Ivy’s Stage 4 EGFR+ Adenocarcinoma Non-Small Cell Lung Cancer Story
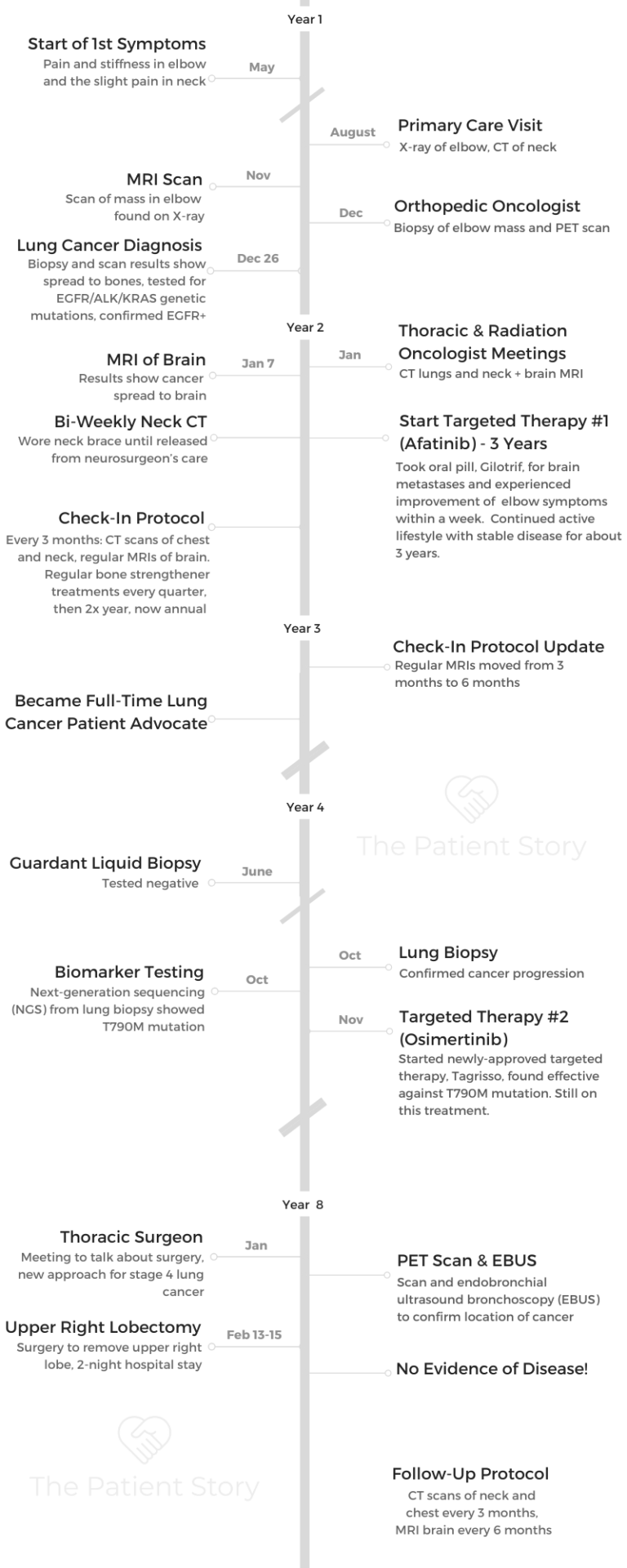
Ivy shares her stage 4 EGFR+ lung cancer story, one that started at just age 47 with a lot of misdiagnoses. She details going through 2 targeted therapies, afatinib and osimertinib, and surgery, a new approach for a stage 4 diagnosis.
The mom, wife, and patient advocate also describes how she approaches life after a stage 4 lung cancer diagnosis, including topics like managing the cancer like a chronic illness, tending to mental health, navigating marriage and parenting with cancer, and her lung cancer patient advocacy work, including co-founding the group EGFR Resisters.

- Name: Ivy Elkins
- Diagnosis (DX)
- Lung Cancer
- Stage 4 (metastatic)
- EGFR+ (epidermal growth factor receptor)
- Age at DX: 47
- Treatment
- First-line treatment
- Targeted therapy #1: afatinib (Gilotrif)
- 3 years
- Second-line treatment
- Targeted therapy #2: osimertinib (ongoing)
- Surgery
- First-line treatment
I have gotten very involved in advocacy and am knowledgeable about the research and trials and treatments that are coming along. That also helped me feel a little bit better about things as they’ve progressed.
There are a lot of good options out there, and more are being developed. That has helped me a bit, too. I try to focus more on living each day and what I can accomplish that day, as opposed to worrying tons about the future.
Ivy E.
- Ivy's Story on Video
- First Symptoms
- Getting Diagnosed
- How did you start getting answers?
- Describe the orthopedic oncologist visit
- Describe the elbow biopsy
- Did you experience anxiety waiting for results?
- What were the results of the scans?
- Recall the moment of the diagnosis
- Did you break the news to loved ones?
- Describe the actual PET scan
- Thrust into a whole new world, overwhelmed by new terminology
- Do you recall when you got the full diagnosis?
- How did you process the stage 4 lung cancer diagnosis?
- Genomic testing for biomarkers
- Treatment plan: targeted therapy
- Did you consider a second opinion?
- Treatment Decisions
- First-Line Treatment: Targeted Therapy, Afatinib
- Second-Line Treatment: Targeted Therapy (Osimertinib)
- Surgery (Lobectomy)
- Navigating Life with Cancer
- Your Work in Patient Advocacy
- How did that community relationship-building shift into advocacy?
- Talk about the patient group you co-founded: EGFR Resisters
- You’re proof of the importance of advocacy and pushing for better treatments
- Top issue #1 in lung cancer research: resistance to treatment
- Top issue #2 in lung cancer research: precision medicine
- More attention now on rarer types of lung cancer
- Final message to other patients and caregivers
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Ivy’s Story on Video
Video #1: First Symptoms & Getting Diagnosed
Video #2: Describing Treatment
Video #3: Navigating Life with Cancer & Patient Advocacy
First Symptoms
First, tell us a bit about yourself
I live in the suburbs of Chicago, northwest of the city, with my husband. In about a month and a half, he and I will be celebrating 25 years of marriage.
I have 2 boys. One of my sons is 20 years old and is a sophomore in college. My other son is 18 and is a senior in high school right now.

