., T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL), Stage 4
Symptoms: Debilitating fatigue, flu-like symptoms without a fever, swollen lymph node under the left arm
Treatments: Chemotherapy (R-EPOCH & RICE), bone marrow transplant
mantle cell lymphoma (mcl)
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: None
Treatments: R-CHOP chemotherapy, rituximab
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: Elevated white blood cell count
Treatments: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Hives, inflamed arms
Treatments: Calabrutinib, Lenalidomide, Rituxan
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Fatigue, enlarged lymph nodes
Treatments: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
marginal zone lymphoma (mzl)
The Importance of Positive Role Models
The example that Nick's father set for him as he was growing up taught him how to prioritize and advocate for his health.
Nick M., Nodal Marginal Zone Lymphoma
Symptoms: Daily hives, GI issues, weight loss, heart issues, night sweats
Treatments: Rituxan (rituximab), high-dose steroids
Kimberly O., Marginal Zone Lymphoma
Symptoms: None at first, routine blood work showed suspicious results, bad nosebleed
Treatment: Chemotherapy (bendamustine & rituximab)
Rachel P., Marginal Zone Lymphoma, Gastric MALT
Symptoms: Fatigue, bloating, stomach pain
Treatments: Chemotherapy, targeted therapy, surgery
primary mediastinal b-cell lymphoma (pmbcl)
Lauren D., Primary Mediastinal (PMBCL)
Symptoms: Dry cough, extreme fatigue, trouble breathing, swollen and discolored left arm, lump under the arm
Treatment: Chemotherapy
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough; low-grade fever; night sweats
Treatments: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.
small lymphocytic lymphoma/chronic lymphocytic leukemia (sll/cll)
Nadia K., Small Lymphocytic Lymphoma (SLL)
Symptoms: Rash, lump under arm, fatigue
Treatments: Ibrutinib and acalabrutinib
waldenstrom Macroglobulinemia
...
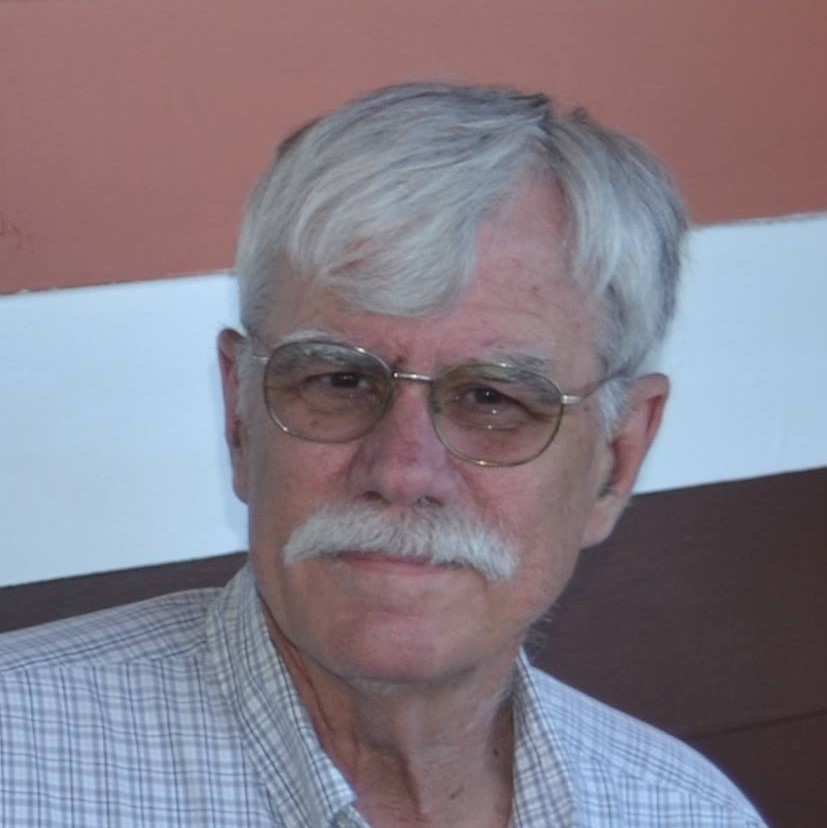
Pete D., Waldenstrom Macroglobulinemia
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
...
Sheree N., Waldenstrom Macroglobulinemia
Symptom: Feeling anemic
Treatment: Chemotherapy (bendamustine & rituximab)
...
*A lot of information on this page came from the National Cancer Institute, under the U.S. Department of Health and Human Services.