How did you know something was wrong?
Around the middle of 2013, I just started having some issues with my right elbow. I couldn’t completely straighten it, and it hurt a little bit. The left side of my neck also was bothering me a bit. Initially, I didn’t think anything of it, but it didn’t go away.
I went to see my primary care physician. He took a look at me and said I was 47 years old and thought it might be my computer and iPad usage. He thought it was an overuse injury.
To be honest, I just completely agreed with him because it seemed that made sense. I had been active, healthy, and never really had any problems.
He sent me to physical therapy and did all the right initial things. He had an X-ray done of my elbow, which showed absolutely nothing wrong, and an MRI done of my neck, which showed nothing other than the typical deterioration that comes with being a little bit older.
You went to a lot of appointments
For about 6 months, I went from physical therapy to visiting an orthopedist, getting a cortisone shot in my elbow, seeing a rheumatologist, and seeing multiple physical therapists.
No one could really figure out why my elbow, which they had deemed tennis elbow at this point, wasn’t responding to any of this treatment. My neck, oddly enough, started to feel better, but my elbow didn’t.
How did you mentally manage the search for answers?
I was actually getting kind of frustrated because I was being really good at following everyone’s recommendation for the next doctor. I was doing all of my physical therapy exercises, getting my cortisone shot, and following up, but nothing was improving.
On the other hand, there was a little piece of me that kept thinking, ‘Do I keep pushing forward?’
My husband and I talked about it. He talked about the problems with his knee and that that was “his thing” now. He suggested maybe this was my thing for getting older, that this would be my “weak spot.”
Part of me was wondering how far I’d keep going in terms of going to doctors and trying to figure things out, but it just all seemed odd. The whole elbow issue kept getting worse, not better. I got to the point where just putting my hands up to wash the back of my hair hurt.
I was 47 years old, and it just didn’t seem right. I kept going and was determined to figure out what was going on. It took a good 6 months!

Getting Diagnosed
How did you start getting answers?
Eventually, I ended up at an orthopedist who specializes in the wrist to the shoulder. He did an MRI of my elbow because he was trying to figure out what was going on.
He saw there was a mass in there that was on the joint and looked like it had eaten away a little bit of the bone in the area. He didn’t really know what to make of it, so he sent me to an orthopedic oncologist.
Describe the orthopedic oncologist visit
When I went to the orthopedic oncologist, I was already terrified because the word “oncologist” is in the name. I went with all my various reports.
When I first saw him, he thought I looked healthy and was in good shape. He said to me that if I presented differently, he would think that this was a metastasis possibly from somewhere else.
But he said he was really 90 to 95% sure that this was a benign condition called a giant cell growth. He said he’d do a biopsy. No rush to get that scheduled. They’d go in and take a look at it.
If that’s what it was, they’d take it out, and I’d be good to go. All that happened, but it wasn’t benign.
Describe the elbow biopsy
The biopsy wasn’t bad. They didn’t put me under general anesthesia. They gave me a twilight drug, so while I was awake, I wasn’t really too concerned about anything going on.
The actual procedure was quick. I remember having to put my arm in a certain position and hold it there. They took the cells that they needed, and after a brief recovery, I just went home. It wasn’t particularly painful afterwards, and it wasn’t something that I felt was particularly traumatic.
Did you experience anxiety waiting for results?
I was pretty nervous after I had the elbow biopsy. Even though my oncologist had said he was pretty sure that it wasn’t going to be anything, I was still nervous. It took a good amount of time before I had results back, a couple of weeks or so.
The thing that complicated everything a little bit was that I was having all of this done in between Thanksgiving and the winter holidays, so things slowed down.
It was hard to get in touch with people. I was preparing for the holidays myself, with 2 kids who were going to be home and out of school. It was a really, really stressful time.
»MORE: Patients describe dealing with scanxiety and waiting for results
What were the results of the scans?
The results came back from scans that the mass was malignant. It came back as adenocarcinoma, which doesn’t originate in the bone. They knew at that point that the cancer I had came from another part of my body.
I remember asking the orthopedic oncologist where adenocarcinoma came from. He said either the lungs or the breast.
Initially, I was convinced that I had breast cancer. I had no idea that lung cancer was something I could get. I didn’t know what I know now, which is you only need lungs to get lung cancer. I didn’t think I had a risk for lung cancer.
Recall the moment of the diagnosis
It was actually a call that I received. My oncologist called me and wanted me to go into the office and set up an appointment, but I already knew why he called.
It’s not good news [when] an oncologist, who already said he thought it was probably benign, tells you he wants you to go into the office to get the news.
I convinced him on the phone to just tell me what was going on. That’s when I had the conversation about how it was malignant and adenocarcinoma. It was over the phone.
My stomach dropped. I don’t know if “shocked” is the right word, because I always knew there was a possibility it could be cancerous. I was very, very shaken by that news. I almost didn’t even know what to do next. It was a nightmare coming true.

Did you break the news to loved ones?
My husband was with me when I found out at home. At that point, I didn’t tell anyone. I didn’t tell my parents. I didn’t want to tell anyone yet because I had no idea what it was.
I wanted to get more information about where it came from and at least have the PET scan, which was the next thing that was scheduled, before I told anyone.
It was slightly complicated by the fact that my kids were young and somebody needed to watch them and get them to school when I went downtown to get to early morning appointments. I do remember telling a couple friends that I needed to get some tests done for my elbow, but I didn’t go into detail at that point.
Describe the actual PET scan
It didn’t take that long for me to get the PET scan scheduled. It was within the week.
Before you actually have the physical scan, you need to get an IV in your arm so that they can put in this (iodine-based) contrast material. That’s how they can see what areas in your body light up that have cancer, basically.
I went in, got my IV, had the contrast injected into the IV, and then I had to sit for about an hour in a room so that there was enough time for the contrast to spread throughout my body before the actual scan.
It was painless. You don’t feel any of that other than the stick of the IV. It’s a bit stressful because you’re sitting there by yourself, waiting for the scan.
The scan itself is relatively painless, too. It doesn’t take all that long. I laid down on a stretcher-type platform, went into the machine, and the scan didn’t even take longer than 30 minutes. Then it was done.
Thrust into a whole new world, overwhelmed by new terminology
This was the beginning of a whole new language. All of a sudden, people were talking about PET scans, getting contrast dye injected, and other scans I might need, like CT scans and brain MRIs. It’s overwhelming to go from being a normal, everyday person to entering the world of oncology.
There’s a lot of terminology you need to learn about. You’re learning about this at a time that you’re at your most vulnerable, because you’re terrified about what’s going on as it is. It’s hard to take all of that in.
Do you recall when you got the full diagnosis?
After the PET scan, I didn’t have to wait very long to find out the results. I found them out the same day while I was still in the hospital, treated in a major medical center in downtown Chicago. It was a quick process.
I remember my husband and I went back after lunch, and then we found out the results of the scan.
I sat down with the orthopedic oncologist. He told me that they found from the PET scan there were some areas in my lungs that had lit up, almost a 3-centimeter mass in my upper right lung, along with some small nodules, but that was the main area.
He also said they found the elbow mass also lit up, so it was also cancerous, as well as an area in my neck, where I had experienced my neck pain. There were a few other bones that did, my rib and my pelvis.
He said that was considered metastatic lung cancer and the next stage would be for me to talk to a thoracic oncologist. He referred me to someone and said he wanted to get someone from that department in the hospital to come in and speak to me that day.
It was over the holidays. My PET scan was on December 26, and it just wasn’t possible to get anyone to talk to me right then because a lot of people were on vacation.
How did you process the stage 4 lung cancer diagnosis?
My husband was there with me. To be honest, a lot of it is really a blur. I know we went home. I know I pretty much didn’t really want to talk to anyone.
I know my husband called his family, called my parents, and told them about the cancer diagnosis. It was a school day, so then my kids came home from school, and we didn’t want them to know what was going on yet. I had just been diagnosed. I didn’t know what my treatment was and what was going to happen.

We put on a fake smile on our face and went on with our regular day. It was almost surreal. I don’t remember a lot about those few days.
I was just trying to process everything and was very upset, crying tons, but also feeling like I wanted to hide that from my kids. It was a crazy time.
Genomic testing for biomarkers
I didn’t know this, but once they had determined it was lung cancer, my hospital, Northwestern, automatically sent my sample for molecular testing. Since this was back in 2013, they didn’t test for as many things as they test now.
They tested for EGFR, ALK, and KRAS. I didn’t know any of that was going on until I got a call from the nurse who works with my new thoracic oncologist, whom I hadn’t even met yet because my appointment was set for January. The nurse called me a couple of days before that appointment.
She was calling and getting my information. She asked if anyone had talked to me about molecular testing, and I said no, though I’d done some reading about it.
The nurse let me know that I had the EGFR mutation, which she said was a good thing because they had drugs and medications that I could take that could target that in the form of oral pills.
This is before I even met my thoracic oncologist. While it didn’t completely calm me down, it did make me feel like there was some hope.
It also changed completely how I thought my treatment would be.
Treatment plan: targeted therapy
Initially, as a person without a background in science and oncology, I had never heard of targeted therapy. I thought that my treatment was going to be what you think of when you think of someone with cancer. You have chemotherapy, you lose your hair, and you’re sick.
I found out from the nurse that it would be a very different type of treatment. That was the one bright ray of sunshine that clicked in before I actually met my oncologist.
Did you consider a second opinion?
I did not consider a second opinion. I was introduced through mutual friends to someone who lives 20 minutes away from me who’s also living with lung cancer, a woman about my age who’d been diagnosed a few years before me. She’s very involved in advocacy.
I talked to her right after I was diagnosed. She was the one who told me about mutations and targeted therapy, so I had somewhat of an idea of what molecular testing is when I spoke to my oncologist nurse.
She had also told me about who some of the best thoracic oncologists were to see in the area and even helped me get an appointment with Dr. Patel at Northwestern, who was my oncologist. I felt very, very good about the person I was seeing.

Treatment Decisions
What was the treatment plan?
I had mentioned that I found out I had an EGFR mutation on the phone with a nurse before I went into the office. When I went for my first appointment, Dr. Patel suggested I have a few more tests, one of which was a brain MRI, which I hadn’t had at that point.
That’s when I found out that I also had 8 small lesions in my brain, in addition to the bone involvement.
As a result of all of these additions, Dr. Patel decided that it would be a good idea for me to speak to a neurosurgeon and to a radiation oncologist in the hospital before we made the final decision about starting me right away or not on an EGFR targeted therapy medication.
Jumping from appointments to the next
During one very, very long day in the hospital, I ended up going to talk to a neurosurgeon because it turns out that the pain that I had in my neck, which was one of my early symptoms, was the result of a pretty large-sized tumor.
It was really high up on my cervical spine that didn’t show up in the initial MRI of my neck that my primary care physician had ordered.
When they got better visuals of that area, they realized that where it was located could actually cause my cervical spine to become unstable and possibly even collapse, which would not be good for my survival.
The neurosurgeon talked to me about the pros and cons of having surgery before I started on treatment for my EGFR mutation. That was one of the visits that I made that day.
Then I also went and talked to a radiation oncologist that day, who talked to me about the pros and cons of having radiation on some of those brain metastases after starting my targeted therapy.
I think the concern there was that if there were 8 small lesions that could be seen on the scan, there might be more lurking that might not even have showed up on the MRI. She gave me the impression that at some point, I might need to do whole-brain radiation.
I went to those 2 appointments and went back to Dr. Patel. I started that day being somewhat terrified, and I was beyond terrified by that time.
My husband was with me, so I had that support. To tell you the truth, it was just so overwhelming. I have to say I am very glad that I had all those conversations, and I’m glad all those doctors weighed in with their opinions and Dr. Patel talked to them.
They really figured out what would be the best approach by speaking and working together. I’m so glad that happened.
Final treatment decision plan
It turned out that Dr. Patel felt that by starting me on a targeted therapy for my EGFR mutation, which she explained to me could basically shrink the tumors or even have them disappear, that that might take away the brain metastases and reduce the tumor in my cervical spine.
The concern with my cervical spine was whether that tumor was actually keeping my cervical spine from collapsing. That’s where the neurosurgeon came in.
Guidance to other patients and caregivers on treatment decisions
When I was first diagnosed, I felt fortunate I found a doctor whom I really felt like I trusted. From the moment I talked to her nurse and the moment I talked to her, I felt she knew what she was talking about. I had verified that with the other lung cancer survivor I had met. I trusted her.
She listened to my questions and tried to get to know me as a person. I decided at that point in my day that I needed to go with that trust. I needed to allow the oncologist and her clinic to coordinate all my appointments and tell me what I needed to do next.
That worked for me, but I don’t know if that would work for everyone. It depends on who your initial doctor is, whom you start with.
Also, there was really no time for me to get a second opinion because of this concern about the lesion on my neck. I listened to her. I left the hospital that day with a prescription for my targeted therapy, while wearing a neck brace.
Why did you have to wear the neck brace?
I had to wear that neck brace for 3 months. That was the concession to the neurosurgeon. If I felt the slightest bit of pain or increased pain in my neck, I would go back and see him.
I did have to have regular follow-ups with the neurosurgeon for a while, every couple of weeks, just to see how my cervical spine was doing.
First-Line Treatment: Targeted Therapy, Afatinib
Describe the targeted therapy (afatinib)
It was a once-a-day oral medication. I took it every night before bed. I had to make sure that I didn’t eat for 2 hours before I took the medication, so no late night snacking after dinner. I had to make sure about that.
In terms of taking it, that was the only restriction.
What were the targeted therapy drug side effects?
There were side effects that I experienced. Very common side effects for these type of TKIs are rash, diarrhea, dry skin, and split fingernails or even the skin around your fingers.
At least at the beginning, I experienced all of those. Again, I have to say that my oncologist was very thorough about letting me know what to expect and what I could do from the very, very beginning to try to be proactive and get ahead of those side effects.
I gargled with mouthwash for mouth sores, I had a prescription to put on the rash if it developed, and I also had an antibiotic to take to prevent it from getting worse upfront. I went into treatment armed very, very well with ways to deal with and handle the side effects that I could develop.
It wasn’t that difficult of a process for me, but I was also very fortunate that I developed what seemed to me to be a good number of side effects, but a mild case for those side effects. Over time, I learned how to get out ahead of them.
How effective was the afatinib?
The bone in my neck that they were very concerned about grew back. I still remember a couple months after visiting my neurosurgeon, he said they wouldn’t have to do surgery. He said there was a profound improvement in my cervical spine, so that was amazing.
All of my brain metastases disappeared! The small nodules on my lung disappeared, while my main tumor shrunk a good amount but didn’t completely go away.
I felt pretty good. Those results continued for close to 3 years.
Managing cancer as a chronic illness
That’s exactly how I was approaching the lung cancer. I had to go back every 3 months during those initial 3 years for scans, and I still do.
In between scans, I pretty much would live a normal life. I was able to do things with my kids. I was driving places and seeing friends. It was a totally normal life.

You were living an active, normal life on the targeted therapy for 3 years
My family and I traveled a lot during those 3 years. I’ve always loved travel, so we went on several trips. I can’t remember which trips were prior to the afatinib’s efficacy slowing or stopping, but we did some fantastic trips.
We went to Puerto Rico, Iceland, Caribbean, to Mexico. We’ve done some really amazing trips! We continued traveling.
I got very involved in advocacy and traveling for lung cancer advocacy work as well. It really did not put any sort of damper on my activities.
Second-Line Treatment: Targeted Therapy (Osimertinib)
What brought you back to treatment?
In the middle of 2016, my oncologist moved from Northwestern to University of Chicago, so I went with her. My first scan of my lungs after that transition looked like I might have a little progression.
We weren’t completely sure because scans were being done on different machines and being read by different people. That sometimes makes things more difficult.
Describe the liquid biopsy
Liquid biopsies had started to become a thing. I had a Guardant360 liquid biopsy to see if anything would show up. Nothing did. The results of the liquid biopsy came back, and it was like I didn’t even have cancer. Literally nothing showed up.
It’s basically a blood test. You get a couple of extra vials of blood taken beyond the regular labs when you go in for a visit.
They send it away to a company that can look at that blood and see if they can cut mutations from cancer cells or pieces of DNA that are actually floating around in your blood.
If they find something, it’s fantastic because you don’t have to have a more invasive biopsy. But if they can’t find something, it’s not necessarily that the cancer isn’t there.
There are false negatives with liquid biopsies, where sometimes people are considered non-shedders, where their cancer doesn’t really shed those cancer cells or parts of cancer cells.
Frequently, if you are just beginning to have disease progression or you have a type of cancer where you don’t have tons of it in your lungs, you might be a non-shedder. That came back, and there were a lot of inconclusive results at the beginning.
Describe the lung tissue biopsy
Some time passed, and I went for my next scheduled CT scan. It looked like there still was some more growth. My oncologist scheduled me for a lung tissue biopsy, where again, this was an outpatient procedure, just a day procedure.
I went in, had twilight medication, and had a biopsy needle put into my lung to take out some tissue. I had that tested to see if I had developed some new mutation that might be able to be targeted with another type of targeted therapy.
What’s the T790M Mutation?
During the time I’d been treated at the beginning, a new drug went through trials and developed to treat T790M, which is a very common secondary EGFR mutation that people get who are treated with some of the original targeted therapies for EGFR, like afatinib and others.
When my results came back and they said I had the T790M mutation, I was able to go on this new targeted therapy medication, osimertinib.
Describe the osimertinib, second targeted therapy drug
I went on that and had a fantastic response to that one as well. The tumor in my neck and brain metastases had never come back since the beginning, but I had a remaining primary tumor in my lung.
That tumor ended up shrinking 50% from the size it originally was. While it hadn’t shrunk that much with the afatinib — it stayed stable — on this second drug, it had really decreased in size until it was about 1.5 centimeters.
Over what period of time did the tumor shrink?
It happened pretty fast, within the first 3 months. Then the tumor remained stable for an incredibly long period of time until I had surgery.
You’re still on the osimertinib
I’ve been on osimertinib now for a little over 4 years. My changes in treatment sort of went along with my oncologist changing hospitals.
At the very end of 2019, my oncologist went back to Northwestern from University of Chicago. They were all promotions for her. It was all in the Chicago area, so it wasn’t difficult for me.
But those switches did make things a little confusing in terms of my scans. When she changed locations, there was a question about whether there was progression in my lungs or not.
Still, nobody knows the answer to that, but a lot of time had passed at that point. I was 6 years out from my initial diagnosis.
Surgery (Lobectomy)
Surgery was brought up as next treatment step

While I was first diagnosed, no one would ever suggest a stage 4 lung cancer patient have surgery.
It was becoming an option for some stage 4 patients to be able to have more of an out-of-the-box treatment, meaning surgery or radiation, of their primary tumor in order to hopefully improve the patient’s overall survival.
Initially, when it was questionable whether my primary tumor was growing again, my oncologist asked how I felt about getting my primary tumor radiated since it was the only place that has even grown in my entire time since diagnosis.
I thought that was a good idea. It went to tumor board at my hospital. They came back and said I was a candidate for surgery. I decided if I was a candidate for surgery, I’d rather do that than radiation because I could [take out] an entire lobe of my lung out, where all of the cancer was, and hopefully not have side effects that might come from radiating that area of the lung. That’s what I ended up having done just about a year ago from today.
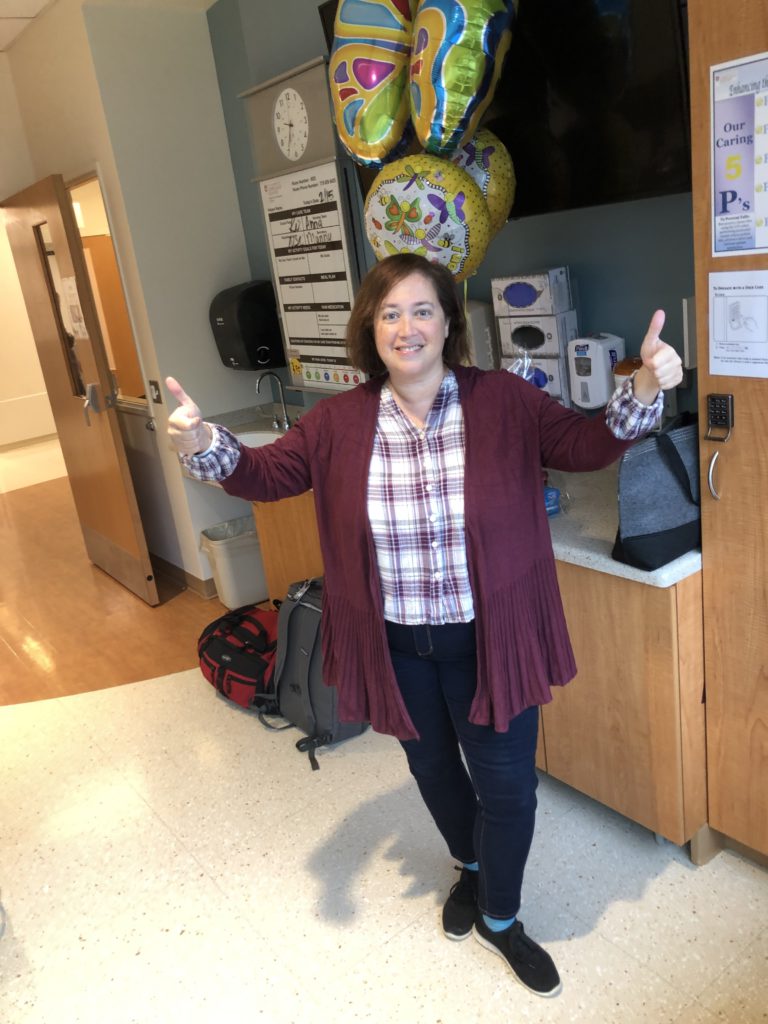
I had surgery, my upper right lobe removed, and as a result of that, became no evidence of disease (NED). It’s a year later, and I still have no evidence of disease!
How did you feel going into surgery?
Right before the lobectomy, I had to do a special bronchoscopy, even though I had a PET scan also prior, to make sure nothing lit up anywhere other than the primary tumor. They wanted to make sure there was no cancer in any of the lymph nodes outside of my upper right lobe.
That was the first thing because they wanted to make sure that if they were going to take out a portion of my lung, they wouldn’t find cancer somewhere else. That would negate the benefit.
I went to the hospital that day with my husband, changed, and got my IV. There I am with my surgeon (picture below) and her physician’s assistant (PA). This was general anesthesia.
It ended up actually being a 4-hour surgery. They removed my upper-right lobe. By the time I came out of surgery, they had me up and walking probably within an hour or 2.
I spent a total of 2 nights in the hospital. Getting up and walking a lot was key to both pain management and getting my lung capacity up again.
I won’t say it was pain-free, but I was so glad I had the surgery. I really am.

Guidance for others on recovering from surgery
There are 2 things to say here about that. I tend to be a person who usually doesn’t take pain medicine. I was given a lot of advice before the surgery. People said, “If you feel pain, you need to take that pain medicine before that pain becomes overwhelming.”
I did do that. I made sure to take advantage of the pain medicine that they were giving me. I was trying not to be a hero and tough it out. I think that made my recovery a little smoother.
I also made a big effort to get up and walk like they told me to, both in the hospital and once I got home.
I walk even to this day 30 minutes daily on the treadmill. I couldn’t do that right out of the hospital. In the beginning, I was walking 5 minutes on the treadmill, and that was enough, but I kept it going.
I’ve never been a marathon runner, but I don’t really notice any long-term impact on my lung capacity.
My advice would be to take your pain meds and walk as much as you can.
How was it hearing that you were NED?
No evidence of disease was never something I thought I’d ever hear when I was diagnosed. Stage 4 lung cancer, you don’t think you’re going to hear that.
It is amazing to hear. Does it mean the cancer will never come back? We don’t know, but it is hopefully going to last long enough to push things a little bit down the road. If it does come back, hopefully there will be newer and better treatment. Fingers crossed, it doesn’t come back. That’s always the hope.
Describe the ongoing treatment
My follow-up hasn’t really changed. I’m still taking the osimertinib because no one really knows what would happen if I stopped taking it in terms of brain meds and the lesion on my neck.
Since I really don’t have any side effects from my second targeted therapy, there’s no real advantage to getting off of it at this point.
I’m still on what’s termed “active treatment,” so I still see my oncologist every 3 months. Every 3 months, I have a CT scan of my neck and my chest to check my lungs and check that lesion. Every 6 months, I have a brain MRI. That’s the ongoing treatment at this point.

Navigating Life with Cancer
Describe living with cancer as a chronic illness
The whole living with my cancer, there is still a lot of uncertainty that comes with it because you still are living between scans. I do have to say earlier on in my whole my diagnosis journey, I probably experienced more anxiety between scans and getting ready for my next scan than I do now.
It’s twofold. It’s after you’ve been living with something for more than 7 years, it’s hard to sustain that amount of anxiety. Also, it helped me knowing that I’m currently no evidence of disease. That helps a little bit.
In addition, just the fact that I have gotten very involved in advocacy and am knowledgeable about the research and trials and treatments that are coming along. That also helped me feel a little bit better about things as they’ve progressed.
There are a lot of good options out there, and more are being developed. That has helped me a bit, too. I try to focus more on living each day and what I can accomplish that day, as opposed to worrying tons about the future.
I’m not saying that’s an easy thing to do. I’m over 7 years out. I’ve had a while to work on that — and a good amount of therapy — to work on that and figure it out, honestly.
Changing my mindset in that way has really helped me in managing the fact that I am living with these ups and downs and constant uncertainty and more anxiety. Then you have your time between scans, where things quiet.
How did you take care of your mental health?
I think it is critical to make sure that you take care of your mental health, as well as your physical health, if you go through something like a cancer diagnosis.
You shouldn’t feel in any way ashamed or like you don’t want to ask for help because, my gosh, a cancer diagnosis is a big deal. People shouldn’t feel like they need to know how to handle that.
If anything, it’s a huge, huge stressor. I cannot imagine having been able to handle living with lung cancer for over 7 years without having a therapist, without being on an antidepressant.
It has really helped me be able to keep myself in a good, stable mindset, in addition to being stable with my cancer so that I could live a good and balanced life.
You don’t want cancer to become your entire life. I’m able to talk about other things and be here for my husband, my kids, my friends, and my 89-year-old mom.
I can’t underestimate the impact of taking care of my mental health because it’s made it so that I’m not just surviving with cancer.
I’m actually living my life fully with cancer. I don’t think I would’ve been able to do that if I hadn’t made that a priority.
How to navigate marriage post-diagnosis
You have to have patience with each other, and you have to talk about things. It was very hard at the very beginning when I was first diagnosed. For him, his wife had just been diagnosed with lung cancer.
I also couldn’t drive because I was wearing a neck brace, and I was a stay-at-home mom at that point. He had to take over a lot of things that he hadn’t been doing. He had to help coordinate rides for our kids and do a whole bunch of other stuff that I wasn’t able to do for a while. On the flip side, once I started feeling better, I wanted all that back.
That was also difficult because he had gotten used to being an active helper, and then all of a sudden, I didn’t want that anymore. Those are things that can cause stress in anyone’s marriage.
In order to get through things like that, we just learned that we really had to talk it out, try to understand how each of us was thinking about things, and try to put ourselves into each other’s shoes. With a lot of patience, we’ve managed to work through issues like that when they arose.
How did you take care of your children while going through treatment?
Once I had that conversation with my oncologist nurse when she told me that I was going to be on an oral medication, that’s when we decided that we were going to tell the kids what was going on.
They were 10 and 12. We wanted to make sure that they knew that there was a plan and what the plan was going to be.
We sat down and told them, which to be honest was probably one of the most difficult things that I’ve ever done in my life, because you feel like you’re ripping their innocence away.

They’re kids, and they never think anything’s going to happen to their parents. Then they found out that I had lung cancer.
We have always tried to be honest with them but not give them information until we know the next play.
Even when I progressed, until I knew what was going to happen, there was no need to go into all of those details with them. We answer any questions, open questions, and all that, but we try not to create concern without addressing what the next plan is.
We also found early on that the boys didn’t really want to ask me questions about what I was going through. They wanted to ask my husband instead because they were afraid that they would upset me or they would say it the wrong way. They tended to go to him more and ask questions about what I was going through, but that was fine.
Again, 2 boys, 2 different personalities. One was more comfortable talking about things; one wasn’t. You have to take your cues from that and address each child with what they need. You might have to go to ask, “Do you have any questions? What are you thinking, and what might just be blurting it out in the breakfast table?” You have to go with their cues.
»MORE: Parents describe how they handled cancer with their kids
Did you seek out connections in the lung cancer community?
I wasn’t ready for it when I was first diagnosed, because different people are ready to connect with others at different times. I needed some time to just grieve.
I think the fact that my life was going to be different from what I expected, that’s when I needed the cancer community. In general, I am more of an extrovert.
After a certain period of months, I reached back out to the woman who I had been introduced to who lives near me. She also has lung cancer and is now one of my dearest friends and partner in advocacy.
Through her, I ended up getting connected with the LUNGevity Foundation, which is a patient advocacy group in lung cancer. They had a local walk that I participated in and met some people locally initially.
Then after some time, I went to one of their big summit events they have each year in Washington, DC, and met some more people. As that occurred, I met more people who were part of the lung cancer community and living with lung cancer.
I actually began to feel an even more sense of hope and potential for my future because I was meeting people who were living well with lung cancer, who were living very long-term, good lives.

Your Work in Patient Advocacy
How did that community relationship-building shift into advocacy?
I started to learn about advocacy opportunities and how I could help other people, which made me feel like I had a purpose. That was really important to me, too — to take what I had learned from talking to other people who had helped me along the way and pass it along to others.
That’s why I first got involved in advocacy. As time went on in advocacy, I found that what I really, really liked was learning more about the research.
Now, just quickly about my background, I have absolutely a completely non-scientific background. I was an English major as an undergrad. I have an MBA in finance, so there’s no science other than the required classes.

Once I was diagnosed with the disease, I wanted to learn all about it. Then once I learned as much as I could through attending conferences and things like that, I wanted to be able to help.
There were various different programs that you can participate in as a patient through the Department of Defense as a consumer reviewer, through ASCO and ACR, where you can help provide your patient perspective and research. I started doing those programs.

Talk about the patient group you co-founded: EGFR Resisters
In 2017, along with 6 other patients and a caregiver, I co-founded the EGFR Resisters Lung Cancer Patient Group, which is an advocacy group completely patient-founded and patient-driven for people like myself who have EGFR-positive lung cancer.
We pretty much are an online patient community. We’ve grown since our very beginnings of just 7 of us to about 2,500 people now from 75 different countries. We have a closed Facebook group where members who are patients and caregivers can interact, learn from each other, support each other, and learn to advocate for themselves.
We share tons of information in this group about things like second opinions, clinical trials, symptom management, and everything. We also are trying to help accelerate research in our own type of lung cancer.
We’ve partnered with other advocacy groups and industry organizations to actually do research on our own disease and also to raise funds to sponsor additional research.
It’s been a very, very fulfilling way for me to get involved in the lung cancer community and both make a difference in other patients’ lives and then hopefully in the ultimate detection, diagnosis, and treatment of lung cancer as well.
You’re proof of the importance of advocacy and pushing for better treatments
If it wasn’t for this research, I wouldn’t be here right now. I fully know it. I had the benefit of these 2 targeted therapies. Both were FDA approved literally months before I started taking them. Surgery is still a cutting edge thing to do in stage 4 patients.
I can see what difference these research and developments can make for people. I can’t tell you how incredibly important I feel like it is to focus and promote more research.
Top issue #1 in lung cancer research: resistance to treatment
One of the biggest things is resistance to treatment for any type of treatment you have, whether it’s targeted therapy, chemotherapy, or immunotherapy. Eventually, somehow the cancer figures out a way to change — not always, but very, very frequently — and get around the treatment, making it necessary to find a new treatment.

That’s a big issue right now in cancer research. We keep developing new treatments to tackle resistance, trying to figure out what’s driving the resistance and how to tackle it.
There’s also starting to be more and more studies on:
- Why is resistance happening?
- What is it?
- Are there some cells that just can never disappear, that go into a sleep mode, and they’re called persister cells that then pop up later on?
- What causes that to happen?
That’s a really, really big topic in lung cancer right now.
Top issue #2 in lung cancer research: precision medicine
I think the other really big topic is just an increased use of precision medicine. There are more and more different subsets of lung cancer that have been uncovered, and different types of lung cancer are treated differently.
Not every type of lung cancer responds the best to the same treatment. There’s been a lot done in terms of finding different mutations like EGFR, like I have, but there’s also work being done in terms of immunotherapy and how to find out which are the best candidates for responding to particularly different types of immunotherapy.
I really think that another focus right now that we’re seeing in lung cancer is narrowing down who responds the best to certain treatments so that people who are diagnosed can start with the best treatment right upfront.
More attention now on rarer types of lung cancer
People are paying more attention to some of the rarer types and subsets of lung cancer, like small cell lung cancer. It’s often very, very deadly but hard to treat.
I’m starting to see a lot more about small cell lung cancer in development. Squamous cell lung cancer is another one. Leptomeningeal disease, which affects the brain and is difficult to treat.
Advances in some of these more difficult-to-treat subsets of lung cancer — those are becoming more and more important and being looked into with increased amounts of research as well.

Final message to other patients and caregivers
The biggest message that I can share is the message of hope, to tell you the truth. Things have changed so much in lung cancer in the 7 years since I was first diagnosed. 7 years isn’t that long in the grand scheme of things.
When I was first diagnosed, immunotherapy didn’t even exist. It was like science fiction. People were talking about it, but they didn’t know what kind of promise that would have. Half of the mutations that are now being tested for in lung cancer hadn’t even been discovered yet.
If you go another decade back beyond my 7 years, all lung cancer patients were pretty much dealing with the same 1 or 2 chemotherapy drugs. In such a relative short time, we have come so far.
This is a good time to be a lung cancer patient. If you end up being a lung cancer patient, there are so many developments, and there are so many new ideas. Patients are living longer and better with lung cancer because of these new treatments. There’s such a potential for more upcoming treatments.
Check out Ivy’s group: EGFR Resisters website

Inspired by Ivy's story?
Share your story, too!
Non-Small Cell Lung Cancer Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza